Management Patterns of Croup in Korean Emergency Departments: A Nationwide Cohort Study
Abstract
Highlights
- Despite guideline recommendations, only around half of children with croup in Korean emergency departments received corticosteroids.
- Dedicated pediatric emergency centers (DPECs) were associated with lower use of potentially low-value interventions (salbutamol and chest and cervical radiography) than general emergency centers (GECs).
- Education and implementation of standardized national clinical guidelines are needed to optimize croup management in Korean emergency departments.
Abstract
1. Background
2. Methods
2.1. Study Setting and Data Sources
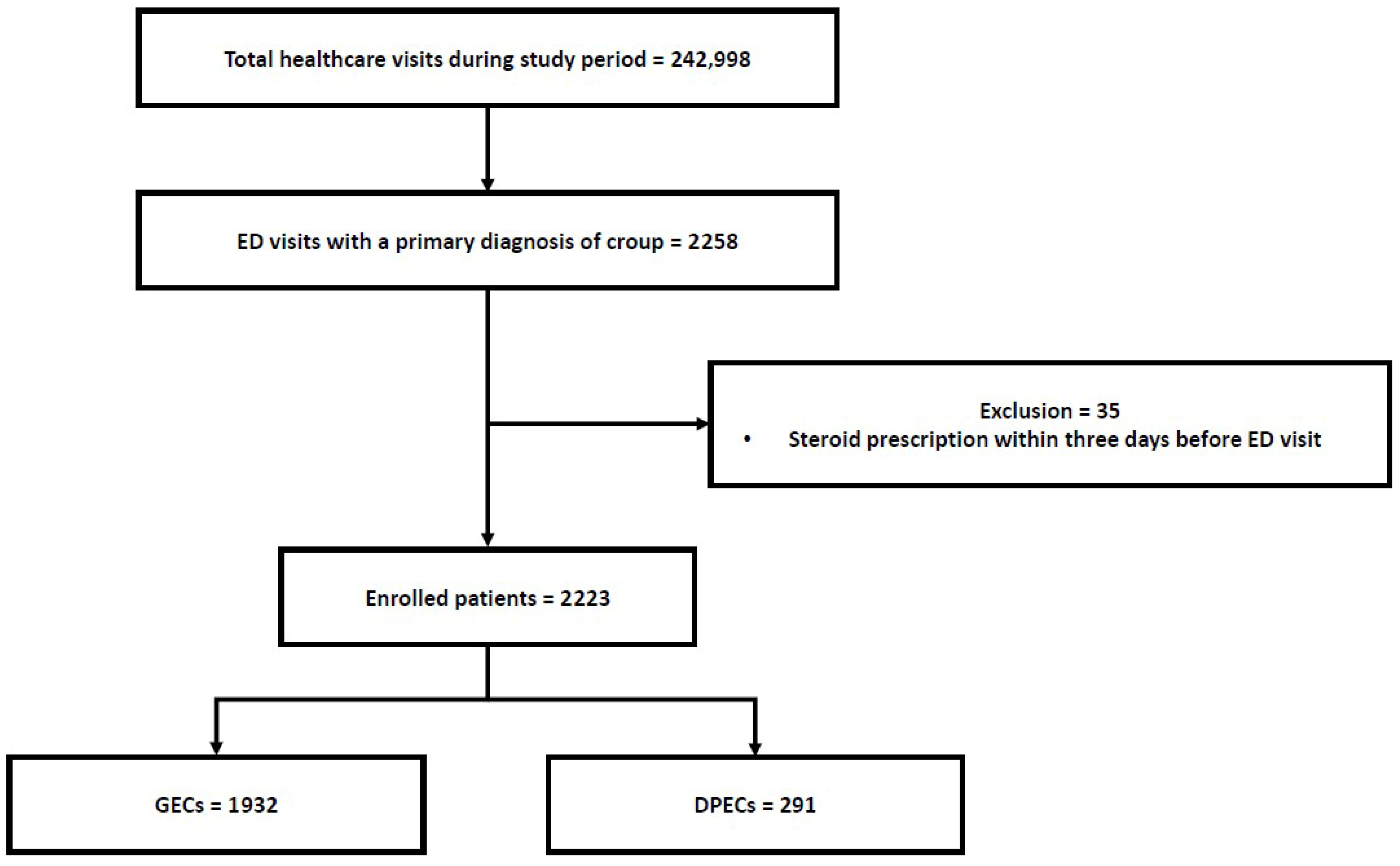
2.2. Study Population
2.3. Dedicated Pediatric Emergency Centers (DPECs) in Korea
2.4. Variables and Measurement
2.5. Outcomes
2.6. Statistical Analysis
2.7. Ethics
3. Results
3.1. Characteristics of the Study Population
3.2. Primary Outcome
3.3. Secondary Outcomes

4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DPECs | Dedicated pediatric emergency centers |
| ED | Emergency department |
| GECs | General emergency Centers |
| ICD-10 | The International Classification of Diseases-10 |
| NHAMCS | National Hospital Ambulatory Medical Care Survey |
| NHIS | National Health Insurance Service |
| NHSPIC | The National Health Screening Program for Infants and Children |
References
- Lee, J.K.; Song, S.H.; Ahn, B.; Yun, K.W.; Choi, E.H. Etiology and epidemiology of croup before and throughout the COVID-19 pandemic, 2018–2022, South Korea. Children 2022, 9, 1542. [Google Scholar] [CrossRef]
- Bjornson, C.L.; Johnson, D.W. Croup in children. Can. Med. Assoc. J. 2013, 185, 1317–1323. [Google Scholar] [CrossRef]
- Johnson, D.W. Croup. BMJ Clin. Evid. 2014, 2014, 0321. [Google Scholar] [PubMed]
- Bjornson, C.L.; Johnson, D.W. Croup. Lancet 2008, 371, 329–339. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.R.; Lee, C.H.; Won, Y.K.; Suh, D.I.; Roh, E.-J.; Lee, M.-H.; Chung, E.H. Clinical characteristics of children and adolescents with croup and epiglottitis who visited 146 Emergency Departments in Korea. Korean J. Pediatr. 2015, 58, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.K.; McDermott, A.J.; Sullivan, J.F. Croup: Diagnosis and Management. Am. Fam. Physician 2018, 97, 575–580. [Google Scholar]
- Aregbesola, A.; Tam, C.M.; Kothari, A.; Le, M.-L.; Ragheb, M.; Klassen, T.P. Glucocorticoids for croup in children. Cochrane Database Syst. Rev. 2023, 1, CD001955. [Google Scholar] [CrossRef]
- Jiang, W.; Hall, M.; Berry, J.G. Comparative effectiveness of dexamethasone versus prednisone in children hospitalized with acute croup. Hosp. Pediatr. 2022, 12, 892–898. [Google Scholar] [CrossRef]
- Zoorob, R.; Sidani, M.; Murray, J. Croup: An overview. Am. Fam. Physician 2011, 83, 1067–1073. [Google Scholar]
- Bjornson, C.; Russell, K.; Vandermeer, B.; Durec, T.; Klassen, T.P.; Johnson, D.W. Nebulized epinephrine for croup in children. Cochrane Database Syst. Rev. 2013, 2, CD006619. [Google Scholar] [CrossRef]
- Hampers, L.C.; Faries, S.G. Practice variation in the emergency management of croup. Pediatrics 2002, 109, 505–508. [Google Scholar] [CrossRef]
- Knapp, J.F.; Simon, S.D.; Sharma, V. Quality of care for common pediatric respiratory illnesses in United States emergency departments: Analysis of 2005 National Hospital Ambulatory Medical Care Survey data. Pediatrics 2008, 122, 1165–1170. [Google Scholar] [CrossRef]
- Knapp, J.F.; Simon, S.D.; Sharma, V.M. Does active dissemination of evidence result in faster knowledge transfer than passive diffusion? An analysis of trends in the management of pediatric asthma and croup in US emergency departments from 1995 to 2009. Pediatr. Emerg. Care 2015, 31, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Pierantoni, L.; Stera, G.; Andreozzi, L.; Pellegrino, F.; Dondi, A.; Fabi, M.; Corsini, I.; Ghizzi, C.; Lanari, M. Multicentre study revealed significant gaps between evidence-based recommendations for using corticosteroids for croup and clinical practice. Acta Paediatr. 2022, 111, 2010–2016. [Google Scholar] [CrossRef] [PubMed]
- Michelson, K.A.; Lyons, T.W.; Hudgins, M.D.; Jason, A.; Levy, M.D.; Monuteaux, M.C.; A Finkelstein, J.; Bachur, R.G. Use of a national database to assess pediatric emergency care across United States emergency departments. Acad. Emerg. Med. 2018, 25, 1355–1364. [Google Scholar] [CrossRef]
- Moon, J.S. Review of National Health Screening Program for infants and children in Korea. J. Korean Med. Assoc. 2010, 53, 377–385. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, J.E.; Shim, S.M.; Ha, E.K.; Yon, D.K.; Kim, O.H.; Baek, J.H.; Koh, H.Y.; Chae, K.Y.; Lee, S.W.; et al. Cohort profile: National Investigation of Birth Cohort in Korea study 2008 (NICKs-2008). Clin. Exp. Pediatr. 2021, 64, 480–488. [Google Scholar] [CrossRef]
- Choi, M.J.; Kang, H.; Choi, J. Risk factors for obesity in five-year-old children: Based on Korean National Health Insurance Service data. Children 2022, 9, 314. [Google Scholar] [CrossRef] [PubMed]
- NHIS. National Health Screening Program for Infants and Children. Available online: https://nhiss.nhis.or.kr/bd/ab/bdaba010cv.do (accessed on 3 September 2025).
- Kim, D.K. Regionalization of pediatric emergency care in Korea. Korean J. Pediatr. 2011, 54, 477–480. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Support for Pediatric Emergency Room Construction in 2011, Selection of 4 Medical Institutions: 1 in Seoul, 1 in Incheon, 2 Hospitals in Other Regions; Ministry of Health and Welfare: Seoul, Korea, 2011.
- Korea Ministry of Government Legislation. Enforcement Rule of Emergency Medical Service Act [Internet]; Korea Ministry of Government Legislation: Sejong, Korea, 2025. Available online: http://www.law.go.kr/lumLsLinkPop.do?lspttninfSeq=79689 (accessed on 3 September 2025).
- Kim, E.Y. Policy direction for the development of pediatric emergency care in Korea. Pediatr. Emerg. Med. J. 2023, 10, 1–2. [Google Scholar] [CrossRef]
- Prentice, B.; Moloney, S.; Hort, J.; Hibbert, P.; Wiles, L.K.; Molloy, C.J.; Arnolda, G.; Ting, H.P.; Braithwaite, J.; Jaffe, A. Assessing the adherence to guidelines in the management of croup in Australian children: A population-based sample survey. Int. J. Qual. Health Care 2019, 31, 759–767. [Google Scholar] [CrossRef]
- Yoon, Y.K.; Park, C.-S.; Kim, J.W.; Hwang, K.; Lee, S.Y.; Kim, T.H.; Park, D.-Y.; Kim, H.J.; Kim, D.-Y.; Lee, H.J.; et al. Guidelines for the antibiotic use in adults with acute upper respiratory tract infections. Infect. Chemother. 2017, 49, 326–352. [Google Scholar] [CrossRef] [PubMed]
- Raudasoja, A.J.; Falkenbach, P.; Vernooij, R.W.M.; Mustonen, J.M.J.; Agarwal, A.; Aoki, Y.; Blanker, M.H.; Cartwright, R.; Garcia-Perdomo, H.A.; Kilpeläinen, T.P.; et al. Randomized controlled trials in de-implementation research: A systematic scoping review. Implement. Sci. 2022, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Yeo, C.Y.; Lee, S.U.; Cho, Y.K.; Jung, H.Y.; Ma, J.S. A clinical study on the patients with viral croup. Chonnam Med. J. 2006, 42, 187–191. [Google Scholar]
- Jeon, I.S.; Cho, W.J.; Lee, J.; Kim, H.M. Epidemiology and clinical severity of the hospitalized children with viral croup. Pediatr. Infect. Vaccine 2018, 25, 8–16. [Google Scholar] [CrossRef]
- Chin, R.; Browne, G.; Lam, L.; McCaskill, M.; Fasher, B.; Hort, J. Effectiveness of a croup clinical pathway in the management of children with croup presenting to an emergency department. J. Paediatr. Child Health 2002, 38, 382–387. [Google Scholar] [CrossRef]
- Haskell, L.; Tavender, E.J.; Wilson, C.L.; O’bRien, S.; Babl, F.E.; Borland, M.L.; Cotterell, E.; Schembri, R.; Orsini, F.; Sheridan, N.; et al. Effectiveness of targeted interventions on treatment of infants with bronchiolitis: A randomized clinical trial. JAMA Pediatr. 2021, 175, 797–806. [Google Scholar] [CrossRef]
| Variables | Overall (N = 2223) | GECs (N = 1932) | DPECs (N = 291) | p-Value |
|---|---|---|---|---|
| Gender | 0.098 | |||
| Female | 748 (33.6) | 663 (34.3) | 85 (29.2) | |
| Age group (Year of birth) | 0.009 | |||
| Group 0 (2008) | 105 (4.7) | 102 (5.3) | 4 (1.4) | |
| Group 1 (2009) | 565 (25.4) | 488 (25.3) | 77 (26.5) | |
| Group 2 (2010) | 739 (33.2) | 657 (34.0) | 82 (28.2) | |
| Group 3 (2011) | 463 (20.8) | 388 (20.1) | 75 (25.8) | |
| Group 4 (2012) | 208 (9.4) | 173 (9.0) | 35 (12.0) | |
| Group 5 (2013) | 98 (4.4) | 87 (4.5) | 11 (3.8) | |
| Group 6 (2014) | 36 (1.6) | 31 (1.6) | 5 (1.7) | |
| Group 7 (2015) | 8 (0.4) | 6 (0.3) | 2 (0.7) | |
| Region | 0.002 | |||
| Rural area | 1262 (56.8) | 1122 (58.1) | 140 (48.1) | |
| Type of national health insurance | 0.112 | |||
| Self-employed | 554 (24.9) | 495 (25.6) | 59 (20.3) | |
| Employee | 1597 (71.8) | 1373 (71.1) | 224 (77.0) | |
| Medical aid | 72 (3.2) | 64 (3.3) | 8 (2.7) |
| Variables | Overall (N = 2223) | GECs (N = 1932) | DPECs (N = 291) | Risk difference (95% CI) | p-Value |
|---|---|---|---|---|---|
| Total steroid prescription | 1265 (56.9) | 1087 (56.3) | 178 (61.2) | 4.9% (−3.0–12.5) | 0.131 |
| Nebulizer | |||||
| Epinephrine nebulizer | 113 (5.1) | 93 (4.8) | 20 (6.9) | 2.1% (−1.4–6.4) | 0.178 |
| Salbutamol nebulizer | 258 (11.6) | 245 (12.7) | 13 (4.5) | −8.2% (−11.6–−3.8) | <0.001 |
| Radiographs | |||||
| Chest radiographs | 1710 (76.9) | 1520 (78.7) | 190 (65.3) | −13.4% (−20.8–−6.3) | <0.001 |
| Cervical spine radiographs | 257 (11.6) | 244 (12.6) | 13 (4.5) | −8.2% (−11.6–−3.7) | <0.001 |
| Sub-diagnosis respiratory disease | 0.346 | ||||
| Viral pneumonia (J12) | 1 (0.0) | 1 (0.1) | 0 (0.0) | −0.1% (−0.3–1.3) | |
| Bacterial pneumonia (J15) | 3 (0.1) | 3 (0.2) | 0 (0.0) | −0.2% (−0.5–1.3) | |
| Pneumonia, unspecified (J18) | 104 (4.7) | 97 (5.0) | 7 (2.4) | −2.6% (−4.9–0.7) | |
| Acute bronchitis (J20) | 302 (13.6) | 260 (13.5) | 42 (14.4) | 1.0% (−4.2–6.9) | |
| Acute bronchiolitis (J21) | 180 (8.1) | 152 (7.9) | 28 (9.6) | 1.8% (−2.4–6.8) | |
| Acute lower respiratory infection, unspecified (J22) | 1 (0.0) | 1 (0.1) | 0 (0.0) | −0.1% (−0.3–1.3) | |
| No sub-diagnosis | 1632 (73.4) | 1418 (73.4) | 214 (73.5) | 0.1% (−7.1–6.9) | |
| Physician’s specialty | 0.950 | ||||
| Emergency medicine | 1152 (51.8) | 1003 (51.9) | 149 (51.2) | −0.7% (−8.7–7.2) | |
| Pediatrics | 1064 (47.9) | 922 (47.7) | 142 (48.8) | 1.1% (−6.8–9.0) | |
| Surgery | 4 (0.2) | 4 (0.2) | 0 (0.0) | −0.2% (−0.5–1.2) | |
| Internal medicine | 1 (0.0) | 1 (0.1) | 0 (0.0) | −0.1% (−0.3–1.3) | |
| Otolaryngology | 1 (0.0) | 1 (0.1) | 0 (0.0) | −0.1% (−0.3–1.3) | |
| Family medicine | 1 (0.0) | 1 (0.1) | 0 (0.0) | −0.1% (−0.3–1.3) | |
| ED outcome | |||||
| Discharge (ED stay < 6 h) | 1563 (70.3) | 1315 (68.1) | 248 (85.2) | 17.2% (10.6–22.9) | <0.001 |
| Variables | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Overall | ED visits (N = 2223) | 16 | 74 | 264 | 270 | 486 | 483 | 411 | 219 | |
| Total steroid prescription | 9 (56.2) | 37 (50.0) | 132 (50.0) | 140 (51.9) | 286 (58.8) | 290 (60.0) | 239 (58.2) | 132 (60.3) | 0.064 | |
| Dexamethasone | 7 (43.8) | 35 (47.3) | 105 (39.8) | 124 (45.9) | 241 (49.6) | 227 (47.0) | 191 (46.5) | 114 (52.1) | 0.230 | |
| Epinephrine nebulizer | 1 (6.2) | 5 (6.8) | 10 (3.8) | 9 (3.3) | 14 (2.9) | 33 (6.8) | 23 (5.6) | 18 (8.2) | 0.028 | |
| Salbutamol nebulizer | 2 (12.5) | 10 (13.5) | 33 (12.5) | 45 (16.7) | 65 (13.4) | 35 (7.2) | 44 (10.7) | 24 (11.0) | 0.012 | |
| Chest radiography | 14 (87.5) | 72 (97.3) | 223 (84.5) | 222 (82.2) | 394 (81.1) | 367 (76.0) | 277 (67.4) | 141 (64.4) | <0.001 | |
| Cervical spine radiography | 4 (25.0) | 15 (20.3) | 27 (10.2) | 37 (13.7) | 53 (10.9) | 56 (11.6) | 52 (12.7) | 13 (5.9) | 0.015 | |
| GECs | ED visits (N = 1932) | 16 | 74 | 264 | 236 | 416 | 399 | 338 | 189 | |
| Total steroid prescription | 9 (56.2) | 37 (50.0) | 132 (50.0) | 120 (50.8) | 240 (57.7) | 243 (60.9) | 196 (58.0) | 110 (58.2) | 0.079 | |
| Dexamethasone | 7 (43.8) | 35 (47.3) | 105 (39.8) | 109 (46.2) | 204 (49.0) | 185 (46.4) | 153 (45.3) | 95 (50.3) | 0.409 | |
| Epinephrine nebulizer | 1 (6.2) | 5 (6.8) | 10 (3.8) | 8 (3.4) | 10 (2.4) | 22 (5.5) | 21 (6.2) | 16 (8.5) | 0.036 | |
| Salbutamol nebulizer | 2 (12.5) | 10 (13.5) | 33 (12.5) | 44 (18.6) | 62 (14.9) | 32 (8.0) | 40 (11.8) | 22 (11.6) | 0.013 | |
| Chest radiography | 14 (87.5) | 72 (97.3) | 223 (84.5) | 191 (80.9) | 345 (82.9) | 308 (77.2) | 240 (71.0) | 127(67.2) | <0.001 | |
| Cervical spine radiography | 4 (25.0) | 15 (20.3) | 27 (10.2) | 36 (15.3) | 51 (12.3) | 53 (13.3) | 46 (13.6) | 12 (6.3) | 0.023 | |
| DPECs | ED visits (N = 291) | N/A | N/A | N/A | 34 | 70 | 84 | 73 | 30 | |
| Total steroid prescription | N/A | N/A | N/A | 20 (58.8) | 46 (65.7) | 47 (56.0) | 43 (58.9) | 22 (73.3) | 0.452 | |
| Dexamethasone | N/A | N/A | N/A | 15 (44.1) | 37 (52.9) | 42 (50.0) | 38 (52.1) | 19 (63.3) | 0.637 | |
| Epinephrine nebulizer | N/A | N/A | N/A | 1 (2.9) | 4 (5.7) | 11 (13.1) | 2 (2.7) | 2 (6.7) | 0.092 | |
| Salbutamol nebulizer | N/A | N/A | N/A | 1 (2.9) | 3 (4.3) | 3 (3.6) | 4 (5.5) | 2 (6.7) | 0.930 | |
| Chest radiography | N/A | N/A | N/A | 31 (91.2) | 49 (70.0) | 59 (70.2) | 37 (50.7) | 14 (46.7) | <0.001 | |
| Cervical spine radiography | N/A | N/A | N/A | 1 (2.9) | 2 (2.9) | 3 (3.6) | 6 (8.2) | 1 (3.3) | 0.514 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.H.; Jung, J.Y.; Hwang, S.; Park, J.W.; Lee, E.J.; Lee, H.N.; Kim, D.K.; Kwak, Y.H. Management Patterns of Croup in Korean Emergency Departments: A Nationwide Cohort Study. Children 2025, 12, 1301. https://doi.org/10.3390/children12101301
Kim JH, Jung JY, Hwang S, Park JW, Lee EJ, Lee HN, Kim DK, Kwak YH. Management Patterns of Croup in Korean Emergency Departments: A Nationwide Cohort Study. Children. 2025; 12(10):1301. https://doi.org/10.3390/children12101301
Chicago/Turabian StyleKim, Jin Hee, Jae Yun Jung, Soyun Hwang, Joong Wan Park, Eui Jun Lee, Ha Ni Lee, Do Kyun Kim, and Young Ho Kwak. 2025. "Management Patterns of Croup in Korean Emergency Departments: A Nationwide Cohort Study" Children 12, no. 10: 1301. https://doi.org/10.3390/children12101301
APA StyleKim, J. H., Jung, J. Y., Hwang, S., Park, J. W., Lee, E. J., Lee, H. N., Kim, D. K., & Kwak, Y. H. (2025). Management Patterns of Croup in Korean Emergency Departments: A Nationwide Cohort Study. Children, 12(10), 1301. https://doi.org/10.3390/children12101301






