Overview of Four Functional Classification Systems Commonly Used in Cerebral Palsy
Abstract
:1. Introduction
2. Classification Measures
2.1. Gross Motor Function Classification System (GMFCS)
2.1.1. Inter-Rater and Test-Retest Reliability
2.2. Manual Ability Classification System (MACS)
2.2.1. Intra-Class Correlation
2.2.2. Inter-Observer Reliability
2.3. Mini-MACS
2.4. Communication Function Classification System (CFCS)
2.4.1. Inter-Rater and Test-Retest Reliability
2.5. Eating and Drinking Ability Classification System (EDACS)
2.5.1. Intra-Class Correlation
3. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Gorter, J.W.; Rosenbaum, P.L.; Hanna, S.E.; Palisano, R.J.; Bartlett, D.J.; Russell, D.J.; Walter, S.D.; Raina, P.; Galuppi, B.E.; Wood, E. Limb distribution, motor impairment, and functional classification of cerebral palsy. Dev. Med. Child Neurol. 2004, 46, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Bax, M.; Goldstein, M.; Rosenbaum, P.; Leviton, A.; Paneth, N.; Dan, B.; Jacobsson, B.; Damiano, D. Executive Committee for the Definition of Cerebral, P. Proposed definition and classification of cerebral palsy, April 2005. Dev. Med. Child Neurol. 2005, 47, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Gormley, M.E., Jr. Treatment of neuromuscular and musculoskeletal problems in cerebral palsy. Pediatr. Rehabil. 2001, 4, 5–16. [Google Scholar] [PubMed]
- Graham, H.K. Classifying cerebral palsy. J. Pediatr. Orthop. 2005, 25, 127–128. [Google Scholar]
- Stanley, F.J.; Blair, E.; Alberman, E. Cerebral Palsies: Epidemiology and Causal Pathways; Cambridge University Press: Cambridge, UK, 2000. [Google Scholar]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.L.; Palisano, R.J.; Bartlett, D.J.; Galuppi, B.E.; Russell, D.J. Development of the gross motor function classification system for cerebral palsy. Dev. Med. Child Neurol. 2008, 50, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.; Rosenbaum, P.; Bartlett, D.; Livingston, M. Gmfcs-e&r. Gross motor function classification system expanded and revised. In Canchild Centre for Childhood Disability Research, Mcmaster University; Institute for Applied Health Sciences McMaster University: Hamilton, ON, Canada, 2007; p. b15. [Google Scholar]
- Palisano, R.J.; Rosenbaum, P.; Bartlett, D.; Livingston, M.H. Content validity of the expanded and revised gross motor function classification system. Dev. Med. Child Neurol. 2008, 50, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Bodkin, A.W.; Robinson, C.; Perales, F.P. Reliability and validity of the gross motor function classification system for cerebral palsy. Pediatr. Phys. Ther. 2003, 15, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Wood, E.; Rosenbaum, P. The gross motor function classification system for cerebral palsy: A study of reliability and stability over time. Dev. Med. Child. Neurol. 2000, 42, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.J.; Cameron, D.; Rosenbaum, P.L.; Walter, S.D.; Russell, D. Stability of the gross motor function classification system. Dev. Med. Child Neurol. 2006, 48, 424–428. [Google Scholar] [CrossRef] [PubMed]
- McCormick, A.; Brien, M.; Plourde, J.; Wood, E.; Rosenbaum, P.; McLean, J. Stability of the gross motor function classification system in adults with cerebral palsy. Dev. Med. Child Neurol. 2007, 49, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.; Galuppi, B.E.; Rosenbaum, P.L. Reliability of family report for the gross motor function classification system. Dev. Med. Child Neurol. 2004, 46, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Eliasson, A.C.; Krumlinde-Sundholm, L.; Rosblad, B.; Beckung, E.; Arner, M.; Ohrvall, A.M.; Rosenbaum, P. The manual ability classification system (macs) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev. Med. Child Neurol. 2006, 48, 549–554. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.; Kurinczuk, J.J.; Fitzpatrick, R.; Rosenbaum, P.L. Reliability of the manual ability classification system for children with cerebral palsy. Dev. Med. Child Neurol. 2006, 48, 950–953. [Google Scholar] [CrossRef] [PubMed]
- Ohrvall, A.M.; Krumlinde-Sundholm, L.; Eliasson, A.C. The stability of the manual ability classification system over time. Dev. Med. Child Neurol. 2014, 56, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Plasschaert, V.F.; Ketelaar, M.; Nijnuis, M.G.; Enkelaar, L.; Gorter, J.W. Classification of manual abilities in children with cerebral palsy under 5 years of age: How reliable is the manual ability classification system? Clin. Rehabil. 2009, 23, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Eliasson, A.C.; Ullenhag, A.; Wahlstrom, U.; Krumlinde-Sundholm, L. Mini-macs: Development of the manual ability classification system for children younger than 4 years of age with signs of cerebral palsy. Dev. Med. Child Neurol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Achilles, R.F. Communicative anomalies of individuals with cerebral palsy. Cereb. Palsy Rev. 1955, 16, 15–24. [Google Scholar]
- Andersen, G.; Mjøen, T.R.; Vik, T. Prevalence of speech problems and the use of augmentative and alternative communication in children with cerebral palsy: A registry-based study in Norway. SIG 12 Perspect. Augment. Altern. Commun. 2010, 19, 12–20. [Google Scholar] [CrossRef]
- Hidecker, M.J.; Paneth, N.; Rosenbaum, P.L.; Kent, R.D.; Lillie, J.; Eulenberg, J.B.; Chester, K., Jr.; Johnson, B.; Michalsen, L.; Evatt, M.; et al. Developing and validating the communication function classification system for individuals with cerebral palsy. Dev. Med. Child Neurol. 2011, 53, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Vander Zwart, K.E.; Geytenbeek, J.J.; de Kleijn, M.; Oostrom, K.J.; Gorter, J.W.; Hidecker, M.J.; Vermeulen, R.J. Reliability of the dutch-language version of the communication function classification system and its association with language comprehension and method of communication. Dev. Med. Child Neurol. 2016, 58, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Soleymani, Z.; Joveini, G.; Baghestani, A.R. The communication function classification system: Cultural adaptation, validity, and reliability of the farsi version for patients with cerebral palsy. Pediatr. Neurol. 2015, 52, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Reilly, S.; Skuse, D.; Poblete, X. Prevalence of feeding problems and oral motor dysfunction in children with cerebral palsy: A community survey. J. Pediatr. 1996, 129, 877–882. [Google Scholar] [CrossRef]
- Sellers, D.; Mandy, A.; Pennington, L.; Hankins, M.; Morris, C. Development and reliability of a system to classify the eating and drinking ability of people with cerebral palsy. Dev. Med. Child Neurol. 2014, 56, 245–251. [Google Scholar] [CrossRef] [PubMed]
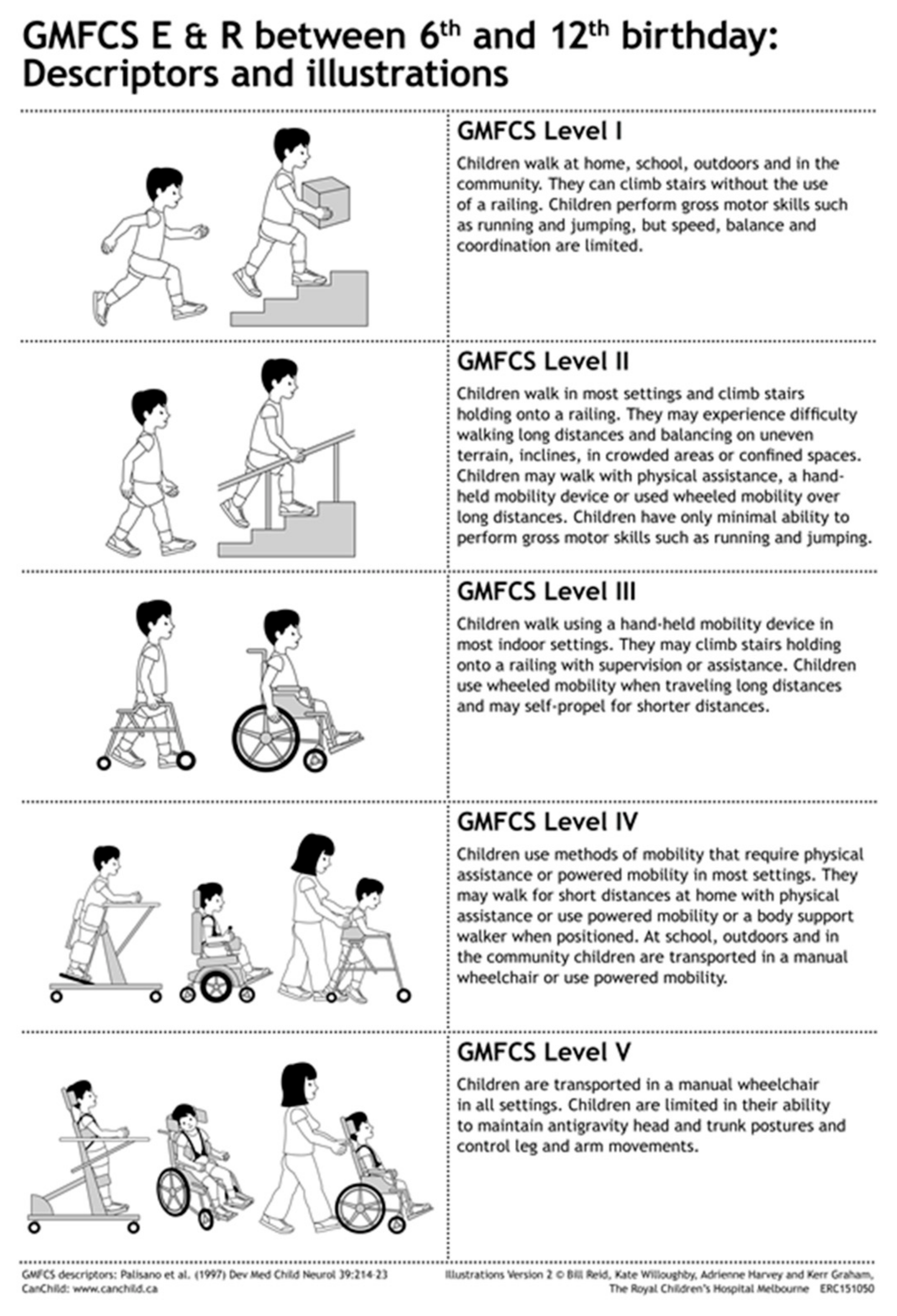
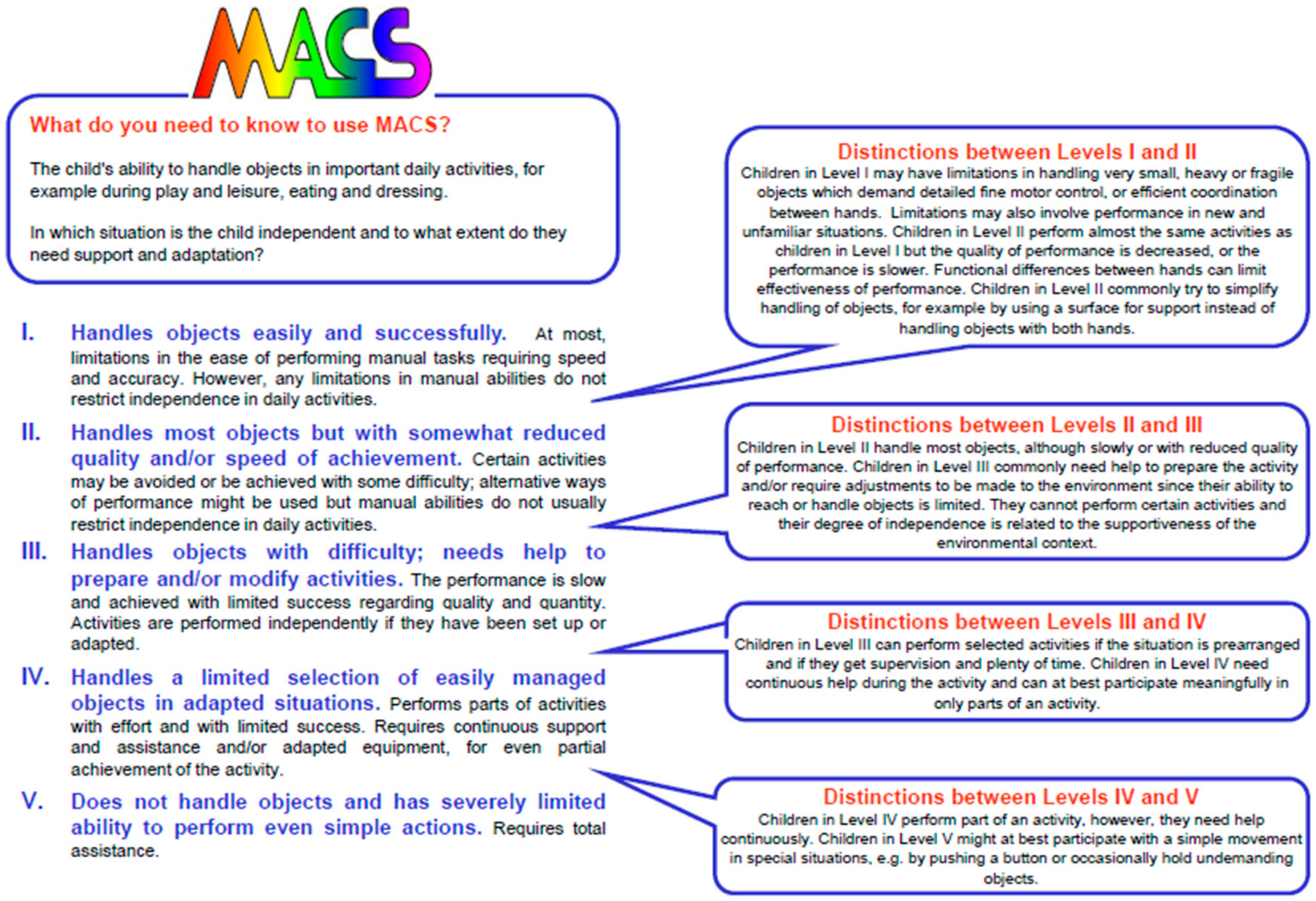
| GMFCS | MACS | CFCS | EDACS | |
|---|---|---|---|---|
| I | Walks without limitation | Handles objects easily and successfully | Effective sender and receiver | Eats and drinks safely and efficiently |
| II | Walks with limitations (no mobility aid by 4yo) | Handles most objects with reduced speed/quality | Effective but slow paced sender and receiver | Eats and drinks safely but with some limitations to efficiency |
| III | Walks with hand-held mobility device | Handles objects with difficulty, help to prepare or modify activity | Effective sender and receiver with familiar partners | Eats and drinks with some limitations to safely; there may also be limitations to efficiency |
| IV | Self-mobility with limitations, may use power | Handles limited number of objects in adapted setting | Inconsistent sender and receiver with familiar partners | Eats and drinks with significant limitations to safety |
| V | Transported in manual wheelchair | Does not handle objects | Seldom effective sender and receiver with familiar partners | Unable to eat or drink safely, consider feeding tube |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paulson, A.; Vargus-Adams, J. Overview of Four Functional Classification Systems Commonly Used in Cerebral Palsy. Children 2017, 4, 30. https://doi.org/10.3390/children4040030
Paulson A, Vargus-Adams J. Overview of Four Functional Classification Systems Commonly Used in Cerebral Palsy. Children. 2017; 4(4):30. https://doi.org/10.3390/children4040030
Chicago/Turabian StylePaulson, Andrea, and Jilda Vargus-Adams. 2017. "Overview of Four Functional Classification Systems Commonly Used in Cerebral Palsy" Children 4, no. 4: 30. https://doi.org/10.3390/children4040030
APA StylePaulson, A., & Vargus-Adams, J. (2017). Overview of Four Functional Classification Systems Commonly Used in Cerebral Palsy. Children, 4(4), 30. https://doi.org/10.3390/children4040030





