Reliability of the Korean Version of the Eating and Drinking Ability Classification System in Children with Cerebral Palsy
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Statistics
3. Results
3.1. Participant Characteristics
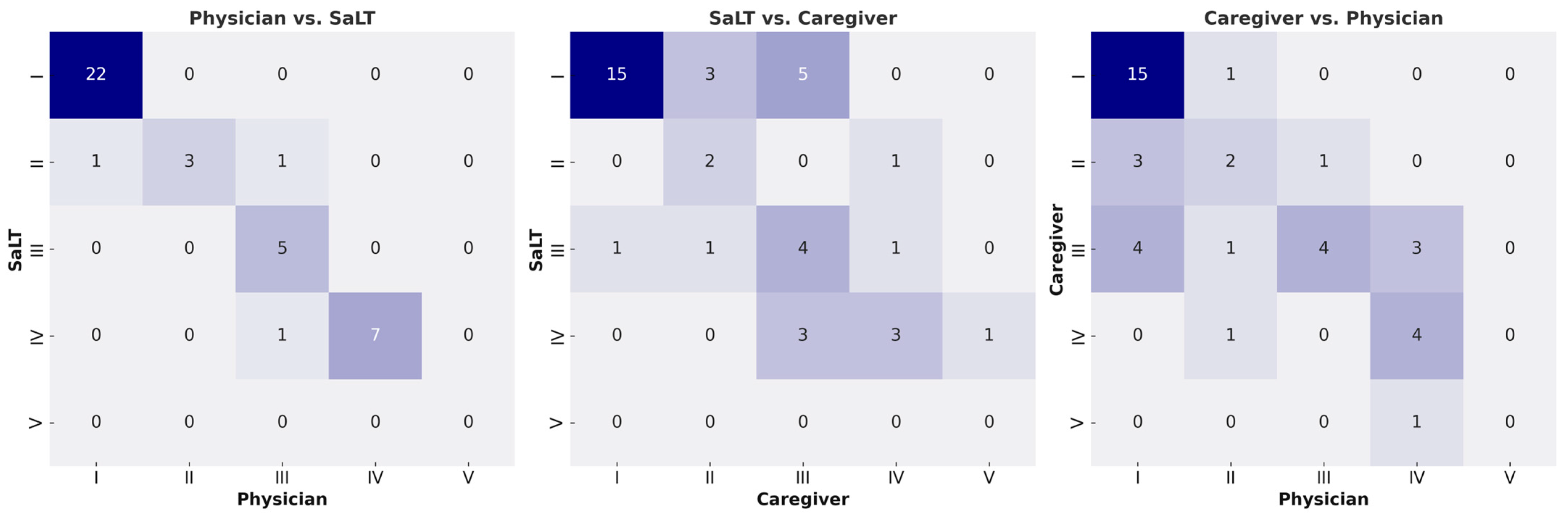
3.2. Assessment of EDACS—Level
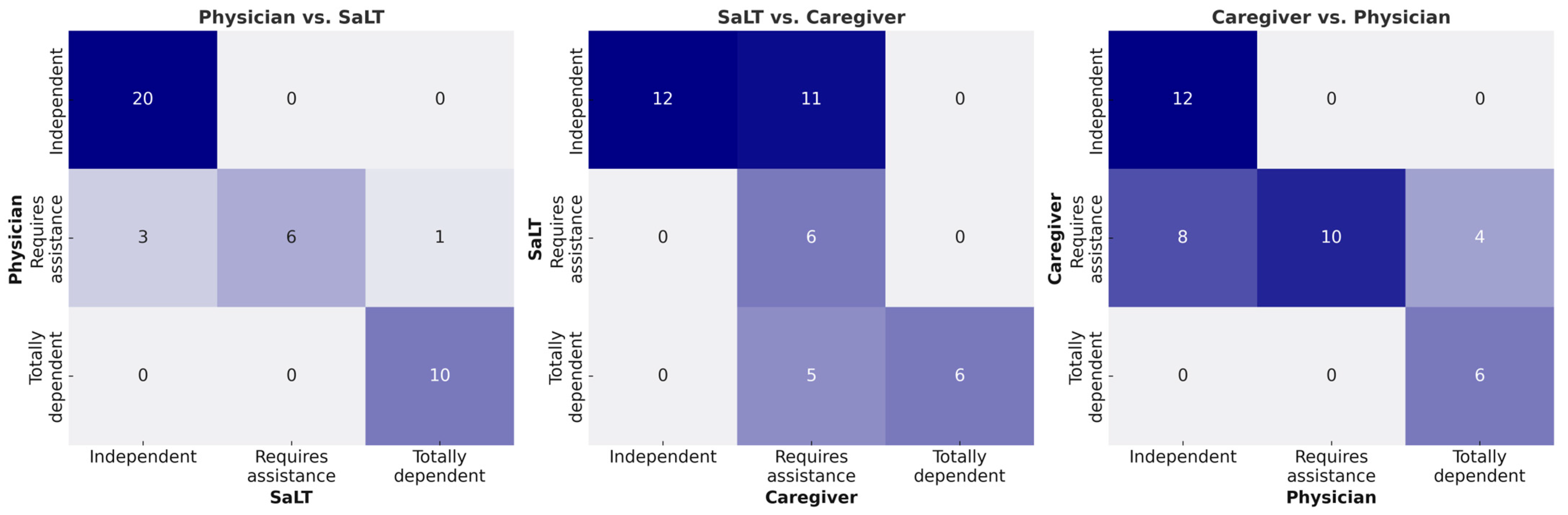
3.3. Assessment of EDACS—Level of Assistance
3.4. Intra-Rater Reliability
3.5. Assessments of EDACS Versus Other Classification Tools
4. Discussion
4.1. Inter and Intra-Rater Reliability
4.2. Relationships Between EDACS and Other Functional Classification Tools
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| EDACS | Eating and Drinking Ability Classification System |
| CP | Cerebral palsy |
| SaLT | Speech and language therapist |
| FOIS | Functional Oral Intake Scale |
| GMFCS | Gross Motor Function Classification System |
| MACS | Manual Ability Classification System |
| CFCS | Communication Function Classification System |
References
- Aisen, M.L.; Kerkovich, D.; Mast, J.; Mulroy, S.; Wren, T.A.; Kay, R.M.; Rethlefsen, S.A. Cerebral palsy: Clinical care and neurological rehabilitation. Lancet Neurol. 2011, 10, 844–852. [Google Scholar] [CrossRef] [PubMed]
- Speyer, R.; Cordier, R.; Kim, J.H.; Cocks, N.; Michou, E.; Wilkes-Gillan, S. Prevalence of drooling, swallowing, and feeding problems in cerebral palsy across the lifespan: A systematic review and meta-analyses. Dev. Med. Child Neurol. 2019, 61, 1249–1258. [Google Scholar] [CrossRef] [PubMed]
- Benfer, K.A.; Weir, K.A.; Bell, K.L.; Ware, R.S.; Davies, P.S.W.; Boyd, R.N. Oropharyngeal dysphagia and cerebral palsy. Pediatrics 2017, 140, e20170731. [Google Scholar] [CrossRef] [PubMed]
- Sadowska, M.; Sarecka-Hujar, B.; Kopyta, I. Cerebral palsy: Current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr. Dis. Treat. 2020, 16, 1505–1518. [Google Scholar] [CrossRef]
- Sellers, D.; Mandy, A.; Pennington, L.; Hankins, M.; Morris, C. Development and reliability of a system to classify the eating and drinking ability of people with cerebral palsy. Dev. Med. Child Neurol. 2014, 56, 245–251. [Google Scholar] [CrossRef]
- Tschirren, L.; Bauer, S.; Hanser, C.; Marsico, P.; Sellers, D.; van Hedel, H.J.A. The Eating and Drinking Ability Classification System: Concurrent validity and reliability in children with cerebral palsy. Dev. Med. Child Neurol. 2018, 60, 611–617. [Google Scholar] [CrossRef]
- Gibson, N.; Blackmore, A.M.; Chang, A.B.; Cooper, M.S.; Jaffe, A.; Kong, W.R.; Langdon, K.; Moshovis, L.; Pavleski, K.; Wilson, A.C. Prevention and management of respiratory disease in young people with cerebral palsy: Consensus statement. Dev. Med. Child Neurol. 2021, 63, 172–182. [Google Scholar] [CrossRef]
- McAllister, A.; Sjöstrand, E.; Rodby-Bousquet, E. Eating and drinking ability and nutritional status in adults with cerebral palsy. Dev. Med. Child Neurol. 2022, 64, 1017–1024. [Google Scholar] [CrossRef]
- Sorhage, A.; Blackmore, A.M.; Byrnes, C.A.; Agnew, C.; Webster, E.F.M.; Mackey, A.; Chong, J.; Hill, T.M.; Han, D.Y.; Stott, N.S. Eating and drinking abilities and respiratory and oral health in children and young adults with cerebral palsy. Dev. Med. Child Neurol. 2025. [Google Scholar] [CrossRef]
- Crary, M.A.; Mann, G.D.; Groher, M.E. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch. Phys. Med. Rehabil. 2005, 86, 1516–1520. [Google Scholar] [CrossRef]
- Christiaanse, M.E.; Mabe, B.; Russell, G.; Simeone, T.L.; Fortunato, J.; Rubin, B. Neuromuscular electrical stimulation is no more effective than usual care for the treatment of primary dysphagia in children. Pediatr. Pulmonol. 2011, 46, 559–565. [Google Scholar] [CrossRef]
- Goh, Y.R.; Choi, J.Y.; Kim, S.A.; Park, J.; Park, E.S. Comparisons of severity classification systems for oropharyngeal dysfunction in children with cerebral palsy: Relations with other functional profiles. Res. Dev. Disabil. 2018, 72, 248–256. [Google Scholar] [CrossRef] [PubMed]
- van Hulst, K.; Snik, D.A.C.; Jongerius, P.H.; Sellers, D.; Erasmus, C.E.; Geurts, A.C.H. Reliability, construct validity and usability of the Eating and Drinking Ability Classification System (EDACS) among Dutch children with Cerebral Palsy. J. Pediatr. Rehabil. Med. 2018, 11, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.C.; Buckeridge, K.; Lee, T.A.; Sellers, D. Reliability and validity of the Eating and Drinking Ability Classification System (EDACS) for children with cerebral palsy in Taiwan. Disabil. Rehabil. 2022, 44, 6438–6444. [Google Scholar] [CrossRef] [PubMed]
- Hyun, S.E.; Yi, Y.G.; Shin, H.I. Reliability and validity of the Eating and Drinking Ability Classification System in adults with cerebral palsy. Dysphagia 2021, 36, 351–361. [Google Scholar] [CrossRef]
- Flack, V.F.; Afifi, A.; Lachenbruch, P.; Schouten, H. Sample size determinations for the two rater kappa statistic. Psychometrika 1988, 53, 321–325. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Sellers, D.; Pennington, L.; Bryant, E.; Benfer, K.; Weir, K.; Aboagye, S.; Morris, C. Mini-EDACS: Development of the Eating and Drinking Ability Classification System for young children with cerebral palsy. Dev. Med. Child Neurol. 2022, 64, 897–906. [Google Scholar] [CrossRef]
- Benfer, K.A.; Weir, K.A.; Bell, K.L.; Ware, R.S.; Davies, P.S.W.; Boyd, R.N. The Eating and Drinking Ability Classification System in a population-based sample of preschool children with cerebral palsy. Dev. Med. Child Neurol. 2017, 59, 647–654. [Google Scholar] [CrossRef]
- Sellers, D.; Mandy, A.; Pennington, L.; Hankins, M.; Morris, C. Korean EDACS. Available online: https://www.sussexcommunity.nhs.uk/patients-and-visitors/resources/research-resources/korean-edacs (accessed on 19 April 2025).
- Schratz, L.M.; Larkin, O.; Dos Santos, N.; Martin, C. Caregiver influences on eating behaviors in children: An opportunity for preventing obesity. Curr. Atheroscler. Rep. 2023, 25, 1035–1045. [Google Scholar] [CrossRef]
- Yim, E.P. Effects of Asian cultural values on parenting style and young children’s perceived competence: A cross-sectional study. Front. Psychol. 2022, 13, 905093. [Google Scholar] [CrossRef] [PubMed]
- Serel Arslan, S.; Demir, N.; Karaduman, A.A.; Belafsky, P.C. The Pediatric Version of the Eating Assessment Tool: A caregiver administered dyphagia-specific outcome instrument for children. Disabil. Rehabil. 2018, 40, 2088–2092. [Google Scholar] [CrossRef] [PubMed]
- Serel Arslan, S.; Demir, N.; Karaduman, A.A. Turkish Version of the Mastication Observation and Evaluation (MOE) Instrument: A Reliability and Validity Study in Children. Dysphagia 2020, 35, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Remijn, L.; Speyer, R.; Groen, B.E.; Holtus, P.C.; van Limbeek, J.; Nijhuis-van der Sanden, M.W. Assessment of mastication in healthy children and children with cerebral palsy: A validity and consistency study. J. Oral Rehabil. 2013, 40, 336–347. [Google Scholar] [CrossRef]
- Nishibu, H.; Seino, T.H.; Himuro, N. Psychometric evaluation and distribution of classification systems in children with cerebral palsy in Japan. J. Pediatr. Rehabil. Med. 2023, 16, 223–233. [Google Scholar] [CrossRef]
- Sellers, D.; Bryant, E.; Hunter, A.; Campbell, V.; Morris, C. The Eating and Drinking Ability Classification System for cerebral palsy: A study of reliability and stability over time. J. Pediatr. Rehabil. Med. 2019, 12, 123–131. [Google Scholar] [CrossRef]
- Hidecker, M.J.; Paneth, N.; Rosenbaum, P.L.; Kent, R.D.; Lillie, J.; Eulenberg, J.B.; Chester, K., Jr.; Johnson, B.; Michalsen, L.; Evatt, M.; et al. Developing and validating the Communication Function Classification System for individuals with cerebral palsy. Dev. Med. Child Neurol. 2011, 53, 704–710. [Google Scholar] [CrossRef]
- Arvedson, J.; Clark, H.; Lazarus, C.; Schooling, T.; Frymark, T. The effects of oral-motor exercises on swallowing in children: An evidence-based systematic review. Dev. Med. Child Neurol. 2010, 52, 1000–1013. [Google Scholar] [CrossRef]
| Characteristics | |
|---|---|
| Age at assessment (years), mean (range) | 8.4 (3–17) |
| Gestational age (weeks), mean (range) | 32.5 (21–40) |
| Sex, n (%) | |
| Male | 21 (52.5) |
| Female | 19 (47.5) |
| Tone abnormality | |
| Spastic | 30 (75.0) |
| Dyskinetic | 2 (5.0) |
| Ataxic | 3 (7.5) |
| Mixed | 2 (5.0) |
| Non-classifiable | 3 (7.5) |
| Motor distribution, n (%) | |
| Unilateral | 6 (12.0) |
| Bilateral | 44 (88.0) |
| GMFCS, n (%) | |
| I | 12 (30.0) |
| II | 9 (22.5) |
| III | 4 (10.0) |
| IV | 10 (25.0) |
| V | 5 (12.5) |
| MACS, n (%) | |
| I | 11 (27.5) |
| II | 8 (20.0) |
| III | 12 (30.0) |
| IV | 4 (10.0) |
| V | 5 (12.5) |
| CFCS, n (%) | |
| I | 13 (32.5) |
| II | 4 (10.0) |
| III | 3 (7.5) |
| IV | 2 (5.0) |
| V | 18 (45.0) |
| Physician * | ||||||
|---|---|---|---|---|---|---|
| SaLT * | I | II | III | IV | V | Total |
| I | 22 | 1 | 0 | 0 | 0 | 23 |
| II | 0 | 3 | 0 | 0 | 0 | 3 |
| III | 0 | 1 | 5 | 1 | 0 | 7 |
| IV | 0 | 0 | 0 | 7 | 0 | 7 |
| V | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 22 | 5 | 5 | 8 | 0 | 40 |
| SaLT † | ||||||
| Caregiver † | I | II | III | IV | V | Total |
| I | 15 | 0 | 1 | 0 | 0 | 16 |
| II | 3 | 2 | 1 | 0 | 0 | 6 |
| III | 5 | 0 | 4 | 3 | 0 | 12 |
| IV | 0 | 1 | 1 | 3 | 0 | 5 |
| V | 0 | 0 | 0 | 1 | 0 | 1 |
| Total | 23 | 3 | 7 | 7 | 0 | 40 |
| Caregiver ‡ | ||||||
| Physician ‡ | I | II | III | IV | V | Total |
| I | 15 | 3 | 4 | 0 | 0 | 22 |
| II | 1 | 2 | 1 | 1 | 0 | 5 |
| III | 0 | 1 | 4 | 0 | 0 | 5 |
| IV | 0 | 0 | 3 | 4 | 1 | 8 |
| V | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 16 | 6 | 12 | 5 | 1 | 40 |
| Physician * | ||||
|---|---|---|---|---|
| SaLT * | Independent | Requires assistance | Totally dependent | Total |
| Independent | 20 | 3 | 0 | 23 |
| Requires assistance | 0 | 6 | 0 | 6 |
| Totally dependent | 0 | 1 | 10 | 11 |
| Total | 20 | 10 | 10 | 40 |
| SaLT † | ||||
| Caregiver † | Independent | Requires assistance | Totally dependent | Total |
| Independent | 12 | 0 | 0 | 12 |
| Requires assistance | 11 | 6 | 5 | 22 |
| Totally dependent | 0 | 0 | 6 | 6 |
| Total | 23 | 6 | 11 | 40 |
| Caregiver ‡ | ||||
| Physician ‡ | Independent | Requires assistance | Totally dependent | Total |
| Independent | 12 | 8 | 0 | 20 |
| Requires assistance | 0 | 10 | 0 | 10 |
| Totally dependent | 0 | 4 | 6 | 10 |
| Total | 12 | 22 | 6 | 40 |
| EDACS | |||||
|---|---|---|---|---|---|
| I | II | III | IV | Total | |
| FOIS | |||||
| IV | 0 | 0 | 0 | 1 | 1 |
| V | 0 | 0 | 3 | 3 | 6 |
| VI | 1 | 3 | 2 | 4 | 10 |
| VII | 21 | 2 | 0 | 0 | 23 |
| Total | 22 | 5 | 5 | 8 | 40 |
| GMFCS | |||||
| I | 11 | 1 | 0 | 0 | 12 |
| II | 7 | 0 | 1 | 1 | 9 |
| III | 3 | 1 | 0 | 0 | 4 |
| IV | 1 | 3 | 3 | 3 | 10 |
| V | 0 | 0 | 1 | 4 | 5 |
| Total | 22 | 5 | 5 | 8 | 40 |
| MACS | |||||
| I | 10 | 1 | 0 | 0 | 11 |
| II | 8 | 0 | 0 | 0 | 8 |
| III | 4 | 3 | 2 | 3 | 12 |
| IV | 0 | 1 | 2 | 1 | 4 |
| V | 0 | 0 | 1 | 4 | 5 |
| Total | 22 | 5 | 5 | 8 | 40 |
| CFCS | |||||
| I | 13 | 0 | 0 | 0 | 13 |
| II | 3 | 1 | 0 | 0 | 4 |
| III | 21 | 1 | 0 | 0 | 3 |
| IV | 1 | 1 | 0 | 0 | 2 |
| V | 3 | 2 | 5 | 8 | 18 |
| Total | 22 | 5 | 5 | 8 | 40 |
| EDACS | ||||
|---|---|---|---|---|
| Independent | Requires Assistance | Totally Dependent | Total | |
| FOIS | ||||
| IV | 0 | 0 | 3 | 2 |
| V | 0 | 3 | 2 | 6 |
| VI | 1 | 4 | 4 | 9 |
| VII | 19 | 3 | 1 | 23 |
| Total | 20 | 10 | 10 | 40 |
| GMFCS | ||||
| I | 11 | 1 | 0 | 12 |
| II | 7 | 1 | 1 | 9 |
| III | 1 | 3 | 0 | 4 |
| IV | 1 | 5 | 4 | 10 |
| V | 0 | 0 | 5 | 5 |
| Total | 20 | 10 | 10 | 40 |
| MACS | ||||
| I | 11 | 1 | 0 | 12 |
| II | 7 | 0 | 0 | 7 |
| III | 2 | 8 | 2 | 12 |
| IV | 0 | 1 | 3 | 4 |
| V | 0 | 0 | 5 | 5 |
| Total | 20 | 10 | 10 | 40 |
| CFCS | ||||
| I | 11 | 2 | 0 | 13 |
| II | 3 | 1 | 0 | 4 |
| III | 2 | 1 | 0 | 3 |
| IV | 1 | 0 | 1 | 2 |
| V | 3 | 6 | 9 | 18 |
| Total | 20 | 10 | 10 | 40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, S.; Jung, K.-J.; Choi, Y.; Rha, D.-W. Reliability of the Korean Version of the Eating and Drinking Ability Classification System in Children with Cerebral Palsy. Children 2025, 12, 673. https://doi.org/10.3390/children12060673
Hwang S, Jung K-J, Choi Y, Rha D-W. Reliability of the Korean Version of the Eating and Drinking Ability Classification System in Children with Cerebral Palsy. Children. 2025; 12(6):673. https://doi.org/10.3390/children12060673
Chicago/Turabian StyleHwang, Sangwon, Kang-Jae Jung, Yeonhee Choi, and Dong-Wook Rha. 2025. "Reliability of the Korean Version of the Eating and Drinking Ability Classification System in Children with Cerebral Palsy" Children 12, no. 6: 673. https://doi.org/10.3390/children12060673
APA StyleHwang, S., Jung, K.-J., Choi, Y., & Rha, D.-W. (2025). Reliability of the Korean Version of the Eating and Drinking Ability Classification System in Children with Cerebral Palsy. Children, 12(6), 673. https://doi.org/10.3390/children12060673








