Child Stunting and Temperature Anomalies: A Cross-Sectional Study in Burkina Faso and Kenya
Abstract
1. Introduction
1.1. Previous Research
1.1.1. Heat
1.1.2. Cold
2. Materials and Methods
2.1. Data
2.2. Methods
2.3. Model Specification
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Clarke, B.; Otto, F.; Stuart-Smith, R.; Harrington, L. Extreme Weather Impacts of Climate Change: An Attribution Perspective. Environ. Res. Clim. 2022, 1, 012001. [Google Scholar] [CrossRef]
- Barry, A.A.; Caesar, J.; Klein Tank, A.M.G.; Aguilar, E.; McSweeney, C.; Cyrille, A.M.; Nikiema, M.P.; Narcisse, K.B.; Sima, F.; Stafford, G.; et al. West Africa Climate Extremes and Climate Change Indices: WEST AFRICA CLIMATE EXTREMES. Int. J. Climatol. 2018, 38, e921–e938. [Google Scholar] [CrossRef]
- Ofori, S.A.; Cobbina, S.J.; Obiri, S. Climate Change, Land, Water, and Food Security: Perspectives from Sub-Saharan Africa. Front. Sustain. Food Syst. 2021, 5, 680924. [Google Scholar] [CrossRef]
- Choi, Y.-W.; Campbell, D.J.; Eltahir, E.A.B. Near-Term Regional Climate Change in East Africa. Clim. Dyn. 2023, 61, 961–978. [Google Scholar] [CrossRef]
- Haile, G.G.; Tang, Q.; Sun, S.; Huang, Z.; Zhang, X.; Liu, X. Droughts in East Africa: Causes, impacts and resilience. Earth-Sci. Rev. 2019, 193, 146–161. [Google Scholar] [CrossRef]
- Phalkey, R.K.; Aranda-Jan, C.; Marx, S.; Höfle, B.; Sauerborn, R. Systematic Review of Current Efforts to Quantify the Impacts of Climate Change on Undernutrition. Proc. Natl. Acad. Sci. USA 2015, 112, E4522–E4529. [Google Scholar] [CrossRef] [PubMed]
- Ebi, K.L. Healthy People 2100: Modeling Population Health Impacts of Climate Change. Clim. Chang. 2008, 88, 5–19. [Google Scholar] [CrossRef]
- Cusick, S.E.; Georgieff, M.K. The Role of Nutrition in Brain Development: The Golden Opportunity of the ‘First 1000 Days’. J. Pediatr. 2016, 175, 16–21. [Google Scholar] [CrossRef] [PubMed]
- de Onis, M.; Branca, F. Childhood Stunting: A Global Perspective. Matern. Child Nutr. 2016, 12 (Suppl. S1), 12–26. [Google Scholar] [CrossRef]
- Duggan, M.B. Anthropometry as a Tool for Measuring Malnutrition: Impact of the New WHO Growth Standards and Reference. Ann. Trop. Paediatr. 2010, 30, 1–17. [Google Scholar] [CrossRef]
- Webb, P.; Danaei, G.; Masters, W.A.; Rosettie, K.L.; Leech, A.A.; Cohen, J.; Blakstad, M.; Kranz, S.; Mozaffarian, D. Global Nutrition and Policy Consortium Modelling the Potential Cost-Effectiveness of Food-Based Programs to Reduce Malnutrition. Glob. Food Secur. 2021, 29, 100550. [Google Scholar] [CrossRef]
- Bunyavanich, S.; Landrigan, C.P.; McMichael, A.J.; Epstein, P.R. The Impact of Climate Change on Child Health. Ambul. Pediatr. 2003, 3, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Cuartas, J.; McCoy, D.C.; Torres, I.; Burghardt, L.; Shonkoff, J.P.; Yoshikawa, H. The Developmental Consequences of Early Exposure to Climate Change-related Risks. Child Dev. Perspect. 2024, 18, 145–154. [Google Scholar] [CrossRef]
- Janssen, H.; Ford, K.; Gascoyne, B.; Hill, R.; Roberts, M.; Bellis, M.A.; Azam, S. Cold Indoor Temperatures and Their Association with Health and Well-Being: A Systematic Literature Review. Public Health 2023, 224, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Advice, P.C. Cold Temperature Exposure. Pediatr. Patient Educ. 2024. [Google Scholar] [CrossRef]
- Bytomski, J.R.; Squire, D.L. Heat Illness in Children. Curr. Sports Med. Rep. 2003, 2, 320–324. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, S.; Wang, C.; Wang, B.; Guo, P. Effects of Moderate Strength Cold Air Exposure on Blood Pressure and Biochemical Indicators among Cardiovascular and Cerebrovascular Patients. Int. J. Environ. Res. Public Health 2014, 11, 2472–2487. [Google Scholar] [CrossRef]
- Thiede, B.C.; Strube, J. Climate Variability and Child Nutrition: Findings from Sub-Saharan Africa. Glob. Environ. Chang. 2020, 65, 102192. [Google Scholar] [CrossRef]
- Caminade, C.; Jones, A.E. Malaria in a Warmer West Africa. Nat. Clim. Chang. 2016, 6, 984–985. [Google Scholar] [CrossRef]
- Rossati, A. Global Warming and Its Health Impact. Int. J. Occup. Environ. Med. 2017, 8, 7–20. [Google Scholar] [CrossRef]
- Moore, T.R.; Matthews, H.D.; Simmons, C.; Leduc, M. Quantifying Changes in Extreme Weather Events in Response to Warmer Global Temperature. Atmosphere-Ocean 2015, 53, 412–425. [Google Scholar] [CrossRef]
- Mueller, V.; Gray, C. Heat and Adult Health in China. Popul. Environ. 2018, 40, 1–26. [Google Scholar] [CrossRef]
- Nelson, G.C.; Vanos, J.; Havenith, G.; Jay, O.; Ebi, K.L.; Hijmans, R.J. Global Reductions in Manual Agricultural Work Capacity due to Climate Change. Glob. Change Biol. 2024, 30, e17142. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, S.; Robinson, E.J.Z. Climate, Weather and Child Health in Burkina Faso. Aust. J. Agric. Resour. Econ. 2023, 67, 576–602. [Google Scholar] [CrossRef]
- Grace, K.; Verdin, A.; Brown, M.; Bakhtsiyarava, M.; Backer, D.; Billing, T. Conflict and Climate Factors and the Risk of Child Acute Malnutrition Among Children Aged 24–59 Months: A Comparative Analysis of Kenya, Nigeria, and Uganda. Spat. Demogr. 2022, 10, 329–358. [Google Scholar] [CrossRef]
- Grace, K.; Davenport, F.; Funk, C.; Lerner, A.M. Child Malnutrition and Climate in Sub-Saharan Africa: An Analysis of Recent Trends in Kenya. Appl. Geogr. 2012, 35, 405–413. [Google Scholar] [CrossRef]
- Food Security Information Network (FSIN); Global Network Against Food Crises (GNAFC). Global Report on Food Crisis 2025. FSIN/GNAC: 2025. Available online: https://www.fsinplatform.org/report/global-report-food-crises-2025/ (accessed on 3 October 2025).
- Agostoni, C.; Baglioni, M.; La Vecchia, A.; Molari, G.; Berti, C. Interlinkages between Climate Change and Food Systems: The Impact on Child Malnutrition-Narrative Review. Nutrients 2023, 15, 416. [Google Scholar] [CrossRef]
- van der Merwe, E.; Clance, M.; Yitbarek, E. Climate Change and Child Malnutrition: A Nigerian Perspective. Food Policy 2022, 113, 102281. [Google Scholar] [CrossRef]
- Brown, M.E.; Backer, D.; Billing, T.; White, P.; Grace, K.; Doocy, S.; Huth, P. Empirical Studies of Factors Associated with Child Malnutrition: Highlighting the Evidence about Climate and Conflict Shocks. Food Secur. 2020, 12, 1241–1252. [Google Scholar] [CrossRef]
- Azan, A.; Nyimbili, S.; Babayode, O.O.; Bershteyn, A. Exceeding the Limits of Paediatric Heat Stress Tolerance: The Risk of Losing a Generation to Climate Inaction. BMJ Paediatr. Open 2025, 9, e002883. [Google Scholar] [CrossRef]
- Wheeler, T.; von Braun, J. Climate Change Impacts on Global Food Security. Science 2013, 341, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Tusting, L.S.; Gething, P.W.; Gibson, H.S.; Greenwood, B.; Knudsen, J.; Lindsay, S.W.; Bhatt, S. Housing and Child Health in Sub-Saharan Africa: A Cross-Sectional Analysis. PLoS Med. 2020, 17, e1003055. [Google Scholar] [CrossRef]
- Tusting, L.S.; Bradley, J.; Bhatt, S.; Gibson, H.S.; Weiss, D.J.; Shenton, F.C.; Lindsay, S.W. Environmental Temperature and Growth Faltering in African Children: A Cross-Sectional Study. Lancet Planet. Health 2020, 4, e116–e123. [Google Scholar] [CrossRef]
- Mackay, A. Climate Change 2007: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. J. Environ. Qual. 2008, 37, 2407. [Google Scholar] [CrossRef]
- Davenport, F.; Grace, K.; Funk, C.; Shukla, S. Child Health Outcomes in Sub-Saharan Africa: A Comparison of Changes in Climate and Socio-Economic Factors. Glob. Environ. Chang. 2017, 46, 72–87. [Google Scholar] [CrossRef]
- Klapka, C.S.; Barbosa, B.B.; Magalhães, A.R.; Carioca, A.A.F.; Lourenço, B.H.; Gomes, S.M.; Martins de Carvalho, A. Exploring the Effects of Climate Change on Child Malnutrition: Protocol for a Scoping Review. BMJ Open 2024, 14, e090285. [Google Scholar] [CrossRef]
- Mulondo, M.; Hege, A.; Tsoka-Gwegweni, J.; Ndirangu, J. Effect of Climate Change on the Health and Nutritional Status of Children and Their Families in Africa: Scoping Review. PLoS Glob. Public Health 2025, 5, e0004897. [Google Scholar] [CrossRef]
- Schilling, J.; Hertig, E.; Tramblay, Y.; Scheffran, J. Climate Change Vulnerability, Water Resources and Social Implications in North Africa. Reg. Environ. Chang. 2020, 20, 15. [Google Scholar] [CrossRef]
- Haile, G.G.; Tang, Q.; Hosseini-Moghari, S.-M.; Liu, X.; Gebremicael, T.G.; Leng, G.; Kebede, A.; Xu, X.; Yun, X. Projected Impacts of Climate Change on Drought Patterns Over East Africa. Earth’s Future 2020, 8, e2020EF001502. [Google Scholar] [CrossRef]
- Conte Keivabu, R.; Cozzani, M. Extreme Heat, Birth Outcomes, and Socioeconomic Heterogeneity. Demography 2022, 59, 1631–1654. [Google Scholar] [CrossRef]
- Chambers, J. Global and Cross-Country Analysis of Exposure of Vulnerable Populations to Heatwaves from 1980 to 2018. Clim. Chang. 2020, 163, 539–558. [Google Scholar] [CrossRef]
- IPCC. Global Warming of 1.5 °C; Cambridge University Press: Cambridge, UK, 2022; ISBN 9781009157957. [Google Scholar]
- Harrington, L.J.; Frame, D.J.; Fischer, E.M.; Hawkins, E.; Joshi, M.; Jones, C.D. Poorest Countries Experience Earlier Anthropogenic Emergence of Daily Temperature Extremes. Environ. Res. Lett. 2016, 11, 055007. [Google Scholar] [CrossRef]
- Herold, N.; Alexander, L.; Green, D.; Donat, M. Greater Increases in Temperature Extremes in Low versus High Income Countries. Environ. Res. Lett. 2017, 12, 034007. [Google Scholar] [CrossRef]
- Worku, M.G.; Mohanty, I.; Mengesha, Z.; Niyonsenga, T. Risk Factors of Standalone and Coexisting Forms of Undernutrition among Children in Sub-Saharan Africa: A Study Using Data from 26 Country-Based Demographic and Health Surveys. Nutrients 2025, 17, 252. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, Q.; Ge, Y.; Du, X.; Wang, H. Growing Prevalence of Heat over Cold Extremes with Overall Milder Extremes and Multiple Successive Events. Commun. Earth Environ. 2022, 3, 73. [Google Scholar] [CrossRef]
- Vizy, E.K.; Cook, K.H. Mid-Twenty-First-Century Changes in Extreme Events over Northern and Tropical Africa. J. Clim. 2012, 25, 5748–5767. [Google Scholar] [CrossRef]
- Walt, A.J.; Fitchett, J.M. Trend Analysis of Cold Extremes in South Africa: 1960–2016. Int. J. Climatol. 2021, 41, 2060–2081. [Google Scholar] [CrossRef]
- Chikoore, H.; Mbokodo, I.L.; Singo, M.V.; Mohomi, T.; Munyai, R.B.; Havenga, H.; Mahlobo, D.D.; Engelbrecht, F.A.; Bopape, M.-J.M.; Ndarana, T. Dynamics of an Extreme Low Temperature Event over South Africa amid a Warming Climate. Weather Clim. Extrem. 2024, 44, 100668. [Google Scholar] [CrossRef]
- Crossett, C.C.; Metz, N.D. A Climatological Study of Extreme Cold Surges along the African Highlands. J. Appl. Meteorol. Climatol. 2017, 56, 1731–1738. [Google Scholar] [CrossRef]
- Hongoli, J.J.; Hahn, Y. Early Life Exposure to Cold Weather Shocks and Growth Stunting: Evidence from Tanzania. Health Econ. 2023, 32, 2855–2879. [Google Scholar] [CrossRef]
- Ogasawara, K.; Yumitori, M. Early-Life Exposure to Weather Shocks and Child Height: Evidence from Industrializing Japan. SSM Popul. Health 2019, 7, 100317. [Google Scholar] [CrossRef] [PubMed]
- Seltenrich, N. Between Extremes: Health Effects of Heat and Cold. Environ. Health Perspect. 2015, 123, A275–A280. [Google Scholar] [CrossRef] [PubMed]
- Knbs, I. Kenya Demographic and Health Survey 2022; KNBS: Nairobi, Kenya; ICF: Rockville, MD, USA, 2022; Volume 1. [Google Scholar]
- INSD. Enquête Démographique et de Santé Du Burkina Faso 2021; INSD: Burkina Faso, West Africa, 2021. [Google Scholar]
- Oliveira, A.; Lopes, A.; Correia, E. Annual Summaries Dataset of Heatwaves in Europe, as Defined by the Excess Heat Factor. Data Brief 2022, 44, 108511. [Google Scholar] [CrossRef] [PubMed]
- Cliffer, I.R.; Naumova, E.N.; Masters, W.A.; Perumal, N.; Garanet, F.; Rogers, B.L. Peak Timing of Slowest Growth Velocity among Young Children Coincides with Highest Ambient Temperatures in Burkina Faso: A Longitudinal Study. Am. J. Clin. Nutr. 2024, 119, 393–405. [Google Scholar] [CrossRef]
- Xu, Z.; FitzGerald, G.; Guo, Y.; Jalaludin, B.; Tong, S. Impact of Heatwave on Mortality under Different Heatwave Definitions: A Systematic Review and Meta-Analysis. Environ. Int. 2016, 89–90, 193–203. [Google Scholar] [CrossRef]
- He, Y.-S.; Cao, F.; Hu, X.; Liu, Y.-C.; Tao, S.-S.; Wang, P.; Hou, S.; Pan, H.-F. Time Trends in the Burden of Environmental Heat and Cold Exposure Among Children and Adolescents. JAMA Pediatr. 2025, 179, 55–64. [Google Scholar] [CrossRef]
- Kirina, T.; Supit, I.; Groot, A.; Ludwig, F.; Demissie, T. Projected Climate Change Impacts on Potato Yield in East Africa. Eur. J. Agron. 2025, 166, 127560. [Google Scholar] [CrossRef]
- Berihu, T.; Chen, W.; Wang, L. Unravelling Atmospheric Factors Associated with Long Rain Precipitation Variability in East Africa. Clim. Dyn. 2025, 63, 111. [Google Scholar] [CrossRef]
- Climate Hazards Center. CHIRTS-ERA5. 2025. Available online: https://www.chc.ucsb.edu/data/chirts-era5 (accessed on 3 October 2025).
- Alderman, H.; Headey, D. The Timing of Growth Faltering Has Important Implications for Observational Analyses of the Underlying Determinants of Nutrition Outcomes. PLoS ONE 2018, 13, e0195904. [Google Scholar] [CrossRef]
- Brown, M.E.; Grace, K.; Shively, G.; Johnson, K.B.; Carroll, M. Using Satellite Remote Sensing and Household Survey Data to Assess Human Health and Nutrition Response to Environmental Change. Popul. Environ. 2014, 36, 48–72. [Google Scholar] [CrossRef]
- Gelman, A.; Hill, J. Data Analysis Using Regression and Multilevel/Hierarchical Models; Cambridge University Press: London, UK, 2006. [Google Scholar]
- Grace, K.; Billingsley, S.; Van Riper, D. Building an Interdisciplinary Framework to Advance Conceptual and Technical Aspects of Population-Environment Research Focused on Women’s and Children’s Health. Soc. Sci. Med. 2020, 250, 112857. [Google Scholar] [CrossRef]
- Ryti, N.R.I.; Guo, Y.; Jaakkola, J.J.K. Global Association of Cold Spells and Adverse Health Effects: A Systematic Review and Meta-Analysis. Environ. Health Perspect. 2016, 124, 12–22. [Google Scholar] [CrossRef]
- Millogo, O.; Doamba, J.E.O.; Sié, A.; Utzinger, J.; Vounatsou, P. Geographical Variation in the Association of Child, Maternal and Household Health Interventions with under-Five Mortality in Burkina Faso. PLoS ONE 2019, 14, e0218163. [Google Scholar] [CrossRef]
- Arisco, N.J.; Sewe, M.O.; Bärnighausen, T.; Sié, A.; Zabre, P.; Bunker, A. The Effect of Extreme Temperature and Precipitation on Cause-Specific Deaths in Rural Burkina Faso: A Longitudinal Study. Lancet Planet. Health 2023, 7, e478–e489. [Google Scholar] [CrossRef] [PubMed]
- Skoufias, E.; Vinha, K. Climate Variability and Child Height in Rural Mexico. Econ. Hum. Biol. 2012, 10, 54–73. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.; Brown, M.E. Environmental Risk Factors and Child Nutritional Status and Survival in a Context of Climate Variability and Change. Appl. Geogr. 2014, 54, 209–221. [Google Scholar] [CrossRef]
- Bakhtsiyarava, M.; Grace, K.; Nawrotzki, R.J. Climate, Birth Weight, and Agricultural Livelihoods in Kenya and Mali. Am. J. Public Health 2018, 108, S144–S150. [Google Scholar] [CrossRef]
- Patlán-Hernández, A.R.; Stobaugh, H.C.; Cumming, O.; Angioletti, A.; Pantchova, D.; Lapègue, J.; Stern, S.; N’Diaye, D.S. Water, Sanitation and Hygiene Interventions and the Prevention and Treatment of Childhood Acute Malnutrition: A Systematic Review. Matern. Child Nutr. 2022, 18, e13257. [Google Scholar] [CrossRef]
- van Cooten, M.H.; Bilal, S.M.; Gebremedhin, S.; Spigt, M. The Association between Acute Malnutrition and Water, Sanitation, and Hygiene among Children Aged 6–59 Months in Rural Ethiopia. Matern. Child Nutr. 2019, 15, e12631. [Google Scholar] [CrossRef]
- Ajide, K.B.; Dauda, R.O.; Alimi, O.Y. Electricity Access, Institutional Infrastructure and Health Outcomes in Africa. Environ. Dev. Sustain. 2022, 25, 198–227. [Google Scholar] [CrossRef]
- Fotso, J.-C. Child Health Inequities in Developing Countries: Differences across Urban and Rural Areas. Int. J. Equity Health 2006, 5, 9. [Google Scholar] [CrossRef]
- Shon, H. Urbanicity and Child Health in 26 Sub-Saharan African Countries: Settlement Type and Its Association with Mortality and Morbidity. Soc. Sci. Med. 2024, 340, 116401. [Google Scholar] [CrossRef]
- Picbougoum, T.B.; Somda, M.A.S.; Zango, S.H.; Lohmann, J.; De Allegri, M.; Saidou, H.; Hien, H.; Meda, N.; Robert, A. Nutritional Status of Children under Five Years and Associated Factors in 24 Districts of Burkina Faso. PLoS Glob. Public Health 2023, 3, e0001248. [Google Scholar] [CrossRef] [PubMed]
- Yaya, S.; Odusina, E.K.; Uthman, O.A.; Bishwajit, G. What Does Women’s Empowerment Have to Do with Malnutrition in Sub-Saharan Africa? Evidence from Demographic and Health Surveys from 30 Countries. Glob. Health Res. Policy 2020, 5, 1. [Google Scholar] [CrossRef] [PubMed]
- Żywiec, J.; Szpak, D.; Wartalska, K.; Grzegorzek, M. The Impact of Climate Change on the Failure of Water Supply Infrastructure: A Bibliometric Analysis of the Current State of Knowledge. Water 2024, 16, 1043. [Google Scholar] [CrossRef]
- Kong, J.; Gao, M.; Liu, X.; Haroon, M. Analysis of Correlation between Climate Change and Energy Poverty: A Panel Data Analysis. Energy 2025, 322, 135247. [Google Scholar] [CrossRef]
- Ameye, H.; De Weerdt, J. Child Health across the Rural–urban Spectrum. World Dev. 2020, 130, 104950. [Google Scholar] [CrossRef]
- Karmaker, S.C.; Sen, K.K.; Singha, B.; Hosan, S.; Chapman, A.J.; Saha, B.B. The Mediating Effect of Energy Poverty on Child Development: Empirical Evidence from Energy Poor Countries. Energy 2022, 243, 123093. [Google Scholar] [CrossRef]
- Ang’u, C.; Muthama, N.J.; Mutuku, M.A.; M’IKiugu, M.H. Analysis of Energy Poverty in Kenya and Its Implications for Human Health. Energy Policy 2023, 176, 113506. [Google Scholar] [CrossRef]
- Compaore, E.W.R.; Ouedraogo, O.; Bationo, P.E.; Traore, K.; Birba, E.; Nakelse, P.; Kambou, O.F.; Ouedraogo, B.; Ilboudo, A.A.D.; Tirogo, S.; et al. Determinants of Stunting in Children Aged 0–59 Months in Three Regions of Burkina Faso. BMC Public Health 2024, 24, 2392. [Google Scholar] [CrossRef] [PubMed]
- Cumming, O.; Cairncross, S. Can Water, Sanitation and Hygiene Help Eliminate Stunting? Current Evidence and Policy Implications. Matern. Child Nutr. 2016, 12 (Suppl. S1), 91–105. [Google Scholar] [CrossRef]
- Schapiro, L.H.; McShane, M.A.; Marwah, H.K.; Callaghan, M.E.; Neudecker, M.L. Impact of Extreme Heat and Heatwaves on Children’s Health: A Scoping Review. J. Clim. Chang. Health 2024, 19, 100335. [Google Scholar] [CrossRef]
- Principi, N.; Campana, B.R.; Argentiero, A.; Fainardi, V.; Esposito, S. The Influence of Heat on Pediatric and Perinatal Health: Risks, Evidence, and Future Directions. J. Clin. Med. 2025, 14, 1123. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Sheffield, P.E.; Su, H.; Wang, X.; Bi, Y.; Tong, S. The Impact of Heat Waves on Children’s Health: A Systematic Review. Int. J. Biometeorol. 2014, 58, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Uibel, D.; Sharma, R.; Piontkowski, D.; Sheffield, P.E.; Clougherty, J.E. Association of Ambient Extreme Heat with Pediatric Morbidity: A Scoping Review. Int. J. Biometeorol. 2022, 66, 1683–1698. [Google Scholar] [CrossRef] [PubMed]
- Grace, K. Considering Climate in Studies of Fertility and Reproductive Health in Poor Countries. Nat. Clim. Chang. 2017, 7, 479–485. [Google Scholar] [CrossRef]


| Variable | Definition |
|---|---|
| Child Age (Months) | Age of the child in months at the time of survey. |
| Child Sex | Biological sex of the child (male/female). |
| Electricity Access | The household has access to electricity (binary: yes/no). |
| Maximum Temperature (Tmax) | CHIRTS dataset: Daily maximum temperature, averaged for the exposure window (e.g., 59 months before survey). |
| Minimum Temperature (Tmin) | CHIRTS dataset: Daily minimum temperature, averaged for the exposure window (e.g., 59 months before survey). |
| Residence (Urban) | Urban versus rural place of residence (binary: urban = 1, rural = 0). |
| Sanitation Improved | The household uses an improved sanitation facility per WHO/UNICEF Joint Monitoring Programme definition (binary: yes/no). |
| Water Source | The household uses an improved drinking water source per WHO/UNICEF definition (binary: yes/no). |
| Wealth (Binary) | Household wealth index categorized as high (1) versus low (0) wealth, based on DHS quintiles. |
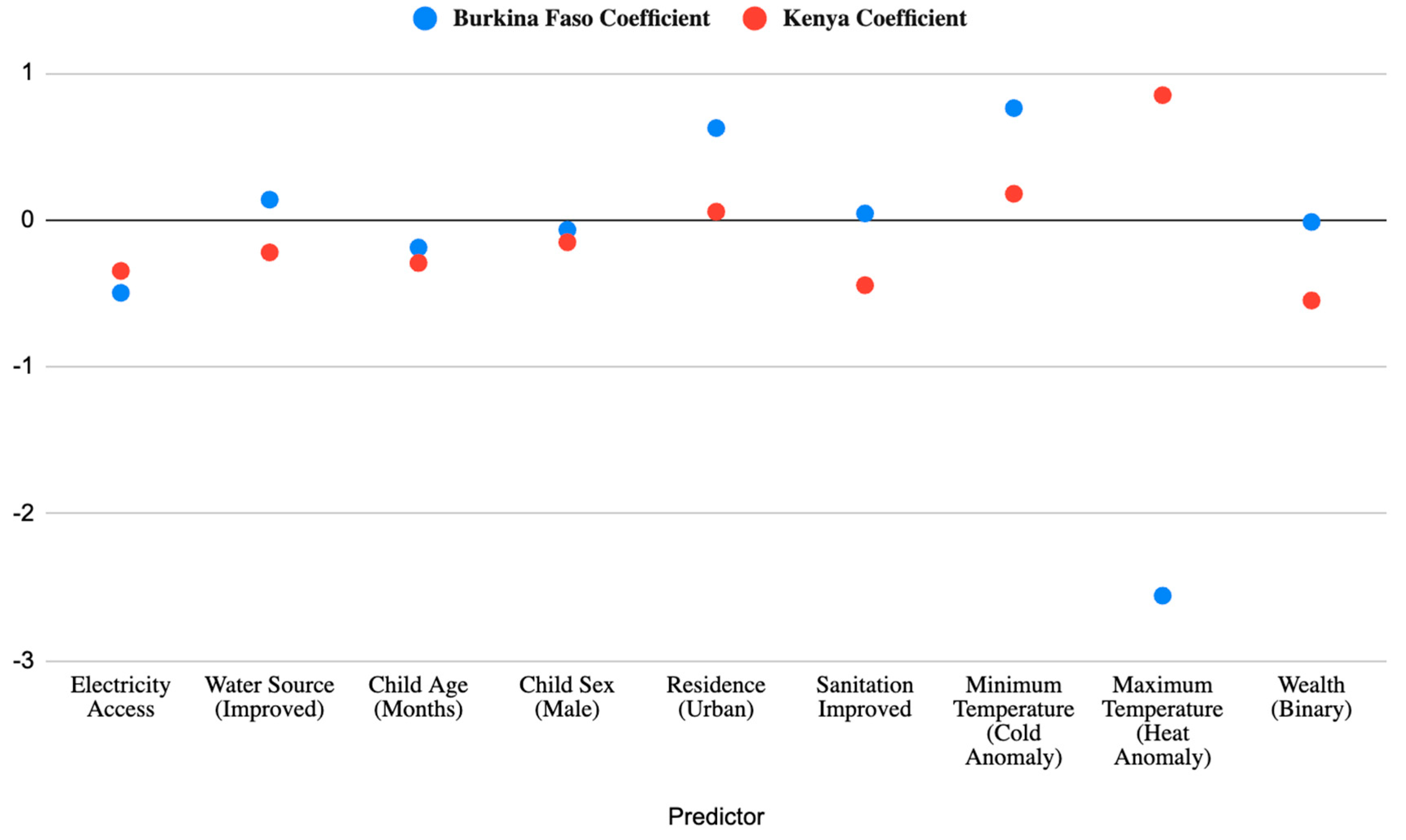
| Predictor | Burkina Faso Coefficient | BF OR | 95% CI (BF) | Kenya Coefficient | Kenya Coefficient | KE OR | 95% CI (KE) |
|---|---|---|---|---|---|---|---|
| Electricity Access | −0.496 * | 0.609 | [0.396, 0.937] | −0.347 *** | −0.347 *** | 0.707 | [0.594, 0.842] |
| Water Source (Improved) | 0.138 | 1.147 | [0.798, 1.648] | −0.221 * | −0.221 * | 0.802 | [0.671, 0.958] |
| Child Age (Months) | −0.188 * | 0.829 | [0.688, 0.999] | −0.293 *** | −0.293 *** | 0.746 | [0.682, 0.815] |
| Child Sex (Male) | −0.067 | 0.935 | [0.701, 1.247] | −0.152 * | −0.152 * | 0.859 | [0.747, 0.988] |
| Residence (Urban) | 0.625 ** | 1.867 | [1.207, 2.887] | 0.056 | 0.056 | 1.057 | [0.888, 1.258] |
| Sanitation Improved | 0.044 | 1.045 | [0.717, 1.524] | −0.444 *** | −0.444 *** | 0.641 | [0.543, 0.758] |
| Minimum Temperature (Cold Anomaly) | 0.761 . | 2.141 | [0.930, 4.925] | 0.178 . | 0.178 . | 1.195 | [0.996, 1.433] |
| Maximum Temperature (Heat Anomaly) | −2.557 * | 0.077 | [0.006, 0.889] | 0.849 *** | 0.849 *** | 2.338 | [1.637, 3.340] |
| Wealth (Binary) | −0.014 | 0.986 | [0.659, 1.473] | −0.548 *** | −0.548 *** | 0.578 | [0.460, 0.726] |
| Country | Random Intercept Variance | AIC | BIC | Log Likelihood | Observations | Clusters |
|---|---|---|---|---|---|---|
| Burkina Faso | ~0 (1.41 × 10−13) | 1242.3 | 1294.6 | –611.1 | 1384 | 380 |
| Kenya | 0.1199 | 5035.2 | 5100.5 | –2507.6 | 5097 | 1523 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mansfield, T.C.; Brown, M.E.; Gore, M.L. Child Stunting and Temperature Anomalies: A Cross-Sectional Study in Burkina Faso and Kenya. Children 2025, 12, 1346. https://doi.org/10.3390/children12101346
Mansfield TC, Brown ME, Gore ML. Child Stunting and Temperature Anomalies: A Cross-Sectional Study in Burkina Faso and Kenya. Children. 2025; 12(10):1346. https://doi.org/10.3390/children12101346
Chicago/Turabian StyleMansfield, Tavis C., Molly E. Brown, and Meredith L. Gore. 2025. "Child Stunting and Temperature Anomalies: A Cross-Sectional Study in Burkina Faso and Kenya" Children 12, no. 10: 1346. https://doi.org/10.3390/children12101346
APA StyleMansfield, T. C., Brown, M. E., & Gore, M. L. (2025). Child Stunting and Temperature Anomalies: A Cross-Sectional Study in Burkina Faso and Kenya. Children, 12(10), 1346. https://doi.org/10.3390/children12101346






