Hospital-Acquired Hyponatremia in Children Following Hypotonic versus Isotonic Intravenous Fluids Infusion
Abstract
1. Introduction
2. Patients and Methods
2.1. Setting and Study Design
2.2. Definitions and Data Collection
2.3. Statistical Analysis
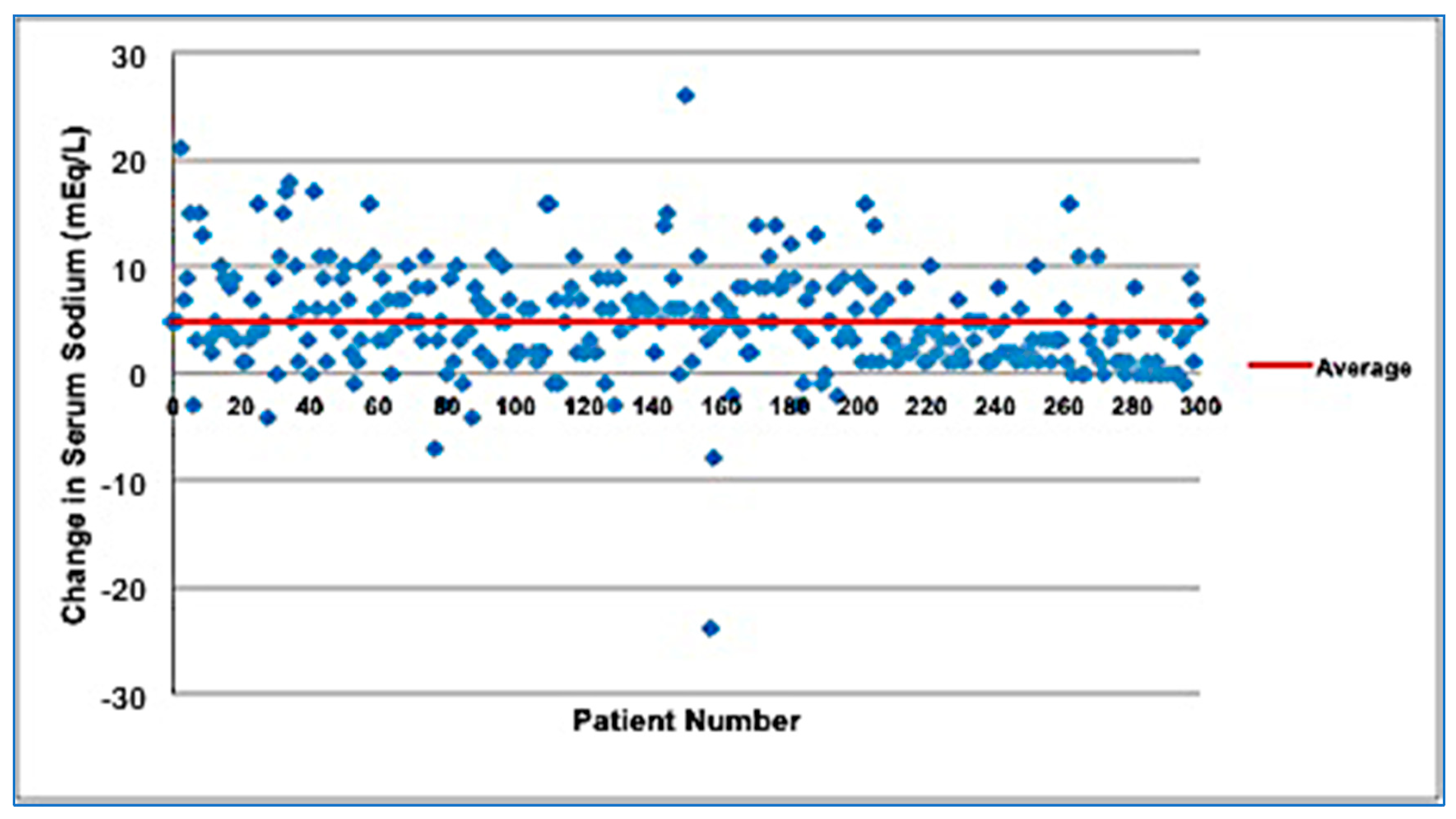
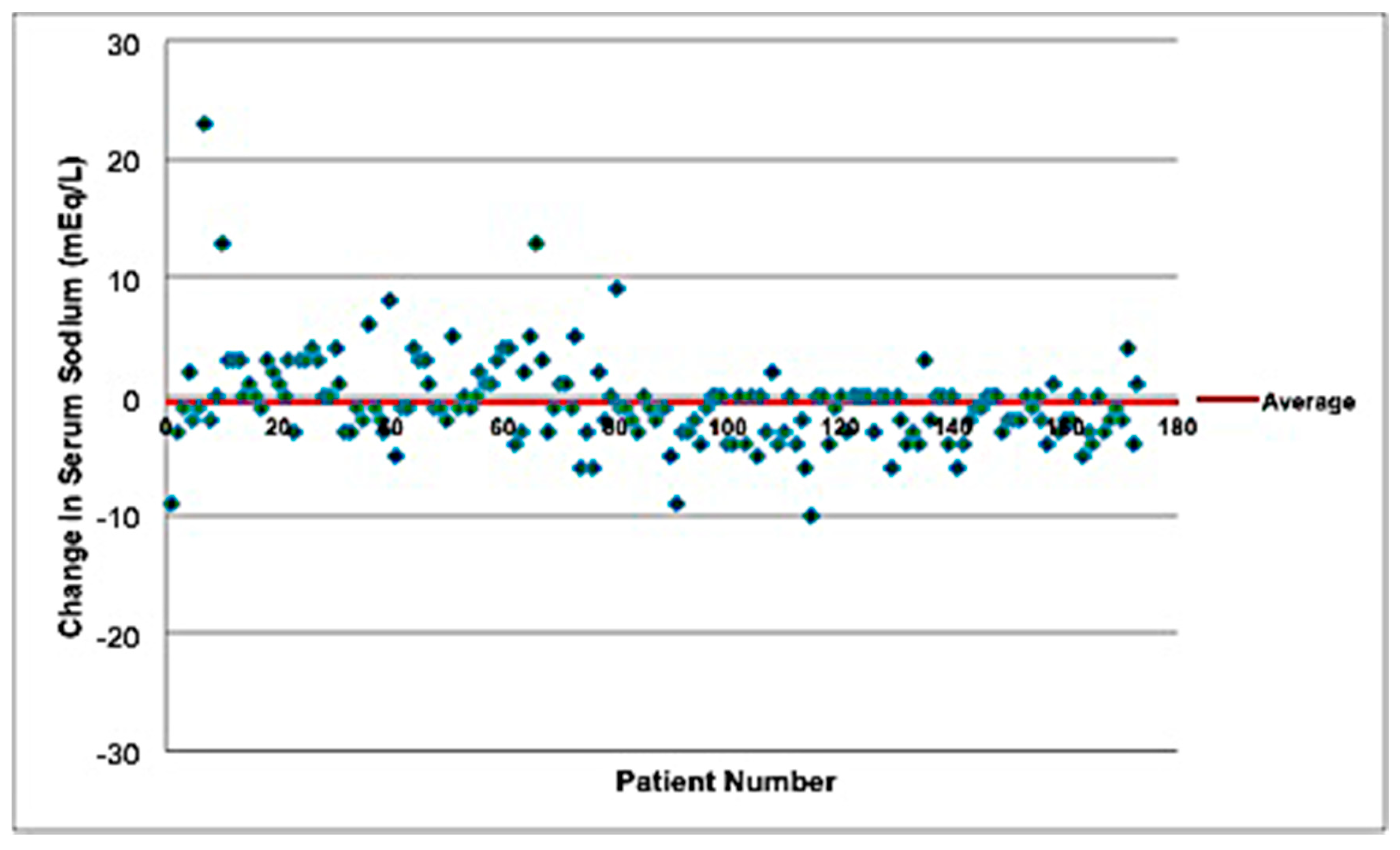
3. Results
3.1. Baseline Characteristics of Included Patients
3.2. Clinical Characteristics and Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Moritz, M.L.; Ayus, J.C. Prevention of hospital-acquired hyponatremia: Do we have the answers? Pediatrics 2011, 128, 980–983. [Google Scholar] [CrossRef] [PubMed]
- Adrogue, H.J.; Madias, N.E. Hyponatremia. N. Engl. J. Med. 2000, 342, 1581–1589. [Google Scholar] [CrossRef] [PubMed]
- Easley, D.; Tillman, E. Hospital-acquired hyponatremia in pediatric patients: A review of the literature. J. Pediatr. Pharmacol. Ther. 2013, 18, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Koczmara, C.; Wade, A.W.; Skippen, P.; Campigotto, M.J.; Streitenberger, K.; Carr, R.; Wong, E.; Robertson, K. Hospital-acquired acute hyponatremia and reports of pediatric deaths. Dynamics 2010, 21, 21–26. [Google Scholar] [PubMed]
- Holliday, M.A.; Segar, W.E. The maintenance need for water in parenteral fluid therapy. Pediatrics 1957, 19, 823–832. [Google Scholar] [CrossRef] [PubMed]
- Carandang, F.; Anglemyer, A.; Longhurst, C.A.; Krishnan, G.; Alexander, S.R.; Kahana, M.; Sutherland, S.M. Association between maintenance fluid tonicity and hospital-acquired hyponatremia. J. Pediatr. 2013, 163, 1646–1651. [Google Scholar] [CrossRef] [PubMed]
- Halberthal, M.; Halperin, M.L.; Bohn, D. Lesson of the week: Acute hyponatraemia in children admitted to hospital: Retrospective analysis of factors contributing to its development and resolution. BMJ 2001, 322, 780–782. [Google Scholar] [CrossRef] [PubMed]
- Moritz, M.L.; Ayus, J.C. Prevention of hospital-acquired hyponatremia: A case for using isotonic saline. Pediatrics 2003, 111, 227–230. [Google Scholar] [CrossRef] [PubMed]
- McNab, S.; Ware, R.S.; Neville, K.A.; Choong, K.; Coulthard, M.G.; Duke, T.; Davidson, A.; Dorofaeff, T. Isotonic versus hypotonic solutions for maintenance intravenous fluid administration in children. Cochrane Database Syst. Rev. 2014, 18, CD009457. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Lava, S.A.; Bianchetti, M.G.; Milani, G.P. Testing Na+ in blood. Clin. Kidney J. 2017, 10, 147–148. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Armon, K.; Riordan, A.; Playfor, S.; Millman, G.; Khader, A.; Paediatric Research, S. Hyponatraemia and hypokalaemia during intravenous fluid administration. Arch. Dis. Child. 2008, 93, 285–287. [Google Scholar] [CrossRef] [PubMed]
- Choong, K.; Arora, S.; Cheng, J.; Farrokhyar, F.; Reddy, D.; Thabane, L.; Walton, J.M. Hypotonic versus isotonic maintenance fluids after surgery for children: A randomized controlled trial. Pediatrics 2011, 128, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Kannan, L.; Lodha, R.; Vivekanandhan, S.; Bagga, A.; Kabra, S.K.; Kabra, M. Intravenous fluid regimen and hyponatraemia among children: A randomized controlled trial. Pediatr. Nephrol. 2010, 25, 2303–2309. [Google Scholar] [CrossRef] [PubMed]
- Rey, C.; Los-Arcos, M.; Hernandez, A.; Sanchez, A.; Diaz, J.J.; Lopez-Herce, J. Hypotonic versus isotonic maintenance fluids in critically ill children: A multicenter prospective randomized study. Acta Paediatr. 2011, 100, 1138–1143. [Google Scholar] [CrossRef] [PubMed]
- McNab, S.; Duke, T.; South, M.; Babl, F.E.; Lee, K.J.; Arnup, S.J.; Young, S.; Turner, H.; Davidson, A. 140 mmol/L of sodium versus 77 mmol/L of sodium in maintenance intravenous fluid therapy for children in hospital (PIMS): A randomised controlled double-blind trial. Lancet 2015, 385, 1190–1197. [Google Scholar] [CrossRef]
- Wang, J.; Xu, E.; Xiao, Y. Isotonic versus hypotonic maintenance IV fluids in hospitalized children: A meta-analysis. Pediatrics 2014, 133, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Foster, B.A.; Tom, D.; Hill, V. Hypotonic versus isotonic fluids in hospitalized children: A systematic review and meta-analysis. J. Pediatr. 2014, 165, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Decaux, G.; Musch, W.; Penninckx, R.; Soupart, A. Low plasma bicarbonate level in hyponatremia related to adrenocorticotropin deficiency. J. Clin. Endocrinol. Metab. 2003, 88, 5255–5257. [Google Scholar] [CrossRef] [PubMed]
- Neville, K.A.; Sandeman, D.J.; Rubinstein, A.; Henry, G.M.; McGlynn, M.; Walker, J.L. Prevention of hyponatremia during maintenance intravenous fluid administration: A prospective randomized study of fluid type versus fluid rate. J. Pediatr. 2010, 156, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Yung, M.; Keeley, S. Randomised controlled trial of intravenous maintenance fluids. J. Paediatr. Child. Health 2009, 45, 9–14. [Google Scholar] [CrossRef] [PubMed]
| Effect | p-Value | Odds Ratio * | 95% Confidence Limits | |
|---|---|---|---|---|
| Hypotonic PS | 0.04 | 3.14 | 1.03 | 9.53 |
| Admission CO2 | <0.01 | 1.05 | 1.01 | 1.09 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karageorgos, S.A.; Kratimenos, P.; Landicho, A.; Haratz, J.; Argentine, L.; Jain, A.; McInnes, A.D.; Fisher, M.; Koutroulis, I. Hospital-Acquired Hyponatremia in Children Following Hypotonic versus Isotonic Intravenous Fluids Infusion. Children 2018, 5, 139. https://doi.org/10.3390/children5100139
Karageorgos SA, Kratimenos P, Landicho A, Haratz J, Argentine L, Jain A, McInnes AD, Fisher M, Koutroulis I. Hospital-Acquired Hyponatremia in Children Following Hypotonic versus Isotonic Intravenous Fluids Infusion. Children. 2018; 5(10):139. https://doi.org/10.3390/children5100139
Chicago/Turabian StyleKarageorgos, Spyridon A., Panagiotis Kratimenos, Ashley Landicho, Joshua Haratz, Louis Argentine, Amit Jain, Andrew D. McInnes, Margaret Fisher, and Ioannis Koutroulis. 2018. "Hospital-Acquired Hyponatremia in Children Following Hypotonic versus Isotonic Intravenous Fluids Infusion" Children 5, no. 10: 139. https://doi.org/10.3390/children5100139
APA StyleKarageorgos, S. A., Kratimenos, P., Landicho, A., Haratz, J., Argentine, L., Jain, A., McInnes, A. D., Fisher, M., & Koutroulis, I. (2018). Hospital-Acquired Hyponatremia in Children Following Hypotonic versus Isotonic Intravenous Fluids Infusion. Children, 5(10), 139. https://doi.org/10.3390/children5100139






