Putting Children’s Sleep Problems to Bed: Using Behavior Change Theory to Increase the Success of Children’s Sleep Education Programs and Contribute to Healthy Development
Abstract
:1. Introduction
1.1. The Detrimental Outcomes of Sleep Problems
1.2. Prevalence of Sleep Problems in Children and Adolescents
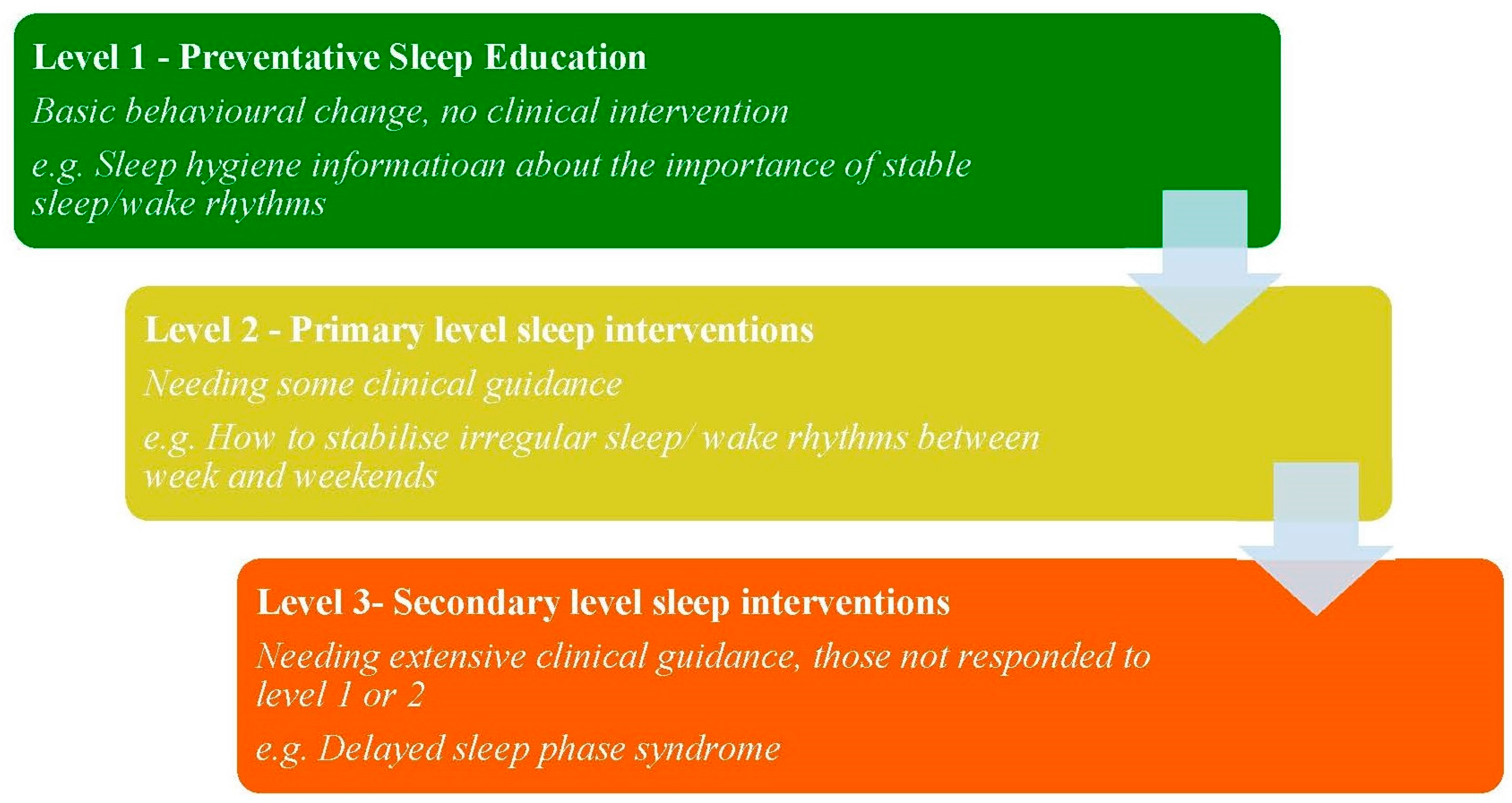
1.3. Treatment of Behavioural Sleep Disorders
2. Is Formal Sleep Education the Answer?
3. Education to Behavioural Change
3.1. Bronfenbrenner’s Ecological Systems Theory
3.1.1. The Micro and Meso Systems in Relation to Sleep
3.1.2. The Exosystem: Economics and Education
3.1.3. The Macrosystem: Culture
3.1.4. The Chronosystem: Time
4. Limitations and Further Research
Author Contributions
Conflicts of Interest
References
- Galland, B.C.; Taylor, B.J.; Elder, D.E.; Herbison, P. Normal sleep patterns in infants and children: A systematic review of observational studies. Sleep Med. Rev. 2012, 16, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Samson, R.; Blunden, S.; Banks, S. The characteristics of sleep and sleep loss in adolescence: A review. Int. Rev. Soc. Sci. Humanit. 2013, 4, 90–107. [Google Scholar]
- Cappucio, F.P.; Taggart, F.M.; Kandala, N.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008, 31, 619–626. [Google Scholar]
- Kjeldsen, J.S.; Hjorth, M.F.; Andersen, R.; Michaelsen, K.F.; Tetens, I.; Astrup, A.; Chaput, J.-P.; Sjödin, A. Short sleep duration and large variability in sleep duration are independently associated with dietary risk factors for obesity in Danish school children. Int. J. Obes. 2014, 38, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Alfano, C.; Gamble, A. The role of sleep in childhood psychiatric disorders. Child Youth Care Forum 2009, 36, 327–340. [Google Scholar] [CrossRef] [PubMed]
- Roane, B.; Taylor, D. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep Breath. 2008, 31, 1351–1356. [Google Scholar]
- Sivertsen, B.; Harvey, A.G.; Pallesen, S.; Hysing, M. Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway. J. Sleep Res. 2015, 24, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Buysse, D.J.; Gentzler, A.L.; Kiss, E.; Mayer, L.; Kapornai, K.; Kovacs, M. Insomnia and hypersomnia associated with depressive phenomenology and comorbidity in childhood depression. Sleep 2007, 30, 83–90. [Google Scholar] [PubMed]
- Ivanenko, A.; Johnson, K. Sleep disturbances in children with psychiatric disorders. Semin. Pediatr. Neurol. 2008, 15, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Alvaro, P.K.; Roberts, R.M.; Harris, J. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep 2013, 36, 1059–1068. [Google Scholar] [CrossRef] [PubMed]
- Fredriksen, K.; Rhodes, J.; Reddy, R.; Way, N. Sleepless in Chicago: Tracking the effects of adolescent sleep loss during the middle school years. Child Dev. 2004, 71, 84–95. [Google Scholar] [CrossRef]
- Lemola, S.; Räikkönen, K.; Scheier, M.F.; Matthews, K.A.; Pesonen, A.K.; Heinonen, K.; Kajantie, E. Sleep quantity, quality and optimism in children. J. Sleep Res. 2011, 20, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Mindell, J.A.; Owens, J. A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems; Lippincott Williams & Wilkins: Philadelphia, USA, 2015. [Google Scholar]
- Blunden, S.L.; Beebe, D. The contribution of intermittent hypoxia, sleep debt and sleep disruption to daytime performance deficits in children: Consideration of respiratory and non-respiratory sleep disorders. Sleep Med. Rev. 2006, 10, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Picchietti, D.L.; Stevens, H.E. Early manifestations of restless legs syndrome in childhood and adolescence. Sleep Med. 2008, 9, 770–781. [Google Scholar] [CrossRef] [PubMed]
- Shakankiry, H.M. Sleep physiology and sleep disorders in childhood. Nat. Sci. Sleep 2011, 3, 101–114. [Google Scholar] [CrossRef] [PubMed]
- Furudate, N.; Komada, Y.; Kobayashi, M.; Nakajima, S.; Inoue, Y. Daytime dysfunction in children with restless legs syndrome. J. Neurol. Sci. 2014, 336, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Saxvig, I.W.; Pallesen, S.; Wilhelmsen-Langeland, A.; Molde, H.; Bjorvatn, B. Prevalence and correlates of delayed sleep phase in high school students. Sleep Med. 2012, 13, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Blunden, S.L. Behavioural sleep disorders across the developmental age span: An overview of causes, consequences and treatment modalitites. Psychology 2012, 3, 249–256. [Google Scholar] [CrossRef]
- AASM. International Classification of Sleep Disorders: Diagnostic and Coding Manual, 2nd ed.; American Academy of Sleep Medicine: Westchester, IL, USA, 2005. [Google Scholar]
- Tan, E.; Healey, D.; Gray, A.R.; Galland, B.C. Sleep hygiene intervention for youth aged 10 to 18 years with problematic sleep: A before-after pilot study. BMC Pediatr. 2012, 12, 189. [Google Scholar] [CrossRef] [PubMed]
- Mindell, J.A.; Sadeh, A.; Wiegand, B.; How, T.H.; Goh, D.Y.T. Developmental aspects of sleep hygiene: Findings from the 2004 national sleep foundation sleep in America Poll. Sleep Med. 2009, 10, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Rigney, G.; Olds, T.; Maher, C.; Blunden, S. Can sleep education improve pre adolescent sleep? Sleep Biol. Rhythms 2013, 11 (Suppl. 2), A128. [Google Scholar]
- Blunden, S.L.; Lushington, K.; Lorenzen, B.; Ooi, T.; Fung, F.; Kennedy, D. Are sleep problems under-recognised in general practice? Arch. Dis. Child. 2004, 89, 708–712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheldon, S.H.; Kryger, M.H.; Ferber, R.; Gozal, D. Principles and Practice of Pediatric Sleep Medicine; Elsevier Health Sciences: New York, USA, 2014. [Google Scholar]
- Boerner, K.; Coulombe, J.A.; Corkum, P. Core competencies for health professionals’ training in pediatric behavioral sleep care: A delphi study. Behav. Sleep Med. 2015, 13, 265–284. [Google Scholar] [CrossRef] [PubMed]
- Blunden, S.; Rigney, G. Lessons learned from sleep education in schools: A review of dos and don’ts. J. Clin. Sleep Med. JCSM 2015, 11, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Gruber, R.; Somerville, G.; Bergmame, L.; Fontil, L.; Paquin, S. School-based sleep education program improves sleep and academic performance of school-age children. Sleep Med. 2016, 21, 93–100. [Google Scholar] [CrossRef]
- Bakotic, M.; Radosevic-Vidacek, B.; Koscec, A. Educating adolescents about healthy sleep: Experimental study of effectiveness of educational leaflet. Croat. Med. J. 2009, 50, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Cain, N.; Gradisar, M.; Moseley, L. A motivational school-based intervention for adolescent sleep problems. Sleep Med. 2011, 12, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Cortesi, F.; Giannotti, F.; Sebastiani, T.; Bruni, O.; Ottaviano, S. Knowledge of sleep in Italian high school students: Pilot-test of school-based sleep educational program. J. Adolesc. Health 2004, 34, 344–351. [Google Scholar] [PubMed]
- Blunden, S.; Champman, J.; Rigney, G. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep Med. Rev. 2011, 16, 355–370. [Google Scholar]
- Espie, C.A. Stepped care: A health technology solution for delivering cognitive behavioral therapy as a first line insomnia treatment. Sleep 2009, 32, 1549–1559. [Google Scholar] [PubMed]
- Lovato, N.; Lack, L.; Wright, H. The napping behaviour of australian university students. PLoS ONE 2014, 9, e113666. [Google Scholar] [CrossRef] [PubMed]
- Cassoff, J.; Knauper, B.; Michaelsen, S.; Gruber, R. School-based sleep promotion programs: Effectiveness, feasibility and insights for future research. Sleep Med. Rev. 2013, 17, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Bronfenbrenner, U.; Ceci, S.J. Nature-nuture reconceptualized in developmental perspective: A bioecological model. Psychol. Rev. 1994, 101, 568–586. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Romack, R.; Jain, J. Bed sharing in school aged children: Clinical and social implications. J. Child Adolesc. Psychiatr. Nurs. 2011, 24, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Keller, P.; El-Sheikh, M. Children’s emotional security and sleep: Longitudinal relations and directions of effects. J. Child Psychol. Psychiatry 2011, 52, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Mindell, J.A.; Sadeh, A.; Kohyama, J.; How, T.H. Parental behaviours and sleep outcomes in infants and toddlers: A cross-cultural comparison. Sleep Med. 2010, 11, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Owens, J.; Jones, C.; Nash, R. Caregivers’ knowledge, behavior, and attitudes regarding healthy sleep in young children. J. Clin. Sleep Med. 2011, 7, 345–350. [Google Scholar] [PubMed]
- Gradisar, M.; Gardner, G.; Dohnt, H. Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region and sleep. Sleep Med. 2011, 12, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.; Kirchner, H.L.; Drotar, D.; Johnson, N.; Rosen, C.; Redline, S. Correlates of adolescent sleep time and variability in sleep time: The role of individual and health related characteristics. Sleep Med. 2011, 12, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Crosby, B.; LeBourgeois, M.K.; Harsh, J. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics 2005, 115, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Whinnery, J.; Jackson, N.; Rattanaumpawan, P.; Grandner, M.A. Short and long sleep duration associated ith race/ethnicity, sociodemographics, and socioeconomic position. Sleep 2014, 37, 601–611. [Google Scholar] [PubMed]
- Bandura, A. Social cognitive theory: An agentic perspective. Ann. Rev. Psychol. 2001, 52, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Wang, H.-S.; Zhang, L.-J.; Liu, X.-C. Co-sleeping and children’s sleep in China. Biol. Rhythm Res. 2010, 41, 169–181. [Google Scholar] [CrossRef]
- Allen, S.L.; Howlett, M.D.; Coulombe, J.A.; Corkum, P.V. ABCs of sleeping: A review of the evidence behind pediatric sleep practice recommendations. Sleep Med. Rev. 2016, 29, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Blunden, S.; Thompson, K.; Dawson, D. Behavioural sleep treatments and night time crying in infants: challenging the status quo. Sleep Med. Rev. 2011, 15, 327–334. [Google Scholar]
- Oskar, J.G.; O’Connor, B.B. Children’s sleep: An interplay between culture and biology. Am. Acad. Paediatr. 2005, 115, 204–216. [Google Scholar]
- Penman, R. The ‘Growing Up’ of Aboriginal and Torres Strait Islander Children: A Literature Review; Department of Families: Canberra, Australia, 2006. [Google Scholar]
- Mindell, J.; Sadeh, A.; Wiegand, B.; How, T.H.; Goh, D.Y. Cross-cultural differences in infant and toddler sleep. Sleep Med 2010, 11, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Matricciani, L.; Olds, T.; Williams, M. A review of evidence for the claim that children are sleeping less than in the past. Sleep 2011, 34, 651–659. [Google Scholar] [PubMed]
- Dollman, J.; Ridley, K.; Olds, T.; Lowe, E. Trends in the duration of school-day sleep among 10- to 15-year-old South Australians between 1985 and 2004. Acta Paediatr. 2007, 96, 1011–1014. [Google Scholar] [CrossRef] [PubMed]
- Blunden, S.; Galland, B. The complexities of defining optimal sleep: Empirical and theoretical considerations with a special emphasis on children. Sleep Med. Rev. 2014, 18, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, G.; McLellan, D.; Dennerlein, J.T.; Pronk, N.P.; Allen, J.D.; Boden, L.I.; Wagner, G.R. Integration of health protection and health promotion: rationale, indicators, and metrics. J. Occup. Environ. Med. 2013, 55 (Suppl. 12), S12–S18. [Google Scholar] [CrossRef] [PubMed]
- Gielen, A.C.; Sleet, D. Application of behavior-change theories and methods to injury prevention. Epidemiol. Rev. 2003, 25, 65–76. [Google Scholar] [CrossRef] [PubMed]
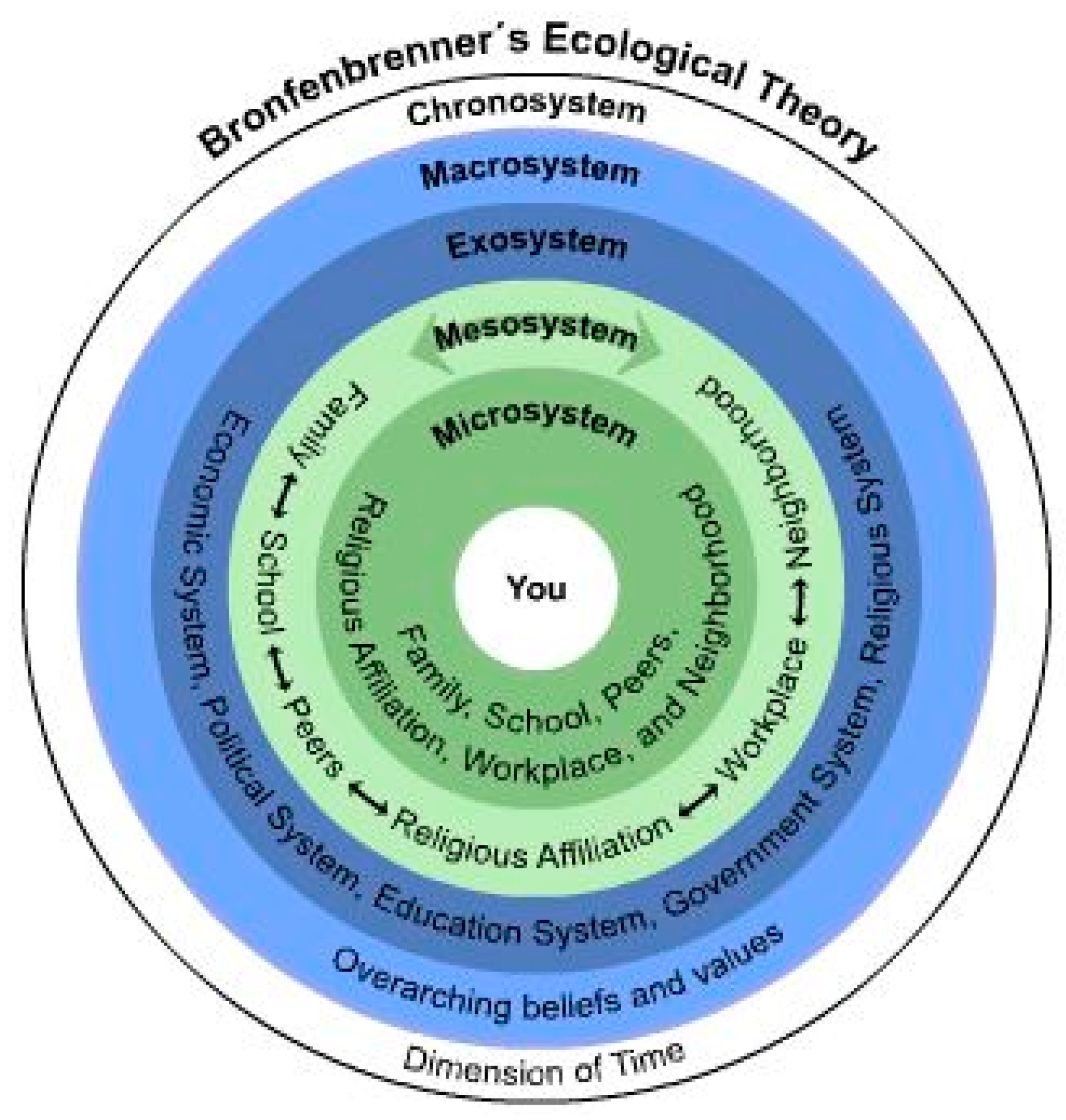
| System Level | Domain | Sleep Impact | Solution |
|---|---|---|---|
| Individual child “you” | The individual child | • Individual differences in sleep need • Individual differences in the importance of sleep • Age • Gender • Temperamental differences in coping with sleep | • Deliver sleep education messages inclusive of individual differences • Promote overall message of sleep health and ability for consumers to critically assess individual sleep need. |
| Microsystem | Family Peers School Close community | • Family preferences • Parental influence and education • Peer pressure • School delivery of sleep education • Close community perceived importance of sleep | • Respect and address individual differences in families • Encourage a whole of school approach • Deliver community based messages of sleep health through close community organisations (sports clubs etc.) |
| Mesosystem | Relationship of Microsystem domains | • Family perceptions are influenced by: education, grandparent perceptions, peers and the importance placed upon sleep by schools, community and peers | • Recognise the relationships between all the above (one cannot be targeted without the other) |
| Exosystem | Education policy | • Sleep education delivered ad hoc in different schools with different agendas • Policy decisions by individual schools and education departments are not systematic • Little sleep education in medical curricula • School curricula are already overloaded | • Introduce systematic sleep education in conjunction with diet and physical activity in schools. • Develop policy guidelines for sleep health • Increase sleep education in medical curricula • Deliver sleep education from the Top down in medical training • Incorporate sleep into overall health messages across curricula areas and ages groups |
| Economy | • Lower SES have poorer sleep • Poorer schools may not prioritise sleep due to curriculum pressures | • Targeting low SES households and/or schools, where sleep health is poorest | |
| Macro System | Culture and ethnicity | • Different cultures prioritise sleep in different ways | • Culturally sensitive sleep education inclusive of how best to improve sleep practices and accounting for cultural differences |
| Chronosystem | Time | • Sleep changes with age • Sleep priorities change with age • One off message are unlikely to have long lasting impact. | • Target specific sleep education to each age group. • Consider that one off messages are not sufficient and sleep health promotion messages needs to be across years and ages |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blunden, S.; Benveniste, T.; Thompson, K. Putting Children’s Sleep Problems to Bed: Using Behavior Change Theory to Increase the Success of Children’s Sleep Education Programs and Contribute to Healthy Development. Children 2016, 3, 11. https://doi.org/10.3390/children3030011
Blunden S, Benveniste T, Thompson K. Putting Children’s Sleep Problems to Bed: Using Behavior Change Theory to Increase the Success of Children’s Sleep Education Programs and Contribute to Healthy Development. Children. 2016; 3(3):11. https://doi.org/10.3390/children3030011
Chicago/Turabian StyleBlunden, Sarah, Tessa Benveniste, and Kirrilly Thompson. 2016. "Putting Children’s Sleep Problems to Bed: Using Behavior Change Theory to Increase the Success of Children’s Sleep Education Programs and Contribute to Healthy Development" Children 3, no. 3: 11. https://doi.org/10.3390/children3030011
APA StyleBlunden, S., Benveniste, T., & Thompson, K. (2016). Putting Children’s Sleep Problems to Bed: Using Behavior Change Theory to Increase the Success of Children’s Sleep Education Programs and Contribute to Healthy Development. Children, 3(3), 11. https://doi.org/10.3390/children3030011






