Association of Place of Residence and Under-Five Mortality in Middle- and Low-Income Countries: A Meta-Analysis
Abstract
1. Introduction
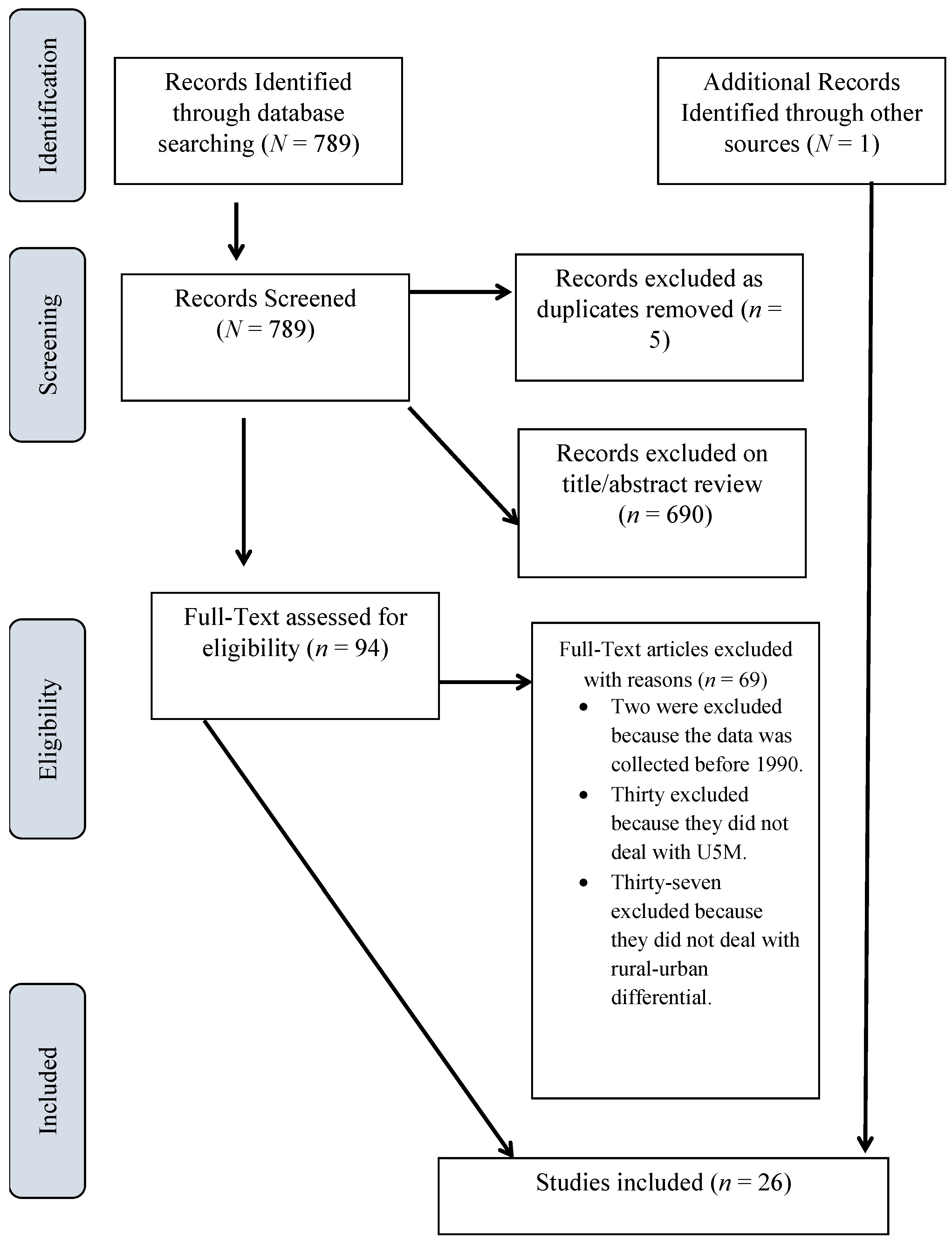
2. Materials and Methods
Ethical Considerations
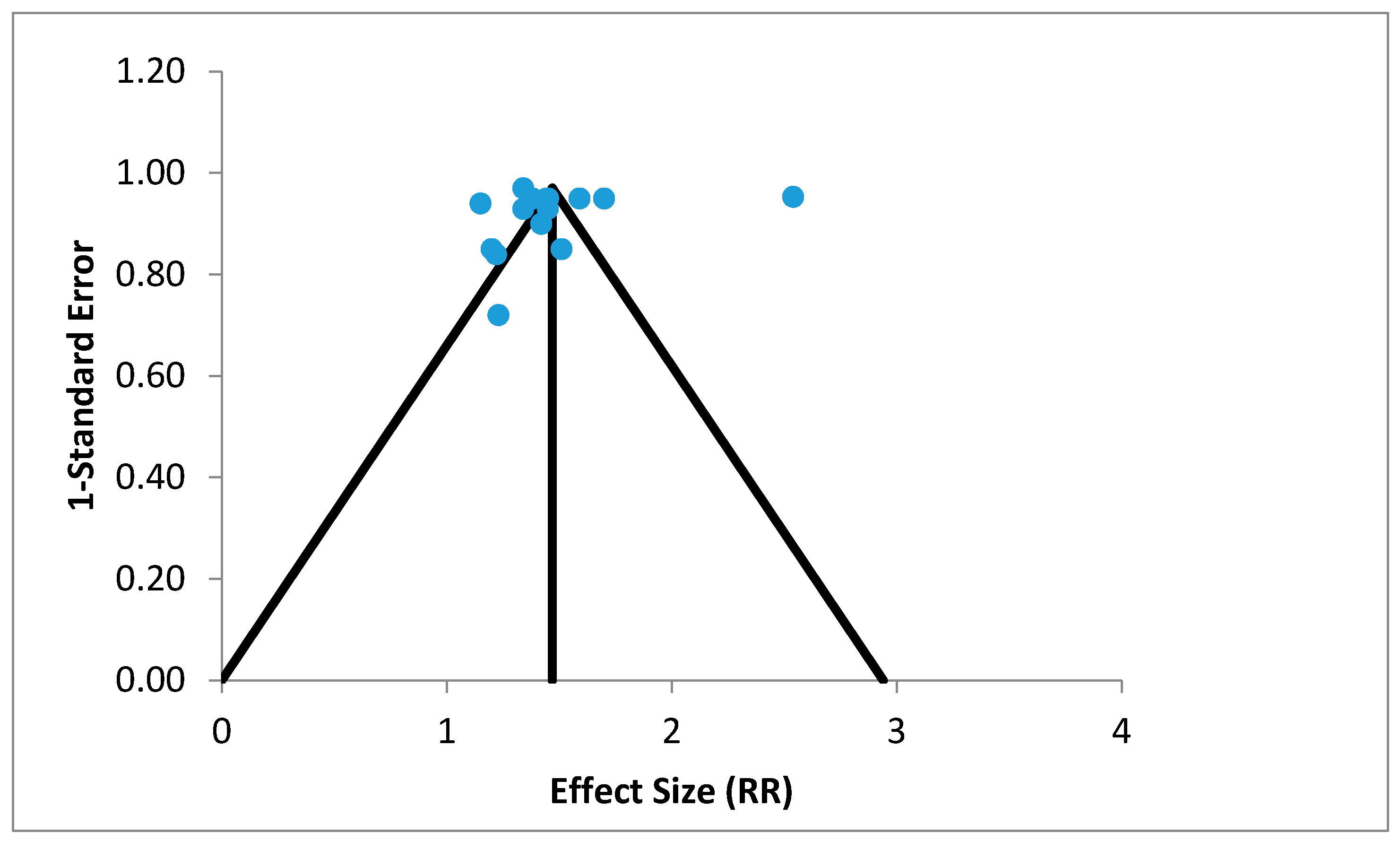
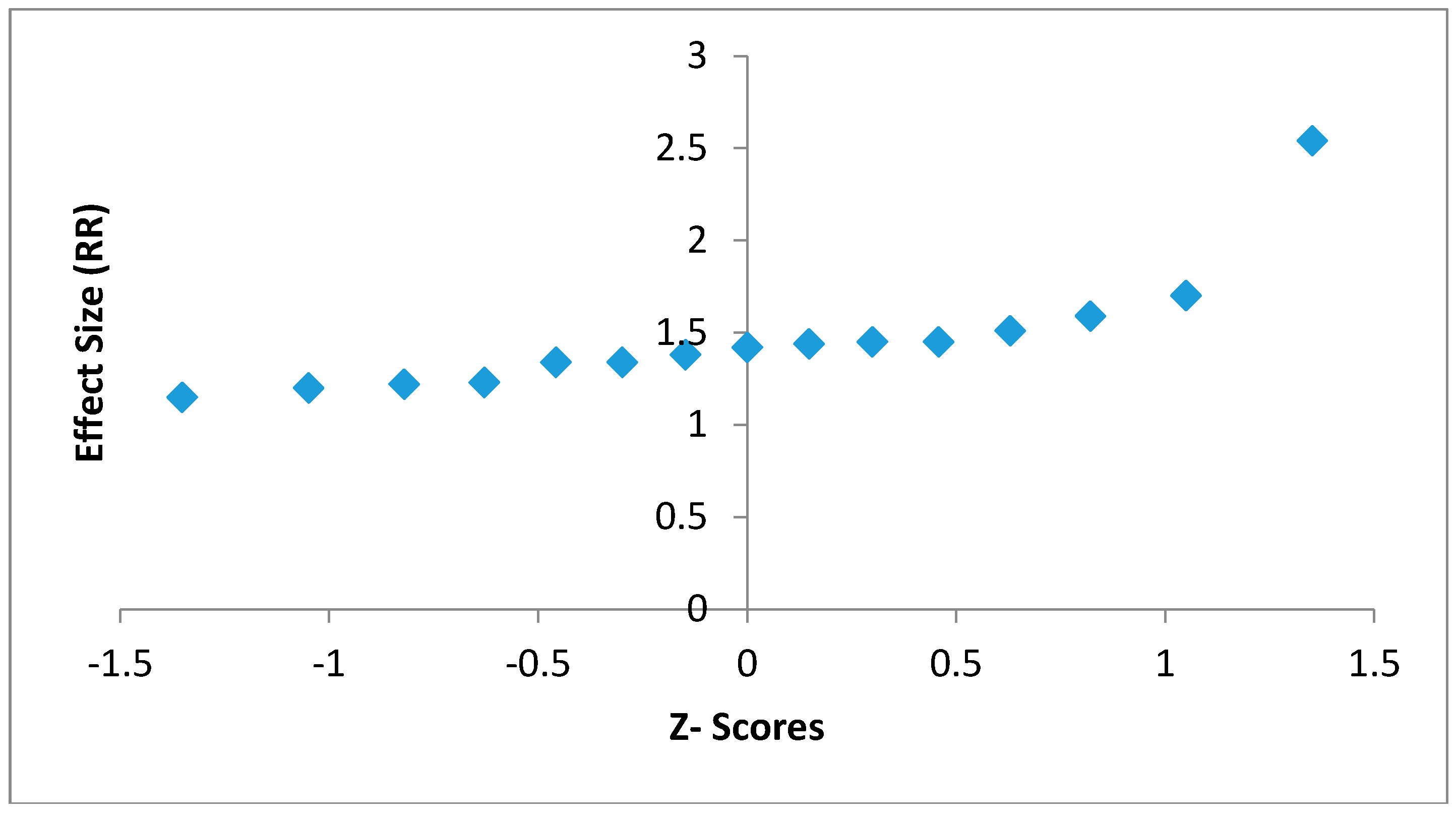
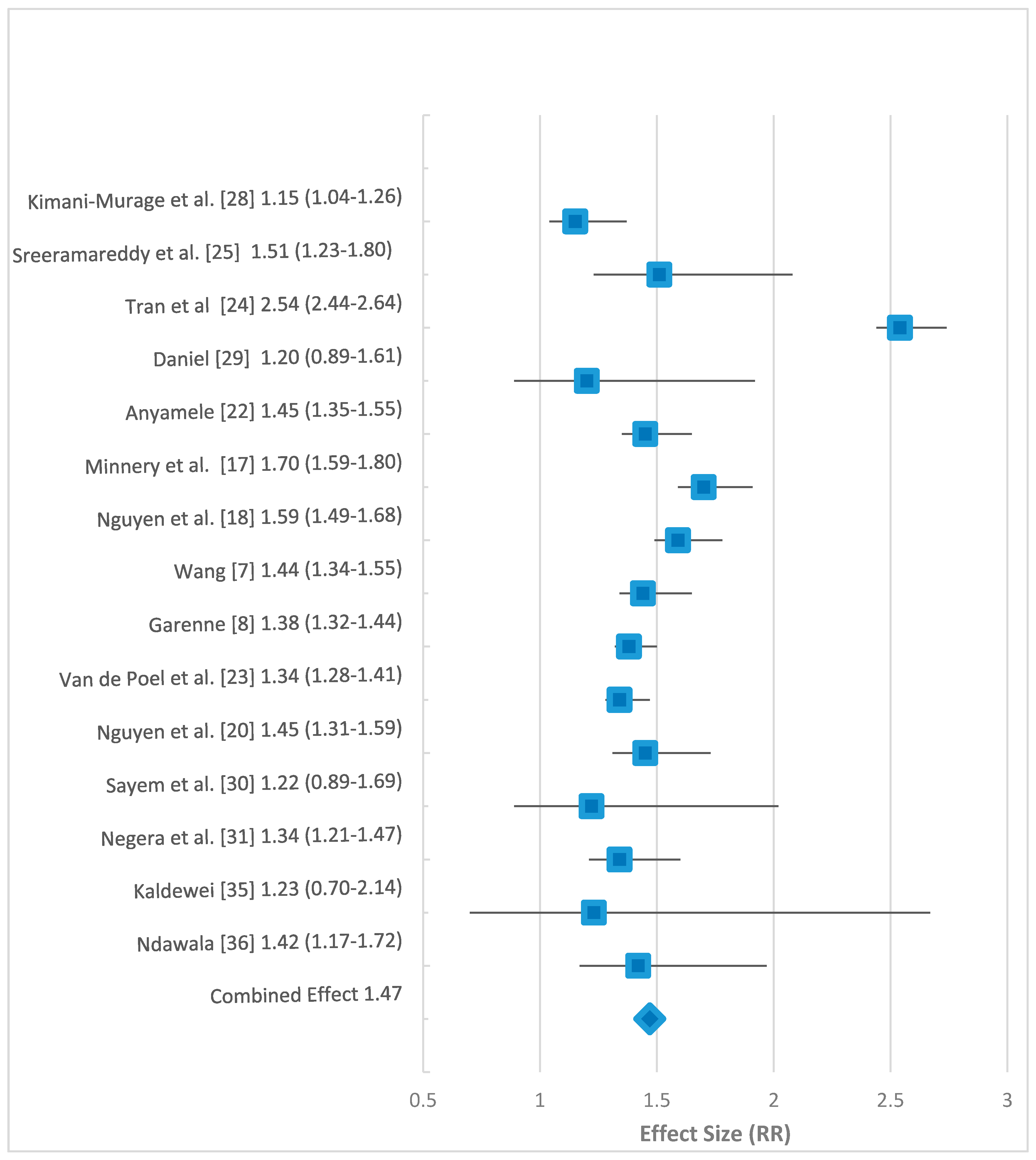
3. Results
4. Discussion
5. Limitations
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. Global Health Observatory (GHO) Data. 2015. Available online: http://www.who.int/gho/child_health/mortality/mortality_under_five_text/en/ (accessed on 20 November 2015).
- UNICEF; WHO; World Bank; UN DESA/Population Division. Levels and Trends in Child Mortality 2015; UNICEF: Hong Kong, China, 2015. [Google Scholar]
- United Nations. Sustainable Development Goals, 17 Goals to Transform Our World. 2015. Available online: http://www.un.org/sustainabledevelopment/sustainable-development-goals/ (accessed on 11 August 2017).
- Houweling, T.J.; Kunst, A.E.; Looman, C.N.; Mackenbach, J.P. Determinants of under-5 mortality among the poor and the rich: A cross-national analysis of 43 developing countries. Int. J. Epidemiol. 2005, 34, 1257–1265. [Google Scholar] [CrossRef] [PubMed]
- Deribew, A.; Tessema, F.; Girma, B. Determinants of under-five mortality in Gilgel Gibe Field Research Center, Southwest Ethiopia. Ethiop. J. Health Dev. 2007, 21, 117–124. [Google Scholar] [CrossRef]
- Shamebo, D.; Muhe, L.; Sandström, A.; Wall, S. The Butajira rural health project in Ethiopia: Mortality pattern of the under fives. J. Trop. Pediatr. 1991, 37, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Wang, L. Health Outcomes in Low-Income Countries and Policy Implications: Empirical Findings from Demographic and Health Surveys; Worldbank Environment Department: Washington, DC, USA, 2002. [Google Scholar]
- Garenne, M. Migration, Urbanisation and Child Health in Africa: A Global Perspective. In Proceedings of the Conference on African Migration in Comparative Perspective, Johannesburg, South Africa, 4–7 June 2003. [Google Scholar]
- Dettrick, Z.; Jimenez-Soto, E.; Hodge, A. Socioeconomic and Geographical Disparities in Under-Five and Neonatal Mortality in Uttar Pradesh, India. Matern. Child Health J. 2014, 18, 960–969. [Google Scholar] [CrossRef] [PubMed]
- Hartling, L.; Featherstone, R.; Nuspi, M.; Shave, K.; Dryden, D.M.; Vandermeer, B. Grey literature in systematic reviews: A cross-sectional study of the contribution of non-English reports, unpublished studies and dissertations to the results of meta-analyses in child-relevant reviews. BMC Med. Res. Methodol. 2017, 17, 64. [Google Scholar] [CrossRef] [PubMed]
- MedCalc Easy-to-Use Statistical Software. Available online: https://www.medcalc.org/calc/relative_risk.php (accessed on 21 November 2015).
- Neyeloff, J.L.; Fuchs, S.C.; Moreira, L.B. Meta-analyses and Forest plots using a microsoft excel spreadsheet: Step-by-step guide focusing on descriptive data analysis. BMC Res. Notes 2012, 5, 52. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- StatsToDo. StatsToDo Meta-Regression Explained. Available online: https://www.statstodo.com/MetaRegression.php (accessed on 21 November 2015).
- World Bank. Rural Population (% of Total Population). 2015. Available online: http://data.worldbank.org/indicator/SP.RUR.TOTL.ZS (accessed on 24 November 2015).
- Khawaja, M.; Dawns, J.; Meyerson-Knox, S.; Yamout, R. Disparities in child health in the Arab region during the 1990s. Int. J. Equity Health 2008, 7, 24. [Google Scholar] [CrossRef] [PubMed]
- Minnery, M.; Jimenez-Soto, E.; Firth, S.; Nguyen, K.; Hodge, A. Disparities in child mortality trends in two new states of India. BMC Public Health 2013, 13, 779. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, K.; Jimenez-Soto, E.; Morgan, A.; Morgan, C.; Hodge, A. How does progress towards the MDG 4 affect inequalities between different subpopulations? Evidence from Nepal. J. Epidemiol. Community Health 2013, 4, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Kayode, G.A.; Adekanmbi, V.T.; Uthman, O.A. Risk factors and a predictive model for under-five mortality in Nigeria: Evidence from Nigeria demographic and health survey. BMC Pregnancy Childbirth 2012, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, K.; Jimenez-Soto, E.; Dayal, P.; Hodge, A. Disparities in child mortality trends: What is the evidence from disadvantaged states in India? The case of Orissa and Madhya Pradesh. Int. J. Equity Health 2013, 12, 45. [Google Scholar] [CrossRef] [PubMed]
- Kazembe, L.; Clarke, A.; Kandala, N. Childhood mortality in sub-Saharan Africa: Cross-sectional insight into small-scale geographical inequalities from Census data. BMJ Open 2012, 2, e001421. [Google Scholar] [CrossRef] [PubMed]
- Anyamele, O.D. Urban and Rural Differences across Countries in Child Mortality in Sub-Saharan Africa. J. Health Care Poor Underserv. 2009, 20, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Van de Poel, E.; O’Donnell, O.; Van Doorslaer, E. Are Urban Children Really Healthier? Evidence from 47 Developing Countries; Tinbergen Institute: Amsterdam, The Netherlands, 2007. [Google Scholar]
- Tran, L.N.; Bauze, A.; Nguyen, K.H.; Jimenez-Soto, E. Under-Five Mortality Analysis for Papua New Guinea; Investment Case MDGs 4 & 5; The University of Queensland School of Population Health: Brisbane, Australia, 2011. [Google Scholar]
- Sreeramareddy, C.T.; Harsha Kumar, H.N.; Sathian, B. Time trends and inequalities of under-five mortality in Nepal: A secondary data. PLoS ONE 2013, 8, e79818. [Google Scholar]
- Jimenez-Soto, E.; Durham, J.; Hodge, A. Entrenched geographical and socioeconomic disparities in child mortality: Trends in absolute and relative inequalities in cambodia. PLoS ONE 2014, 9, e109044. [Google Scholar] [CrossRef] [PubMed]
- Hodge, A.; Firth, S.; Marthias, T.; Jimenez Soto, E. Location matters: Trends in inequalities in child mortality in Indonesia. Evidence from repeated cross-sectional surveys. PLoS ONE 2014, 9, e103597. [Google Scholar] [CrossRef] [PubMed]
- Kimani-Murage, E.W.; Fotso, J.C.; Egondi, T.; Abuya, B.; Elungata, P.; Ziraba, A.K.; Kabiru, C.W.; Madise, N. Trends in childhood mortality in Kenya: The urban advantage has seemingly been wiped out. Health Place 2014, 29, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Daniel, Y. Classification Trees as a Tool for Decomposing Inequalities in Under-Five Mortality in Ghana M. Ph.D. Thesis, Kwane Nkrumah University of Science and Technology, Kumasi, Ghana, 2014. [Google Scholar]
- Sayem, A.; Taher, A.; Nury, S.; Hossain, D. Achieving the Millennium Development Goal for Under-five Mortality in Bangladesh: Current status and lessons for issues and challenges for further improvements. Health Popul. Nutr. 2011, 29, 92–102. [Google Scholar] [CrossRef]
- Negera, A.; Abelti, G.; Bogale, T.; Gebreselassie, T.; Roger, P. An Analysis of the Trends, Differentials and Key Proximate Determinants of Infant and Under-Five Mortality in Ethiopia; Further Analysis of the 2000, 2005 and 2011 Demographic and Health Surveys Data; DHS Further Analysis Reports No. 79; ICF International: Calverton, MD, USA, 2013. [Google Scholar]
- Amouzou, A. Child mortality and Socioeconomic Status in Sub-Saharan Africa. Etude Popul. Afr. 2004, 19, 1–12. [Google Scholar]
- Van Malderen, C.; Van Oyen, H.; Speybroeck, N. Contributing determinants of overall and wealth-related inequality in under-5 mortaltiy in 13 African countries. J. Epidemiol. Community Health 2013, 667–676. [Google Scholar]
- Ettarh, R.R.; Kimani, J. Determinants of under-five mortality in rural and urban Kenya. Rural Remote Health 2012, 12, 1812. [Google Scholar] [PubMed]
- Kaldewei, C. Determinants of Infant and Under-Five Mortality—The Case of Jordan; Technical Note; UN-DESA: New York, NY, USA, 2010. [Google Scholar]
- Ndawala, J. Infant and Child Mortality; National Statistics Office (Malawi); Malawi Demographic and Health Survey: Zomba, Malawi; ORC Macro: Calverton, MD, USA, 2001; pp. 97–104.
- Adedini, S.; Odimegwu, C.; Bamiwuye, O.; Fadeyibi, O.; Wet, N.D. Barriers to accessing health care in Nigeria: Implications for child survival. Glob. Health Action 2014, 7, 23499. [Google Scholar] [CrossRef] [PubMed]
- Dejene, T.; Girma, E. Social determinants of under-five mortality in Ethiopia: Event history analysis using evidence from Ethiopia Demographic and Health Survey. Health 2013, 5, 879–884. [Google Scholar] [CrossRef]
- Corker, J. Urban Advantage or Urban Penalty? Under-5 Mortality and Urbanization in Sub-Saharan Africa; University of Pennsylvania: Philadelphia, PA, USA, 2012. [Google Scholar]
- Sastry, N. Urbanization, development and under-five mortality differentials by place of residence in São Paulo, Brazil, 1970–1991. Demograh. Res. 2004, 2, 355–386. [Google Scholar] [CrossRef]
- Van Enst, W.A.; Ochodo, E.; Scholten, R.J.; Hooft, L.; Leeflang, M.M. Investigation of publication bias in meta-analyses of diagnostic test accuracy: A meta-epidemiological study. BMC Med. Res. Methodol. 2014, 14, 70. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, M.E.; Mulholland, K.; Hill, P.C. How access to health care relates to under-five mortality in sub-Saharan Africa: Systematic review. Trop. Med. Int. Health 2010, 15, 508–519. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Number of Studies |
|---|---|
| Regions | |
| Africa | 1 |
| Sub-Saharan Africa | 14 |
| South Asia | 5 |
| Southeast Asia | 2 |
| Middle East | 2 |
| Global (low income/developing countries) | 1 |
| Southwestern Pacific | 1 |
| Place of Residence | |
| Both urban and rural | 26 |
| Source of Data | |
| Demographic health survey (DHS) | 16 |
| Census | 1 |
| Others | 2 |
| Combination of Surveys | 7 |
| Study | Country/Region | Measure | Source of Data | Study Period (years) | Results | Rural Population (%) | Notes |
|---|---|---|---|---|---|---|---|
| Khawaja et al. [16] | 18 Middle eastern countries | Rural deaths/100 urban | DHS 1990–1998 | 1990–1999 | 112–231 | 29 | Urban advantage observed. |
| Minnery et al. [17] | India | U5M | NFHS (National Family Health Survey) 1992–1993, 1998–1999, 2005–2006 DLHS (District Level Household and Facility Surveys 1998–1999, 2002–2004, 2007–2008 SRS (Sample Registration System 1971–2008 | 1990–2007 | R 81–144 U 50–78 | 72 | Study on two states in India, Chattisgarh and Jharkhand. Notes disparities between urban and rural place of residence and U5M at district level. Notes lower progress in reduction of U5M in urban areas. |
| Nguyen et al. [18] | Nepal | RR RD | NDHS (Nepal Demographic Health Survey) 1996, 2001, 2006 NLSS I (Nepal Living Standards Survey) 1995–1996, NLSS II 2003–2004 | 1990–2005 | 1.27–1.58 13.8–40.4 | 72 | Inequities in rural/urban location. Urban children have a better chance of survival than those born in rural areas. |
| Wang [7] | 60 Low income countries | U5M | DHS 1990–99, WDI (World Development Indicators) | 1990–1999 | R 34–347 U 34–210 | 56 | Gap in U5M in rural and urban areas. The assumption is that most poor live in rural areas. Rural areas have slower reduction in U5M than urban areas. Overall, in rural areas, U5M has reduced from 143 in 1990 to 126 in 1999. In urban areas, U5M has reduced from 105 in 1990 to 89 in 1999. |
| Garenne [8] | 31 African countries | RR | 47 DHS and WFS (World Fertility Survey) | 1950–2000 | 0.94–2.03 | 72 | Reported no change in status in 19 countries; convergence in 11 countries; and divergence in 1 country in the association of U5M and rural and urban areas of residence. |
| Kayode et al. [19] | Nigeria | OR | Nigeria DHS 2008 | 2003–2008 | R 1.53 U 1.00 | 51 | Living in urban areas reduced the odds of U5M. |
| Nguyen et al. [20] | India | U5M | NFHS 1992–1993, 1998–1999, 2005–2006, DLHS 1998–1999, 2002–2004, 2007–2008, SRS 1971–2008, WHS (World Health Survey) 2003 | 1990–2007 | MadhyaPradesh R 104–178 U 67–97 Orissa R 92–150 U 68–98 | 88 | Data on two states, Madhya Pradesh and Orissa. Convergence between rural and Urban U5M rates; attribute to largely inadequate progress in urban areas. |
| Kazembe et al. [21] | Rwanda, Senegal and Uganda | HR BV(MV) | Census data 2001 (Rwanda) 2002 (Senegal, Uganda) | 2001–2002 | Rwanda U 0.67 (MV 0.79) Senegal 0.63 (MV 1.01) Uganda 0.68 (MV 1.04) | 77 | Three sub-Saharan countries. Lower deaths associated with living in urban areas. |
| Anyamele. [22] | 11 Sub-Saharan African countries | RR | DHS 2003–2007 | 2000–2006 | 1.16–1.66 | 71 | Those born in Urban areas have better odds of survival past their fifth birthday than those in rural areas. Calculated the ratio of rural to urban areas and U5M. Report a wide difference. |
| Van de Poel et al. [23] | 47 Developing Countries | RR | DHS 1994–2004 | 1989–2003 | 0.72–1.80 | 62 | Considerable rural–urban gap in child health outcomes. Higher U5M in rural areas. In a number of countries urban poor has higher mortality than rural counterparts. Controlling for wealth, the rural urban gap remains significant in 17 countries. |
| Tran et al. [24] | Papua New Guinea | U5M | DHS 1996, 2006 National Census 2000 | 1985–1999 | R 83–92 U 32–38 | 86 | Lower U5M in urban areas. National estimates closer to rural estimates. Estimates at provincial and district level. Reduction in U5M lower in rural areas. Poverty a significant indicator. |
| Sreeramareddy et al. [25] | Nepal | U5M | DHS 1996, 2001, 2006, 2011 | 1991–2010 | R decreased from 123 to 56. U decreased from 73 to 44. | 86 | Relative and absolute inequalities for U5M reduced for rural/urban. Decrease higher in rural areas. |
| Jimenez-Soto et al. [26] | Cambodia | Rr and RD Base = Urban | DHS 2000, 2005, 2010 | 1995–2010 | Rr increased from 1.56 in 1989–90 to 2.41 in 2009–2010. RD 31–46 | 79 | U5M decreasing however inequalities increasing. Rural disadvantage observed. |
| Hodge et al. [27] | Indonesia | Rr and RD Base = Urban | 7 IDHS 1980–2011 (1987, 1991, 1994, 1997, 2002–03, 2007–2008, 2012 | 1980–2011 | Rr 1.24–1.75 RD 15.5–40.3 | 46 | Decline in national U5M and decline in absolute inequality in rural/urban location. Rural population migrating into urban slums may have caused closing gap. |
| Kimani-Murage et al. [28] | Kenya | U5M | KDHS (Kenya DHS) 1993, 1998, 2003, 2008, NUHDSS (Nairobi Urban Health and Demographic Surveillance System) 2003–2010 | 1979–2008 | R 73–105 U 69–100 | 82 | Disparities narrowing because of more rapid decline in U5M in rural than urban areas. But they report higher U5M in urban slums than in rural and non-slum urban areas. |
| Daniel [29] | Ghana | U5M | Ghana DHS 2008 | 2003–2007 | R 90 U 75 | 51 | U5M rates were consistently higher in rural areas. 62.5% greater chance of dying in rural areas compared to urban areas. |
| Sayem et al. [30] | Bangladesh | U5M | Bangladesh DHS 2007 | 2007 | U 63 R 77 | 72 | U5M decline is faster in urban than in rural areas. Rural poor are more vulnerable population that needs more attention. |
| Negera et al. [31] | Ethiopia | U5M | DHS 2000, 2005, 2011 | 1995–2011 | U 149 to 83 R 193 to 114 | 84 | U5M higher in rural areas for the 3 survey periods under study. |
| Amouzou [32] | Sub-Saharan Africa | U5M | DHS | 1960–2000 | % Urban Bivariate model −0.02 Main effects model −0.01 Extended model −0.01 | 71 | Negative association between urbanization and U5MR observed. |
| Van Malderen et al. [33] | Africa | Percentage Under-five deaths | DHS 2007–2010 | 2002–2007 | U 2.7–11.9 R 2.4–12.5 | 60 | 13 African countries. U5M higher in rural areas. Focus on wealth related inequalities. |
| Ettarh and Kimani. [34] | Kenya | Multivariate HR | DHS 2008–2009 | 2003–2009 | 3.61 R compared with U R 1040/13149 U 167/3013 | 82 | Likelihood of death in rural areas significantly higher than in the urban areas. |
| Kaldewei [35] | Jordan | U5M | JPFHS (Jordan Population and Family Health Survey) 2007 | 2002–2006 | R 27 U 22 | 18 | Urban advantage persists even though the rural population is only 16.5% in the survey. Overall, MDG4 targets to be achieved. |
| Ndawala [36] | Malawi | U5M | DHS 2000 | 1991–2000 | 10-year estimates U 147.9 per 1000 R 210.4 per 1000 | 85 | Rural mortality rates higher than urban. The rural-urban differential larger in the neonatal period than the postneonatal period. |
| Adedini et al. [37] | Nigeria | HR | DHS 2008 | 2003–2008 | Rural = Model 5 1.22 (1.07 1.38), Model 6 1.21 (1.07 1.37) Model 7 1.23 (1.08 1.39) Model 8 1.21 (1.08 1.37) For all urban =1 | 51 | All models were significant and indicated a rural disadvantage for children under-five. |
| Dejene and Girma [38] | Ethiopia | HR | DHS 2011 | 2001–2010 | Unadjusted U 1 R 1.4 (1.24, 1.58) Adjusted U 1 R 1.02 (0.86, 1.21) | 80 | Urban advantage however gap narrowing. |
| Corker [39] | 12 Sub-Saharan African countries | Kaplan-Meier Survival Estimates | DHS 1995–2000, 2005–2010 | 1990–2010 | Change in AD-0.006% U-R R 1.045 in 1995–2000 To R 1.037 in 2005–2010 | 64 | 12 Sub-Saharan countries, the urban advantage remains but decreases slightly. Urbanisation poses new threat. Higher gains in rural areas led to decrease in inequalities in U5M. |
| Variable | β | 95% CI for β | Standard Error | p-value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Constant | 0.988 | 0.038 | 1.94 | 0.485 | 0.041 |
| Rural population (%) | 0.007 | −0.006 | 0.02 | 0.007 | 0.3 |
| Study Omitted | Effect Size (RR) | CI |
|---|---|---|
| Kimani-Murage et al. [28] | 1.50 | 1.29–1.71 |
| Daniel [29] | 1.49 | 1.29–1.70 |
| Van de Poel et al. [23] | 1.48 | 1.26–1.71 |
| Garenne [8] | 1.48 | 1.26–1.70 |
| Wang [7] | 1.48 | 1.26–1.69 |
| Anyamele [22] | 1.48 | 1.26–1.69 |
| Sreeramareddy et al. [25] | 1.47 | 1.26–1.70 |
| Nguyen et al. [18] | 1.47 | 1.25–1.68 |
| Minnery et al. [17] | 1.46 | 1.24–1.67 |
| Tran et al. [24] | 1.41 | 1.33–1.49 |
| Nguyen et al. [20] | 1.48 | 1.26–1.69 |
| Sayem et al. [30] | 1.49 | 1.28–1.70 |
| Negera et al. [31] | 1.48 | 1.27–1.70 |
| Kaldewei [35] | 1.49 | 1.28–1.69 |
| Ndawala [36] | 1.48 | 1.27–1.69 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forde, I.; Tripathi, V. Association of Place of Residence and Under-Five Mortality in Middle- and Low-Income Countries: A Meta-Analysis. Children 2018, 5, 51. https://doi.org/10.3390/children5040051
Forde I, Tripathi V. Association of Place of Residence and Under-Five Mortality in Middle- and Low-Income Countries: A Meta-Analysis. Children. 2018; 5(4):51. https://doi.org/10.3390/children5040051
Chicago/Turabian StyleForde, Ian, and Vrijesh Tripathi. 2018. "Association of Place of Residence and Under-Five Mortality in Middle- and Low-Income Countries: A Meta-Analysis" Children 5, no. 4: 51. https://doi.org/10.3390/children5040051
APA StyleForde, I., & Tripathi, V. (2018). Association of Place of Residence and Under-Five Mortality in Middle- and Low-Income Countries: A Meta-Analysis. Children, 5(4), 51. https://doi.org/10.3390/children5040051





