Prevalence and Characteristics of Sleep Disorders in Children Aged 7–17: Insights from Parental Observations at the Dental Office
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Aspects
2.2. Population and Eligibility Criteria
2.3. Sample Size
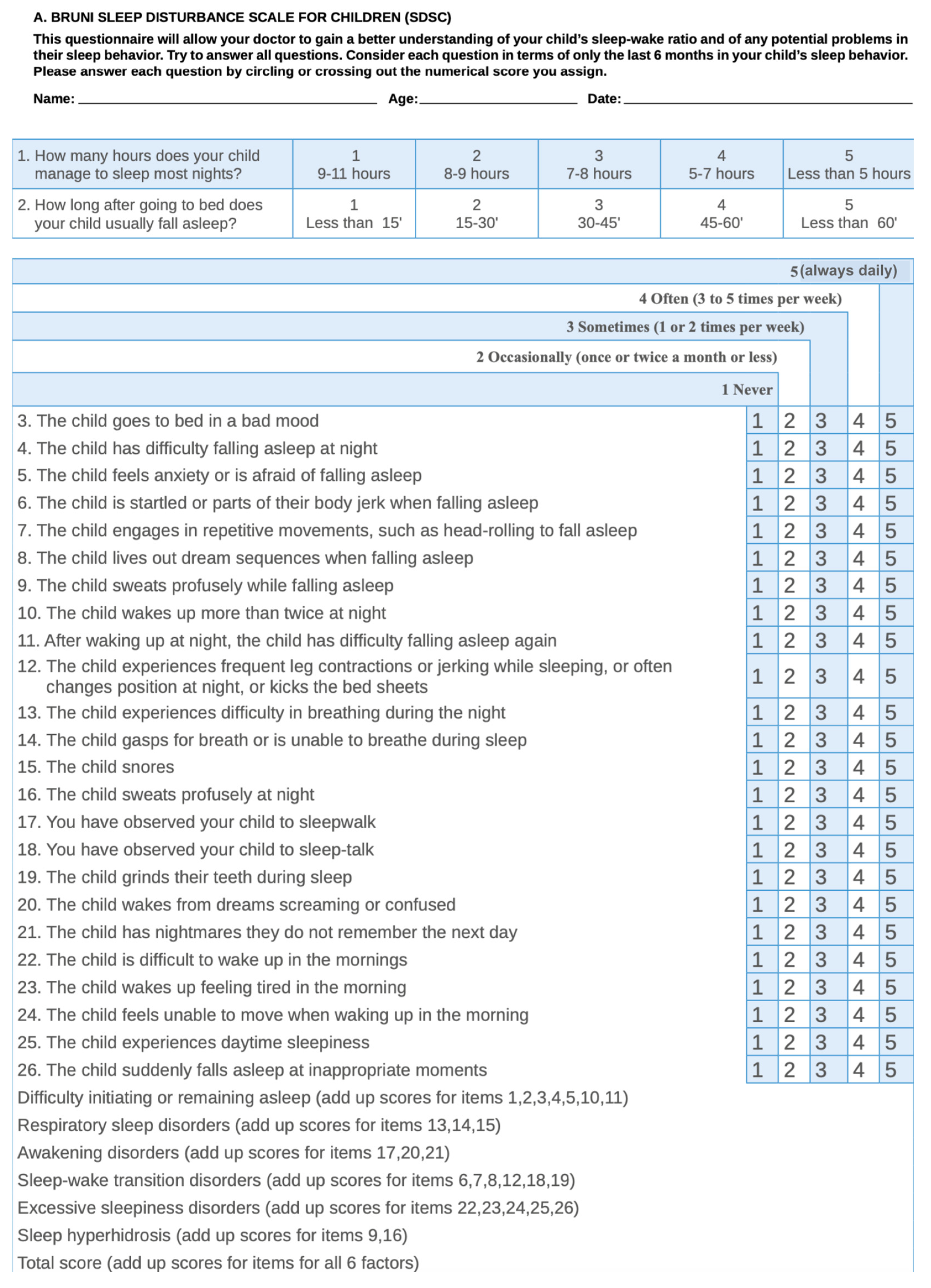
2.4. Variables and Procedures for Their Collection
2.5. Statistic Analysis
3. Results
3.1. Sample Description
3.2. Scores Gathered from the Sleep Disturbance Scale Survey
3.3. Frequency of Sleep Disturbances
3.4. Comparison between Both Groups
4. Discussion
4.1. Validated Questionnaires
4.2. Prevalence of Sleep Disturbances
4.3. Research on the Spanish Population
4.4. Respiratory Sleep Disorders
4.5. Other Considerations: Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amy Licis, M.D. Sleep-Wake Disorders in Childhood. Sleep Neurol. 2020, 26, 1034–1069. [Google Scholar]
- Chokroverty, S. Overview of sleep & sleep disorders. Indian J. Med. Res. 2010, 131, 126–140. [Google Scholar] [PubMed]
- Trosman, I.; Ivanenko, A. Classification and Epidemiology of Sleep Disorders in Children and Adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2021, 30, 47–64. [Google Scholar] [CrossRef] [PubMed]
- Leung, T.N.H.; Wong, K.L.; Chan, A.K.C.; Li, A.M. Common Childhood Sleep Problems and Disorders. Curr. Pediatr. Rev. 2024, 20, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Mulas, F.; Rojas, M.; Gandía, R. Sleep in neurodevelopmental disorders, attention deficit hyperactivity disorder and autism spectrum disorders [Sueño en los trastornos del neurodesarrollo, deficit de atención e hiperactividad y en espectro autista]. Medicina 2019, 79, 33–36. [Google Scholar] [PubMed]
- Navarro Vergara, A.; González Rabelino, G. Sleep disorders and their impact on neurodevelopmental development. [Trastornos del sueño y su impacto en el neurodesarrollo]. Medicina 2022, 84, 30–34. [Google Scholar]
- Ordway, M.R.; Logan, S.E.; Sutton, E.H. Sleep Deficiency in Young Children. Clin. Chest Med. 2022, 43, 229–237. [Google Scholar] [CrossRef]
- Reiter, J.; Ramagopal, M.; Gileles-Hillel, A.; Forno, E. Sleep disorders in children with asthma. Pediatr. Pulmonol. 2022, 57, 1851–1859. [Google Scholar] [CrossRef]
- Coleman, J. Overview of sleep disorders: Where does obstructive sleep apnea syndrome fit in? Otolaryngol. Clin. N. Am. 1999, 32, 187–193. [Google Scholar] [CrossRef]
- Lazaratou, H.; Soldatou, A.; Dikeos, D. Medical comorbidity of sleep disorders in children and adolescents. Curr. Opin. Psychiatry 2012, 25, 391–397. [Google Scholar] [CrossRef]
- Carter, K.A.; Hathaway, N.E.; Lettiieri, C.F. Common sleep disorders in children. Am. Fam. Physician 2014, 89, 368–377. [Google Scholar] [PubMed]
- Schnatschmidt, M.; Schlarb, A. Sleep and mental disorders in childhood and adolescence. Z. Kinder Jugendpsychiatr. Psychother. 2018, 46, 368–381. [Google Scholar] [CrossRef] [PubMed]
- Arns, M.; Kooij, J.J.S.; Coogan, A.N. Review: Identification and Management of Circadian Rhythm Sleep Disorders as a Transdiagnostic Feature in Child and Adolescent Psychiatry. J. Am. Acad. Child Adolesc. Psychiatry 2021, 60, 1085–1095. [Google Scholar] [CrossRef]
- Baddam, S.K.R.; Canapari, C.A.; Van de Grift, J.; McGirr, C.; Nasser, A.Y.; Crowley, M.J. Screening and Evaluation of Sleep Disturbances and Sleep Disorders in Children and Adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2021, 30, 64–85. [Google Scholar] [CrossRef]
- Lam, L.T.; Lam, M.K. Sleep disorders in early childhood and the development of mental health problems in adolescents: A systematic review of longitudinal and prospective studies. Int. J. Environ. Res. Public Health 2021, 18, 11782. [Google Scholar] [CrossRef] [PubMed]
- Arias-Mera, C.; Paillama-Raimán, D.; Lucero-González, N.; Leiva-Bianchi, M.; Avello-Saez, D. Relation between sleep disorders and attention deficit disorder with hyperactivity in children and adolescents: A systematic review. Res. Dev. Disabil. 2023, 137, 104500. [Google Scholar] [CrossRef] [PubMed]
- Ophoff, D.; Slaats, M.A.; Boudewyns, A.; Glazemakers, I.; Van Hoorenbeeck, K.; Verhulst, S.L. Sleep disorders during childhood: A practical review. Eur. J. Pediatr. 2018, 177, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Quinteros-Hinojosa, M.; Diéguez-Pérez, M. Survey of the Potential Association of Childhood Sleep Disorders with Sleep Bruxism. Científica Dent. 2019, 16, 14–20. [Google Scholar]
- Diéguez-Pérez, M.; Ticona-Flores, J.M.; Prieto-Regueiro, B. Prevalence of Possible Sleep Bruxism and Its Association with Social and Orofacial Factors in Preschool Population. Healthcare 2023, 11, 1450. [Google Scholar] [CrossRef]
- Pagerols, M.; Bosch, R.; Prat, R.; Pagespetit, È.; Cilveti, R.; Chaparro, N.; Esteve, A.; Casas, M. The Sleep Disturbance Scale for Children: Psychometric properties and prevalence of sleep disorders in Spanish children aged 6–16 years. J. Sleep Res. 2023, 32, e13871. [Google Scholar] [CrossRef]
- Serdar, C.C.; Cihan, M.; Yücel, D.; Serdar, M.A. Sample size, power and effect size revisited: Simplified and practical approachin pre-clinical, clinical and laboratory studies. Biochem. Medica 2021, 31, 27–53. [Google Scholar] [CrossRef] [PubMed]
- Bruni, O.; Ottaviano, S.; Guidetti, V.; Romoli, M.; Innocenzi, M.; Cortesi, F.; Giannotti, F. The Sleep Disturbance Scale for Children (SDSC) construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J. Sleep Res. 1996, 5, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Babcock, D.A. Evaluating sleep and sleep disorders in the pediatric primary care setting. Pediatr. Clin. N. Am. 2011, 58, 543–554. [Google Scholar] [CrossRef] [PubMed]
- Dékány, L.; Molnár, V.; Molnár, A.; Bikov, A.; Lázár, Z.; Bárdos-Csenteri, O.; Benedek, P. Analysis of possible risk factors for the severity of paediatric obstructive sleep apnoea syndrome. Eur. Arch. Oto-Rhino-Laryngol. 2023, 280, 5607–5614. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.L.; Kyriaki, L.; Arciuli, J. Associations between sleep, reading, and mathematics in Taiwanese children. Br. J. Educ. Psychol. 2023, 93, 694–711. [Google Scholar] [CrossRef] [PubMed]
- Ağca, S.; Görker, I.; Turan, F.N.; Öztük, L. Validity and reliability of the Turkish version of Sleep Disturbance Scale for Children. Sleep Med. 2021, 84, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Van Litsenburg, R.R.; Waumans, R.C.; Van Den Berg, G.; Gemke, R.J. Sleep habits and sleep disturbances in Dutch children: A population-based study. Eur. J. Pediatr. 2010, 169, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Xu, P.; Aizetiguli, M.; Surong, S.; Zhu, Z.; Zhang, J. Prevalence and influencing factors of sleep disorders among preschool children in Urumqi city: A cross-sectional survey. Ital. J. Pediatr. 2023, 49, 68. [Google Scholar] [CrossRef] [PubMed]
- Brockmann, P.E.; Poggi, H.; Martinez, A.; D’Apremont, I.; Moore, R.; Smith, D.; Gozal, D. Perinatal antecedents of sleep disturbances in schoolchildren. Sleep 2020, 43, zsaa021. [Google Scholar] [CrossRef]
- Tachibana, M.; Kato, T.; Kato-Nishimura, K.; Matsuzawa, S.; Mohri, I.; Taniike, M. Associations of sleep bruxism with age, sleep apnea, and daytime problematic behaviors in children. Oral Dis. 2016, 22, 557–565. [Google Scholar] [CrossRef]
- Alencar, N.A.; de Fernandes, A.B.N.; Souza, M.M.G.; de Luiz, R.R.; Fonseca-Gonçalves, A.; Maia, L.C. Lifestyle and oral facial disorders associated with sleep bruxism in children. Cranio 2017, 35, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Baidas, L.; Al-Jobair, A.; Al-Kawari, H.; Alshehri, A.; Al-Madani, S.; Al-Balbeesi, H. Prevalence of sleep-disordered breathing and associations with orofacial symptoms among Saudi primary school children. BMC Oral Health 2019, 19, 43. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, N.A.; Aronin, C.; Kantrowitz, B.; Hershcopf, R.; Fishkin, S.; Lee, H.; Weaver, D.E.; Yip, C.; Liaw, G.; Saadia, T.A.; et al. The prevalence of sleep-disordered breathing in children with asthma and its behavioral effects. Pediatr. Pulmonol. 2015, 50, 1128–1136. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, M.; Halabi, M.; Kowash, M.; Hussein, I.; Khamis, A.; Salami, A. Sleep-disordered breathing in children and adolescents seeking paediatric dental care in Dubai, UAE. Eur. Arch. Paediatr. Dent. 2022, 23, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Di Carlo, G.; Zara, F.; Rocchetti, M.; Venturini, A.; Ortiz-Ruiz, A.J.; Luzzi, V.; Cattaneo, P.M.; Polimeni, a.; Vozza, I. Prevalence of sleep-disordered breathing in children referring for first dental examination. A multicenter cross-sectional study using pediatric sleep questionnaire. Int. J. Environ. Res. Public Health 2020, 17, 8460. [Google Scholar] [CrossRef] [PubMed]
- D’Elia, C.; Gozal, D.; Bruni, O.; Goudouris, E.; Meira e Cruz, M. Allergic rhinitis and sleep disorders in children–coexistence and reciprocal interactions. J. Pediatr. 2022, 98, 444–454. [Google Scholar] [CrossRef] [PubMed]
- Zreaqat, M.; Hassan, R.; Samsudin, A.R.; Stas, Y. Prevalence of Sleep-disordered Breathing and its Association with Obesity among Saudi Schoolchildren. J. Contemp. Dent. Pract. 2020, 21, 1022–1026. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, T.; Rojas, C.; Casals, M.; Bennett, J.T.; Gálvez, C.; Betancur, C.; Mesa, J.T.; Brockmann, P.E. Prevalence and risk factors for sleep-disordered breathing in chilean schoolchildren [Trastornos respiratoriors del sueño en niños escolares chilenos: Prevalencia y factores de riesgo]. Rev. Chil. Pediatr. 2018, 89, 718–725. [Google Scholar]
- Sakamoto, N.; Gozal, D.; Smith, D.L.; Yang, L.; Morimoto, N.; Wada, H.; Maruyama, K.; Ikeda, A.; Suzuki, Y.; Nakayama, M.; et al. Sleep duration, snoring prevalence, obesity, and behavioral problems in a large cohort of primary school students in Japan. Sleep 2017, 40, zsw082. [Google Scholar] [CrossRef]

| Age | Gender | |||||
|---|---|---|---|---|---|---|
| Groups | Total Participants | Males | Females | |||
| Mean | SD | Mean | SD | Mean | SD | |
| A | 9.11 | 1.66 | 8.98 | 1.67 | 9.16 | 1.7 |
| B | 13.66 | 2.01 | 14.03 | 1.8 | 13.42 | 2.14 |
| Mean | SD | Median | Sex | Mean | SD | Median | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Initiating and maintaining sleep | 12.49 | 4.39 | 11.50 | M | 12.38 | 4.16 | 12.00 | 0.990 |
| F | 12.59 | 4.74 | 11.00 | |||||
| Respiratory Sleep disorders | 4.25 | 2.16 | 3.00 | M | 4.41 | 2.29 | 4.00 | 0.127 |
| F | 4.05 | 2.02 | 3.00 | |||||
| Arousal disorders | 4.06 | 1.66 | 3.00 | M | 4.11 | 1.61 | 4.00 | 0.359 |
| F | 4.05 | 1.74 | 3.00 | |||||
| Sleep–wake transition disorders | 10.85 | 4.73 | 10.00 | M | 11.15 | 5.21 | 10.00 | 0.703 |
| F | 10.61 | 4.40 | 9.00 | |||||
| Excessive somnolence disorders | 8.51 | 3.84 | 7.00 | M | 8.81 | 4.59 | 7.00 | 0.820 |
| F | 8.24 | 3.09 | 7.00 | |||||
| Hyperhidrosis | 3.53 | 2.43 | 2.00 | M | 4.07 | 2.78 | 3.00 | 0.003 * |
| F | 3.01 | 1.96 | 2.00 |
| Presence of Sleep Alteration * | n | % 1 | Sex | n | % 2 | p-Value |
|---|---|---|---|---|---|---|
| Initiating and maintaining sleep (score > 10) | 143 | 69.4 | M | 66 | 33.3 | 0.985 |
| F | 70 | 35.4 | ||||
| Respiratory Sleep disorders (score > 4) | 56 | 27.2 | M | 31 | 15.7 | 0.061 |
| F | 21 | 10.6 | ||||
| Arousal disorders (score > 4) | 100 | 48.5 | M | 49 | 24.7 | 0.575 |
| F | 48 | 24.2 | ||||
| Sleep–wake transition disorders (score > 9) | 127 | 61.7 | M | 58 | 29.3 | 0.846 |
| F | 63 | 31.8 | ||||
| Excessive somnolence disorders (score > 8) | 86 | 41.7 | M | 39 | 19.7 | 0.827 |
| F | 43 | 21.7 | ||||
| Hyperhidrosis (score > 3) | 92 | 44.7 | M | 49 | 24.7 | 0.070 |
| F | 39 | 19.7 |
| Group | Mean | SD | Median | Maximum Value | Minimum Value | p-Value | |
|---|---|---|---|---|---|---|---|
| Initiating and maintaining sleep | A | 11.86 | 4.33 | 11.00 | 29.00 | 7.00 | 0.003 * |
| B | 13.24 | 4.38 | 12.50 | 29.00 | 7.00 | ||
| Respiratory Sleep disorders | A | 4.26 | 2.23 | 3.00 | 15.00 | 3.00 | 0.889 |
| B | 4.24 | 2.08 | 3.50 | 12.00 | 3.00 | ||
| Arousal disorders | A | 4.10 | 1.64 | 4.00 | 11.00 | 3.00 | 0.702 |
| B | 4.02 | 1.68 | 3.00 | 11.00 | 3.00 | ||
| Sleep–wake transition disorders | A | 10.59 | 4.53 | 10.00 | 26.00 | 4.00 | 0.785 |
| B | 11.16 | 4.97 | 9.50 | 26.00 | 6.00 | ||
| Excessive somnolence disorders | A | 7.99 | 3.20 | 7.00 | 23.00 | 5.00 | 0.013 ** |
| B | 9.13 | 4.42 | 7.00 | 23.00 | 5.00 | ||
| Hyperhidrosis | A | 3.44 | 2.27 | 2.00 | 10.00 | 2.00 | 0.403 |
| B | 3.64 | 2.63 | 2.00 | 10.00 | 2.00 |
| Group | n | % | p-Value | OR | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Initiating and maintaining sleep | A | 68 | 33.0 | 0.003 * | 2.554 | 1.360 | 4.797 |
| B | 75 | 36.4 | |||||
| Respiratory Sleep disorders | A | 30 | 14.6 | 0.888 | 1.045 | 0.565 | 1.935 |
| B | 26 | 12.6 | |||||
| Arousal disorders | A | 53 | 25.7 | 0.702 | 1.113 | 0.643 | 1.927 |
| B | 47 | 22.8 | |||||
| Sleep–wake transition disorders | A | 70 | 34.0 | 0.784 | 0.924 | 0.526 | 1.624 |
| B | 57 | 27.7 | |||||
| Excessive somnolence disorders | A | 38 | 18.4 | 0.013 ** | 2.032 | 1.158 | 3.567 |
| B | 48 | 23.3 | |||||
| Hyperhidrosis | A | 53 | 25.7 | 0.402 | 0.789 | 0.454 | 1.372 |
| B | 39 | 18.9 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diéguez-Pérez, M.; Burgueño-Torres, L.; Reichard-Monefeldt, G.; Tapia-Sierra, F.E.; Ticona-Flores, J.M. Prevalence and Characteristics of Sleep Disorders in Children Aged 7–17: Insights from Parental Observations at the Dental Office. Children 2024, 11, 609. https://doi.org/10.3390/children11050609
Diéguez-Pérez M, Burgueño-Torres L, Reichard-Monefeldt G, Tapia-Sierra FE, Ticona-Flores JM. Prevalence and Characteristics of Sleep Disorders in Children Aged 7–17: Insights from Parental Observations at the Dental Office. Children. 2024; 11(5):609. https://doi.org/10.3390/children11050609
Chicago/Turabian StyleDiéguez-Pérez, Montserrat, Laura Burgueño-Torres, Guillermo Reichard-Monefeldt, Fanny Esther Tapia-Sierra, and Jesús Miguel Ticona-Flores. 2024. "Prevalence and Characteristics of Sleep Disorders in Children Aged 7–17: Insights from Parental Observations at the Dental Office" Children 11, no. 5: 609. https://doi.org/10.3390/children11050609
APA StyleDiéguez-Pérez, M., Burgueño-Torres, L., Reichard-Monefeldt, G., Tapia-Sierra, F. E., & Ticona-Flores, J. M. (2024). Prevalence and Characteristics of Sleep Disorders in Children Aged 7–17: Insights from Parental Observations at the Dental Office. Children, 11(5), 609. https://doi.org/10.3390/children11050609






