Abstract
Background: Rotavirus is globally the most common viral pathogen in childhood gastroenteritis. This study aimed to estimate the number of Turkish children suffering from early-childhood gastroenteritis by rotavirus by performing a meta-analysis. Methods: Meta-analysis following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was performed. Following the guidelines, primary studies were found reporting the prevalence of rotavirus gastroenteritis in Turkey. We performed a computerized search of published studies in national and international databases from 1990 to 2018. We selected 38 out of 721 studies for our study. Meta-analysis was carried out using R statistical software. The Cochrane Q statistic was calculated to assess the heterogeneity of the study results. Heterogeneity among studies was evaluated using the I2 statistic. Effect-size estimate was reported with 95% confidence interval. Results: On the basis of 38 selected articles, 80,113 children up to five years of age were diagnosed with symptoms of acute gastroenteritis, of whom the stool samples of 13,651 children were positive for rotavirus. The pooled prevalence of rotavirus was 19% in children younger than five years of age with acute gastroenteritis. In terms of seasonal prevalence, the highest prevalence rate was found in winter. Conclusion: This study supports the major prevalence of early-childhood gastroenteritis by rotavirus among Turkish children. Therefore, the decision to adopt immunization programs to prevent rotavirus infection might be helpful in Turkey.
1. Introduction
Diarrhea is one of the world’s top three infectious diseases that cause death. Viral gastroenteritis is most prevalent among infectious diarrhea, especially in childhood [1,2,3]. Diarrheal disease is the leading cause of death in early childhood, mostly in developing countries [1,3]. However, rotaviruses are the second leading cause of vaccine-preventable disease deaths after pneumococcal pneumonia in children under five years of age [4]. Rotavirus is highly contagious among children. Most children experience several episodes of rotavirus infection during the first years of life. Rotavirus is the leading etiologic agent of acute gastroenteritis in children under the age of five years. Due to rotavirus diarrhea, there are 111 million diarrhea attacks, 25 million outpatient clinics, and 2 million children hospitalized every year [3,5]. Diarrhea, vomiting, fever, abdominal pain, and dehydration occur in infants and children with rotavirus infection. In children under the age of two, the risk of dehydration is higher and may require hospitalization.
The virus is highly resistant to environmental conditions and can survive for months at room temperature [4]. Unlike other agents that cause gastroenteritis, rotaviruses are seen in the same frequency in developed and developing countries [1,3]. Rotavirus gastroenteritis causes mortality in developing countries where treatment options are insufficient and morbidity and economic losses in developed countries [1,5,6]. Although several studies were conducted in Turkey related to rotavirus infection, data are not available to develop preventive policies and programs. This study is the first meta-analysis on the prevalence of rotavirus gastroenteritis among the Turkish early-childhood population. This study’s primary purpose was to calculate pooled prevalence and evaluate the epidemiology of rotavirus infection in children younger than five years of age with acute gastroenteritis.
2. Methods
2.1. Systematic-Review Registration
A search protocol was prepared and registered with the PROSPERO database (PROSPERO/CRD42019117809. https://www.crd.york.ac.uk/prospero/export_details_pdf.php). Meta-analysis with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was performed. Different phases of the study included searching for, screening, and selecting studies, and extracting, cleaning, and analyzing the data.
2.2. Search Strategy and Screening
We conducted a computerized review of the articles related to the subject published in national and international databases from 1990 to 2018. Ulakbim Turkish Medical Literature (ULAKBİM, Ankara, Turkey) and TürkMedline National Biomedical Periodicals (Turkish Medline) were used as national databases. As international databases, the literature was searched in the Embase, PubMed, Web of Science, Scopus, and Google Scholar databases. We used the following terms during the search: “rotavirus infections/epidemiology” OR “gastroenteritis/epidemiology” OR “diarrhea/epidemiology” AND “Turkey” AND “humans” AND “infant” OR “infant, newborn” OR “infant” OR “child, preschool”.
2.3. Study Selection
Prospective epidemiological, cross-sectional, and cohort studies that reported the prevalence of rotavirus infections in children with acute gastroenteritis were used. The titles and abstracts were scanned for possible inclusion. Meta-analysis was restricted to studies published in the English and Turkish languages. Studies on rotavirus epidemiology and prevalence only in Turkish children were evaluated.
2.4. Inclusion Criteria
The study participants had to be children under five years of age with acute gastroenteritis. positive and negative rotavirus results had to be reported. The rotavirus infection in these children was assessed by one of the acceptable laboratory diagnostic tests, including polymerase chain reaction (PCR), enzyme immunoassay (ELISA), immunochromatographic-method (IM) rapid test, and latex agglutination (LA). Articles written in English and Turkish with full texts were included.
2.5. Exclusion Criteria
Studies that had the following characteristics were excluded: studies using nonstandard methods, duplicate studies, studies published in languages other than English or Turkish, studies on ages other than early childhood, nonhuman studies, congress abstracts, review articles, meta-analyses, and articles only available in abstract form.
2.6. Quality Assessment
The researchers assessed the quality of articles with a checklist of Strengthening the Reporting of Observational Studies in Epidemiology (STROBE), using a PRISMA checklist and diagram. The majority of studies selected for this study had been assessed to be of moderate-to-good quality. Scores of 4 or less were evaluated as weak, between 5 and 7 as moderate, and between 8 and 10 as good. Articles thought to be of lower quality were excluded. The quality of the studies documented in the articles was primarily evaluated on the basis of tests used to detect rotavirus, age groups, and seasonal distribution.
2.7. Data Extraction and Definitions
Within the scope of the PRISMA report, exclusion criteria were determined at the first stage, and a literature review was carried out. In the next steps, the literature was re-examined with the exclusion criteria in mind; study data were collected, and statistical analysis was performed. Variables such as the name of the first author, duration of the study, year of study, the number of rotavirus gastroenteritis cases, and diagnostic methods were determined and recorded on the form. These data were obtained from only published articles in national and international journals. Both authors independently evaluated articles for compliance with the study criteria.
2.8. Meta-Analysis
We collected and cleaned the data on a Microsoft Excel sheet. We used the meta package of the R statistical software for standard meta-analysis [7]. Heterogeneity was assessed using the Q test and the I2 statistic. Effect-size (ES) estimate was reported with 95% confidence interval (CI). The p-value assessed the statistical heterogeneity between studies for Q test < 0.001 or I2 statistic of more than 50%. To assess any possible publication bias, the Begg rank-correlation and Egger weighted-regression methods, in combination with a funnel plot, were used. A p value of <0.05 was considered to be statistically significant.
3. Results
3.1. Description of Individual Studies
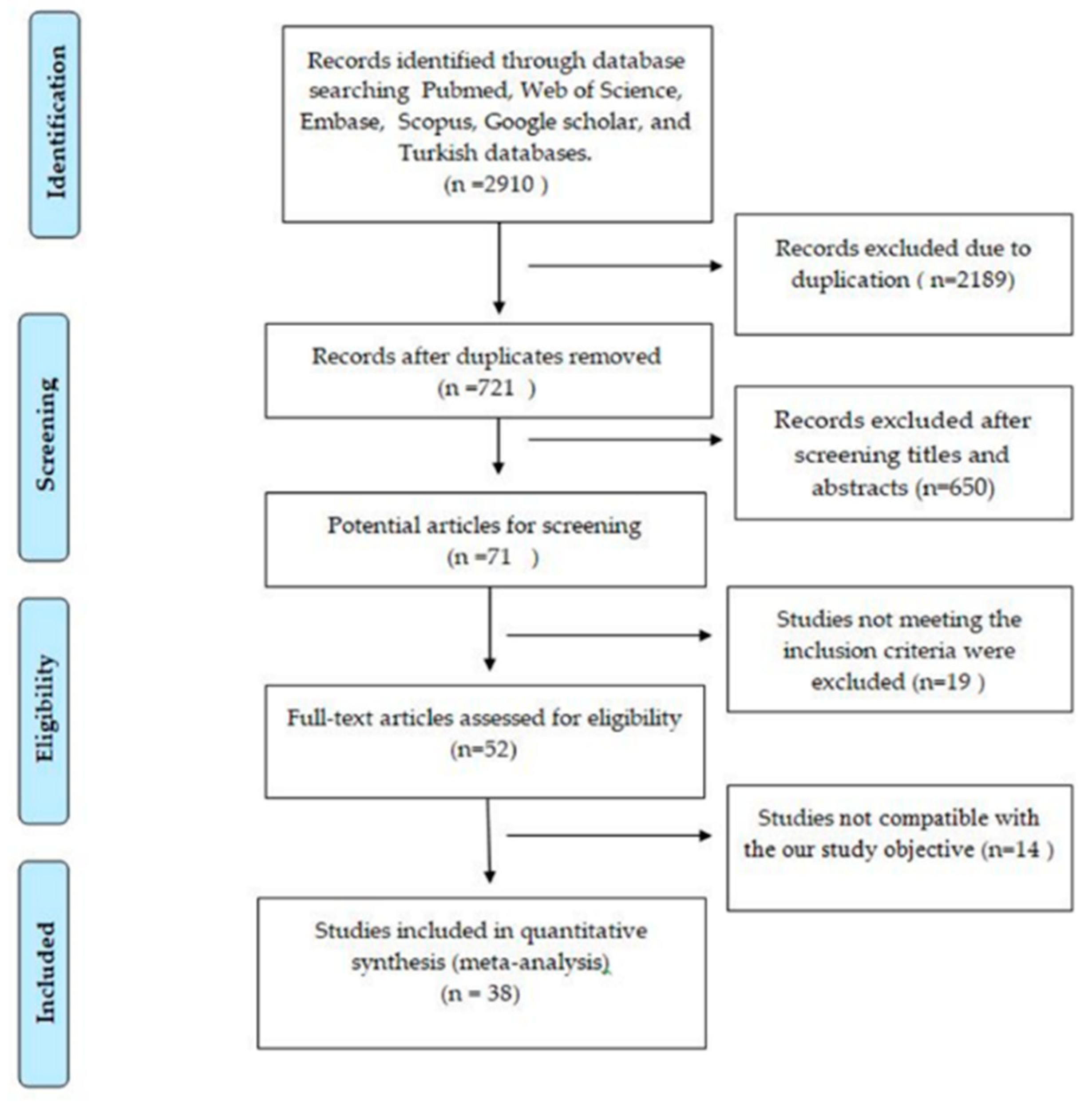
Overall, 2910 studies were identified with electronic searching. Out of these 2910 studies, 2189 were duplicates. In total, 721 potential articles were screened, and 650 were not included because they were not directly related to our study. After reviewing the full text of 71 related articles, they were checked for eligibility criteria. As a result, 19 studies were excluded. Lastly, 38 studies evaluated the epidemiology of rotavirus infection in children younger than five years of age with acute gastroenteritis. The study-selection process is shown in Figure 1, and the main characteristics of the selected studies are described in Table 1 [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
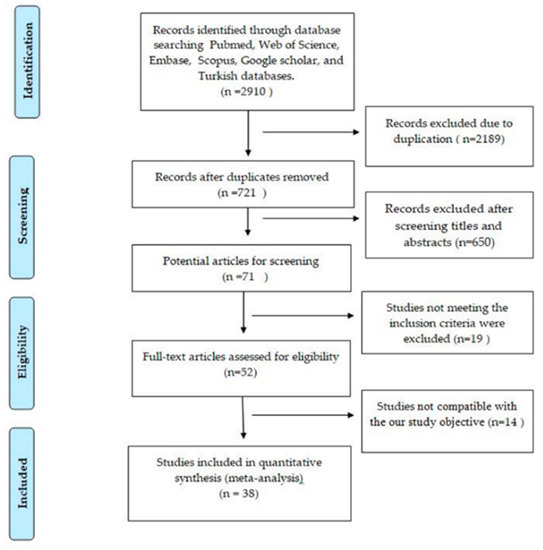
Figure 1.
Flowchart of selection of utilized studies in meta-analysis.

Table 1.
Characteristics of studies included in meta-analysis.
3.2. Prevalence of Rotavirus Infection among Children under Five
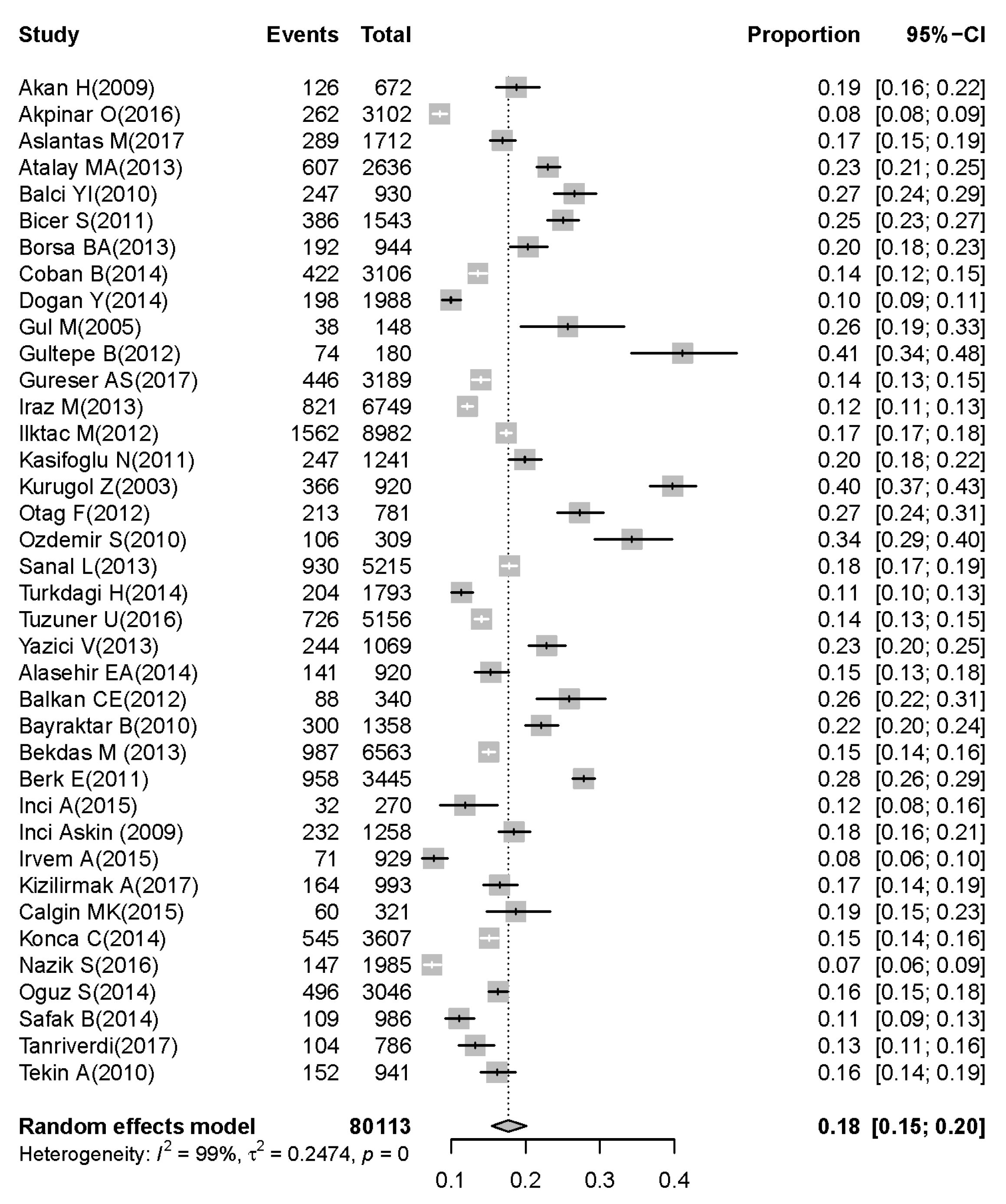
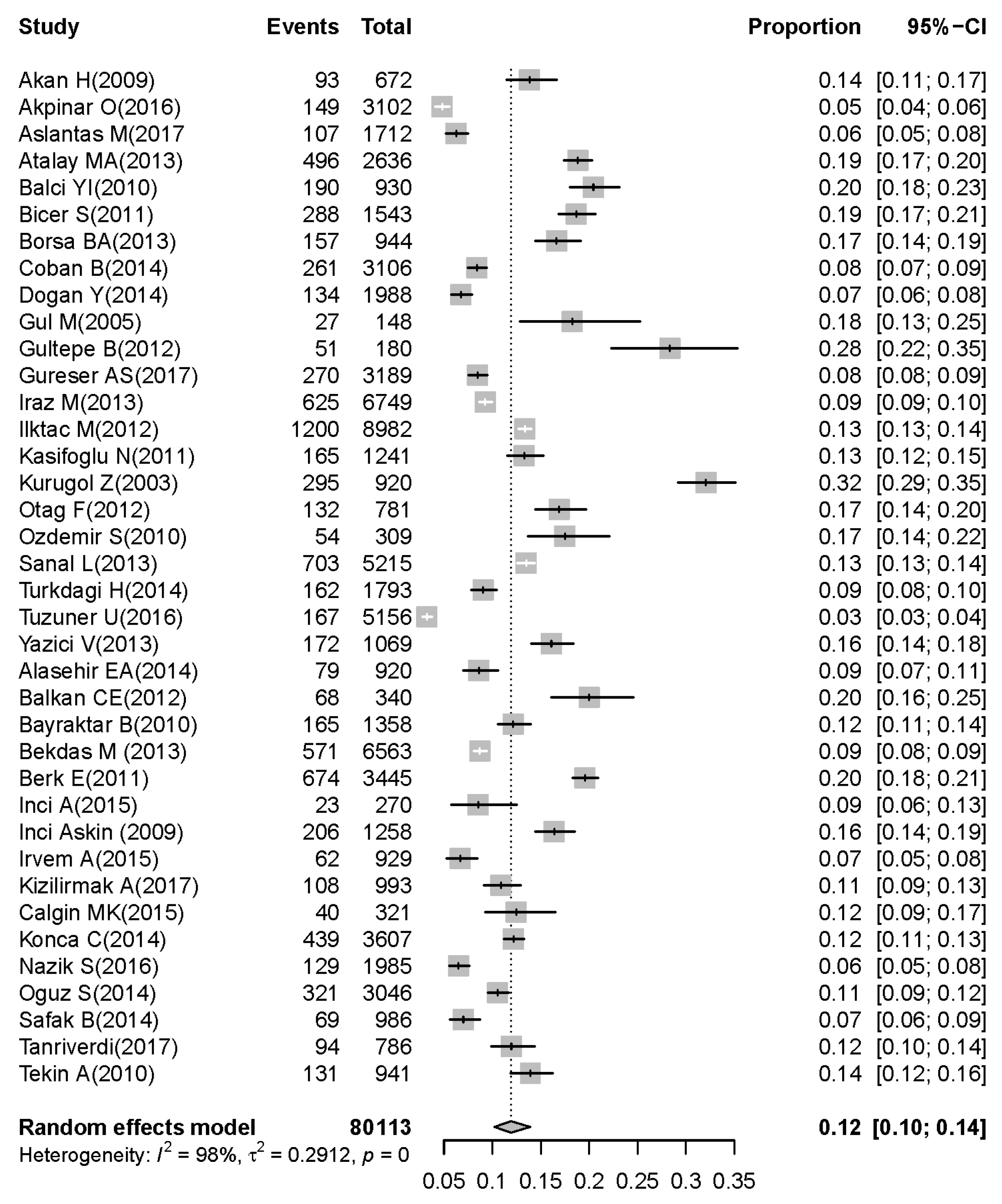
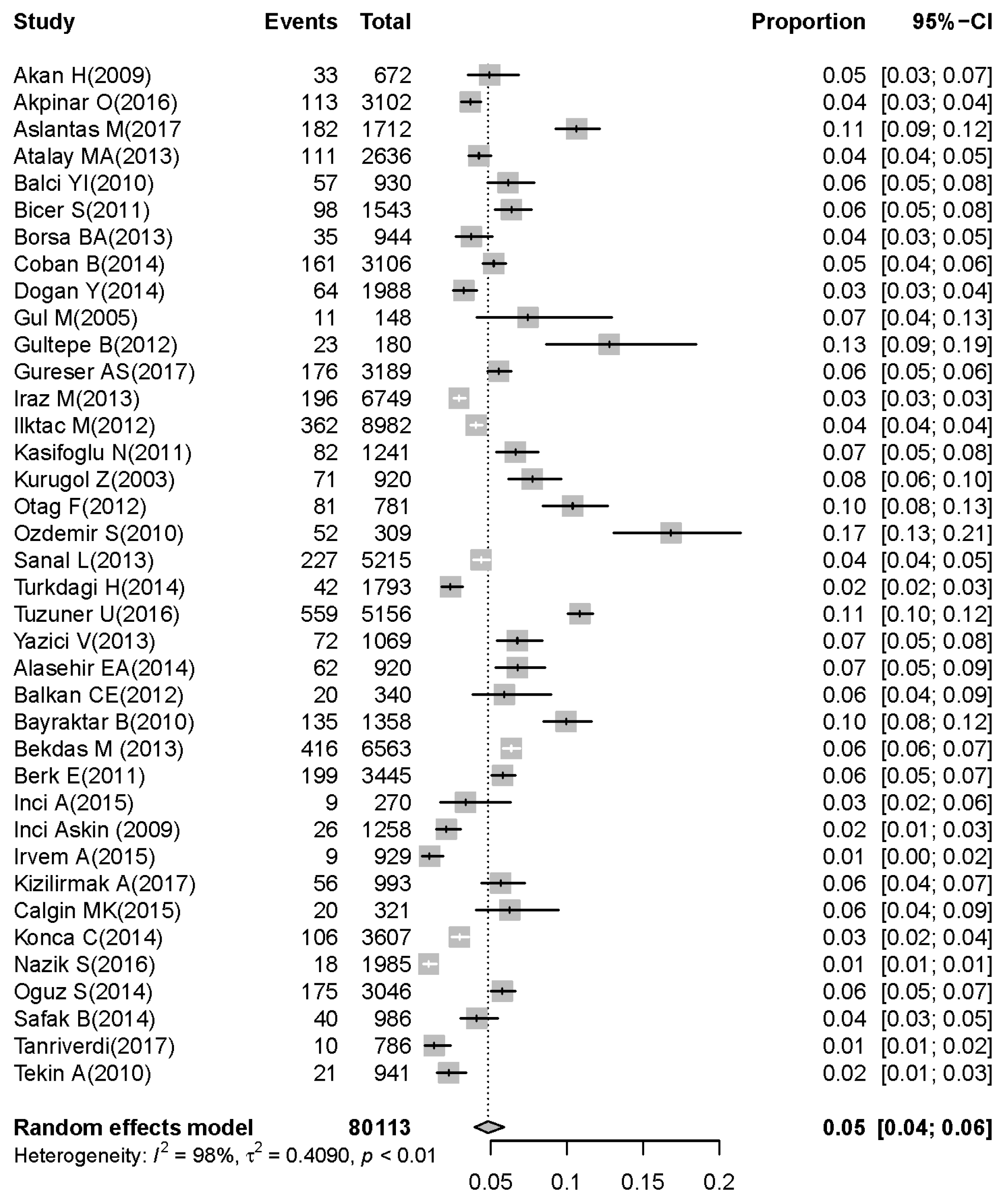
On the basis of the 38 selected articles [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45], 80,113 children under five years were diagnosed with symptoms of acute gastroenteritis, of whom the stool samples of 13,651 children were positive for rotavirus. The pooled prevalence of rotavirus was 18% (95% CI: 15–20) in children under five years with acute gastroenteritis (Figure 2). The prevalence of rotavirus was 12% (95% CI: 10–14) in children younger than two years (Figure 3). The prevalence of rotavirus was 5% (95% CI: 4–6) in children between two and five years with acute gastroenteritis (Figure 4).
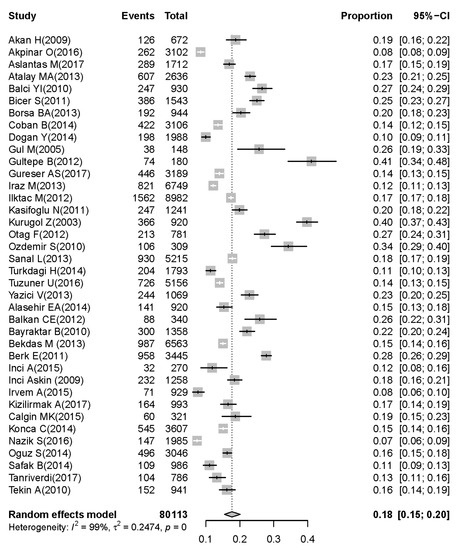
Figure 2.
Prevalence of rotavirus-associated acute gastroenteritis cases in early childhood (0–5 years; results of meta-analysis for pooled prevalence with 95% confidence interval and its forest plot).
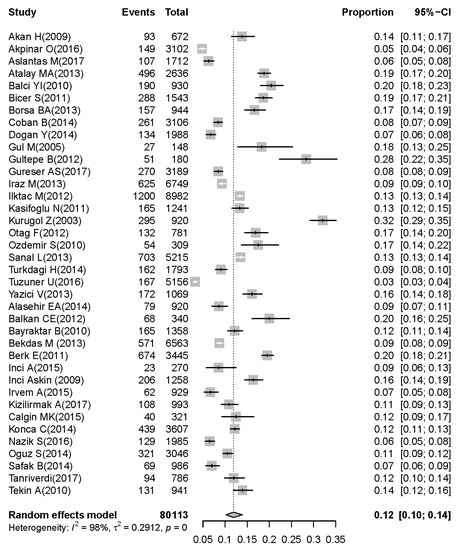
Figure 3.
Prevalence of rotavirus-associated acute gastroenteritis cases in children aged 0–2 years.
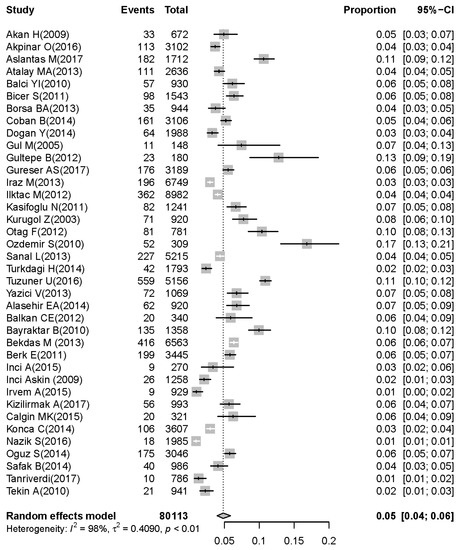
Figure 4.
Prevalence of rotavirus-associated acute gastroenteritis cases in children aged 2–5 years.
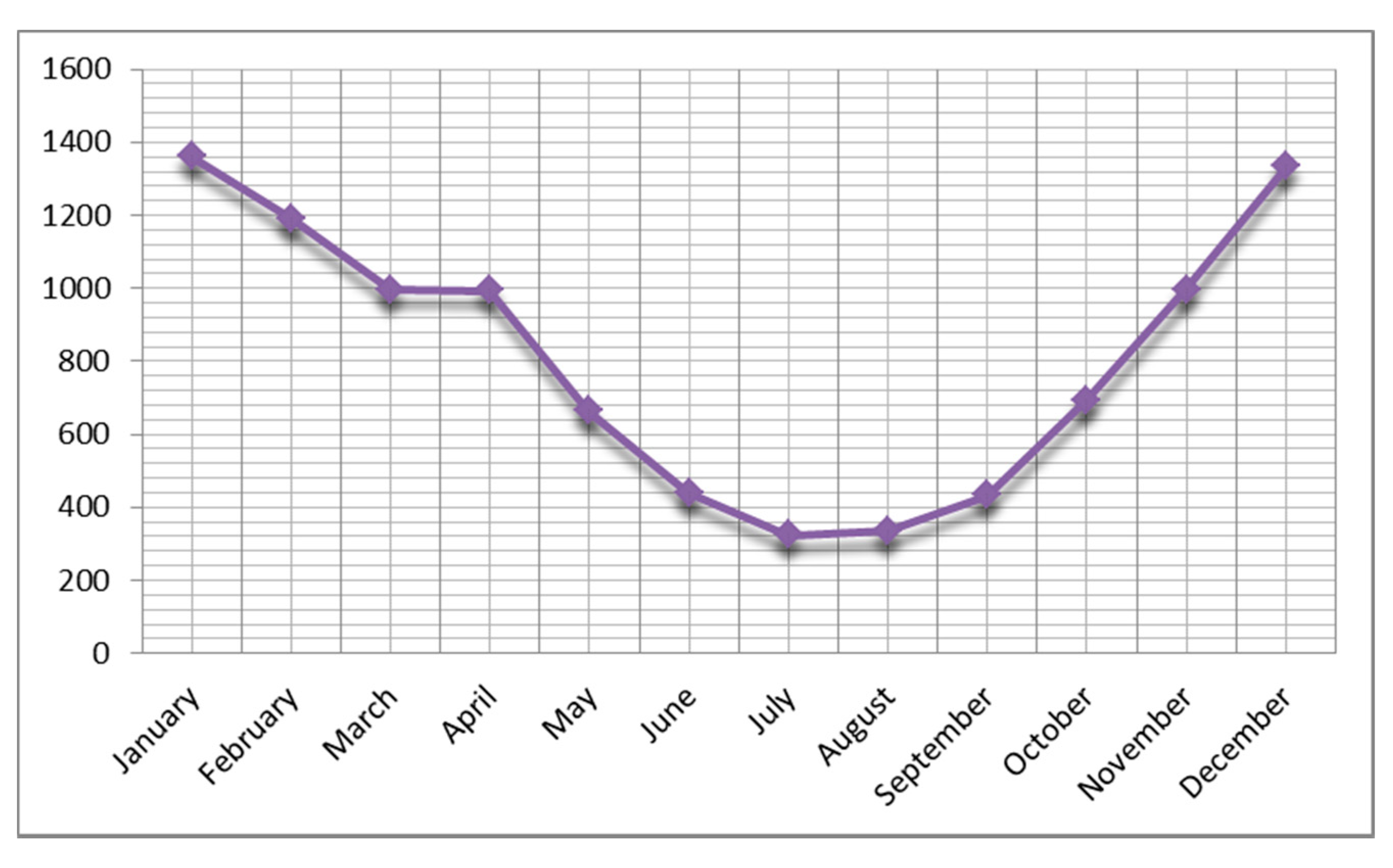
3.3. Seasonal Distribution of Rotavirus Infection
In terms of seasonal prevalence, the highest prevalence rate was found in winter (4532/13,778; 32.9%). In addition, seasonal distribution was 3652/13,778 (26.5%) in spring, 3500/13,778 (25.4%) in autumn, and 2080/13,778 (15.1%) in summer. The highest incidence of rotavirus was observed in winter and spring. The ratio of rotavirus positivity was highest in December and January, while the lowest ratio was in July. This result was statistically significant (p = 0.001). The seasonal distribution is demonstrated in Figure 5.
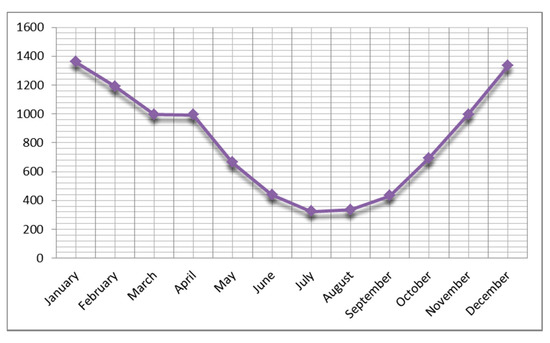
Figure 5.
Distribution of prevalence of rotavirus gastroenteritis by month.
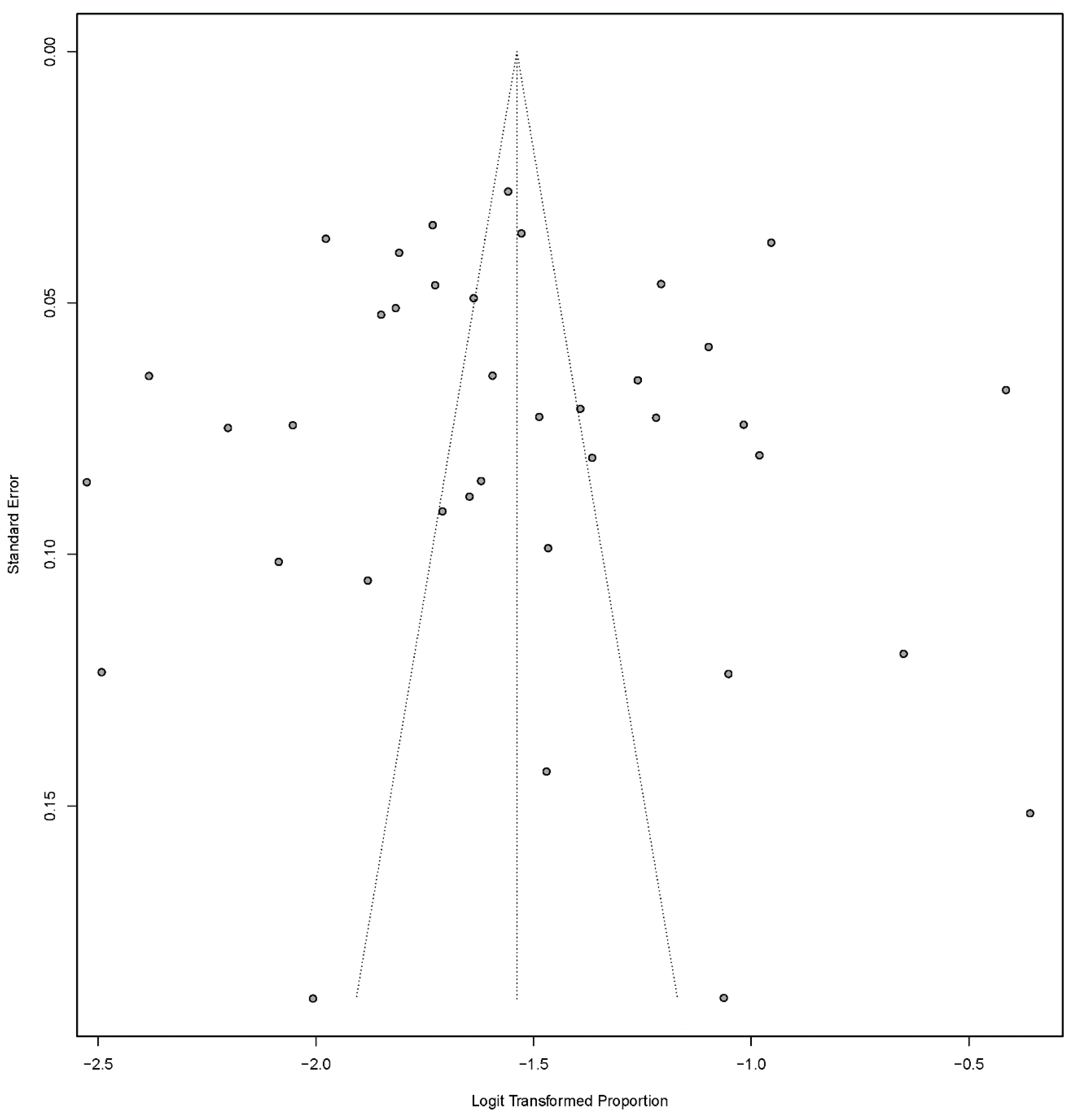
3.4. Meta-Analysis Results
Heterogeneities between studies (Cochran’s Q-test, I2 = 99.0; p < 0.001) were found, so the random-effect model was used for meta-analysis. Details of the meta-analysis are summarized in Figure 2, Figure 3 and Figure 4. To assess possible publication bias, Begg rank correlation, Egger weighted regression tests, and a funnel plot were used. The results of Begg rank correlation were Z value for Kendall’s tau of 0.29 and p = 0.77 (p > 0.05), and those of the Egger weighted regression test were intercept −1.62, t = 0.40, and p = 0.69 (p > 0.05). No evidence of publication bias was observed. The funnel plot for the prevalence rate of rotavirus is shown in Figure 6.
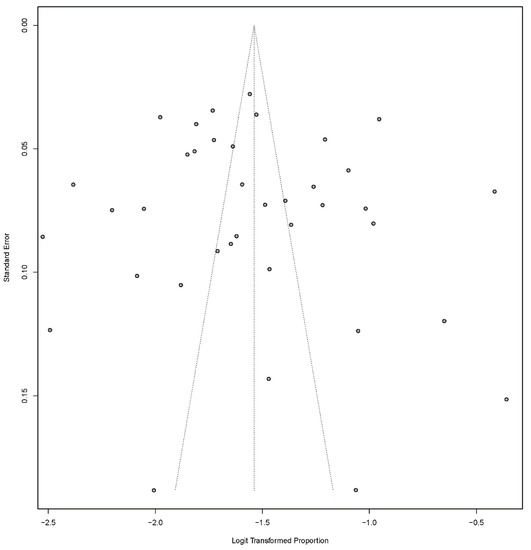
Figure 6.
Funnel plot of prevalence of rotavirus-associated acute gastroenteritis cases in early childhood among Turkish children.
4. Discussion
Acute gastroenteritis is the most critical health problem in early childhood. Diarrhea-related mortality was partially reduced due to advances in safe water and sanitation, as well as reduced undernutrition in early childhood [1,2]. Viral gastroenteritis is the most common cause of hospitalization in early childhood. Gastroenteritis caused by rotaviruses, also defined as a “democratic” virus, occurs at a similar frequency in developed and developing countries regardless of cleaning conditions [24]. Globally, most viral acute gastroenteritis cases are caused by rotavirus in children, especially in the first five years of life [1,2,6]. Rotavirus (RV) is one of the 13 gastroenteritis etiologic agents shown in the Global Burden of Disease Study [1,3,8]. Rotaviruses are the second leading cause of vaccine-preventable disease deaths after pneumococcal pneumonia in early childhood. In this context, the World Health Organization recommends that all countries add rotavirus vaccines to their national vaccination programs [4,46]. In Turkey, both monovalent and pentavalent vaccines were licensed in 2006. However, these vaccines are not funded by the Turkish national health system. The vaccine is not included in the national routine-vaccination program, but is available from pharmacies. Although not included in the routine national immunization program, the RV vaccination rate in Turkey was approximately 16% in 2018 [46]. Our study is the first and only meta-analysis of rotavirus-associated acute gastroenteritis cases in early childhood in Turkey.
According to data from the World Health Organization, the rotavirus-related mortality rate of children under five years was found to be 1.7 per 100,000 in 2013 in Turkey. Rotavirus-related deaths were reported to be 0.4% of all deaths of children under five years of age [1,3,8]. Turkey has a low child mortality and low adult mortality group in the European B group when analyzing countries by region and the type of death [47]. According to our study results, the overall proportion of rotavirus infection among gastroenteritis cases was 18% (95% CI: 15–20) in children under five years of age; in children under two years of age, this rate was 12% (95% CI: 10–14) These rates were found to be consistent with WHO data. Rotavirus gastroenteritis is very common in infants and young children. Early-childhood children, especially between the ages of six months and two years, are incredibly vulnerable. Due to the high incidence, morbidity, and mortality risk in this age group, research is focused on the pediatric-age group [3]. The rates of rotavirus-positive cases reported from other parts of the world are highly variable, varying between 20% and 50% in different countries and different pediatric-age groups [9]. This rate was reported as 27–52% in European countries [48]. In a study involving 20 countries in the Mediterranean region, the median rate of rotavirus diarrhea in children with acute gastroenteritis was 40% in hospitalized children and 23% in outpatients [49]. Another study covering the Middle East determined the overall percentage of rotavirus detection among gastroenteritis cases ranging from 16% to 61% [50]. A study of rotavirus infections and genotype distribution reported them to be 31.8% in children under five years of age and 25.9% in children under two years of age [51]. In our study, the seasonal distribution of rotavirus gastroenteritis was higher, especially in the spring and winter months. The proportion of children with gastroenteritis positive for the rotavirus antigen was found to be high between November and April, and it was highest in January and December. The lowest rates were recorded in July and August (Figure 5). The seasonal distribution of rotavirus gastroenteritis in European countries is similar to that in the United States [52]. Rotavirus gastroenteritis peaks in France and northern Europe in February or March. The Netherlands and Finland peak in March, while Spain generally has high rates in December and February. In Africa, the incidence of disease peaks during the dry season.
Interestingly, in December and January, the rate of rotavirus is the lowest in Iran, the eastern neighbor of Turkey [53,54]. As seen in the results of the study, although it is seen at the highest rates in winter and spring, the seasonality of this diarrhea form changes in different parts of the world. In our study, we determined a significant difference between disease rates in December, January, and February and its rates seen in other months.
Study Limitations
Since the vaccination rates could not be reached in the articles, pre- and postvaccination evaluations could not be made.
5. Conclusions
Rotaviruses are the most critical form of viral gastroenteritis in childhood. They remain a significant public health concern because of their global social and economic burden. Accurately diagnosing and treating gastroenteritis factors in early childhood helps patients to quickly recover and avoid unnecessary costs. This study revealed that rotavirus is associated with gastroenteritis in Turkish children. We also demonstrated an epidemiologic picture of rotavirus gastroenteritis in Turkey. This study provides information about the different geographical areas of Turkey, and it is essential for drawing attention to the early-childhood route of viral gastroenteritis in Turkey.
Author Contributions
Conceptualization, methodology, supervision, writing original draft, and investigation, O.A. and M.G. Data curation, formal analysis, software, review and editing, M.B.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- GBD Diarrhoeal Diseases Collaborators. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect. Dis. 2017, 17, 909–948. [Google Scholar] [CrossRef]
- Wazny, K.; Zipursky, A.; Black, R.; Curtis, V.; Duggan, C.; Guerrant, R.; Sherman, P.M. Setting research priorities to reduce mortality and morbidity of childhood diarrhoeal disease in the next 15 years. PLoS Med. 2013, 10, e1001446. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Naghavi, M.; Allen, C. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of disease study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef]
- Leung, D.T.; Chisti, M.J.; Pavia, A.T. Prevention and control of childhood pneumonia and diarrhea. Pediatric Clin. 2016, 63, 67–79. [Google Scholar] [CrossRef]
- Badur, S.; Öztürk, S.; Pereir, P.; Abdel Ghany, M.; Khalaf, M.; Lagoubi, Y.; Ozudogru, O.; Hanif, K.; Saha, D. Systematic review of the rotavirus infection burden in the WHO-EMRO region. Hum. Vaccines Immunother. 2019, 15, 2754–2768. [Google Scholar] [CrossRef]
- Troeger, C.; Khalil, I.A.; Rao, P.C.; Cao, S.; Blacker, B.F.; Ahmed, T.; Kang, G. Rotavirus vaccination and the global burden of rotavirus diarrhea among children younger than 5 years. JAMA Pediatr. 2018, 172, 958–965. [Google Scholar] [CrossRef]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with R: A practical tutorial. Evid. Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef]
- Akan, H.; İzbırak, G.; Gürol, Y.; Sarıkaya, S.; Gündüz, S.T.; Yılmaz, G.; Hayran, O.; Vitrinel, A. Rotavirus and adenovirus frequency among patients with acute gastroenteritis and their relationship to clinical parameters: A retrospective study in Turkey. Asia Pac. Fam. Med. 2009, 8, 8. [Google Scholar] [CrossRef]
- Akpınar, O.; Akpınar, H.; Keskin, E.Ş. Investigation of group a rotavirus antigen frequency in children who have acute gastroenteritis with immunochromatographic methods. J. DU Health Sci. Inst. 2017, 7, 78–81. [Google Scholar]
- Aslantaş, M.; Kılıçaslan, Ö.; Engin, M.; Büyük, N.; Yalçın, G.; Ankaralı, H.; Kocabay, K. Prevalence of rotavirus and adenovirus in children with acute gastroenteritis: A tertiary care hospital data. Fam. Pract. Palliat. Care 2017, 3, 1–5. [Google Scholar] [CrossRef]
- Atalay, M.A.; Kandemir, İ.; Gökahmetoğlu, S. Frequency of rotavirus infection in children with gastroenteritis in a tertiary hospital. Dicle Med. J. 2013, 40, 212–215. [Google Scholar] [CrossRef]
- Yasemin, I.; Balcı, I.; Polat, Y.; Çövüt, İ.E.; Canural, R.; Görüşen, İ.; Sarı, F. Frequency of rotavirus and adenovirus types 40/41 in children with gastroenteritis between 0–5 years of age in Denizli. Yeni Tıp Derg. 2010, 27, 15–17. [Google Scholar]
- Biçer, S.; Sahin, G.T.; Koncay, B.; Gemici, H.; Siraneci, R.; Ozturk, N.Y.; Sevketoğlu, E. Incidence assessment of rotavirus and adenovirus associated acute gastroenteritis cases in early childhood. Infez. Med. 2011, 19, 113–119. [Google Scholar] [PubMed]
- Borsa, B.A.; Tokman, H.B.; Çağatay, P. Determination of rotavirus and adenovirus frequency. Ankem Derg. 2013, 27, 75–79. [Google Scholar] [CrossRef]
- Çoban, B.; Topal, B. Evaluation of rotavirus gastroenteritis in children: Five years surveillance in Alanya, Antalya. Turk. J. Pediatr. 2014, 56, 280–284. [Google Scholar] [PubMed]
- Doğan, Y.; Ekşi, F.; Karslıgil, T.; Bayram, A. The investigation of the presence of rotavirus and adenovirus in patients with acute gastroenteritis. Türk. Mikrobiyol. Cem. Derg. 2014, 44, 18–22. [Google Scholar]
- Gül, M.; Garipardıç, M.; Çıragil, P.; Aral, M.; Karabiber, H.; Güler, L. Investigation of rotavirus and adenovirus types 40/41 in children with gastroenteritis between 0–5 years of age. Ankem Derg. 2005, 19, 64–67. [Google Scholar]
- Gültepe, B.; Yaman, G.; Çıkman, A.; Güdücüoğlu, H. The frequency of rotavirus and adenovirus among childhood gastroenteritis. Türk. Mikrobiyol. Cem. Derg. 2012, 42, 16–20. [Google Scholar]
- Güreser, A.S.; Karasartova, D.; Taşçı, L.; Özkan, T.H.A. Rotavirus and adenovirus frequency in children with acute gastroenteritis in corum. Flora 2017, 22, 58–66. [Google Scholar] [CrossRef]
- Iraz, M.; Ceylan, A. Frequency of rotavirus in children with acute gastroenteritis between 0–5 years of age. Ankem Derg. 2013, 27, 2–6. [Google Scholar] [CrossRef]
- İlktaç, M.; Şahin, A.; Nazik, H.; Ongen, B. Investigation of rotavirus frequency and following up the rotavirus season among children with acute gastroenteritis: Evaluation of five-year results. Ankem Derg. 2012, 26, 25–29. [Google Scholar] [CrossRef]
- Kaşifoğlu, N.; Us, T.; Aslan, F.G.; Akgün, Y. The rate of rotavirus antigen positivity during 2005–2011. Türk Mikrobiyol. Cem. Derg. 2011, 41, 111–115. [Google Scholar]
- Kurugol, Z.; Geylani, S.; Karaca, Y.; Umay, F.; Erensoy, S.; Vardar, F.; Ozkinay, C. Rotavirus gastroenteritis among children under five years of age in Izmir, Turkey. Turk. J. Pediatr. 2003, 45, 290–294. [Google Scholar] [PubMed]
- Otağ, F.; Direkel, Ş.; Özgür, D.; Delialioğlu, N.; Aslan, G.; Emekdaş, G. Investigation of rotavirus and enteric adenovirus in pediatric patients with acute gastroenteritis by rapid immunochromatographic methods. Mersin Univ. Saglık. Bilim. Derg. 2012, 11, 18–23. [Google Scholar]
- Özdemir, S.; Delialioğlu, N.; Emekdaş, G. Investigatıon of rotavirus, adenovirus and astrovirus frequencies in children with acute gastroenteritis and evaluation of epidemiological features. Mikrobiyol. Bull. 2010, 44, 571–578. [Google Scholar]
- Şanal, L. Determination of rotavirus and adenovirus frequency in children with gastroenteritis between 0–5 years of age. Ortadogu Med. J. 2013, 5, 73–77. [Google Scholar]
- Dağı, H.T.; Fındık, D. Investigation of rotavirus and adenovirus antigens in patients with acute gastroenteritis. J. Clin. Exp. Investig. 2014, 5, 256–260. [Google Scholar] [CrossRef]
- Tüzüner, U.; Gülcen, B.S.; Özdemir, M.; Feyzioglu, B. Frequency of adenovirus and rotavirus and their seasonal distribution in children with gastroenteritis. Klimik Derg. 2016, 29, 121–124. [Google Scholar] [CrossRef]
- Yazıcı, V.; Manzur, Y.; Akbulut, A. Investigation of rotavirus and enteric adenovirus infection frequency in cases with acute gastroenteritis. Klimik Derg. 2013, 26, 13–16. [Google Scholar] [CrossRef]
- Alaşehir, E.A.; Balıkcı, A.; Topkaya, A.E. Rotavirus antigen positivity in children with acute gastroenteritis and its relationship with demographic data. Ankem Derg. 2014, 28, 41–43. [Google Scholar] [CrossRef]
- Balkan, Ç.E.; Çelebi, D.; Çelebi, Ö.; Altoparlak, Ü. Investigation of rotavirus and adenovirus frequency among 0–5 years old children with acute gastroenteritis in Erzurum. Türk Mikrobiyol. Cem. Derg. 2012, 42, 51–54. [Google Scholar]
- Bayraktar, B.; Toksoy, B.; Bulut, E. Detection of rotavirus and adenovirus in children with acute gastroenteritis. Klimik Derg. 2010, 23, 15–17. [Google Scholar] [CrossRef]
- Bekdaş, M.; Demircioğlu, F.; Göksügür, S.B.; Küçükbayrak, B.; Kısmet, E. Acute gastroenteritis during childhood in Bolu, Turkey: 3 years of experience. GJMEDPH 2013, 2, 1–7. [Google Scholar]
- Berk, E.; Kayman, T. Frequency of rotavirus in children with acute gastroenteritis. Ankem Derg. 2011, 25, 103–106. [Google Scholar] [CrossRef]
- Ayşe, I. The frequency of rotavirus in children with acute gastroenteritis. J. Clin. Anal. Med. 2015, 6, 449–451. [Google Scholar]
- İnci, A.; Kurtoğlu, M.G.; Baysal, B. Investıgatıon of the prevalence of rotavirus gastroenterıtıs ın an educational and research hospıtal. Turk. J. Infect. 2009, 23, 79–82. [Google Scholar]
- İrvem, A.; Yücel, F.M.; Yıldırım, M.; Kadanalı, A.; Dede, B. Frequency of rotavirus in children with acute gastroenteritis. Türk Mikrobiyol. Cem. Derg. 2014, 44, 98–100. [Google Scholar] [CrossRef]
- Kızılırmak, A.; Çalışkan, E.; Temizkan, R.C. Frequency in children with acute gastroenteritis. Konuralp Tıp Derg. 2017, 9, 35–39. [Google Scholar] [CrossRef]
- Çalgın, M.K.; Çetinkol, Y.; Yıldırım, A.A.; Erdil, A.; Dağlı, A. Investigation of rotavirus and enteric adenovirus frequency among children with acute gastroenteritis in ordu. Ankem Derg. 2015, 29, 59–65. [Google Scholar] [CrossRef]
- Konca, Ç.; Tekin, M.; Akgün, S.; Bülbül, M.; Çoban, M.; Kahramaner, Z.; Turgut, M. Prevalence of rotavirus in children with acute gastroenteritis, seasonal distribution, and laboratory findings in the southeast of Turkey. J. Pediatr. Inf. 2014, 8, 7–11. [Google Scholar] [CrossRef]
- Nazik, S.; Sezer, A.; Duran, İ. Rotavirus and adenovirus incidences in diarrheas existing in the early childhood. Flora 2016, 21, 10–14. [Google Scholar]
- Oğuz, S.; Kurt, F.; Tekin, D.; Kocabas, B.A.; Ince, E.; Suskan, E. Burden of rotavirus gastroenteritis in the pediatric emergency service. J. Pediatr. Inf. 2014, 8, 99–104. [Google Scholar] [CrossRef]
- Şafak, B. The frequency of rotavirus and adenovirus ın pedıatrıc patıents wıth acute gastroenterıtıs. ACU Sağlık Bil. Derg. 2014, 2, 121–124. [Google Scholar]
- Tanrıverdi, Ç.Y.; Yılmaz, G.; Birinci, A. Investigation of the frequency of rotavirus and adenovirus in acute gastroenteritis cases. Pamukkale Tıp Derg. 2017, 1, 61–65. [Google Scholar] [CrossRef]
- Tekin, A. The frequency of rotavirus and enteric adenovirus in children with acute gastroenteritis in Mardin. J. Clin. Exp. Investig. 2010, 1, 43–45. [Google Scholar] [CrossRef]
- Gönüllü, E.; Soysal, A.; Yıldız, İ.; Karaböcüoğlu, M. Impact of self-financed rotavirus vaccination on acute gastroenteritis in young children in Turkey. Hum. Vaccinesand Immunother. 2020, 1–7. [Google Scholar] [CrossRef]
- Malek, M.A.; Teleb, N.; Abu, R.E.; Riddle, M.S.; Sherif, M.E.; Steele, A.D.; Bresee, J.S. The epidemiology of rotavirus diarrhea in countries in the Eastern Mediterranean Region. J. Infect. Dis. 2010, 202, 12–22. [Google Scholar] [CrossRef]
- Loharikar, A.; Dumolard, L.; Chu, S.; Hyde, T.; Goodman, T.; Mantel, C. Status of new vaccine introduction worldwide, september 2016. Morb. Mortal. Wkly. Rep. 2016, 65, 1136–1140. [Google Scholar] [CrossRef]
- Bányai, K.; Estes, M.K.; Martella, V. Parashar UD. Viral gastroenteritis. Lancet 2018, 392, 175–186. [Google Scholar] [CrossRef]
- Khoury, H.; Ogilvie, I.; El Khoury, A.C.; Duan, Y.; Goetghebeur, M.M. Burden of rotavirus gastroenteritis in the Middle Eastern and North African pediatric population. BMC Infect. Dis. 2011, 11, 9. [Google Scholar] [CrossRef]
- Procop, G.W. Gastrointestinal infections. Infect. Dis. Clin. N. Am. 2001, 15, 1073–1108. [Google Scholar] [CrossRef]
- Tapisiz, A.; Demirdag, B.T.; Cura, B.C.Y.; Gunes, C.; Ugraş, A.D.; Tezer, H.; Ozkan, S. Rotavirus infections in children in Turkey: A systematic review. Rev. Med. Virol. 2019, 291, e2020. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics; Subcommittee on Acute Gastroenteritis. Practice parameter: The management of acute gastroenteritis in young children. Paediatrics 1996, 97, 424–435. [Google Scholar]
- Amini, S.; Solati, A.A.; Fayaz, A.; Mahmoodi, M. Rotavirus infection in children with acute diarrhoea in Tehran. Med. J. Islam Repub. Iran 1990, 4, 25–28. [Google Scholar] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).