Congenital Vascular Malformations in Children: From Historical Perspective to a Multidisciplinary Approach in the Modern Era—A Comprehensive Review
Abstract
1. Introduction
2. History
3. Etiology
4. Subtypes of Congenital Vascular Malformations
4.1. Arteriovenous Malformations
4.2. Venous Malformations
4.3. Lymphatic Malformations
5. Diagnosis
6. Treatment
6.1. Conservative
6.2. Surgery
6.3. Sclerotherapy/Embolization
6.4. Medical Therapy
7. Quality of Life
8. Future Perspectives
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tasnádi, G. Epidemiology and etiology of congenital vascular malformations. Semin. Vasc. Surg. 1993, 6, 200–203. [Google Scholar]
- Foley, L.S.; Kulungowski, A.M. Vascular Anomalies in Pediatrics. Adv. Pediatr. 2015, 62, 227–255. [Google Scholar] [CrossRef]
- Jondeau, G.; Hallac, J.; Hurard, M.; Daoud, K.; Barr, N.; Domnez, I. The VASCERN European Reference Network: An overview. Eur. J. Med. Genet. 2022, 65, 104420. [Google Scholar] [CrossRef]
- Mulliken, J.B.; Burrows, P.E.; Fishman, S.J. Classification of vascular anomalies. In Mulliken and Young’s Vascular Anomalies: Hemangiomas and Malformations; Oxford University Press: Oxford, UK, 2013; pp. 22–27. [Google Scholar]
- Mulliken, J.B.; Glowacki, J. Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast. Reconstr. Surg. 1982, 69, 412–422. [Google Scholar] [CrossRef]
- ISSVA Classification of Vascular Anomalies ©2018 International Society for the Study of Vascular Anomalies. Available online: https://www.issva.org/classification (accessed on 10 March 2024).
- Mulliken, J.B.; Burrows, P.E.; Fishman, S.J. Mulliken and Young’s Vascular Anomalies: Hemangiomas and Malformations; Oxford University Press: Oxford, UK, 2013; pp. 562–594. [Google Scholar]
- Martelli, E.; Piredda, F.; Catanese, V.; Donelli, C.; Pinna, A.; Usai, M. Vascular Embryology. In Vascular Surgery—Why, When, How, 1st ed.; Settembrini, P., Ed.; Minerva Medica: Turin, Italy, 2017; pp. 6–13. [Google Scholar]
- Borst, A.J.; Nakano, T.A.; Blei, F.; Adams, D.M.; Duis, J. A Primer on a Comprehensive Genetic Approach to Vascular Anomalies. Front. Pediatr. 2020, 8, 579591. [Google Scholar] [CrossRef]
- Nguyen, H.-L.; Boon, L.M.; Vikkula, M. Vascular Anomalies Caused by Abnormal Signaling within Endothelial Cells: Targets for Novel Therapies. Semin. Interv. Radiol. 2017, 34, 233–238. [Google Scholar] [CrossRef]
- Steiner, J.E.; Drolet, B.A. Classification of Vascular Anomalies: An Update. Semin. Interv. Radiol. 2017, 34, 225–232. [Google Scholar] [CrossRef]
- Kohout, M.P.; Hansen, M.; Pribaz, J.J.; Mulliken, J.B. Arteriovenous malformations of the head and neck: Natural history and management. Plast. Reconstr. Surg. 1998, 102, 643–654. [Google Scholar] [CrossRef]
- Fishman, S.J.; Mulliken, J.B. Hemangiomas and Vascular Malformations of Infancy and Childhood. Pediatr. Clin. N. Am. 1993, 40, 1177–1200. [Google Scholar] [CrossRef]
- Fraulin, F.O.; Flannigan, R.K.; Sharma, V.K.; McPhalen, D.F.; Harrop, R.A. The epidemiological profile of the Vascular Birthmark Clinic at the Alberta Children’s Hospital. Can. J. Plast. Surg. 2012, 20, 67–70. [Google Scholar] [CrossRef]
- Suami, H.; Lee, B.B. Congenital Vascular Malformations—A Comprehensive Review of Current Management; Springer: Berlin/Heidelberg, Germany, 2017; pp. 31–34. [Google Scholar]
- Schöbinger, R. Schöbinger classification of Arteriovenous Malformations. In Proceedings of the International Society for the Study of Vascular Anomalies Congress, Rome, Italy, 23–26 June 1996. [Google Scholar]
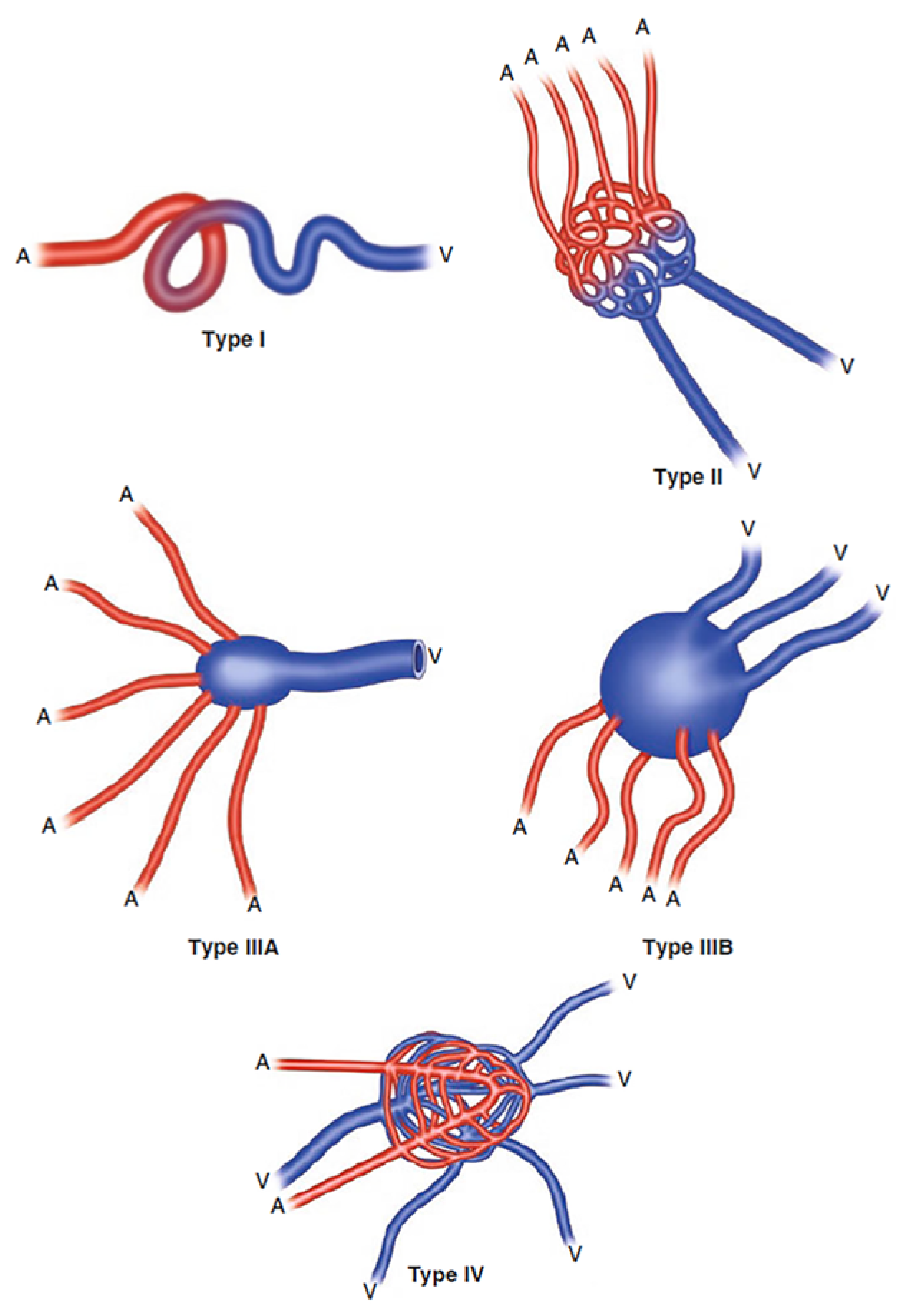
- Yakes, W.F.; Vogelzang, R.L.; Ivancev, K.; Yakes, A.M. New Arteriographic Classification of AVM Based on the Yakes Classification System. In Congenital Vascular Malformations—A Comprehensive review of Current Management; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Hu, L.; Chen, H.; Yang, X.; Wang, Y.; Gu, H.; Liu, M.; Lin, X. Risk factors associated with pain in patients with venous malformations of the extremities. Vasc. Med. 2019, 24, 56–62. [Google Scholar] [CrossRef]
- Baker, L.L.; Dillon, W.P.; Hieshima, G.B.; Dowd, C.F.; Frieden, I.J. Hemangiomas and vascular malformations of the head and neck: MR characterization. Am. J. Neuroradiol. 1993, 14, 307–314. [Google Scholar]
- Calligaris, L.; Berti, I.; Barbi, E. Phleboliths as a marker of slow-flow venous malformation. Arch. Dis. Child. 2015, 100, 1012. [Google Scholar] [CrossRef]
- Dompmartin, A.; Acher, A.; Thibon, P.; Tourbach, S.; Hermans, C.; Deneys, V.; Pocock, B.; Lequerrec, A.; Labbé, D.; Barrellier, M.-T.; et al. Association of localized intravascular coagulopathy with venous malformations. Arch. Dermatol. 2008, 144, 873–877. [Google Scholar] [CrossRef]
- Puig, S.; Aref, H.; Chigot, V.; Bonin, B.; Brunelle, F. Classification of venous malformations in children and implications for sclerotherapy. Pediatr. Radiol. 2003, 33, 99–103. [Google Scholar] [CrossRef]
- Eliasson, J.J.; Weiss, I.; Høgevold, H.E.; Oliver, N.; Andersen, R.; Try, K.; Tønseth, K.A. An 8-year population description from a national treatment centre on lymphatic malformations. J. Plast. Surg. Hand Surg. 2017, 51, 280–285. [Google Scholar] [CrossRef]
- Chaudry, G.; Guevara, C.J.; Rialon, K.L.; Kerr, C.; Mulliken, J.B.; Greene, A.K.; Fishman, S.J.; Boyer, D.; Alomari, A.I. Safety and efficacy of bleomycin sclerotherapy for microcystic lymphatic malformation. Cardiovasc. Interv. Radiol. 2014, 37, 1476–1481. [Google Scholar] [CrossRef]
- Defnet, A.M.; Bagrodia, N.; Hernandez, S.L.; Gwilliam, N.; Kandel, J.J. Pediatric lymphatic malformations: Evolving understanding and therapeutic options. Pediatr. Surg. Int. 2016, 32, 425–433. [Google Scholar] [CrossRef]
- Manning, S.C.; Perkins, J. Lymphatic malformations. Curr. Opin. Otolaryngol. Head Neck Surg. 2013, 21, 571–575. [Google Scholar] [CrossRef]
- Acevedo, J.L.; Shah, R.K.; Brietzke, S.E. Nonsurgical therapies for lymphangiomas: A systematic review. Otolaryngol. Neck Surg. 2008, 138, 418–424. [Google Scholar] [CrossRef]
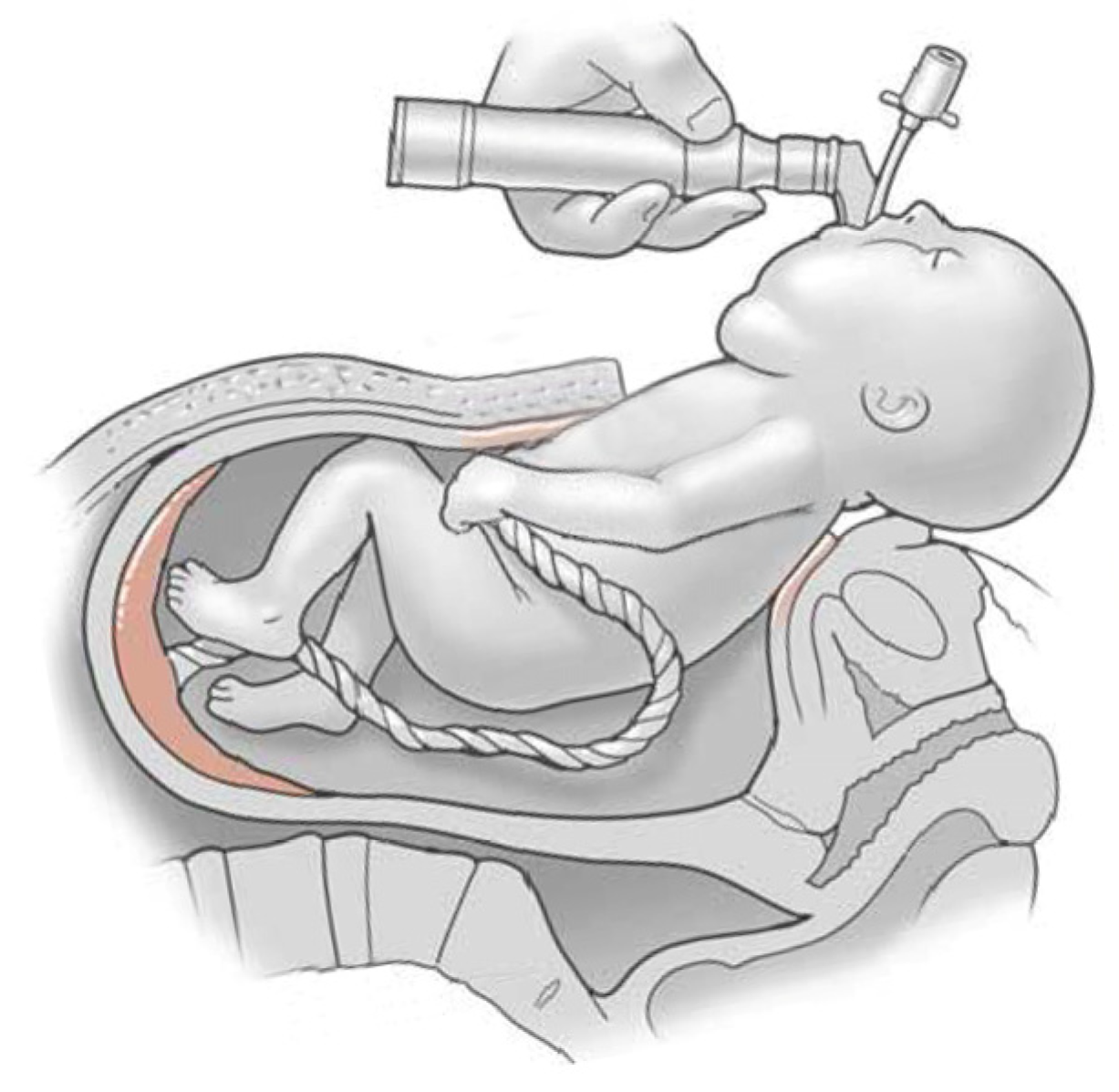
- Skarsgard, E.D.; Chitkara, U.; Krane, E.J.; Riley, E.T.; Halamek, L.P.; Dedo, H.H. The OOPS procedure (operation on placental support): In utero airway management of the fetus with prenatally diagnosed tracheal obstruction. J. Pediatr. Surg. 1996, 31, 826–828. [Google Scholar] [CrossRef]
- Bouwman, F.C.; Klein, W.M.; de Blaauw, I.; Woiski, M.D.; Verhoeven, B.H.; Botden, S.M. Lymphatic malformations adjacent to the airway in neonates: Risk factors for outcome. J. Pediatr. Surg. 2021, 56, 1764–1770. [Google Scholar] [CrossRef]
- Veld, M.I.; Fronczek, R.; dos Santos, M.P.; van Walderveen, M.A.A.; Meijer, F.J.A.; Willems, P.W.A. High sensitivity and specificity of 4D-CTA in the detection of cranial arteriovenous shunts. Eur. Radiol. 2019, 29, 5961–5970. [Google Scholar] [CrossRef]
- Thorburn, C.; Price, D. Expectant management of pediatric lymphatic malformations: A 30-year chart review. J. Pediatr. Surg. 2022, 57, 883–887. [Google Scholar] [CrossRef]
- Bonilla-Velez, J.; Whitlock, K.B.; Ganti, S.; Theeuwen, H.A.; Manning, S.C.; Bly, R.A.; Dahl, J.P.; Perkins, J.A. Active Observation as an Alternative to Invasive Treatments for Pediatric Head and Neck Lymphatic Malformations. Laryngoscope 2021, 131, 1392–1397. [Google Scholar] [CrossRef] [PubMed]
- Ramien, M.L.; Ondrejchak, S.; Gendron, R.; Hatami, A.; McCuaig, C.C.; Powell, J.; Marcoux, D. Quality of life in pediatric patients before and after cosmetic camouflage of visible skin conditions. J. Am. Acad. Dermatol. 2014, 71, 935–940. [Google Scholar] [CrossRef]
- Karunaratne, Y.G.; Greer, D.; Hong, L.H.; Somia, N.; Wargon, O.; Adams, S. Low-flow vascular malformations of the hand and forearm: A multidisciplinary experience in a tertiary paediatric centre. ANZ J. Surg. 2021, 91, 1739–1743. [Google Scholar] [CrossRef]
- Moreno-Alfonso, J.C.; Triana, P.; Ferrero, M.M.; González, M.D.; Gutiérrez, J.C.L. Risk factors for sequelae after surgery for lymphatic malformations in children. J. Vasc. Surg. Venous Lymphat. Disord. 2024, 12, 101730. [Google Scholar] [CrossRef]
- Laurian, C.; Bisdorff, A.; Masonni, C.; Cerceau, P.; Paraskevas, N. Surgical resection of venous malformations of the forearm. J. Hand Surg. 2022, 47, 716–721. [Google Scholar] [CrossRef]
- Ryu, J.Y.; Eo, P.S.; Lee, J.S.; Lee, J.W.; Lee, S.J.; Lee, J.M.; Lee, S.Y.; Huh, S.; Kim, J.Y.; Chung, H.Y. Surgical approach for venous malformation in the head and neck. Arch. Craniofacial Surg. 2019, 20, 304–309. [Google Scholar] [CrossRef]
- Hu, S.; Muss, T.E.; Toyoda, Y.; Kim, M.S.; Chang, A.E.; Banala, M.; Graham, E.M.; Gunturi, D.; Deepthi; Lin, I.C. Surgical Management of Vascular Malformations of the Upper Extremity: A 12-Year Retrospective Cohort Study. Ann. Plast. Surg. 2024, 92 (Suppl. S2), S132–S135. [Google Scholar] [CrossRef] [PubMed]
- Gasparella, P.; Flucher, C.; Beqo, B.P.; Schmidt, B.; Spendel, S.; Arneitz, C.; Till, H.; Haxhija, E.Q.; Singer, G. Outcome after surgical treatment of venous malformations of the hand in childhood. J. Vasc. Surg. Venous Lymphat. Disord. 2023, 11, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Bonilla-Velez, J.; Moore, B.P.; Cleves, M.A.; Buckmiller, L.; Richter, G.T. Surgical resection of macrocystic lymphatic malformations of the head and neck: Short and long-term outcomes. Int. J. Pediatr. Otorhinolaryngol. 2020, 134, 110013. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Du, J.; Liu, Y.; Zhang, J.; Ge, W.; Zhang, Y.; Guo, Y.; Li, Y.; Zhang, X.; Li, X.; et al. Clinical analysis of surgical treatment for head and neck lymphatic malformations in children: A series of 128 cases. Acta Otolaryngol. 2019, 139, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Hein, K.D.; Mulliken, J.B.; Kozakewich, H.P.W.; Upton, J.; Burrows, P.E. Venous malformations of skeletal muscle. Plast. Reconstr. Surg. 2002, 110, 1625–1635. [Google Scholar] [PubMed]
- Penington, A. Surgical Resection of an Arteriovenous Malformation. J. Vasc. Anom. 2021, 2, e009. [Google Scholar] [CrossRef]
- Chen, R.J.M.; Vrazas, J.I.M.; Penington, A.J.M. Surgical Management of Intramuscular Venous Malformations. J. Pediatr. Orthop. 2021, 41, e67–e73. [Google Scholar] [CrossRef] [PubMed]
- MacArthur, C.J.; Nesbit, G. Simultaneous intra-operative sclerotherapy and surgical resection of cervicofacial venous malformations. Int. J. Pediatr. Otorhinolaryngol. 2019, 118, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Puccia, R.; Staricha, K.; Carlberg, V.M.; Moe, D.; Chun, R. Utilizing immediate preoperative n-BCA in the resection of head and neck venous and lymphatic malformations. Int. J. Pediatr. Otorhinolaryngol. 2020, 138, 110388. [Google Scholar] [CrossRef]
- Caton, M.T.; Duvvuri, M.; Baker, A.; Smith, E.R.; Narsinh, K.H.; Amans, M.R.; Hetts, S.W.; Higashida, R.T.; Cooke, D.L.; Dowd, C.F. Percutaneous sclerotherapy for head and neck lymphatic malformations in neonates and infants ≤ 12 months of age. J. NeuroInterv. Surg. 2023, 15, 1242–1246. [Google Scholar] [CrossRef]
- Schmidt, V.F.; Masthoff, M.; Goldann, C.; Brill, R.; Sporns, P.B.; Segger, L.; Schulze-Zachau, V.; Takes, M.; Köhler, M.; Deniz, S.; et al. Multicentered analysis of percutaneous sclerotherapies in venous malformations of the face. Front. Med. 2022, 9, 1066412. [Google Scholar] [CrossRef] [PubMed]
- Bouwman, F.C.M.; Kooijman, S.S.; Verhoeven, B.H.; Kool, L.J.S.; van der Vleuten, C.J.M.; Botden, S.M.B.I.; de Blaauw, I. Lymphatic malformations in children: Treatment outcomes of sclerotherapy in a large cohort. Eur. J. Pediatr. 2021, 180, 959–966. [Google Scholar] [CrossRef] [PubMed]
- Park, K.B.; Do, Y.S.; Kim, D.-I.; Kim, Y.W.; Park, H.S.; Shin, S.W.; Cho, S.K.; Hyun, D.-H.; Choo, S.W. Endovascular treatment results and risk factors for complications of body and extremity arteriovenous malformations. J. Vasc. Surg. 2019, 69, 1207–1218. [Google Scholar] [CrossRef] [PubMed]
- Markovic, J.N.; Nag, U.; Shortell, C.K. Safety and efficacy of foam sclerotherapy for treatment of low-flow vascular malformations in children. J. Vasc. Surg. Venous Lymphat. Disord. 2020, 8, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Wu, Y.-X.; Zhang, M.-X.; Song, D.-Q.; Su, B.-L.; Li, S.-M.; Shan, W.-Y.; Liu, Z.-J.; Luo, C.-F.; Yu, L.-J. Efficacy of Bleomycin-Lauromacrogol Foam in Pediatric Macrocystic Lymphatic Malformations with and Without Intracapsular Hemorrhage. J. Pediatr. Surg. 2024. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.; Yeung, P.; Heran, M.; Courtemanche, D.; Chadha, N.; Baird, R. Sclerosing agents in the management of lymphatic malformations in children: A systematic review. J. Pediatr. Surg. 2022, 57, 888–896. [Google Scholar] [CrossRef] [PubMed]
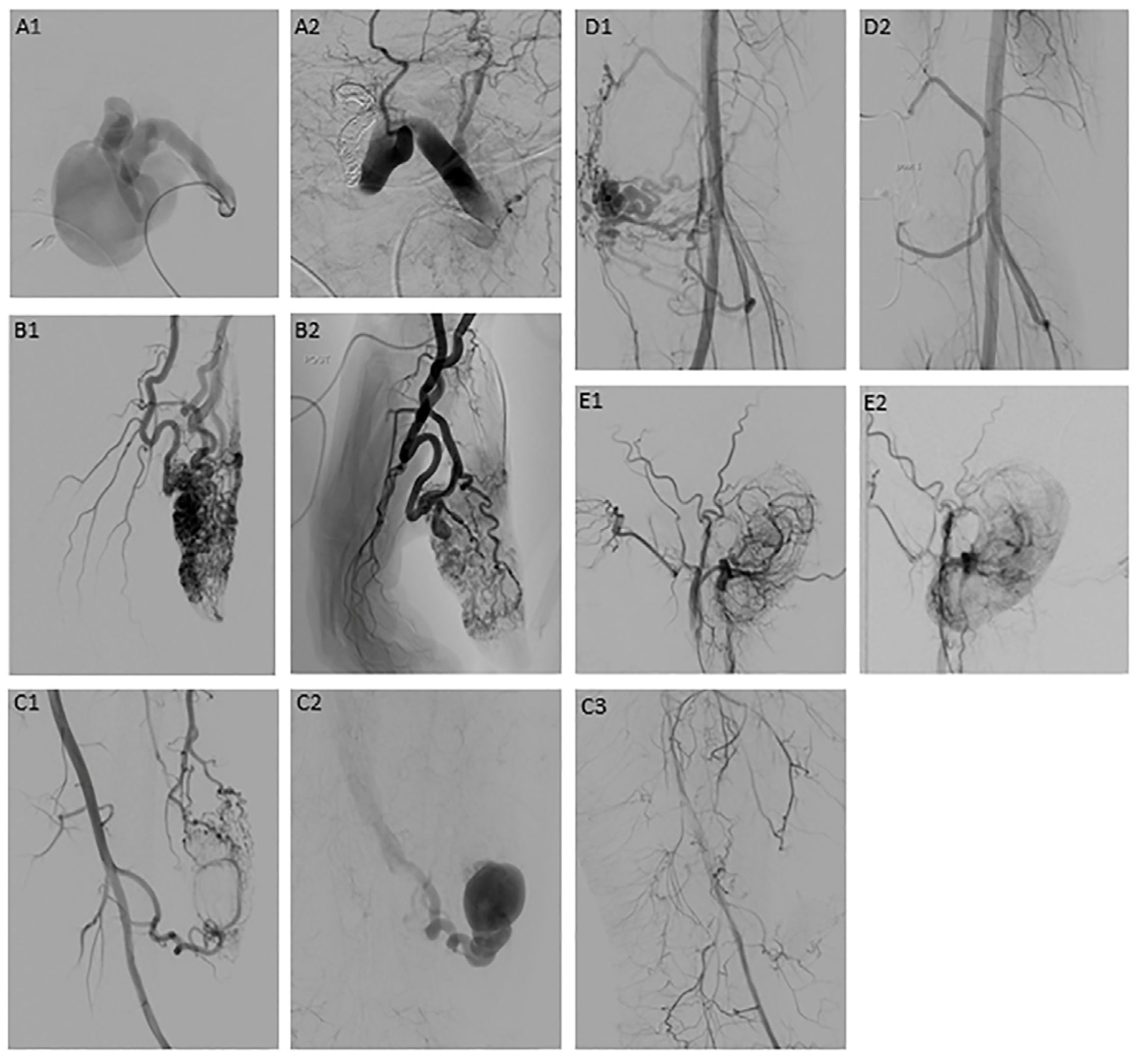
- Bouwman, F.C.; Botden, S.M.; Verhoeven, B.H.; Kool, L.J.S.; van der Vleuten, C.J.; de Blaauw, I.; Klein, W.M. Treatment Outcomes of Embolization for Peripheral Arteriovenous Malformations. J. Vasc. Interv. Radiol. 2020, 31, 1801–1809. [Google Scholar] [CrossRef]
- Pfeifer, J.; Wohlgemuth, W.A.; Abdul-Khaliq, H. Liquid Embolization of Peripheral Arteriovenous Malformations with Ethylene-Vinyl Alcohol Copolymer in Neonates and Infants. Cardiovasc. Ther. 2022, 2022, 1022729. [Google Scholar] [CrossRef] [PubMed]
- Hou, F.; Chen, J.; Xia, M.; Ding, K.; Zeng, Q.; Liu, W. Percutaneous sclerotherapy with polidocanol under the guidance of ultrasound for venous malformations in children—A retrospective cohort study from a single tertiary medical center. Medicine 2020, 99, e18839. [Google Scholar] [CrossRef]
- Caton, M.T.; Baker, A.; Smith, E.R.; Perez, E.; Hemphill, K.; Cooke, D.L.; Dowd, C.F. Dual-agent percutaneous sclerotherapy technique for macrocystic lymphatic malformations. J. NeuroInterv. Surg. 2023, 15, 931. [Google Scholar] [CrossRef]
- Yakes, W.F. Use of Multiple Sclerosant Agents in Vascular Malformation Management: A World in Endovascular Confusion and Chaos. J. Vasc. Interv. Radiol. 2015, 26, 1494–1496. [Google Scholar] [CrossRef] [PubMed]
- Hyun, D.; Do, Y.S.; Park, K.B.; Kim, D.-I.; Kim, Y.W.; Park, H.S.; Shin, S.W.; Song, Y.G. Ethanol embolotherapy of foot arteriovenous malformations. J. Vasc. Surg. 2013, 58, 1619–1626. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Park, H.S.; Do, Y.S.; Park, K.B.; Kim, D.-I.; Kim, Y.W.; Kim, M.J.; Shin, B.S.; Choo, I.W. Ethanol embolotherapy of hand arteriovenous malformations. J. Vasc. Surg. 2011, 53, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Zochowski, C.G.; Salgado, C.J.; Jamali, A.A. Extensive muscle necrosis and infection following treatment of a lower extremity vascular malformation with Sotradecol and absolute ethanol. Blood Coagul. Fibrinolysis 2010, 21, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, P.; Dubois, J.; Giroux, M.F.; Soulez, G. New Treatment Approaches to Arteriovenous Malformations. Semin. Interv. Radiol. 2017, 34, 258–271. [Google Scholar] [CrossRef] [PubMed]
- Nassiri, N.; Cirillo-Penn, N.C.; Thomas, J. Evaluation and management of congenital peripheral arteriovenous malformations. J. Vasc. Surg. 2015, 62, 1667–1676. [Google Scholar] [CrossRef] [PubMed]
- Chapot, R.; Laurent, A.; Enjolras, O.; Payen, D.; Houdart, E. Fatal cardiovascular collapse during ethanol sclerotherapy of a venous malformation. Interv. Neuroradiol. 2002, 8, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Su, L.; Fan, X. Cardiovascular collapse and disseminated intravascular coagulation as complications of ethanol embolization of arteriovenous malformations in the upper lip: Case report and literature review. J. Oral Maxillofac. Surg. 2014, 72, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Khera, D.; Bhatnagar, A.; Khera, P.S.; Kumar, P. Percutaneous Sclerotherapy of Superficial Vascular Malformation Leading to Bleomycin Induced Lung Injury and Lipoid Pneumonia. Indian J. Pediatr. 2019, 86, 97–98. [Google Scholar] [CrossRef]
- Atwa, K.; Abuhasna, S.; Shihab, Z.; Hashaykeh, N.; Hasan, R. Acute pulmonary toxicity following intralesional administration of bleomycin for a lymphovenous malformation. Pediatr. Pulmonol. 2010, 45, 192–196. [Google Scholar] [CrossRef]
- Cho, A.L.; Kiang, S.C.; Lodenkamp, J.; Tritch, W.T.H.; Tomihama, R.T. Fatal Lung Toxicity After Intralesional Bleomycin Sclerotherapy of a Vascular Malformation. Cardiovasc. Interv. Radiol. 2020, 43, 648–651. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, N.; Lorenz, J.; Hohenstatt, S.; Semmelmayer, K.; Ruping, F.; Hoffmann, J.; Günther, P.; Bendszus, M.; Möhlenbruch, M.A.; Vollherbst, D.F. Sclerotherapy of Venous Malformations Using Polidocanol: Effectiveness, Safety, and Predictors of Outcomes and Adverse Events. J. Vasc. Interv. Radiol. 2023, 34, 2103–2109. [Google Scholar] [CrossRef] [PubMed]
- Hyvönen, H.; Salminen, P.; Kyrklund, K. Long-term outcomes of lymphatic malformations in children: An 11-year experience from a tertiary referral center. J. Pediatr. Surg. 2022, 57, 1005–1010. [Google Scholar] [CrossRef] [PubMed]
- Do, Y.S.; Kim, Y.-W.; Park, K.B.; Kim, D.-I.; Park, H.S.; Cho, S.K.; Shin, S.W.; Park, Y.J. Endovascular treatment combined with emboloscleorotherapy for pelvic arteriovenous malformations. J. Vasc. Surg. 2012, 55, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Wagner, K.M.; Lokmic, Z.; Penington, A.J. Prolonged antibiotic treatment for infected low flow vascular malformations. J. Pediatr. Surg. 2018, 53, 798–801. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, K.Y.; Russell, S.; Wargon, O.; Adams, S. Localised intravascular coagulation complicating venous malformations in children: Associations and therapeutic options. J. Paediatr. Child Health 2017, 53, 737–741. [Google Scholar] [CrossRef]
- Liu, H.; Hu, L.; Yang, X.; Xu, Z.; Gu, H.; Chen, H.; Lin, X. Dabigatran etexilate is efficacious in consumptive coagulopathy and pain associated with venous malformations. J. Vasc. Surg. Venous Lymphat. Disord. 2023, 11, 397–403.e1. [Google Scholar] [CrossRef] [PubMed]
- Ge, Z.; Chen, H.; Gao, Y.; Liu, W.; Xu, C.; Tan, H.; Chen, H.; Wei, W.; Fang, J.; Xiao, S. Efficacy of Thalidomide for Refractory Gastrointestinal Bleeding from Vascular Malformation. Gastroenterology 2011, 141, 1629–1637.e4. [Google Scholar] [CrossRef] [PubMed]
- Adams, D.M.; Trenor, C.C.; Hammill, A.M.; Vinks, A.A.; Patel, M.N.; Chaudry, G.; Wentzel, M.S.; Mobberley-Schuman, P.S.; Campbell, L.M.; Brookbank, C.; et al. Efficacy and Safety of Sirolimus in the Treatment of Complicated Vascular Anomalies. Pediatrics 2016, 137, e20153257. [Google Scholar] [CrossRef]
- Engel, E.R.; Hammill, A.; Adams, D.; Phillips, R.J.; Jeng, M.; Tollefson, M.M.; Iacobas, I.; Schiff, D.; Greenberger, S.; Kelly, M.; et al. Response to sirolimus in capillary lymphatic venous malformations and associated syndromes: Impact on symptomatology, quality of life, and radiographic response. Pediatr. Blood Cancer 2023, 70, e30215. [Google Scholar] [CrossRef]
- Seront, E.; Van Damme, A.; Legrand, C.; Bisdorff-Bresson, A.; Orcel, P.; Funck-Brentano, T.; Sevestre, M.-A.; Dompmartin, A.; Quere, I.; Brouillard, P.; et al. Preliminary results of the European multicentric phase III trial regarding sirolimus in slow-flow vascular malformations. JCI Insight 2023, 8, e173095. [Google Scholar] [CrossRef] [PubMed]
- Harbers, V.E.M.; Zwerink, L.G.J.M.; Rongen, G.A.; Klein, W.M.; van der Vleuten, C.J.M.; van Rijnsoever, I.M.P.; Gerdsen-Drury, L.; Flucke, U.E.; Verhoeven, B.H.; de Laat, P.C.J.; et al. Clinical differences in sirolimus treatment with low target levels between children and adults with vascular malformations—A nationwide trial. Clin. Transl. Sci. 2023, 16, 781–796. [Google Scholar] [CrossRef]
- Ji, Y.; Chen, S.; Yang, K.; Zhou, J.; Zhang, X.; Jiang, X.; Xu, X.; Lu, G.; Qiu, L.; Kong, F.; et al. A prospective multicenter study of sirolimus for complicated vascular anomalies. J. Vasc. Surg. 2021, 74, 1673–1681.e3. [Google Scholar] [CrossRef]
- Maruani, A.; Tavernier, E.; Boccara, O.; Mazereeuw-Hautier, J.; Leducq, S.; Bessis, D.; Guibaud, L.; Vabres, P.; Carmignac, V.; Mallet, S.; et al. Sirolimus (Rapamycin) for Slow-Flow Malformations in Children: The Observational-Phase Randomized Clinical PERFORMUS Trial. JAMA Dermatol. 2021, 157, 1289–1298. [Google Scholar] [CrossRef] [PubMed]
- Tian, R.; Liang, Y.; Zhang, W.; Wang, J.; Shan, Y.; Gao, H.; Xie, C.; Li, J.; Xu, M.; Gu, S. Effectiveness of sirolimus in the treatment of complex lymphatic malformations: Single center report of 56 cases. J. Pediatr. Surg. 2020, 55, 2454–2458. [Google Scholar] [CrossRef]
- Kolitz, E.B.; Fernandes, N.J.; Agim, N.G.; Ludwigl, K. Response to Alpelisib in Clinically Distinct Pediatric Patients With PIK3CA-related Disorders. J. Pediatr. Hematol./Oncol. 2022, 44, 482–485. [Google Scholar] [CrossRef]
- Remy, A.; Tran, T.H.; Dubois, J.; Gavra, P.; Lapointe, C.; Winikoff, R.; Facundo, G.-B.; Théorêt, Y.; Kleiber, N. Repurposing alpelisib, an anti-cancer drug, for the treatment of severe TIE2-mutated venous malformations: Preliminary pharmacokinetics and pharmacodynamic data. Pediatr. Blood Cancer 2022, 69, e29897. [Google Scholar] [CrossRef]
- Chowers, G.; Abebe-Campino, G.; Golan, H.; Vivante, A.; Greenberger, S.; Soudack, M.; Barkai, G.; Fox-Fisher, I.; Li, D.; March, M.; et al. Treatment of severe Kaposiform lymphangiomatosis positive for NRAS mutation by MEK inhibition. Pediatr. Res. 2023, 94, 1911–1915. [Google Scholar] [CrossRef]
- Nguyen, H.L.; Bonadurer, G.F.; Tollefson, M.M. Tollefson, Vascular Malformations and Health-Related Quality of Life: A Systematic Review and Meta-analysis. JAMA Dermatol. 2018, 154, 661–669. [Google Scholar] [CrossRef]
- Horbach, S.; van der Horst, C.; Blei, F.; van der Vleuten, C.; Frieden, I.J.; Richter, G.; Tan, S.; Muir, T.; Penington, A.; Boon, L.; et al. Development of an international core outcome set for peripheral vascular malformations: The OVAMA project. Br. J. Dermatol. 2018, 178, 473–481. [Google Scholar] [CrossRef]
- Bouwman, F.C.M.; Verhaak, C.; de Blaauw, I.; Kool, L.J.S.; Loo, D.M.W.M.T.; van Rooij, I.A.L.M.; van der Vleuten, C.J.M.; Botden, S.M.B.I.; Verhoeven, B.H. Health-related quality of life in children with congenital vascular malformations. Eur. J. Pediatr. 2023, 182, 5067–5077. [Google Scholar] [CrossRef]
- Arleo, T.L.; Swerdlin, R.F.D.; Gill, A.E.; Goudy, S.L.; Meisel, J.A.; Briones, M.A.; Shah, J.H.; Wright, A.R.; Hawkins, C.M. Baseline Quality of Life in Pediatric Patients with Low-flow Vascular Malformations. J. Pediatr. Hematol./Oncol. 2023, 45, e847–e856. [Google Scholar] [CrossRef]
- Lokhorst, M.; Horbach, S.; Waner, M.; O, T.M.; Vleuten, C.; Mokkink, L.; Horst, C.; Spuls, P. Responsiveness of quality-of-life measures in patients with peripheral vascular malformations: The OVAMA project. Br. J. Dermatol. 2020, 182, 1395–1403. [Google Scholar] [CrossRef]
- Wohlgemuth, W.A.; Müller-Wille, R.; Teusch, V.; Hammer, S.; Wildgruber, M.; Uller, W. Ethanolgel sclerotherapy of venous malformations improves health-related quality-of-life in adults and children—Results of a prospective study. Eur. Radiol. 2017, 27, 2482–2488. [Google Scholar] [CrossRef]
- Ghaffarpour, N.; Claesson, G.; Wester, T.; Boman, K.K. Long-term health-related quality of life in children with lymphatic malformations treated with sclerotherapy generally matched age-appropriate standardised population norms. Acta Paediatr. 2019, 108, 1499–1506. [Google Scholar] [CrossRef]
- Schmidt, V.F.; Masthoff, M.; Vielsmeier, V.; Seebauer, C.T.; Cangir, Ö.; Meyer, L.; Mükke, A.; Lang, W.; Schmid, A.; Sporns, P.B.; et al. Clinical Outcome and Quality of Life of Multimodal Treatment of Extracranial Arteriovenous Malformations: The APOLLON Study Protocol. Cardiovasc. Interv. Radiol. 2023, 46, 142–151. [Google Scholar] [CrossRef]
- Harbers, V.E.M.; Bouwman, F.C.M.; van Rijnsoever, I.M.P.; Verhoeven, B.H.; van der Vleuten, C.J.M.; Kool, L.J.S.; de Laat, P.C.J.; van der Horst, C.M.A.M.; Kievit, W.; Loo, D.M.W.M.T. Magnitude and relevance of change in health-related quality of life in patients with vascular malformations treated with sirolimus. Front. Med. 2023, 10, 1155476. [Google Scholar] [CrossRef]
- Horbach, S.E.R.; van de Ven, J.S.; Nieuwkerk, P.T.; Spuls, P.I.; van der Horst, C.M.A.M.; Reekers, J.A. Patient-Reported Outcomes of Bleomycin Sclerotherapy for Low-Flow Vascular Malformations and Predictors of Improvement. Cardiovasc. Interv. Radiol. 2018, 41, 1494–1504. [Google Scholar] [CrossRef]
- Breugem, C.C.; Merkus, M.P.; Smitt, J.S.; Legemate, D.A.; van der Horst, C.M. Quality of life in patients with vascular malformations of the lower extremity. Br. J. Plast. Surg. 2004, 57, 754–763. [Google Scholar] [CrossRef]
- Fahrni, J.O.; Cho, E.-Y.N.; Engelberger, R.P.; Baumgartner, I.; von Känel, R. Quality of life in patients with congenital vascular malformations. J. Vasc. Surg. Venous Lymphat. Disord. 2014, 2, 46–51. [Google Scholar] [CrossRef]
- Pang, C.; Gibson, M.; Nisbet, R.; Evans, N.; Khalifa, M.; Papadopoulou, A.; Tsui, J.; Hamilton, G.; Brookes, J.; Lim, C.S. Quality of life and mental health of patients with vascular malformations in a single specialist center in the United Kingdom. J. Vasc. Surg. Venous Lymphat. Disord. 2022, 10, 159–169. [Google Scholar] [CrossRef]
- Seront, E.; Biard, J.M.; Van Damme, A.; Revencu, N.; Lengelé, B.; Schmitz, S.; de Toeuf, C.; Clapuyt, P.; Veyckemans, F.; Prégardien, C.; et al. A case report of sirolimus use in early fetal management of lymphatic malformation. Nat. Cardiovasc. Res. 2023, 2, 595–599. [Google Scholar] [CrossRef]
- Livingston, J.; Alrowaily, N.; John, P.; Campisi, P.; Ranguis, S.; Van Mieghem, T.; Carcao, M.; Ryan, G. Fetal therapy using rapamycin for a rapidly enlarging, obstructive, cervical lymphatic malformation: A case report. Prenat. Diagn. 2021, 41, 884–887. [Google Scholar] [CrossRef]
- Lokhorst, M.; Horbach, S.; Young-Afat, D.; Stor, M.; Haverman, L.; Spuls, P.; Horst, C.; the OVAMA Steering Group. Development of a condition-specific patient-reported outcome measure for measuring symptoms and appearance in vascular malformations: The OVAMA questionnaire. Br. J. Dermatol. 2021, 185, 797–803. [Google Scholar] [CrossRef]
| Stage I—quiescence | Pink-bluish stain, warmth, arteriovenous shunting on Doppler |
| Stage II—expansion | Stage I plus enlargement, pulsations, thrill, bruit and tortuous/tense veins |
| Stage III—destruction | Stage II plus dystrophic skin changes, ulceration, bleeding, tissue necrosis. Lytic bone lesions may occur. |
| Stage IV—decompensation | Stage III plus congestive cardiac failure with increased cardiac output and left ventricle hypertrophy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bouwman, F.C.M.; Verhoeven, B.H.; Klein, W.M.; Schultze Kool, L.J.; de Blaauw, I. Congenital Vascular Malformations in Children: From Historical Perspective to a Multidisciplinary Approach in the Modern Era—A Comprehensive Review. Children 2024, 11, 567. https://doi.org/10.3390/children11050567
Bouwman FCM, Verhoeven BH, Klein WM, Schultze Kool LJ, de Blaauw I. Congenital Vascular Malformations in Children: From Historical Perspective to a Multidisciplinary Approach in the Modern Era—A Comprehensive Review. Children. 2024; 11(5):567. https://doi.org/10.3390/children11050567
Chicago/Turabian StyleBouwman, Frédérique C. M., Bas H. Verhoeven, Willemijn M. Klein, Leo J. Schultze Kool, and Ivo de Blaauw. 2024. "Congenital Vascular Malformations in Children: From Historical Perspective to a Multidisciplinary Approach in the Modern Era—A Comprehensive Review" Children 11, no. 5: 567. https://doi.org/10.3390/children11050567
APA StyleBouwman, F. C. M., Verhoeven, B. H., Klein, W. M., Schultze Kool, L. J., & de Blaauw, I. (2024). Congenital Vascular Malformations in Children: From Historical Perspective to a Multidisciplinary Approach in the Modern Era—A Comprehensive Review. Children, 11(5), 567. https://doi.org/10.3390/children11050567





