Abstract
Background/Objectives: This review aims to identify existing protocols and evaluate the effects of prone positioning on oxygenation and clinical outcomes in pediatric patients with hypoxemia. Methods: A systematic review was conducted in accordance with the PRISMA guidelines and registered in PROSPERO (CRD42023457270). Literature research was performed in Scopus, PubMed, Web of Science, and ScienceDirect. The final search was completed in January 2025. Results: A total of 2033 studies were identified, with 5 meeting inclusion criteria. Forty percent applied prone positioning for 12 to 20 h, improving pulmonary function. Combined with alveolar recruitment, prone positioning increased functional residual capacity and reduced atelectasis, with SpO2 improvements from 13% to 38% and atelectasis reduction from 8% to 47%. Another 40% focused on oxygenation, reporting PaO2 increases from 52 to 59 mmHg and SpO2 improvements from 93.2% to 96.2% within 2 to 4 h. One study found a significant SpO2 difference between prone (98.3%) and supine (96.2%) positions (p = 0.003). Protocols commonly included facial tilt and pillows to reduce compression. Safety measures involved checking catheter and tube placement, suspending enteral nutrition 30 min before repositioning, and hemodynamic monitoring. Adverse events were rare, including two cases of tube obstruction and one hypercapnia. No significant differences were observed in ventilation duration, oxygen therapy length, or 28-day survival between groups. Conclusions: Prone positioning improves pulmonary function and addresses refractory hypoxemia in pediatric patients. However, the optimal duration remains unclear, underscoring the need for further research to establish standardized guidelines.
1. Introduction
Prone positioning is commonly used in the management of pediatric patients requiring invasive mechanical ventilation due to pulmonary dysfunction and severe hypoxemia [1]. This approach reduces the pleural pressure gradient, generating more negative dorsal pleural pressures, increasing transpulmonary pressure, and improving alveolar permeability in patients with severe lung diseases [2,3]. It also induces key physiological changes, such as increased functional residual capacity via alveolar recruitment, lung re-expansion, improved ventilation–perfusion ratio (V/Q), reduction in pulmonary shunt, and optimization of positive end-expiratory pressure [4,5].
Prone ventilation is particularly effective for patients with refractory hypoxemia (PaO2 ≤ 60 mmHg) [6], resulting from conditions including pneumonia, pediatric acute respiratory distress syndrome (ARDS), hyaline membrane disease, pulmonary hypertension in neonates, congestive heart failure, and respiratory failure following cardiac surgery [7,8]. ARDS affects 85.4% of premature newborns (<28 weeks) and 44.1% of those born at 28–32 weeks gestation. It is the most prevalent condition in this population and is associated with approximately 40,000 cases annually worldwide, representing the leading cause of neonatal death within the first week of life [4]. However, no standardized ventilatory protocols for prone positioning exist for pediatric patients with refractory hypoxemia. Studies in adults, such as the PROSEVA trial [9], suggest that prone positioning improves V/Q and oxygenation and reduces mortality in severe ARDS. Prolonged prone positioning (>72 h) [10] and early initiation in adults have been shown to decrease mortality at 28 and 90 days [6]. Pediatric studies [11,12] report similar outcomes, including enhanced lung compliance and reduced airway resistance [13,14].
The implementation of the PROSEVA protocol in pediatric intensive care units (PICUs) presents challenges due to anatomical and physiological differences between children and adults [15]. The lack of pediatric-specific prone positioning protocols and limited evidence regarding their effectiveness highlight the need to adapt these strategies to the unique characteristics of pediatric patients. Further research is necessary to assess the safety and efficacy of prone positioning in this population to support evidence-based recommendations [16,17].
The optimal duration of prone positioning in pediatric patients with hypoxemia remains undefined [14,18]. However, advanced pulmonary and thoracic monitoring techniques, such as electrical impedance tomography and biomarker analysis, offer precise tools to guide the timing of transitions between supine and prone positions [19]. Given the limited data on the use of prone positioning during mechanical ventilation in pediatric patients with hypoxemia, this review aims to consolidate current evidence to better understand its effectiveness, safety, and potential benefits or risks.
The primary objective of this review is to identify existing protocols and evaluate the effects of prone positioning on oxygenation, lung function, and clinical safety outcomes in pediatric patients with hypoxemia.
2. Materials and Methods
A systematic review was conducted following the guidelines outlined in the PRISMA statement [20], with registration in PROSPERO (CRD42023457270).
2.1. Research Question
The research question was formulated using the PICO framework: What are the protocols and effects of prone positioning during invasive mechanical ventilation in pediatric patients with hypoxemia? The question was designed based on the following criteria for population, intervention, and outcomes:
- -
- P (Population): Pediatric patients with artificial airways and hypoxemia.
- -
- I (Intervention): Prone positioning during invasive mechanical ventilation.
- -
- C (Comparison): Not applicable.
- -
- O (Outcome): Prone positioning protocols, effects on oxygenation, reduction in lung injury, and associated complications.
2.2. Search Strategy
Based on the research question, a comprehensive search was conducted in the following electronic databases: Web of Science, PubMed, Scopus, and ScienceDirect. The search terms were determined using Medical Subject Headings (MeSH), Health Sciences Descriptors (DeCS), and natural language.
Search Terms
This review was based on existing studies that addressed the previously described topic, including management protocols in the pediatric population. The selection of studies was limited to the PICO question using the following search terms: “pediatrics,” “children,” “prone position,” “artificial ventilation,” and “protocols.” The logical operators “AND” and “OR” were used, which allowed us to generate the equation.
2.3. Eligibility Criteria
The following selection and inclusion criteria were applied: articles addressing the review topic, “Protocols and effects of prone positioning during invasive mechanical ventilation in pediatric patients with hypoxemia,” and articles detailing protocols related to the duration of prone positioning and transitions between supine and prone positions during mechanical ventilation. Only studies involving pediatric patients aged 0 to 18 years (infants/toddlers, school-age children, adolescents) with artificial airways and hypoxemia were included, and publications were accepted without language restrictions. Exclusion criteria included studies where the population did not have artificial airways or receive supplemental oxygen support, as well as secondary literature, such as systematic reviews, reflective reviews, conference proceedings, theses, partial data, and letters to the editor.
2.4. Selection of Sources of Evidence
A systematic search was conducted across multiple databases to identify relevant studies. Duplicates were subsequently removed to maintain the integrity of the selection process. Each study was independently assessed based on predefined inclusion criteria, and those that did not meet these criteria or were duplicated across sources were excluded. To ensure the reliability of the study selection, an agreement analysis between reviewers was performed. Any discrepancies were resolved through discussion or, when necessary, by the involvement of a third reviewer, ensuring accuracy and objectivity in the final selection. The included studies specifically examined the effects and efficacy of supplemental oxygen administration in the prone position, without considering the underlying pathology or the specific indications for its use (Appendix A).
2.5. Data Extraction
A descriptive table was created in Excel once the review and selection of the articles that met the inclusion criteria was completed, and relevant data for each article was collected, including information about the author, year of publication, country where the study was carried out, sample size, study design, and detail of the intervention protocol used. The effects detected in aspects such as oxygenation, lung function, reduction in lung lesions, and possible complications during mechanical ventilation in the prone position in pediatric patients were also included.
2.6. Data Synthesis
The selected articles, which met the eligibility criteria, provided crucial data on the duration and sequence of prone and supine positions and the benefits associated with prone positioning in severe lung diseases. The collected information was organized into descriptive tables highlighting the concepts relevant to the investigation. A flowchart was also outlined based on the PRISMA statement guidelines [20], illustrating the search and selection process for the included studies.
2.7. Quality Assessment
The quality of the studies was assessed independently and in a blinded manner using the PEDro scale [21]. The PEDro scale was employed to evaluate the quality of randomized controlled trials, focusing on factors such as participant randomization, allocation concealment, blinding in assessments, and the use of standardized outcome measurement methods.
3. Results
The initial search identified 2033 studies across four databases. After removing duplicates and articles for various reasons, 1390 records were screened for eligibility, resulting in the selection of 5 articles for full review and methodological quality assessment. Figure 1 provides a graphical representation of the study selection process.
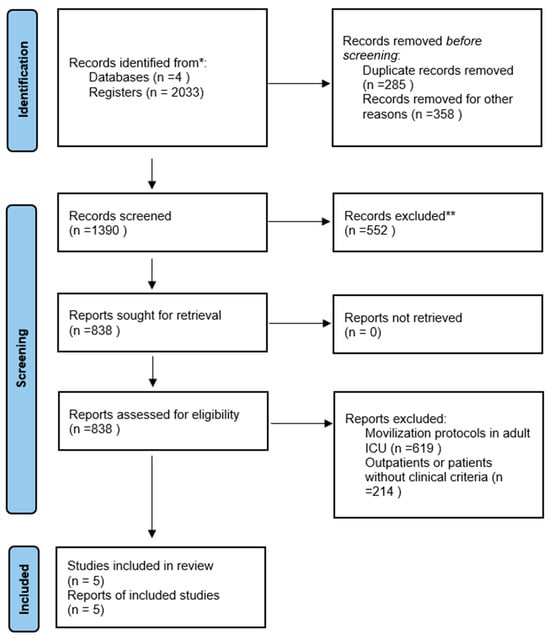
Figure 1.
Flowchart of the systematic review. * Web of Science, PubMed, Scopus, and ScienceDirect ** Review by title.
3.1. Methodological Quality Assessment
The studies selected, published between 2001 and 2020, employed a randomized controlled methodology. After applying the PEDro scale [21], the studies achieved scores ranging from six to eight points, as shown in Table 1.

Table 1.
Evaluation of methodological quality according to the PEDro scale.
3.2. Effect of Prone Positioning on Pulmonary Function and Oxygenation
The review of studies showed that 40% employed prone positioning to enhance lung function in conditions like acute lung injury, with positioning maintained for 12–20 h over a span of 7 days [22,25]. Additionally, Eun et al. (2020) [26] found that combining prone positioning with alveolar recruitment significantly reduced atelectasis formation. The remaining 40% of studies [23,24] focused on the impact of prone positioning on oxygenation, with a duration of 2–4 h being effective for observing changes in PaO2/FiO2 during the first hour.
No studies reported specific respiratory changes due to pathology or hemodynamic instability. Although prone positioning protocols varied, common practices included facial tilt/rotation and the use of pillows on the chest, abdomen, and extremities to relieve compression. It was suggested that the transition from supine to prone should be managed by an interdisciplinary team in a prospective, randomized controlled trial [24].
In the five included randomized controlled trials, two groups were compared: one assessed invasive mechanical ventilation in the supine position, while the other assessed ventilation in the prone position. Zheng et al. [25] further combined prone positioning with high-frequency oscillatory ventilation, observing improvements in SpO2 and PaO2 in the prone group compared to the supine group. All studies reported clinical improvements in oxygenation indices (PaO2/FiO2), lung compliance, mean airway pressure, PaO2, and gas exchange with prone positioning. No significant differences were observed, as summarized in Table 2.

Table 2.
Key characteristics and outcomes of studies on prone positioning in pediatric ventilation.
4. Discussion
This systematic review aimed to assess the protocols and effects of prone positioning during mechanical ventilation in pediatric patients. Five studies were identified, each proposing different protocols; however, a definitive consensus on the transition between supine and prone positions is still lacking. Xu et al. (2021) [27] and Fineman et al. (2006) [28] agree that prior to transitioning from supine to prone, it is essential to evaluate the position of vascular catheters and the endotracheal tube, suspend enteral nutrition 30 min before the transition, and monitor hemodynamics. Diwate et al. (2018) [29] also recommended that pediatric patients remain in the lateral decubitus position for 30 min postprandially as a preventive measure against aspiration.
Sawhney et al. (2005) [24] proposed alternating between the supine and prone positions every 4 h, while Curley et al. (2006) [22] recommended maintaining the prone position for 20 h, followed by 4 h in the supine position. Zheng et al. (2022) [25] combined high-frequency oscillatory ventilation with 12 h of prone positioning in patients with ARDS. This approach resulted in higher SpO2 levels and fewer hypoxic episodes, leading to a reduction in FiO2 requirements. In contrast, Bruno et al. (2001) [23] studied 18 pediatric patients with an average age of 11 months and found statistically significant differences in SpO2 levels between the prone and supine positions (96.2 vs. 98.3, p = 0.003), indicating improved oxygenation in the prone position. Jang et al. (2020) [26] reported that ultrasound-guided alveolar recruitment, when combined with the prone position, significantly increased functional residual capacity (FRC) and improved SpO2 by 13%, preventing atelectasis in the thoracic regions (47% vs. 8%).
Evidence regarding the effects of prone positioning on pediatric lung function remains limited and controversial. Jang et al. (2020) [26] conducted a randomized, non-controlled study with 18 pediatric patients with severe hypoxemia, ventilated in the prone position for 2 h. After 1 h, five patients showed a significant increase in PaO2/FiO2, but no significant differences were observed in those with changes in lung function. The efficacy of prone physiotherapy was also evaluated in pediatric patients with V/Q mismatches and compared with conventional physiotherapy. The experimental group received prone physiotherapy for 4 h daily, in 120 min sessions at 6 h intervals. Significant improvements were noted in SpO2 (96.2 vs. 93.2) and PaO2 (59 mmHg vs. 52 mmHg) levels, with no significant differences in maximum inspiratory pressure (14.60 cmH2O vs. 15.60 cmH2O) [23].
Prone positioning during mechanical ventilation promotes gas exchange and lung function [3,30], but it also carries risks. A randomized controlled trial involving 102 pediatric patients with acute lung injury found no significant reduction in the duration of supplemental oxygenation compared with the supine position (15.6 vs. 15.8 days). The 28-day survival and mechanical ventilation rates were similar, and the mortality rate was 8% in both positions [22]. Furthermore, in the same cohort, adverse effects were noted during prone positioning. While no critical incidents occurred in the 97 patients who were transitioned to the prone position, two cases of endotracheal tube obstruction were observed, and one patient on high-frequency oscillatory ventilation developed hypercapnia [27].
A significant challenge in the current literature on prone positioning for pediatric hypoxemia is the frequent use of small sample sizes, which limits the external validity and generalizability of findings to more heterogeneous pediatric populations. Small cohorts reduce statistical power, hindering the identification of consistent response patterns and rare adverse events, which limit the comprehensive evaluation of the clinical and physiological impacts. Additionally, the lack of standardization in prone positioning protocols complicates the interpretation of research findings [22,23,24,25,26]. Variability in factors such as positioning duration and management strategies introduces inconsistencies across studies. While protocols emphasize patient preparation and continuous monitoring for safety, the absence of standardized guidelines results in practice variability, which affects both outcomes and comparability [16].
The clinical heterogeneity of pediatric hypoxemia further complicates the evaluation of prone positioning. Conditions such as ARDS, infections, congenital malformations, and neuromuscular disorders each involve distinct pathophysiological mechanisms that may alter the response to prone positioning. This makes it difficult to develop a uniform approach applicable to all pediatric subgroups. Furthermore, respiratory physiology and anatomy differ between neonates, infants, and older children, adding another layer of complexity to the assessment of prone positioning. Variations in lung mechanics, respiratory control, and ventilation distribution influence the response to the intervention. These age-related differences necessitate distinct clinical protocols for each subgroup to optimize outcomes [31,32,33].
Despite these variations, prone positioning has been shown to improve oxygenation by increasing the PaO2/FiO2 ratio and arterial oxygen saturation through better ventilation homogeneity, alveolar recruitment, and reduced cardiac compression on the lung parenchyma [31,32,33]. Improved lung compliance and enhanced regional ventilation further optimize gas exchange. While serious complications such as airway obstruction and hemodynamic instability are infrequent, they do require controlled sedation and preventive measures against pressure injuries [34]. Current evidence supports prone positioning as an effective and safe intervention to improve respiratory function in pediatric patients with hypoxemic respiratory failure [35,36].
In the PICU, the effects of prone mechanical ventilation and the associated protocols have been analyzed to inform clinical decision-making. The lack of standardized protocols regarding the optimal duration of prone positioning underscores the need for further research. Although adapting existing protocols to individual patient conditions is recommended, establishing evidence-based, standardized protocols is essential for improving clinical outcomes.
The reviewed studies show significant variability in patient populations, intervention protocols, and outcome measures. Differences in prone positioning duration (ranging from 2 to 20 h), ventilation modalities, and timing of physiological assessments hinder direct comparisons of efficacy and safety outcomes. Some studies also combined prone positioning with adjunct therapies such as high-frequency oscillatory ventilation or ultrasound-guided alveolar recruitment, while others did not. This variability in methodologies may have influenced the oxygenation and lung mechanics results. Moreover, differences in patient age and severity of hypoxemia further limit the generalizability of the findings.
Despite supporting evidence of the benefits of prone positioning—such as improved pulmonary function and correction of hypoxemia—several limitations must be considered when interpreting the results. Variations in study designs, patient characteristics, and methodological approaches hinder direct comparisons and restrict the applicability of findings. Additionally, the lack of standardized protocols for prone mechanical ventilation in pediatric patients remains a barrier to its routine clinical implementation. These challenges underscore the need for multicenter studies with enhanced methodological rigor and standardized protocols to strengthen the evidence on the safety and efficacy of this intervention in the pediatric population.
5. Conclusions
The implementation of prone positioning as a therapeutic strategy in pediatric patients with hypoxemia has shown positive effects on key respiratory parameters, including improvements in oxygenation and ventilatory mechanics. However, challenges remain regarding the standardization of the procedure, inclusion criteria, intervention duration, and monitoring of potential adverse effects. This knowledge gap underscores the importance of continuing to develop controlled, well-structured studies that will allow for the establishment of robust clinical guidelines, tailored to the specific physiological needs of the pediatric population.
Author Contributions
Conceptualization, J.L.E.-Z.; methodology, J.L.E.-Z., V.S.-C., and L.T.O.-M.; validation, J.L.E.-Z.; formal analysis, J.L.E.-Z. and V.S.-C.; investigation, J.L.E.-Z., V.S.-C., and L.T.O.-M.; resources, J.L.E.-Z.; data curation, J.L.E.-Z. and V.S.-C.; writing—original draft preparation, J.L.E.-Z., V.S.-C., and L.T.O.-M.; writing—review and editing, J.L.E.-Z. and V.S.-C.; visualization, J.L.E.-Z. and L.T.O.-M.; supervision, J.L.E.-Z.; project administration, J.L.E.-Z.; funding acquisition, J.L.E.-Z. and L.T.O.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research has been funded by the General Directorate of Investigations of Universidad Santiago de Cali under call No. DGI 01-2025.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| V/Q | Ventilation–perfusion ratio |
| ARDS | Acute respiratory distress syndrome |
| PICUs | Pediatric intensive care units |
| VOAF-PP | High-frequency oscillatory ventilation combined with prone position |
| SpO2 | Oxygen saturation |
| PaO2 | Arterial oxygen pressure |
| PVAm | Mean airway pressure |
| FiO2 | Inspired fraction of oxygen |
| FRC | Functional residual capacity |
Appendix A
Search strategies carried out in each database.
| Database | Search Date | Search Equation | Articles Found |
| Scopus | 7 January 2025 | ((((((Pediatric)) OR (Infant)) OR (Child)) AND (Prone)) AND (Protocol)) AND (Respiration, Artificial) | 542 |
| PubMed | 7 January 2025 | ((((((Pediatric)) OR (Infant)) OR (Child)) AND (Prone)) AND (Protocol)) AND (Respiration, Artificial) | 23 |
| Web of Science | 8 January 2025 | ((((((Pediatric)) OR (Infant)) OR (Child)) AND (Prone)) AND (Protocol)) AND (Respiration, Artificial) | 5 |
| ScienceDirect | 8 January 2025 | ((((((Pediatric)) OR (Infant)) OR (Child)) AND (Prone)) AND (Protocol)) AND (Respiration, Artificial) | 1463 |
References
- Miller, A.G.; Curley, M.A.; Destrampe, C.; Flori, H.; Khemani, R.; Ohmer, A.; Thomas, N.J.; Yehya, N.; Ward, S.; West, L.; et al. A Master Protocol Template for Pediatric ARDS Studies. Respir. Care 2024, 69, 1284–1293. [Google Scholar] [CrossRef] [PubMed]
- Rocha, A.D.S.; Diaper, J.; Balogh, A.L.; Marti, C.; Grosgurin, O.; Habre, W.; Peták, F.; Südy, R. Effect of body position on the redistribution of regional lung aeration during invasive and non-invasive ventilation of COVID-19 patients. Sci. Rep. 2022, 12, 11085. [Google Scholar] [CrossRef]
- Alibrahim, O.; Rehder, K.J.; Miller, A.G.; Rotta, A.T. Mechanical Ventilation and Respiratory Support in the Pediatric Intensive Care Unit. Pediatr. Clin. N. Am. 2022, 69, 587–605. [Google Scholar] [CrossRef] [PubMed]
- Consenso para el Manejo Inicial del Síndrome de Dificultad Respiratoria en Recién Nacidos de Muy Bajo Peso. Available online: https://www.sarda.org.ar/images/2020/8_Guias.pdf (accessed on 8 June 2023).
- Leroue, M.K.; Maddux, A.B.; Mourani, P.M. Prone positioning in children with respiratory failure because of coronavirus disease 2019. Curr. Opin. Pediatr. 2019, 33, 319–324. [Google Scholar] [CrossRef]
- Wong, J.J.M.; Dang, H.; Gan, C.S.; Phan, P.H.; Kurosawa, H.; Aoki, K.; Lee, S.W.; Ong, J.S.M.; Fan, L.J.; Tai, C.W.; et al. Lung-Protective Ventilation for Pediatric Acute Respiratory Distress Syndrome: A Nonrandomized Controlled Trial. Crit. Care Med. 2024, 52, 1602–1611. [Google Scholar] [CrossRef]
- Bhandari, A.P.; Nnate, D.A.; Vasanthan, L.; Konstantinidis, M.; Thompson, J. Positioning for acute respiratory distress in hospitalised infants and children. Cochrane Database Syst. Rev. 2022, 6, CD003645. [Google Scholar] [CrossRef]
- Tavazzi, G. Mechanical ventilation in cardiogenic shock. Curr. Opin. Crit. Care 2021, 27, 447–453. [Google Scholar] [CrossRef]
- Guérin, C.; Reignier, J.; Richard, J.-C.; Beuret, P.; Gacouin, A.; Boulain, T.; Mercier, E.; Badet, M.; Mercat, A.; Baudin, O.; et al. Prone positioning in severe acute respiratory distress syndrome. N. Engl. J. Med. 2013, 368, 2159–2168. [Google Scholar] [CrossRef]
- Jozwiak, M.; Teboul, J.-L.; Anguel, N.; Persichini, R.; Silva, S.; Chemla, D.; Richard, C.; Monnet, X. Beneficial hemodynamic effects of prone positioning in patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2013, 188, 1428–1433. [Google Scholar] [CrossRef]
- Rivas Fernández, M.; Roqué IFiguls, M.; Diez Izquierdo, A.; Escribano, J.; Balaguer, A. Infant position in neonates receiving mechanical ventilation. Cochrane Database Syst. Rev. 2016, 11, CD003668. [Google Scholar] [CrossRef]
- Li, H.; Zhang, X.; Liu, F.; Zhao, B.; Wang, P.; Wang, Y. Application of Ventilator-Assisted Breathing in the Rescue of Neonatal Respiratory Distress Syndrome. Matern. Child. Health Care China 2015, 30, 1293–1294. [Google Scholar]
- Jiang, H.; Zhou, J.; Hai, L.V. Effect of Prone Mechanical Ventilation on Oxygenation Index in Neonates with Respiratory Failure. Med. J. Qilu 2009, 24, 143–144. [Google Scholar]
- Coronado Muñoz, Á.; Escalante Kanashiro, R. Pediatric acute respiratory distress syndrome: How to protect the lungs during mechanical ventilation? Bol. Med. Hosp. Infant. Mex. 2021, 78, 181–190. [Google Scholar] [CrossRef]
- Scholten, E.L.; Beitler, J.R.; Prisk, G.K.; Malhotra, A. Treatment of ARDS with Prone Positioning. Chest 2017, 151, 215–224. [Google Scholar] [CrossRef]
- Kneyber, M.C.; Cheifetz, I.M.; Asaro, L.A.; Graves, T.L.; Viele, K.; Natarajan, A.; Wypij, D.; Curley, M.A.; Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network. Protocol for the Prone and Oscillation Pediatric Clinical Trial (PROSpect). Pediatr Crit Care Med. 2024, 25, e385–e396. [Google Scholar] [CrossRef]
- Egbuta, C.; Easley, R.B. Update on ventilation management in the Pediatric Intensive Care Unit. Paediatr. Anaesth. 2022, 32, 354–362. [Google Scholar] [CrossRef]
- Gattinoni, L.; Carlesso, E.; Taccone, P.; Polli, F.; Guérin, C.; Mancebo, J. Prone Positioning Improves Survival in Severe ARDS: A Pathophysiologic Review and Individual Patient Meta-Analysis. Minerva Anestesiol. 2010, 76, 448–454. [Google Scholar] [PubMed]
- Guérin, C.; Albert, R.K.; Beitler, J.; Gattinoni, L.; Jaber, S.; Marini, J.J.; Munshi, L.; Papazian, L.; Pesenti, A.; Vieillard-Baron, A.; et al. Prone position in ARDS patients: Why, when, how and for whom. Intensive Care Med. 2020, 46, 2385–2396. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef]
- Curley, M.A.; Arnold, J.H.; Thompson, J.E.; Fackler, J.C.; Grant, M.J.; Fineman, L.D.; Cvijanovich, N.; Barr, F.E.; Molitor-Kirsch, S.; Steinhorn, D.M.; et al. Clinical trial design—Effect of prone positioning on clinical outcomes in infants and children with acute respiratory distress syndrome. J. Crit. Care 2006, 21, 23–32; discussion 32–37. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bruno, F.; Piva, J.P.; García, P.C.; Einloft, P.; Fiori, R.; Barreto, S.M. Efeito a curto prazo da posição prona na oxigenação de crianças em ventilação mecânica. J. Pediatr. 2001, 77, 361–368. [Google Scholar] [CrossRef]
- Sawhney, A.; Kumar, N.; Sreenivas, V.; Gupta, S.; Tyagi, V.; Puliyel, J.M. Prone versus supine position in mechanically ventilated children: A pilot study. Med. Sci. Monit. 2005, 11, CR235–CR240. [Google Scholar] [PubMed]
- Zheng, Y.R.; Chen, Y.K.; Lin, S.H.; Cao, H.; Chen, Q. Effect of High-Frequency Oscillatory Ventilation, Combined with Prone Positioning, in Infants with Acute Respiratory Distress Syndrome After Congenital Heart Surgery: A Prospective Randomized Controlled Trial. J. Cardiothorac. Vasc. Anesth. 2022, 36, 3847–3854. [Google Scholar] [CrossRef]
- Jang, Y.E.; Ji, S.H.; Kim, E.H.; Lee, J.H.; Kim, J.T.; Kim, H.S. Effect of regular alveolar recruitment on intraoperative atelectasis in paediatric patients ventilated in the prone position: A randomised controlled trial. Br. J. Anaesth. 2020, 124, 648–655. [Google Scholar] [CrossRef]
- Xu, Y.-L.; Mi, Y.-P.; Zhu, M.-X.; Ren, Y.-H.; Gong, W.-J.; Fu, W.-J.; Wang, H.-M.; Ye, L.; Wang, Y.; Zhou, X.-Y.; et al. Feasibility and effectiveness of prone position ventilation technique for postoperative acute lung injury in infants with congenital heart disease: Study protocol for a prospective randomized study. Trials 2021, 22, 929. [Google Scholar] [CrossRef]
- Fineman, L.D.; LaBrecque, M.A.; Shih, M.C.; Curley, M.A. Prone positioning can be safely performed in critically ill infants and children. Pediatr. Crit. Care Med. 2006, 7, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Diwate, A.; Khatri, S.; Mhaske, S. The effectiveness of cardiopulmonary physiotherapy versus prone positioning on respiratory functions in ventilated neonates: A randomized controlled pilot study. Int. J. Physiother. 2018, 5, 18–22. [Google Scholar] [CrossRef]
- Sanclemente-Cardoza, V.; Estela-Zape, J.L. Adaptaciones mitocondriales en el síndrome de dificultad respiratoria aguda. Rev. Med. Inst. Mex. Seguro Soc. 2024, 62, e5450. (In Spanish) [Google Scholar] [CrossRef]
- Munshi, L.; Del Sorbo, L.; Adhikari, N.K.J.; Hodgson, C.L.; Wunsch, H.; Meade, M.O.; Uleryk, E.; Mancebo, J.; Pesenti, A.; Ranieri, V.M.; et al. Prone Position for Acute Respiratory Distress Syndrome. A Systematic Review and Meta-Analysis. Ann. Am. Thorac. Soc. 2017, 14 (Suppl. S4), S280–S288. [Google Scholar] [CrossRef]
- Rampon, G.L.; Simpson, S.Q.; Agrawal, R. Prone Positioning for Acute Hypoxemic Respiratory Failure and ARDS: A Review. Chest 2023, 163, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Yehya, N.; Smith, L.; Thomas, N.J.; Steffen, K.M.; Zimmerman, J.; Lee, J.H.; Erickson, S.J.; Shein, S.L. Definition, Incidence, and Epidemiology of Pediatric Acute Respiratory Distress Syndrome: From the Second Pediatric Acute Lung Injury Consensus Conference. Pediatr. Crit. Care Med. 2023, 24 (Suppl. S2), S87–S98. [Google Scholar] [CrossRef] [PubMed]
- Qin, W.; Mao, L.; Shen, Y.; Zhao, L. Prone position in the mechanical ventilation of acute respiratory distress syndrome children: A systematic review and meta-analysis. Front. Pediatr. 2024, 12, 1293453. [Google Scholar] [CrossRef] [PubMed]
- Noreña-Buitrón, L.D.; Sanclemente-Cardoza, V.; Espinosa-Cifuentes, M.A.; Payán-Salcedo, H.A.; Estela-Zape, J.L. Early Mobilization Protocols in Critically Ill Pediatric Patients: A Scoping Review of Strategies, Tools and Perceived Barriers. Children 2025, 12, 633. [Google Scholar] [CrossRef]
- Schouten, L.R.A.; Veltkamp, F.; Bos, A.P.; van Woensel, J.B.M.; Neto, A.S.; Schultz, M.J.; Asperen, R.M.W. Incidence and Mortality of Acute Respiratory Distress Syndrome in Children: A Systematic Review and Meta-Analysis. Crit. Care Med. 2016, 44, 819–829. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).