Minimal Access in Pediatric Surgery: An Overview on Progress towards Dedicated Instrument Developments and Anesthesiologic Advances to Enhance Safe Completion of Procedures
Abstract
1. Introduction
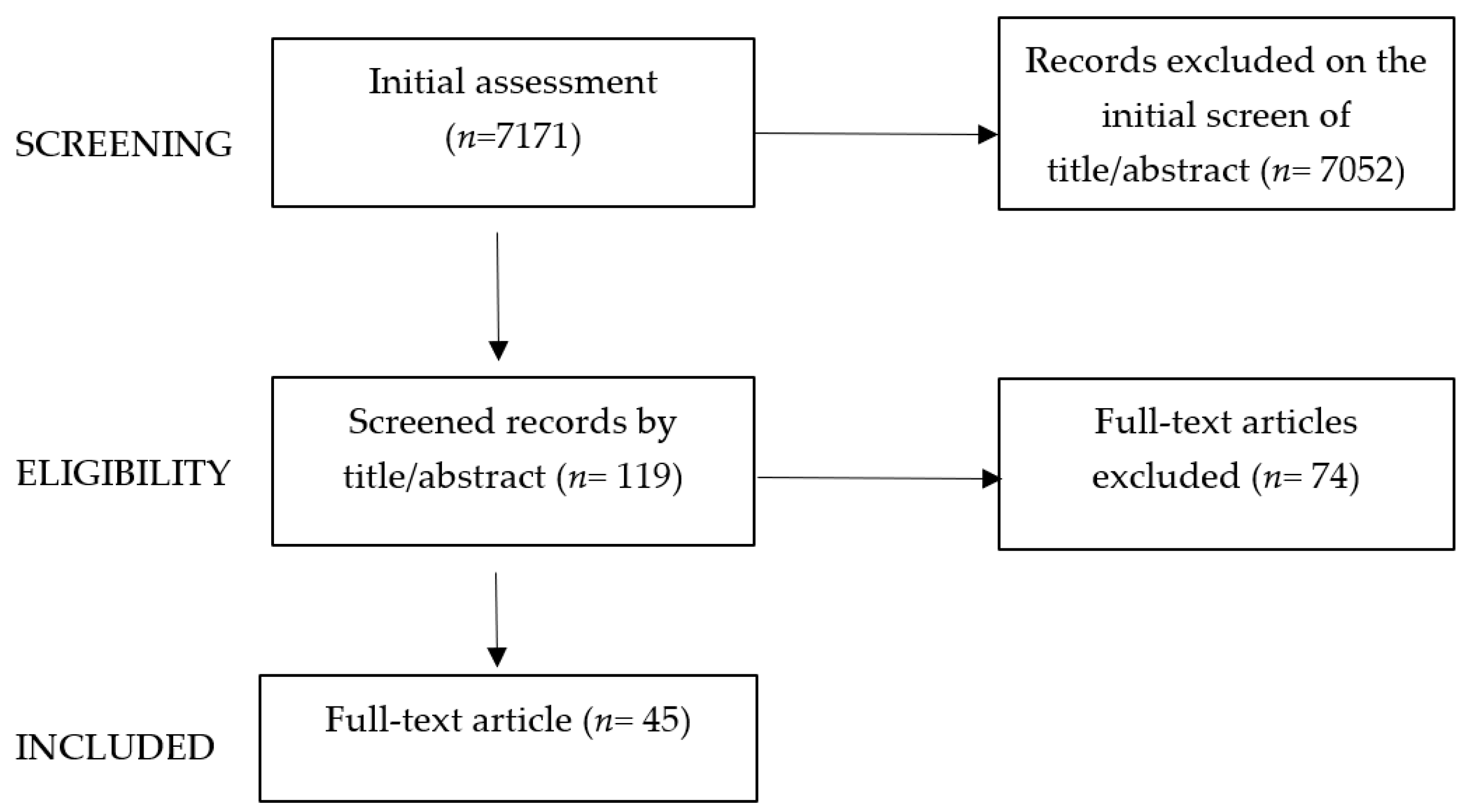
2. Methods
3. Key Content and Findings
4. History of Pediatric MAS: Devices Development
4.1. Visualization and Light-Sourcing [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]
4.2. Access to Cavities (Ports) and Insufflation [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]
5. MAS in Pediatrics: Recent Advancements
5.1. Orphan Pediatric Devices
5.2. Equipment in Pediatric MAS
6. Pediatric Endoscopic Surgery and Robotics
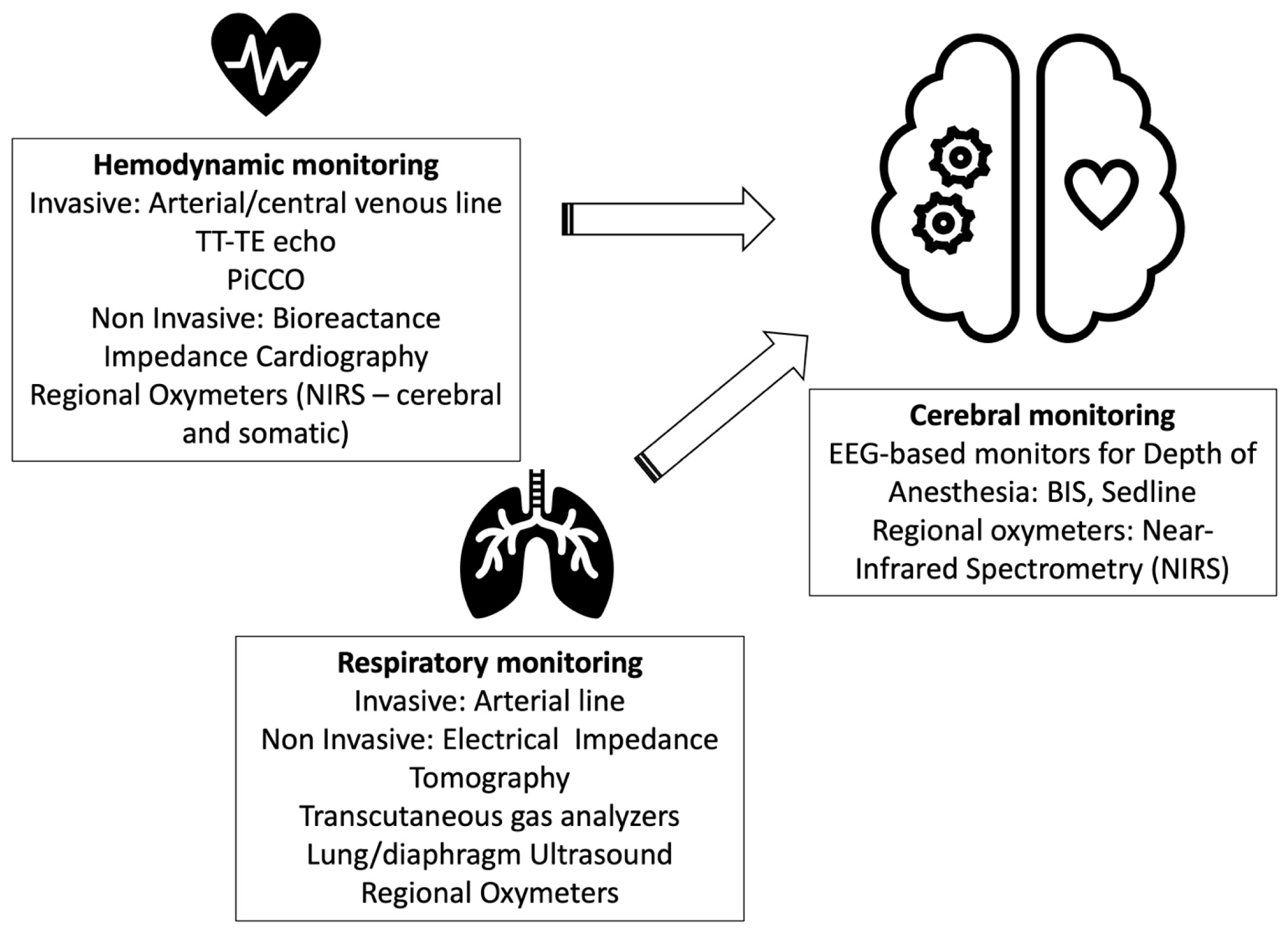
7. Pediatric Anesthesia during MAS
7.1. Cerebral Oxygenation: NIRS
7.2. Hypothermia
8. Discussion
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Meinzer, A.; Alkatout, I.; Krebs, T.F.; Baastrup, J.; Reischig, K.; Meiksans, R.; Bergholz, R. Advances and Trends in Pediatric Minimally Invasive Surgery. J. Clin. Med. 2020, 9, 3999. [Google Scholar] [CrossRef] [PubMed]
- Schukfeh, N.; Kuebler, J.F.; Dingemann, J.; Ure, B.M. Thirty Years of Minimally Invasive Surgery in Children: Analysis of Meta-Analyses. Eur. J. Pediatr. Surg. 2020, 30, 420–428. [Google Scholar] [PubMed]
- Bellon, M.; Skhiri, A.; Julien-Marsollier, F.; Malbezin, S.; Thierno, D.; Hilly, J.; ElGhoneimi, A.; Bonnard, A.; Michelet, D.; Dahmani, S. Paediatric minimally invasive abdominal and urological surgeries: Current trends and perioperative management. Anaesth. Crit. Care Pain Med. 2018, 37, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z. Advances and Future Challenges of Minimally Invasive Surgery in Children. Children 2022, 9, 1959. [Google Scholar] [CrossRef] [PubMed]
- Shu, B.; Feng, X.; Martynov, I.; Lacher, M.; Mayer, S. Pediatric Minimally Invasive Surgery—A Bibliometric Study on 30 Years of Research Activity. Children 2022, 9, 1264. [Google Scholar] [CrossRef] [PubMed]
- Dingemann, J.; Ure, B.M. Systematic review of level 1 evidence for laparoscopic pediatric surgery: Do our procedures comply with the requirements of evidence-based medicine? Eur. J. Pediatr. Surg. 2013, 23, 474–479. [Google Scholar]
- Pelizzo, G.; Costanzo, S.; Roveri, M.; Lanfranchi, G.; Vertemati, M.; Milani, P.; Zuccotti, G.; Cassin, S.; Panfili, S.; Rizzetto, F.; et al. Developing Virtual Reality Head Mounted Display (HMD) Set-Up for Thoracoscopic Surgery of Complex Congenital Lung Malformations in Children. Children 2022, 9, 50. [Google Scholar] [CrossRef]
- Destro, F.; Salerno, R.; Calcaterra, V.; Ardizzone, S.; Meroni, M.; Roveri, M.; Pierucci, U.M.; Zaja, A.; Rizzetto, F.; Campari, A.; et al. Echo-Endoscopy Combined with Virtual Reality: A Whole Perspective of Laparoscopic Common Bile Duct Exploration in Children. Children 2023, 10, 760. [Google Scholar] [CrossRef]
- Nezhat, C.; Page, B. Endoscopy as a philosophy. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Ball, K.A. The Evolution of Endoscopy. In Endoscopic Surgery; Ledbetter, M.S., Ed.; Mosby: St. Louis, MO, USA, 1997; pp. 1–14. [Google Scholar]
- Nezhat, C.; Page, B. Ancient to pre-modern period. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. Renaissance, scientific revolution, age of enlightenment. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. Hovering on the brink of modernity. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Cunningham, L.L.; Gilman, P.P. Historical Development of Endoscopy; Atlas of the Oral and Maxillofacial Surgery Clinics of North America: Philadelphia, PA, USA, 2003; Volume 11.2, pp. 109–127. [Google Scholar]
- Léger, P. Antonin Jean Desormeaux. Prog. Urol. 2004, 14, 1231–1238. (In French) [Google Scholar]
- Nezhat, C.; Page, B. Desormeaux. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. After Desormeaux. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. The era of Nitze. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Powers, C.J. A Brief History of Endoscopy. Semin. Perioper. Nurs. 1993, 2, 129–132. [Google Scholar]
- Culjat, M.; Rahul, S.; Hua, L. Medical Devices Surgical and Image-Guided Technologies; John Wiley & Sons: Hoboken, NJ, USA, 2012; pp. 277–286. [Google Scholar]
- Rauchfuss, A.E. The Nasal Speculum. Its Historical Development and Remarks on the History of Rhinoscopy. Laryngol. Rhinol. Otol. 1985, 64, 551–558. [Google Scholar] [CrossRef]
- Nezhat, C.; Page, B. Bozzini: The beginning of early modern endoscopy. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. 1970’S. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. Post-Bozzini. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. 1940’S. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. 1960’S. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. The Larynx illuminated. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. Nezhat & the rise of advanced operative video-laparoscopy. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. Early 20th century. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Nezhat, C.; Page, B. Recap of where endoscopy stood. In History of Endoscopy; Wetter, P.A., Ed.; Society of Laparoendoscopic Surgeons: Miami, FL, USA, 2023. [Google Scholar]
- Esposito, C.; Autorino, G.; Castagnetti, M.; Cerulo, M.; Coppola, V.; Cardone, R.; Esposito, G.; Borgogni, R.; Escolino, M. Robotics and future technical developments in pediatric urology. Semin. Pediatr. Surg. 2021, 30, 151082. [Google Scholar] [CrossRef]
- Niemelä, R.; Pikkarainen, M.; Ervasti, M.; Reponen, J. The change of pediatric surgery practice due to the emergence of connected health technologies. Technol. Forecast. Soc. Chang. 2019, 146, 352–365. [Google Scholar] [CrossRef]
- Sack, B.S.; Elizondo, R.A.; Huang, G.O.; Janzen, N.; Espinoza, J.; Sanz-Cortes, M.; Dietrich, J.E.; Hakim, J.; Richardson, E.S.; Oden, M.; et al. Pediatric medical device development by surgeons via capstone engineering design programs. J. Pediatr. Surg. 2018, 53, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Dimitri, P.; Pignataro, V.; Lupo, M.; Bonifazi, D.; Henke, M.; Musazzi, U.M.; Ernst, F.; Minghetti, P.; Redaelli, D.F.; Antimisiaris, S.G.; et al. Medical Device Development for Children and Young People—Reviewing the Challenges and Opportunities. Pharmaceutics 2021, 13, 2178. [Google Scholar] [CrossRef] [PubMed]
- United States Code: Federal Food, Drug, and Cosmetic Act, 21 U.S.C. §§ 301-392 (Suppl. 5 1934). Available online: https://www.fda.gov/medical-devices/products-and-medical-procedures/pediatric-medical-devices#:~:text=The%20Federal%20Food%2C%20Drug%2C%20and,first%2028%20days%20of%20life (accessed on 12 January 2022).
- Li, Y.W.; Han, X.; Wang, T.Y. Innovation: An Eternal Theme in the Development of Pediatrics. Chin. Med. J. 2017, 130, 2773–2775. [Google Scholar] [CrossRef] [PubMed]
- Frader, J.E.; Flanagan-Klygis, E. Innovation and research in pediatric surgery. Semin. Pediatr. Surg. 2001, 10, 198–203. [Google Scholar] [CrossRef]
- Lee, S.J.; Cho, L.; Klang, E.; Wall, J.; Rensi, S.; Glicksberg, B.S. Quantification of US Food and Drug Administration Premarket Approval Statements for High-Risk Medical Devices With Pediatric Age Indications. JAMA Netw. Open 2021, 4, e2112562. [Google Scholar] [CrossRef]
- Rome, B.N.; Kramer, D.B.; Kesselheim, A.S. Approval of high-risk medical devices in the US: Implications for clinical cardiology. Curr. Cardiol. Rep. 2014, 16, 489. [Google Scholar] [CrossRef]
- Zuckerman, B.; Margolis, P.A.; Mate, K.S. Health services innovation: The time is now. JAMA 2013, 309, 1113–1114. [Google Scholar] [CrossRef]
- Hwang, T.J.; Kesselheim, A.S.; Bourgeois, F.T. Postmarketing trials and pediatric device approvals. Pediatrics 2014, 133, e1197–e1202. [Google Scholar] [CrossRef] [PubMed]
- Bleicher, E.W. Encouraging research and development of pediatric medical devices through legislative and regulatory action: The Pediatric Medical Device Safety and Improvement Act of 2007 in context. Food Drug Law J. 2009, 64, 531–564. [Google Scholar]
- Loftus, P.D.; Elder, C.T.; D’Ambrosio, T.; Langell, J.T. Addressing challenges of training a new generation of clinician-innovators through an interdisciplinary medical technology design program: Bench-to- bedside. Clin. Transl. Med. 2015, 4, 15. [Google Scholar] [CrossRef] [PubMed]
- Melvin, T.; Kenny, D.; Gewillig, M.; Fraser, A.G. Orphan Medical Devices and Pediatric Cardiology—What Interventionists in Europe Need to Know, and What Needs to be Done. Pediatr. Cardiol. 2023, 44, 271–279. [Google Scholar]
- Section on Surgery; Committee on Bioethics; American Pediatric Surgical Association New Technology Committee. Responsible Innovation in Children’s Surgical Care. Pediatrics 2017, 139, e20163437. [Google Scholar] [CrossRef]
- Ulrich, L.C.; Joseph, F.D.; Lewis, D.Y.; Koenig, R.L. FDA’s pediatric device consortia: National program fosters pediatric medical device development. Pediatrics 2013, 131, 981–985. [Google Scholar] [CrossRef]
- Iqbal, C.W.; Wall, J.; Harrison, M.R. Challenges and climate of business environment and resources to support pediatric device development. Semin. Pediatr. Surg. 2015, 24, 107–111. [Google Scholar] [CrossRef]
- O’Donovan, P.J.; McGurgan, P. Microlaparoscopy. Semin. Laparosc. Surg. 1999, 6, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Cuaresma, R.; Benavides, M.; Buela, E.; Bignon, H.; Martínez-Ferro, M. Laparoscopic appendectomies in pediatric patients using Hem-o-lock clips. Cir. Pediatr. 2009, 22, 103–105. [Google Scholar]
- Lv, B.; Zhang, X.; Li, J.; Leng, S.; Li, S.; Zeng, Y.; Wang, B.; Yuan, J.; Fan, J.; Xing, S.; et al. Absorbable polymeric surgical clips for appendicular stump closure: A randomized control trial of laparoscopic appendectomy with laparo-clips. Oncotarget 2016, 7, 41265–41273. [Google Scholar] [CrossRef]
- Harrell, A.G.; Kercher, K.W.; Heniford, B.T. Energy sources in laparoscopy. Semin. Laparosc. Surg. 2004, 11, 201–209. [Google Scholar] [CrossRef]
- Highlights|KARL STORZ Endoskope. Available online: https://www.karlstorz.com/it/it/75-years.htm (accessed on 12 November 2020).
- FlexDex System—A SAGES Technology and Value Assessment. Available online: https://www.sages.org/publications/tavac/flexdex-system/ (accessed on 6 November 2020).
- Tokas, T.; Gözen, A.S.; Avgeris, M.; Tschada, A.; Fiedler, M.; Klein, J.; Rassweiler, J. Combining of ETHOS Operating Ergonomic Platform, Three-dimensional Laparoscopic Camera, and Radius Surgical System Manipulators Improves Ergonomy in Urologic Laparoscopy: Comparison with Conventional Laparoscopy and da Vinci in a Pelvi Trainer. Eur. Urol. Focus 2017, 3, 413–420. [Google Scholar] [CrossRef]
- Artisential Articulating Laparoscopic Instrument(s)—A SAGES Technology and Value Assessment. Available online: https://www.sages.org/publications/tavac/artisential-articulating-laparoscopic-instruments/ (accessed on 6 November 2020).
- Cui, X.; He, Y.-B.; Huang, W.-H.; Chen, L.; Chen, J.-C.; Zhou, C.-M. Mini-laparoscopic pyeloplasty to treat UPJO in infants. Minim. Invasive Ther. Allied Technol. 2022, 31, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Lacher, M.; Kuebler, J.F.; Dingemann, J.; Ure, B.M. Minimal invasive surgery in the newborn: Current status and evidence. Semin. Pediatr. Surg. 2014, 23, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Boscarelli, A.; Giglione, E.; Caputo, M.R.; Guida, E.; Iaquinto, M.; Scarpa, M.G.; Olenik, D.; Codrich, D.; Schleef, J. Robotic-assisted surgery in pediatrics: What is evidence-based?—A literature review. Transl. Pediatr. 2023, 12, 271–279. [Google Scholar] [CrossRef]
- Cundy, T.P.; Shetty, K.; Clark, J.; Chang, T.P.; Sriskandarajah, K.; Gattas, N.E.; Najmaldin, A.; Yang, G.-Z.; Darzi, A. The first decade of robotic surgery in children. J. Pediatr. Surg. 2013, 48, 858–865. [Google Scholar] [CrossRef]
- Adler, A.C.; Siddiqui, A.; Chandrakantan, A.; Matava, C.T. Lung and airway ultrasound in pediatric anesthesia. Pediatr. Anesth. 2022, 32, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Lazar, A.; Chatterjee, D.; Templeton, T.W. Error traps in pediatric one-lung ventilation. Pediatr. Anesth. 2022, 32, 346–353. [Google Scholar] [CrossRef]
- Faulk, D.J.; Austin, T.M.; Thomas, J.J.; Strupp, K.; Macrae, A.W.; Yaster, M. A Survey of the Society for Pediatric Anesthesia on the Use, Monitoring, and Antagonism of Neuromuscular Blockade. Anesth. Analg. 2021, 132, 1518–1526. [Google Scholar]
- Lee, J.H.; Song, I.S.; Kang, P.; Ji, S.H.; Jang, Y.E.; Kim, E.H.; Kim, H.S.; Kim, J.T. Validation of the Masimo O3™ regional oximetry device in pediatric patients undergoing cardiac surgery. J. Clin. Monit. Comput. 2022, 36, 1703–1709. [Google Scholar] [CrossRef]
- Beck, R.; Milella, L.; Labellarte, C. Continuous non-invasive measurement of stroke volume and cardiac index in infants and children: Comparison of Impedance Cardiography NICaS® vs CardioQ® method. Clin. Ter. 2018, 169, e110–e113. [Google Scholar] [PubMed]
- Trieu, C.T.; Williams, T.M.; Cannesson, M.; Marijic, J. Babies and Children at Last: Pediatric Cardiac Output Monitoring in the Twenty-first Century. Anesthesiology 2019, 130, 671–673. [Google Scholar] [CrossRef] [PubMed]
- Weber, F.; Scoones, G.P. A practical approach to cerebral near-infrared spectroscopy (NIRS) directed hemodynamic management in noncardiac pediatric anesthesia. Pediatr. Anesth. 2019, 29, 993–1001. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Miao, M.; Li, P.; Yang, Y.; Zhang, H.; Zhang, B.; Sun, M.; Zhang, J. EEG-Parameter-Guided Anesthesia for Prevention of Emergence Delirium in Children. Brain Sci. 2022, 12, 1195. [Google Scholar] [CrossRef] [PubMed]
- Pelizzo, G.; Bernardi, L.; Carlini, V.; Pasqua, N.; Mencherini, S.; Maggio, G.; De Silvestri, A.; Bianchi, L.; Calcaterra, V. Laparoscopy in children and its impact on brain oxygenation during routine inguinal hernia repair. J. Minimal Access Surg. 2017, 13, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Kılınç, L.; Türk, H.Ş.; Sayın, P.; Çınar, S.; Demir, M.; İslamoğlu, S. Effects of Pneumoperitoneum on Splanchnic Oxygenation during Abdominal Laparoscopic Surgery in Paediatric Patients: A prospective, Observational Study. Turk. J. Anaesthesiol. Reanim. 2021, 49, 138–143. [Google Scholar] [CrossRef]
- Oztan, M.O.; Aydin, G.; Cigsar, E.B.; Sutas Bozkurt, P.; Koyluoglu, G. Effects of Carbon Dioxide Insufflation and Trendelenburg Position on Brain Oxygenation During Laparoscopy in Children. Surg. Laparosc. Endosc. Percutaneous Tech. 2019, 29, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Tuna, A.T.; Akkoyun, I.; Darcin, S.; Palabiyik, O. Effects of carbon dioxide insufflation on regional cerebral oxygenation during laparoscopic surgery in children: A prospective study. Braz. J. Anesthesiol. 2016, 66, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Ytgat, S.H.; van Herwaarden, M.Y.; Stolwijk, L.J.; Keunen, K.; Benders, M.J.; de Graaff, J.C.; Milstein, D.M.J.; van der Zee, D.C.; Lemmers, P.M.A. Neonatal brain oxygenation during thoracoscopic correction of esophageal atresia. Surg. Endosc. 2016, 30, 2811–2817. [Google Scholar] [CrossRef]
- Sessler, D.I. Perioperative thermoregulation and heat balance. Lancet 2016, 387, 2655–2664. [Google Scholar] [CrossRef]
- Buggy, D.J.; Crossley, A.W. Thermoregulation, mild perioperative hypothermia and postanaesthetic shivering. Br. J. Anaesth. 2000, 84, 615–628. [Google Scholar] [CrossRef]
- Kaya, A.C.; Radosa, M.P.; Zimmermann, J.S.M.; Stotz, L.; Findeklee, S.; Hamza, A.; Sklavounos, P.; Takacs, F.Z.; Wagenpfeil, G.; Radosa, C.G.; et al. Intraoperative and postoperative complications of gynecological laparoscopic interventions: Incidence and risk factors. Arch. Gynecol. Obstet. 2021, 304, 1259–1269. [Google Scholar] [CrossRef] [PubMed]
- Frank, S.M.; Higgins, M.S.; Fleisher, L.A.; Sitzmann, J.V.; Raff, H.; Breslow, M.J. Adrenergic, respiratory, and cardiovascular effects of core cooling in humans. Am. J. Physiol. 1997, 272 Pt 2, R557–R562. [Google Scholar] [CrossRef]
- Frank, S.M.; Fleisher, L.A.; Breslow, M.J.; Higgins, M.S.; Olson, K.F.; Kelly, S.; Beattie, C. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. JAMA 1997, 277, 1127–1134. [Google Scholar] [CrossRef] [PubMed]
- Melling, A.C.; Ali, B.; Scott, E.M.; Leaper, D.J. Effects of preoperative warming on the incidence of wound infection after clean surgery: A randomized controlled trial. Lancet 2001, 358, 876–880. [Google Scholar] [CrossRef]
- Bessell, J.R.; Karatassas, A.; Patterson, J.R.; Jamieson, G.G.; Maddern, G.J. Hypothermia induced by laparoscopic insufflation. A randomized study in a pig model. Surg. Endosc. 1995, 9, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Bessell, J.R.; Ludbrook, G.; Millard, S.H.; Baxter, P.S.; Ubhi, S.S.; Maddern, G.J. Humidified gas prevents hypothermia induced by laparoscopic insufflation: A randomized controlled study in a pig model. Surg. Endosc. 1999, 13, 101–105. [Google Scholar] [CrossRef]
- Hazebroek, E.J.; Schreve, M.A.; Visser, P.; De Bruin, R.W.; Marquet, R.L.; Bonjer, H.J. Impact of temperature and humidity of carbon dioxide pneumoperitoneum on body temperature and peritoneal morphology. J. Laparoendosc. Adv. Surg. Tech. A 2002, 12, 355–364. [Google Scholar] [CrossRef]
- Schwartz, R. Why a teenager over age 14 should be able to consent, rather than merely assent, to participation as a human subject of research. Am. J. Bioeth. 2003, 3, 38–40. [Google Scholar]
- Riskin, D.J.; Longaker, M.T.; Krummel, T.M. The ethics of innovation in pediatric surgery. Semin. Pediatr. Surg. 2006, 15, 319–323. [Google Scholar] [CrossRef]
- McKneally, M.F.; Daar, A.S. Introducing new technologies: Protecting subjects of surgical innovation and research. World J. Surg. 2003, 27, 930–935. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.A. Innovation in pediatric surgery: The surgical innovation continuum and the ETHICAL model. J. Pediatr. Surg. 2014, 49, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Antiel, R.M.; Flake, A.W. Responsible surgical innovation and research in maternal-fetal surgery. Semin. Fetal Neonatal Med. 2017, 22, 423–427. [Google Scholar] [CrossRef] [PubMed]
- National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. Ethical Principles and Guidelines for the Protection of Human Subjects of Research; The Belmont Report; National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research: Bethesda, MD, USA, 1979. [Google Scholar]
- Reitsma, A.M.; Moreno, J.D. Chapter 9: Ethics guidelines for innovative surgery: Recommendations for national policy. In Ethical Guidelines for Innovative Surgery; University of Pennsylvania: Philadelphia, PA, USA, 2006. [Google Scholar]
| Definition at the Time of Diagnosis or Treatment | Age Range |
|---|---|
| Neonates | From birth through the first 28 days of life |
| Infants | From 29 days to less than 2 years |
| Children | From 2 years to less than 12 years |
| Adolescents | Aged 12 through 21 (up to but not including the 22nd birthday) |
| Videoscopes | 5 mm and 10 mm |
| 4 mm and 10 mm IMAGE1 STM 3D (HD and 3D vision; 0- and 30-degree optic) by Karl Storz | |
| Operative instruments (by Karl Storz, Tuttlingen, Baden-Württemberg, Germany; Wolff, Knittlingen/Germany, Aesculap-B.Braun, Tuttlingen, Baden-Württemberg, Germany) | |
| Grasping | 2 mm (fragility; tendency to bend; grasping difficulties), 3 mm, 5 mm |
| Hemostasis | 5-mm-clip staplers |
| LigasureTM (Medtronic, Minneapolis, MN, USA) | |
| EnSeal® (Ethicon, Raritan, NJ, USA) |
| Instruments for NOTES | Indications | Challenges | Advantages |
|---|---|---|---|
| ANUBIS by Karl Storz ENDOSAMURAI (endoscope with two arms on the tip + forceps channel) by Olympus, Westborough, MA, USA |
| Instrument clashing, suboptimal exposure, and inline placement of the instruments vs. laparoscopic triangulation | Less pain, increased aesthetic result, improved post-operative QoL |
| Da Vinci by Intuitive Surgical (Sunnyvale, CA, USA) from 2001 |
|
| Senhance (in children > 10 kg) by Transenterix (Morrisville, NC, USA) from 2020 |
|
| Dexter (Distalmotion, Lausanne, Switzerland) |
|
| Robotic system (Verb Surgical- Johnson & Johnson, New Brunswick, NJ, USA) with enhanced medical data science (emerging) | |
| Avatera (Avateramedical, Jena, Germany) |
|
| Versius robotic system (CMR Surgical, Cambridge, UK) |
|
| Automated suturing robots (e.g., KidsArm, Ottawa, ON, Canada, STAR, Intuitive Surgical, Sunnyvale, CA, USA) | |
| Deployable minirobots (minirobots inserted through incisions; research) |
| Indications | Features of the Instrumentation | |
|---|---|---|
| SILS or laparoscopic-assisted procedures | FlexDex (Brighton, MI, USA) needle driver (wristed angulation) | |
| VATS (video-assisted thoracoscopic surgery) | Radius Surgical System by Tüebingen Scientific, (Tuebingen, Germany) (improved maneuverability) | |
| Artisential Laparoscopic System by Livsmed (San Diego, CA, USA) (wide range of articulating instruments) | ||
| 5 mm Hand-X electronic articulating needle driver by Human Xtensions (Metanya, Israel) | ||
| SymphonX Surgical Platform for SILS by Fortimedix Surgical B.V. (Geleen, The Netherlands) | 15 mm trocar Four channels (5 and 3 mm) | |
| Spider Surgical system (Single Port Instrument Delivery Extended Reach) for SILS by Transenterix-Asensus (Morrisville, NC, USA) | ||
| MUSA (robot for open microsurgical procedures) by Microsure (Son, The Netherlands) |
| Indications | Features of the Instrumentation |
|---|---|
| Hybrid Procedures |
|
| Area | Topic | Specific Considerations |
|---|---|---|
| Gastrointestinal surgery | Inguinal hernia repair (1/3 of citations) |
|
| Appendectomy | ||
| Pyloromyotomy | ||
| Urology | Pyeloplasty |
|
| Nephrectomy | ||
| Ureteral reimplantation | ||
| Thoracic surgery | Esophageal atresia |
|
| Congenital diaphragmatic hernia | ||
| Congenital lung malformations | ||
| Thoracic empyema |
| Area | Topic | Specific Considerations |
|---|---|---|
| Gastrointestinal surgery | Fundoplication |
|
| Other: splenectomy, Heller’s myotomy, intestinal anastomosis, anorectal pull-through, ovarian cystectomy, salpingo-oophorectomy |
| |
| Hepatobiliary diseases (choledochal cyst excision, cholecystectomy) |
| |
| Urology (main RAS indications) | Pyeloplasty Ureteral reimplantation (Lich-Gregoire) |
|
| Thoracic surgery | Robotic assisted thoracoscopic surgery (RATS) |
|
| Oncological surgery |
|
| Laparoscopy | Advantages (Number of Meta-Analyses) | Disadvantages (Number of Meta-Analyses) | |||||
|---|---|---|---|---|---|---|---|
| Shorter Hospital Stay | Shorter Time to Full Feeding | Reduced Complication Rate | Other (Number of Meta-Analyses) | Longer Operative Time | Higher Recurrence Rate | Other | |
| Adhesiolysis (1) | - | - | 1 | - | - | - | - |
| Anorectal malformation repair (1) | - | - | - | - | - | - | - |
| Appendectomy (5) | 3/5 | 1/5 | - | Reduced wound infection (4/5), reduced bowel obstruction (4/5) | 2/5 | - | Intrabdominal abscess (2/5) |
| Choledochal cyst resection (2) | 2/2 | 1/2 | - | Reduced intraoperative blood loss (1), reduced bowel obstruction (1) | 2/2 | - | - |
| Duodenal obstruction repair (2) | - | - | - | - | 1/2 | - | Increased anastomotic complications (1/2) |
| Fundoplication (4) | 1/4 | 1/4 | 1/4 | Reduced retching (1/4) and morbidity at 30 days (1/4) | 3/4 | 2/4 | - |
| Intussusception reduction (1) | 1/1 | - | - | - | - | - | - |
| Kasai portoenterostomy (1) | - | - | - | - | - | - | Reduced survival with native liver (1/1) |
| Ladd’s procedure (1) | 1/1 | 1/1 | 1/1 | Reduced readmissions (1/1) | - | - | Postoperative volvulus (1/1) |
| Pyloromyotomy (5) | 3/5 | 4/5 | 1/5 | - | - | 1/5 | Increased overall complications (1/5) |
| Splenectomy (1) | 1/1 | - | - | Reduced intraoperative blood loss (1/1) | 1/1 | - | - |
| Urology | Advantages (Number of Meta-Analyses) | Disadvantages (Number of Meta-Analyses) | |||||
|---|---|---|---|---|---|---|---|
| Shorter Hospital Stay | Shorter Time to Full Feeding | Reduced Complication Rate | Other (Number of Meta-Analyses) | Longer Operative Time | Higher Recurrence Rate | Other | |
| Inguinal hernia repair (4) | - | - | 2/4 | Reduced operative time in case of bilateral hernia (3/4), reduced rate of contralateral hernia (2/4) | - | - | - |
| Orchidopexy (1) | 1/1 | - | - | - | - | - | - |
| Pyeloplasty (3) | 2/3 | - | 1/3 | - | 2/3 | - | - |
| Varicocelectomy (2) | - | - | - | - | - | - | - |
| Thoracoscopy | Advantages (Number of Meta-Analyses) | Disadvantages (Number of Meta-Analyses) | |||||
|---|---|---|---|---|---|---|---|
| Shorter Hospital Stay | Shorter Time to Full Feeding | Reduced Complication Rate | Other (Number of Meta-Analyses) | Longer Operative Time | Higher Recurrence Rate | Other | |
| Congenital diaphragmatic hernia (4) | 1/4 | 1/4 | - | Reduced postoperative mortality (3/4), reduced postoperative ventilator time (2/4) | 3/4 | 4/4 | - |
| Esophageal atresia repair (3) | 2/3 | 2/3 | - | Reduced postoperative ventilator time (1/3) | - | - | - |
| Pulmonary malformation resection (2) | 2/2 | - | 1/2 | Shorter chest-tube placement (1/2) | - | - | - |
| Congenital diaphragmatic hernia (4) | 1/4 | 1/4 | - | Reduced postoperative mortality (3/4), reduced postoperative ventilator time (2/4) | 3/4 | 4/4 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pelizzo, G.; Destro, F.; Pierucci, U.M.; Costanzo, S.; Camporesi, A.; Diotto, V.; Calcaterra, V.; Saxena, A.K. Minimal Access in Pediatric Surgery: An Overview on Progress towards Dedicated Instrument Developments and Anesthesiologic Advances to Enhance Safe Completion of Procedures. Children 2024, 11, 679. https://doi.org/10.3390/children11060679
Pelizzo G, Destro F, Pierucci UM, Costanzo S, Camporesi A, Diotto V, Calcaterra V, Saxena AK. Minimal Access in Pediatric Surgery: An Overview on Progress towards Dedicated Instrument Developments and Anesthesiologic Advances to Enhance Safe Completion of Procedures. Children. 2024; 11(6):679. https://doi.org/10.3390/children11060679
Chicago/Turabian StylePelizzo, Gloria, Francesca Destro, Ugo Maria Pierucci, Sara Costanzo, Anna Camporesi, Veronica Diotto, Valeria Calcaterra, and Amulya K. Saxena. 2024. "Minimal Access in Pediatric Surgery: An Overview on Progress towards Dedicated Instrument Developments and Anesthesiologic Advances to Enhance Safe Completion of Procedures" Children 11, no. 6: 679. https://doi.org/10.3390/children11060679
APA StylePelizzo, G., Destro, F., Pierucci, U. M., Costanzo, S., Camporesi, A., Diotto, V., Calcaterra, V., & Saxena, A. K. (2024). Minimal Access in Pediatric Surgery: An Overview on Progress towards Dedicated Instrument Developments and Anesthesiologic Advances to Enhance Safe Completion of Procedures. Children, 11(6), 679. https://doi.org/10.3390/children11060679






