Residual Adenoid Tissue After Conventional Adenoidectomy and the Role of Intraoperative Nasal Endoscopy: A Prospective Cohort Study
Abstract
Highlights
- What are the main findings?
- Residual adenoid tissue was detected in 61.8% of patients after conventional curettage adenoidectomy.
- Revision status and age ≥ 7.5 years were strong predictors of incomplete clearance.
- What is the implication of the main findings?
- Intraoperative endoscopic assessment with completion resection significantly improves surgical outcomes.
- Primary endoscopic adenoidectomy is recommended for children ≥ 7.5 years and for revision cases.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
- Group 1: Primary surgery in patients under 9 years of age (40 patients);
- Group 2: Secondary surgery in patients under 9 years of age (40 patients);
- Group 3: Primary surgery in patients aged 9 years or older (60 patients);
- Group 4: Secondary surgery in patients aged 9 years or older (38 patients).
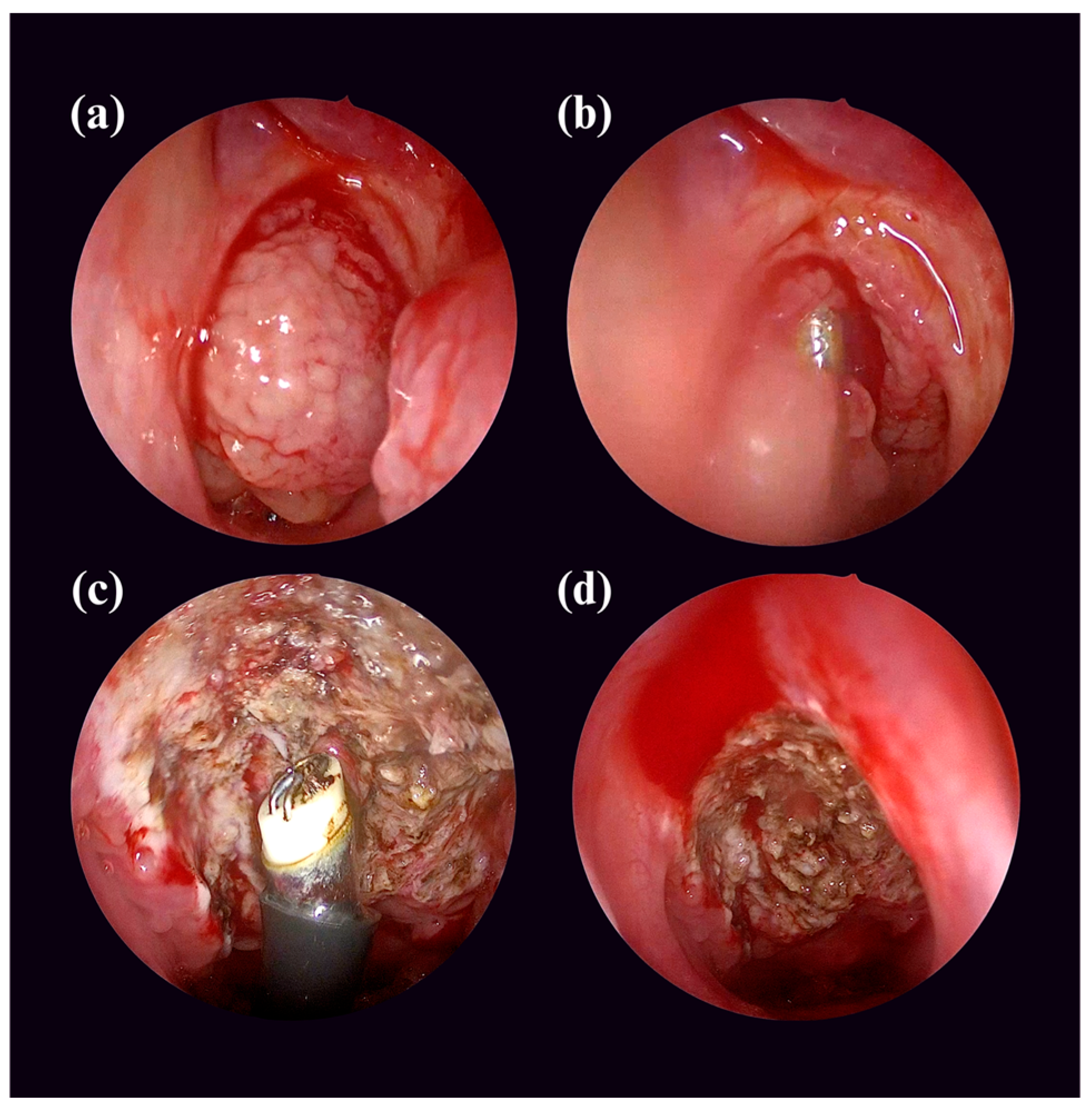
2.3. Surgical Intervention
2.4. Variables
- 1
- Anamnesis data, including symptoms and history of previous adenoidectomy.
- 2
- Preoperative clinical findings, including nasal endoscopy and general examination results.
- 3
- Subjective measures of symptom severity, assessed both preoperatively and postoperatively:
- 4
- Operative details, including the type of surgical procedure performed, whether concomitant tonsillectomy was conducted, Parikh et al.’s adenoid hypertrophy grading [14], and other relevant intraoperative observations.
- 5
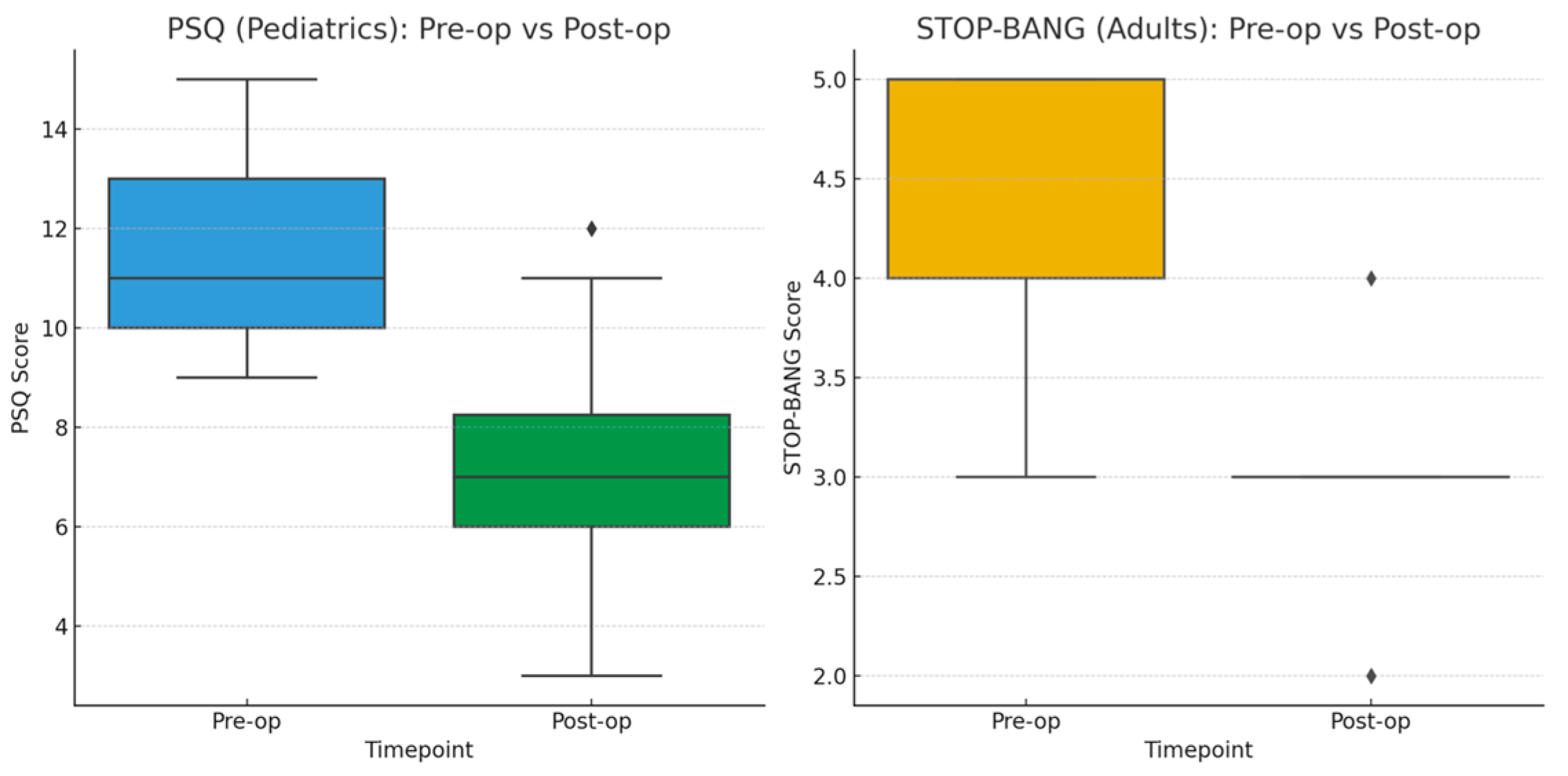
- All patients were followed postoperatively at 1 week, 1 month, and 2 months. Each visit included clinical examination, evaluation of symptom resolution, and documentation of complications such as bleeding, infection, or otalgia. Parents or patients were questioned regarding persistence or recurrence of nasal obstruction and otologic symptoms. Symptom severity was assessed at each visit using the Pediatric Sleep Questionnaire (PSQ) for patients younger than 18 years and the STOP-Bang questionnaire for patients aged 18 years or older. Both instruments were re-administered at the final 2-month follow-up to evaluate postoperative improvement in sleep-disordered breathing. Nasal endoscopy was not performed routinely, but was selectively conducted in patients with persistent symptoms to rule out residual or recurrent adenoid tissue.
2.5. Ethical Approval and Participation Consent
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PSQ | Pediatric Sleep Questionnaire |
| STOP-BANG | Snoring, Tiredness, Observed apnea, Pressure, Body-mass index, Age, Neck circumference, Gender (OSA screening tool) |
| OSA | Obstructive Sleep Apnea |
| IQR | Interquartile Range |
| ROC | Receiver Operating Characteristic |
| AUC | Area Under the Curve |
| CI | Confidence Interval (95% CI) |
| RR | Relative Risk |
| OR | Odds Ratio |
| χ2 | Chi-square statistic |
| W | Wilcoxon signed-rank test statistic |
| z | Standard normal z-score |
| ΔAUC | Difference in area under the curve |
References
- Malas, M.; Althobaiti, A.A.; Sindi, A.; Bukhari, A.F.; Zawawi, F. Comparison of the efficacy and safety of conventional curettage adenoidectomy with those of other adenoidectomy surgical techniques: A systematic review and network meta-analysis. J. Otolaryngol. Head Neck Surg. 2023, 52, 21. [Google Scholar] [CrossRef]
- Abo Elmagd, E.A.; Khalifa, M.S.; Abeskharoon, B.K.; El Tahan, A.A. Comparative study between conventional adenoidectomy and adenoidectomy using micro-debrider. Egypt. J. Otolaryngol. 2021, 37, 56. [Google Scholar] [CrossRef]
- Rosenfeld, R.M.; Shin, J.J.; Schwartz, S.R.; Coggins, R.; Gagnon, L.; Hackell, J.M.; Hoelting, D.; Hunter, L.L.; Kummer, A.W.; Payne, S.C.; et al. Clinical practice guideline: Otitis media with effusion (update). Otolaryngol. Head Neck Surg. 2016, 154 (Suppl. S1), S1–S41. [Google Scholar] [CrossRef]
- Skoloudik, L.; Kalfert, D.; Valenta, T.; Chrobok, V. Relation between adenoid size and otitis media with effusion. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2018, 135, 399–402. [Google Scholar] [CrossRef] [PubMed]
- Sahni, D.; Kaur, G.; Bhagat, S.; Singh, P.; Verma, P.; Chhabra, N. Comparison between endoscope assisted powered and conventional adenoidectomy. Int. J. Otorhinolaryngol. Head Neck Surg. 2021, 7, 50–55. [Google Scholar] [CrossRef]
- Pradeesh, D.; Pillai, A.R.; Rajamma, K.B. Comparison of perioperative collateral injury, presence of residual adenoid tissue and recovery time in conventional versus microdebrider assisted endoscopic adenoidectomy in children ≤12 years. Int. J. Contemp. Med. Res. 2019, 6, D6–D9. [Google Scholar] [CrossRef]
- Krishnakumar, N.; Bashir, N.K.; Raj, G. Comparison of blood loss in endoscopic powered adenoidectomy and conventional curettage. Int. J. Otorhinolaryngol. Head Neck Surg. 2019, 5, 577–580. [Google Scholar] [CrossRef]
- Kumaraswamy, N.H.; Warhapande, S.S.; Saritha, H.M. Adequacy of traditional curette versus powered shaver for adenoid clearance: A comparative study. Int. J. Contemp. Pediatr. 2023, 10, 1240–1244. [Google Scholar] [CrossRef]
- Katakdhond, H.; Mestry, V.; Sardesai, R.B. Clinical outcomes of endoscopy assisted conventional adenoidectomy and endoscopic adenoidectomy with microdebrider: A prospective randomized control study. Int. J. Otorhinolaryngol. Head Neck Surg. 2025, 11, 117–125. [Google Scholar] [CrossRef]
- Kim, J.W.; Kim, H.J.; Lee, W.H.; Kim, D.-K.; Kim, S.W.; Kim, Y.H.; Nam, J.G.; Park, S.-W.; Park, C.-S.; Bae, W.Y.; et al. Comparative study for efficacy and safety of adenoidectomy according to the surgical method: A prospective multicenter study. PLoS ONE 2015, 10, e0135304. [Google Scholar] [CrossRef]
- Gheorghe, D.C.; Zamfir-Chiru-Anton, A. Surgical considerations about shaver adenoidectomy: Our experience. Practice Med. 2014, 9, 7–10. [Google Scholar] [CrossRef]
- Chervin, R.D.; Hedger, K.; Dillon, J.E.; Pituch, K.J. Pediatric Sleep Questionnaire (PSQ): Validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000, 1, 21–32. [Google Scholar] [CrossRef]
- Chen, L.; Pivetta, B.; Nagappa, M.; Saripella, A.; Islam, S.; Englesakis, M.; Chung, F. Validation of the STOP-Bang questionnaire for screening of obstructive sleep apnea in the general population and commercial drivers: A systematic review and meta-analysis. Sleep Breath. 2021, 25, 1741–1751. [Google Scholar] [CrossRef]
- Parikh, S.R.; Coronel, M.; Lee, J.J.; Brown, S.M. Validation of a new grading system for endoscopic examination of adenoid hypertrophy. Otolaryngol. Head Neck Surg. 2006, 135, 684–687. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, N.; Don, D.M.; Koempel, J.A. The incidence of revision adenoidectomy: A comparison of four surgical techniques over a 10-year period. Otolaryngol. Head Neck Surg. 2021, 165, 523–529. [Google Scholar] [CrossRef]
- Muniraju, M.; Saifulla, M. A comparative study of adenoidectomy by microdebrider vs conventional method. Int. J. Otorhinolaryngol. Head Neck Surg. 2018, 4, 808–814. [Google Scholar] [CrossRef]
- Saibene, A.M.; Rosso, C.; Pipolo, C.; Lozza, P.; Scotti, A.; Ghelma, F.; Allevi, F.; Maccari, A.; Felisati, G. Endoscopic adenoidectomy: A systematic analysis of outcomes and complications in 1006 patients. Acta Otorhinolaryngol. Ital. 2020, 40, 79–86. [Google Scholar] [CrossRef]
- Kumar, A.; Narayan, P.; Narain, P.; Singh, J.; Porwal, P.K.; Sharma, S. A comparative study of endoscopic assisted curettage adenoidectomy with conventional adenoidectomy. Int. J. Otorhinolaryngol. Head Neck Surg. 2018, 4, 1053–1056. [Google Scholar] [CrossRef]
- Modi, A.T.; Raval, J.B.; Aiyer, R.G.; Shah, P.C. Comparative study between conventional curettage adenoidectomy versus endoscopic microdebrider assisted adenoidectomy: Our experience. Indian J. Otolaryngol. Head Neck Surg. 2020, 72, 388–393. [Google Scholar] [CrossRef]
- Raj, A.; Saldanha, M.; Kalam, A.S.; Aroor, R.; Kamath, S.D. Conventional adenoidectomy versus endoscope-assisted adenoidectomy: Comparative study. J. Health Allied Sci. NU 2025, 15, 70–73. [Google Scholar] [CrossRef]
- John, J.; Thomas, R.; Velayutham, P.; Abraham, U.; Varghese, K.; Mathew, V. Objective and subjective outcome measures in conventional curettage adenoidectomy vs endoscopic guided microdebrider assisted adenoidectomy: A prospective randomized single-blind study. South East. Eur. J. Public. Health 2025, 13, 4381–4390. [Google Scholar] [CrossRef]
- Venkatesh, S.; Murthy, S.K.; Parameswaran, G. Endoscopic coblation adenoidectomy and conventional adenoidectomy: A comparative study. Int. J. Otorhinolaryngol. Head Neck Surg. 2023, 9, 704–708. [Google Scholar] [CrossRef]
- Alharbi, F.; Ahmed, M.R.; Juraibi, W.A. Microdebrider-assisted powered adenoidectomy: A prospective study. Egypt. J. Otolaryngol. 2019, 35, 37–40. [Google Scholar] [CrossRef]
- MacKeith, S.; Mulvaney, C.A.; Galbraith, K.; Webster, K.E.; Paing, A.; Connolly, R.; Marom, T.; Daniel, M.; Venekamp, R.P.; Schilder, A.G.M. Adenoidectomy for otitis media with effusion (OME) in children. Cochrane Database Syst. Rev. 2023, 2023, CD015252. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Shan, Y.; Wang, S.; Cai, C.; Zhang, H. Endoscopic assisted adenoidectomy versus conventional curettage adenoidectomy: A meta-analysis of randomized controlled trials. SpringerPlus 2016, 5, 426. [Google Scholar] [CrossRef] [PubMed]
- Ravishakar, C.; Killera, S. Comparing endoscopic microdebrider assisted adenoidectomy with curettage procedure. Int. J. Otorhinolaryngol. Head Neck Surg. 2018, 4, 559–562. [Google Scholar] [CrossRef]
- Elsherif, A.; Raaof, A.M.N.A.; Issa, S.H. Comparative study of adenoidectomy by endoscopic transoral suction coagulation versus the traditional method. Egypt. J. Hosp. Med. 2020, 81, 2405–2409. [Google Scholar] [CrossRef]

| Variables | N (%) |
|---|---|
| Patient History | |
| Nasal Obstruction | 178 (100%) |
| Otalgia | 28 (15.7%) |
| Rhinorrhea | 86 (48.3%) |
| Nasal Tone | 122 (68.5%) |
| Postnasal Discharge | 98 (55.1%) |
| History of Adenotonsillectomy | 84 (47.2%) |
| Nasal Obstruction | 178 (100%) |
| Otalgia | 28 (15.7%) |
| Rhinorrhea | 86 (48.3%) |
| Nasal Tone | 122 (68.5%) |
| Comorbidities | |
| Secretory Otitis Media | 34 (19.1%) |
| Chronic Suppurative Otitis Media | 4 (2.2%) |
| Total Patients | 178 (100%) |
| Variables | N (%) |
|---|---|
| Adenoid Tissue Surface | |
| Smooth | 74 (41.6%) |
| Uneven | 104 (58.4%) |
| Parikh Grading Scale | |
| Grade 3 | 54 (30.3%) |
| Grade 4 | 124 (69.7%) |
| Intraoperative Detail | |
| Endoscopic Clearance from Hidden Areas 1 After Conventional Adenoidectomy | 110 (61.8%) |
| Soft Palate Elevation | 178 (100%) |
| Postoperative Complications | |
| Bleeding | 6 (3.4%) |
| Otalgia | 18 (10.1%) |
| Postoperative Nasal Obstruction | 0 (0%) |
| Recurrence of Adenoid Tissue | 0 (0%) |
| Total Patients | 178 (100%) |
| Group 1 | Group 2 | Group 3 | Group 4 | p-Value | ||
|---|---|---|---|---|---|---|
| Endoscopic Clearance from Hidden Areas 1 After Conventional Adenoidectomy | Yes | 10 (9.1%) | 26 (23.6%) | 34 (30.9%) | 40 (36.4%) | <0.001 |
| No | 30 (44.1%) | 14 (20.6%) | 4 (5.9%) | 20 (29.4%) | ||
| Postoperative Complications | None | 24 (15.6%) | 36 (23.4%) | 60 (38.9%) | 34 (22.1%) | <0.001 |
| Bleeding | 6 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Otalgia | 10 (55.6%) | 4 (22.2%) | 0 (0%) | 4 (22.2%) | ||
| Adenoid Tissue Surface | Smooth | 26 (35.1%) | 16 (21.6%) | 32 (21.6%) | 0 (43.3%) | <0.001 |
| Uneven | 14 (13.5%) | 24 (23.1%) | 28 (26.9%) | 38 (36.5%) | ||
| Postoperative Complication | p-Value | ||||
|---|---|---|---|---|---|
| No Complications | Bleeding | Otalgia | |||
| Parikh Grading Scale | Grade 3 | 48 (31.2%) | 4 (66.7%) | 2 (11.1%) | 0.031 |
| Grade 4 | 106 (68.8%) | 2 (33.3%) | 16 (88.9%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Omer, G.L.; Abdullah, A.S.; Ali, S.S.; Di Girolamo, S.; Viola, S.; Bravetti, A.; Maglie, M.G.; Maurantonio, S.; Borghesi, L.; Ahmed, O.H.; et al. Residual Adenoid Tissue After Conventional Adenoidectomy and the Role of Intraoperative Nasal Endoscopy: A Prospective Cohort Study. Children 2025, 12, 1393. https://doi.org/10.3390/children12101393
Omer GL, Abdullah AS, Ali SS, Di Girolamo S, Viola S, Bravetti A, Maglie MG, Maurantonio S, Borghesi L, Ahmed OH, et al. Residual Adenoid Tissue After Conventional Adenoidectomy and the Role of Intraoperative Nasal Endoscopy: A Prospective Cohort Study. Children. 2025; 12(10):1393. https://doi.org/10.3390/children12101393
Chicago/Turabian StyleOmer, Goran Latif, Aland Salih Abdullah, Sahand Soran Ali, Stefano Di Girolamo, Sveva Viola, Andrea Bravetti, Maria Grazia Maglie, Sara Maurantonio, Laura Borghesi, Othman Hussein Ahmed, and et al. 2025. "Residual Adenoid Tissue After Conventional Adenoidectomy and the Role of Intraoperative Nasal Endoscopy: A Prospective Cohort Study" Children 12, no. 10: 1393. https://doi.org/10.3390/children12101393
APA StyleOmer, G. L., Abdullah, A. S., Ali, S. S., Di Girolamo, S., Viola, S., Bravetti, A., Maglie, M. G., Maurantonio, S., Borghesi, L., Ahmed, O. H., Ahmed, A. K., Hamaamin, A. H., Othman, H. H., & De Donato, G. (2025). Residual Adenoid Tissue After Conventional Adenoidectomy and the Role of Intraoperative Nasal Endoscopy: A Prospective Cohort Study. Children, 12(10), 1393. https://doi.org/10.3390/children12101393






