Abstract
Background/Objectives: Preparing families to support children after hospital discharge is crucial, particularly due to the fragile health of pediatric patients and the care required at home. In this study, the aim was to assess the readiness for hospital discharge among primary caregivers of pediatric patients in medical–surgical units in Jeddah, Saudi Arabia, and to identify factors influencing their preparedness. Methods: A quantitative cross-sectional study was conducted among 258 primary caregivers recruited from two hospitals in Jeddah: King Abdulaziz University Hospital (KAUH) and a Ministry of Health (MOH) hospital. A purposive sampling method was used. Data were collected through the Pediatric Readiness for Hospital Discharge Scale (Ped-RHDS) and the Quality of Discharge Teaching Scale (QDTS), translated into Arabic. Descriptive statistics, t-tests, and multiple regression analyses were employed to identify key predictors of discharge readiness. Results: Caregivers reported moderate to high readiness for discharge, with mean scores of 8.28 (SD = 2.65) for personal strength and 8.62 (SD = 2.26) for their child’s strength. Knowledge scores averaged 7.49 (SD = 3.27). The quality of discharge teaching was higher at KAUH (M = 6.43, SD = 2.56) than at the MOH hospital (M = 5.48, SD = 2.89, p = 0.006). Caregiver age, child age, and discharge teaching quality were significant predictors of readiness (p < 0.05). Conclusions: In this study, the importance of discharge readiness is emphasized, highlighting the role of discharge education in enhancing preparedness. Addressing caregivers’ specific needs, especially for younger children or prolonged stays, can improve readiness and reduce post-discharge complications.
1. Introduction
Preparing families to support their children after hospital discharge is complex and intricate. Research on preparedness for discharge is gaining importance due to the fragile health of pediatric patients and the elevated level of care required at home [1]. More than one-fifth of caregivers encounter readiness difficulties when transitioning their child’s care from the hospital to the home [2]. An estimated one out of five families experience a readmission or emergency room visit due to a failure to comprehend discharge instructions [3]. The transition from hospital to home-based care is greatly influenced by the readiness of caregivers for discharge, which is particularly true for primary caregivers of children who often face significant challenges in providing care after discharge [4]. The term “primary caregiver” is defined as “the individual who provides the greatest amount of care to and accepts responsibility for the sick child during the illness, treatment, and rehabilitation process” [5]. Therefore, caregivers need support in helping children adjust well when transitioning to home.
Patient readiness for hospital discharge (RHD) was defined by Fenwick [6] as an ability to cope with the realities of life after hospitalization. Discharge readiness is an outcome indication of proper hospital care [7]. According to a study conducted by Berry et al. [8], parental preparedness for discharge correlates with the incidence of unplanned 30-day readmissions. Assessing discharge readiness is crucial for improving patient safety, satisfaction, and outcomes during the transition from hospital- to home-based recovery and care [9,10]. As per the analysis by Galvin et al. [11], readiness for hospital discharge has the four following dimensions: (a) functional ability, which involves the capability to take care of oneself at home; (b) having appropriate support in place to assist with post-hospital tasks; (c) being psychologically prepared to handle the process of change; and (d) knowing how to manage their own care and address minor issues that may arise after leaving the hospital. The readiness for discharge of the caregiver involves objectively evaluating the patient’s capacity to recover post-discharge, as well as considering the caregiver’s personal perception of the readiness for discharge [12]. The perceptions of patients and their families regarding readiness serve as crucial indicators of the discharge preparation process. These perceptions offer insight into the potential risks associated with a challenging post-discharge transition, which may result in adverse outcomes and readmission [4].
Nurses play a crucial role in preparing the family before hospital discharge; discharge planning is critical to completing the patient’s recovery process [13,14]. Implementing an assessment that identifies patients with low readiness for hospital discharge can assist nurses and other healthcare professionals improve patient readiness and prevent problematic discharges [15]. The primary approach employed by nurses for the preparation of patients and their families for discharge and the subsequent transition home from the hospital is through the provision of comprehensive education and instruction [16].
Several factors may affect caregivers’ readiness for discharge from a hospital setting to the home, such as satisfaction with hospitalization experience [17], quality of discharge education [18], and age-related vulnerabilities [19]. In contrast to clinical criteria for assessing readiness, the authors of [20] contend that the quality of discharge education largely predicts discharge readiness. Effective discharge teaching significantly improves caregivers’ capabilities, reduces the ambiguity surrounding their child’s illness, and enhances their confidence in being prepared for discharge [21]. Previous studies have highlighted the unique challenges and needs specific to these populations, emphasizing the importance of tailored discharge planning to ensure caregivers are adequately prepared for the transition to home care. However, there is a notable lack of comprehensive data that provide an overview of caregiver experiences in general pediatric hospitalizations, leaving a gap in understanding the broader scope of discharge readiness across more diverse pediatric patient populations [22].
There are evident adverse outcomes related to low perceptions of discharge readiness; additionally, the quality of discharge education plays a significant role in supporting the family transition home after hospitalization. To our knowledge, there is a limited number of studies to support pediatric patients and their caregivers transition post-discharge. In Saudi Arabia, the research concerning discharge readiness has not yet been implemented.
2. Materials and Methods
2.1. Theoretical Framework
Meleis’ middle-range theory of transition will be utilized as a conceptual framework for examining the transition for pediatric primary caregivers during discharge from a hospital to a patient’s home. This middle-range theory aims to investigate, understand, and forecast the experiences of individuals during various kinds of transitions, including transitions related to health and illness, situational changes, personal growth, and organizational shifts. Based on Meleis [23], transitions theory consists of the following major concepts: types and patterns of transitions, properties of transition experiences, transition conditions (facilitators and inhibitors), patterns of response/process and outcome indicators, and nursing therapeutics. Figure 1 illustrates the hypothesized theoretical framework.
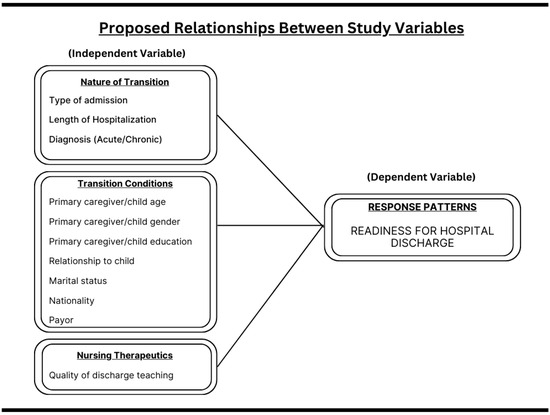
Figure 1.
Hypothesized theoretical framework.
2.2. Research Design
In this study, a quantitative cross-sectional design was used to examine phenomena or relationships at a specific time [24].
2.3. Target Population
The target population consisted of the primary caregivers of pediatric patients admitted to the medical and surgical pediatric units at a university hospital and a governmental hospital under the Ministry of Health (MOH) in Jeddah, Saudi Arabia. These caregivers were responsible for providing care during hospitalization and after discharge. They were recruited from pediatric inpatient units.
2.4. Sampling
Sample size determination is critical in research planning [25]. The sample size was calculated using G*Power 3.1 [26]. A two-tailed test with an effect size of 0.15, 5% significance level, and 0.95 power yielded a minimum required sample size of 214. To account for potential missing data, 20% more participants were added, resulting in a total sample size of 257 [27].
2.5. Sampling Design
A purposive (non-probability sampling) was used to recruit 257 primary caregivers from medical and surgical pediatric units. Purposive sampling involves deliberately selecting individuals with unique characteristics or experiences relevant to the study [28]. While this method is cost-effective and widely used, it has the drawback of potential researcher bias in the selection process [29,30].
2.6. Inclusion and Exclusion Criteria
The sample consisted of primary caregivers of hospitalized children from King Abdulaziz University Hospital (KAUH) and a Ministry of Health (MOH) hospital in Jeddah, Saudi Arabia. Inclusion criteria were as follows: (a) caregivers aged 18 or older with a child aged 18 or younger; (b) discharge to the home setting; (c) primary responsibility for the child’s care after discharge; and (d) sufficient Arabic language skills for consent and study participation. Caregivers of children discharged to hospice care and transferred to extended care were excluded.
2.7. Procedure of Data Collection
Daily discharge lists were obtained from discharge instructors and in-charge nurses at the KAUH and MOH hospitals. Caregivers were recruited within four hours of discharge after the principal investigator introduced this study. A demographic survey, Ped-RHDS, and QDTS data were collected from eligible participants. Consent was obtained, and caregivers completed electronic forms on iPads/tablets to facilitate data collection and analysis. Ethical approval was secured from the KAUH and MOH hospitals’ committees, and the principal investigator personally handled data collection with the help of trained nursing interns.
2.8. Variables and Their Measurement
Three instruments were used, a Demographic questionnaire, the Quality of Discharge Teaching Scale (QDTS), and the Readiness for Hospital Discharge Scale (RHDS).
2.8.1. Demographic Questionnaire
A 10-question survey gathered demographic information divided into (a) nature of transition (admission type, diagnosis, length of stay) and (b) transition conditions (caregiver/child age, caregiver gender, relationship to child, marital status, nationality, payor, and education level).
2.8.2. Readiness for Hospital Discharge Scale (Ped-RHDS)
The Ped-RHDS measures caregivers’ readiness for pediatric discharge, assessing knowledge for post-discharge care, personal and emotional status, coping ability, and expected support [20]. In this study, the short form (8 items) was used to reduce survey fatigue, which can affect response accuracy [31]. The Ped-RHDS is scored on a 10-point Likert scale (0 to 10), with higher scores indicating greater discharge readiness. The Cronbach’s alpha for the Ped-RHDS is 0.73, confirming its reliability [4].
2.8.3. Quality of Discharge Teaching Scale (QDTS)
The QDTS, developed by Dr. Weiss, evaluates the effectiveness of discharge teaching [32]. It consists of 19 items across the following three subscales: needed content, received content, and delivered content. Responses are measured on a 10-point Likert scale. The tool is highly reliable, with a Cronbach’s alpha of 0.88 for caregivers of hospitalized children [33].
These instruments assessed the independent variable (quality of discharge teaching, 19 items) and the dependent variable (readiness for hospital discharge, 8 items), measured at the interval level. Demographic data, measured at nominal and ordinal levels, were also included to explore their influence on the study outcomes. This comprehensive approach aims to enhance healthcare practices for patient discharge and inform policymakers to improve patient outcomes.
2.9. Tool Translation
Following Weiss et al. [20], and a thorough literature review, the original QDTS and Ped-RHDS tools were developed in English. A rigorous translation process, including forward and back translation, was employed to ensure accuracy [28]. Independent translators handled both stages. Permission for translation was obtained from Dr. Weiss. The translation from English to Arabic involved four Ph.D.-qualified experts proficient in both languages. Two experts conducted the forward translation, followed by a back translation by another two experts. This approach ensured the target version remained faithful to the original text [34]. Dr. Weiss supervised the process, providing guidance and feedback at each stage to ensure accuracy and consistency. The translation team included Dr Adel Bashatah (King Saud University), Dr Sabria Johar (King Saud bin Abdulaziz University for Health Sciences), and Dr Rasha AlSaiegh and Dr Salmah Alghamdi (King Abdulaziz University). Their expertise in nursing and language studies and commitment contributed to the high-quality final translation.
2.10. Pilot Study
Performing a pilot test is essential in identifying potential issues before initiating the final study and determining feasibility. A pilot study was conducted with 30 participants, representing 10% of the sample size, to test research protocols, data collection instruments, and recruitment strategies [28]. The pilot evaluated the feasibility, duration, and design of this study, as well as the applicability of the translated tool. The pilot study was conducted from 2 November 2023 to 15 January 2024. Participants in the pilot study were excluded from the main research to ensure the validity of the results.
3. Results
3.1. Preparation for Data Analysis
Data preparation was essential for the statistical analysis. SPSS (versions 26 and 28) was used for its reliability and established use in quantitative analysis. Demographic data, such as admission type, diagnosis, and caregiver details, were collected via a questionnaire. The raw data were exported from Google Forms, organized in Excel, and imported into SPSS for analysis.
Two key instruments, the Pediatric Readiness for Hospital Discharge Scale (Ped-RHDS) and the Quality of Discharge Teaching Scale (QDTS), both used a 10-point Likert scale. Higher scores indicated greater discharge readiness or higher perceived quality. The 10-point scale improved construct validity [35], and the Likert scales with five or more options were suitable for parametric analysis [36]. All variables were properly labeled in SPSS, and data accuracy was verified by comparing dataset codes with original values. The absence of reverse-coded items simplified interpretation. The analysis followed five steps:
- Descriptive statistics were used to describe demographic characteristics and readiness for discharge.
- Overall readiness was defined by the mean of the items in each category to provide an average measure of responses.
- Assumption checks were conducted to ensure the validity of each statistical test.
- Multiple regression analysis predicted the relationship between readiness for discharge (dependent variable) and other factors (independent variables) using a stepwise selection method. F-statistics and p-values (≤0.05) determined the best model fit and significant variables [37].
- T-tests compared the means between hospitals for overall readiness and quality of discharge, assessing statistical significance [38].
3.2. Data Analysis
3.2.1. Demographic and Hospitalization Characteristics
A total of 258 pediatric primary caregivers participated in this study. Most admissions (86.0%) occurred through the emergency department, with 8.1% through clinics and 5.8% being planned admissions. Regarding diagnosis, 47.7% of the children had acute conditions, 45.3% had chronic conditions, and 7.0% were admitted for planned operations. The majority of caregivers were female (98.1%), with mothers accounting for 93.4% of the sample. The average caregiver age was 34.04 years (SD = 7.6), and the majority of children were either in childhood (54.7%) or infancy (34.9%). The average length of hospital stay was 7.72 days (SD = 8.5). Regarding education, 42.2% of caregivers had a bachelor’s degree, 26.0% had completed high school, and 15.1% had a middle school education. A small percentage (6.2%) were illiterate, and only 2.3% had higher education beyond a bachelor’s degree. The majority of caregivers were married (89.9%) and Saudi nationals (69.0%). Most children (77.1%) were covered by government health programs, 12.4% by charitable organizations, 6.2% paid in cash, and 4.3% used medical insurance (Table 1).

Table 1.
Caregiver and child characteristics (transition conditions).
3.2.2. Readiness for Hospital Discharge (RHD)
Caregivers reported relatively high levels of readiness for hospital discharge (RHD). Caregivers rated their strength on the day of discharge with a mean score of 8.28 (SD = 2.65), while the strength of their children was rated slightly higher (M = 8.62, SD = 2.26). In terms of knowledge, caregivers reported a moderate understanding of post-discharge issues (M = 7.49, SD = 3.27) and what their child was allowed to do (M = 8.04, SD = 2.98). Confidence in handling the demands of home care was high, particularly for performing medical treatments (M = 9.14, SD = 1.87), while expected support after discharge was rated moderately (M = 7.69, SD = 2.96) (Table 2).

Table 2.
Readiness for Hospital Discharge Scale (response patterns).
3.2.3. Quality of Discharge Teaching (QDT)
The quality of discharge teaching (QDT) provided by nurses was also rated moderately by caregivers. The overall need for information was scored at 5.96 (SD = 2.77), while the information received from nurses was rated slightly lower at 5.62 (SD = 3.18). Caregivers found that nurses were responsive to their concerns (M = 6.86, SD = 3.64) and provided consistent information across healthcare professionals (M = 7.87, SD = 3.19). Confidence in knowing how to handle emergencies was rated relatively high (M = 7.48, SD = 3.24) (Table 3).

Table 3.
Quality of Discharge Teaching Scale (QDTS).
3.2.4. RHD and QTD Comparison
When comparing the two hospital types, there was no significant difference in overall readiness for discharge between the King Abdulaziz University Hospital (KAUH) and the Ministry of Health (MOH) hospital (p = 0.067; see Table 4). However, the quality of discharge teaching was perceived as significantly better at KAUH (M = 6.43, SD = 2.56) compared to the MOH hospital (M = 5.48, SD = 2.89, p = 0.006; see Table 5).

Table 4.
The t-test results for readiness for hospital discharge between two hospitals.

Table 5.
The t-test results for quality of discharge teaching between two hospitals.
3.2.5. RHD Predictors
Regression analysis identified several predictors of discharge readiness. Caregiver age and quality of discharge teaching (QDT) were significant predictors of personal readiness (F(2, 255) = 6.37, p = 0.002). Older caregivers and those who received comprehensive discharge education were more prepared for discharge. In terms of the child’s readiness, child age and diagnosis type significantly influenced perceptions. Caregivers of infants felt their children were less ready for discharge compared to older children (p = 0.013), and children with acute diagnoses were perceived as more ready for discharge than those undergoing planned operations (p = 0.010) (Table 6). Finally, hospital stay length negatively impacted caregivers’ coping and knowledge readiness. Longer hospital stays were associated with lower coping abilities (p = 0.001) and lower knowledge retention (p = 0.019). Caregiver nationality also influenced expectations, with non-Saudi caregivers reporting significantly lower expectations of support post-discharge (p < 0.001) (Table 6).

Table 6.
Multivariate regression model.
4. Discussion
In this study, a critical gap in research on discharge readiness in pediatric care is addressed, focusing on primary caregivers in medical and surgical departments. While discharge preparedness has gained recognition in pediatric critical care, research in non-critical care settings still needs to be expanded. This gap is significant given the growing importance of discharge preparedness in pediatric care, mainly due to children’s fragile health status and increased home care needs [1]. Our findings emphasize that caregivers in medical and surgical units face substantial barriers to feeling prepared for discharge, similar to those in critical care settings. By focusing on this underserved population, our study highlights the urgent need for tailored discharge interventions addressing the unique challenges pediatric primary caregivers face. As the first study of its kind conducted in Saudi Arabia for the pediatric population, our research provides valuable insights into caregivers’ specific needs and concerns in this cultural context, informing the development of culturally sensitive and targeted discharge preparation strategies.
4.1. Readiness for Hospital Discharge
In this study, it was found that discharge readiness among caregivers in pediatric medical and surgical units was moderate, addressing the first research question about the current level of discharge readiness for pediatric primary caregivers. Moderate readiness means that while many caregivers felt reasonably equipped, there were still significant challenges in managing their child’s care after leaving the hospital. These findings are consistent with the prior research indicating that although discharge readiness is generally adequate, many caregivers still require extra support and education to feel completely ready to care for their child at home [9,18,39]. Participants demonstrated moderate to high scores across all aspects of discharge readiness, including personal status, knowledge, coping, and expected support, with knowledge and expected support being the lowest-scoring components. For the low-scored aspects, simple and cost-effective interventions, such as tailored guidance or visual aids, can enhance caregivers’ preparedness by addressing weak areas. Additionally, models such as the IDEAL discharge planning framework can be employed to structure and improve the discharge process [40]. Furthermore, assessing discharge readiness (RHD) is crucial, as it is key in preventing or reducing adverse outcomes associated with discharge [41]. Utilizing an evaluation that determines patients’ readiness for leaving the hospital can help nurses and other medical staff enhance patient preparedness and avoid discharge-related issues [15]. In this study, it was also found that discharge readiness scores were similar in both organizations, indicating no significant difference in discharge readiness levels between the pediatric medical and surgical units.
4.2. Quality of Discharge Teaching
Despite this similarity in readiness, the quality of discharge education was notably higher at the King Abdulaziz University Hospital (KAUH) compared to the Ministry of Health Hospital (MOH). This aligns with the discharge policies of the two institutions, where KAUH emphasizes early discharge planning and comprehensive education for patients and their families, ensuring more thorough preparation. In contrast, the MOH hospital focuses more on the practical aspects of patient preparation and coordination for discharge. The stronger discharge teaching at KAUH reflects its policy focus on education, which may account for the higher quality of instruction provided to caregivers despite the similar overall readiness levels between the two hospitals. This distinction underscores the importance of robust educational support in the discharge process to improve caregiver confidence and preparedness.
In the current study at the aforementioned medical organizations, a moderate quality of discharge teaching (QDT) was reported, addressing the second question regarding the level of discharge teaching provided by nurses. The delivery sub-scale received moderate to high ratings, while the content and received sub-scales were rated at moderate levels, indicating room for improvement in these areas. This finding aligns that inconsistencies in both the content and delivery of discharge information can also negatively affect caregivers’ perceptions of discharge readiness and their overall recovery experience [42], further emphasizing the need for standardized, high-quality education during the discharge process.
4.3. Predictors of Readiness for Hospital Discharge
According to this study, there is a clear link between the quality of discharge teaching and higher levels of readiness for hospital discharge (RHD), specifically the personal status aspect, showing that comprehensive and empathetic education is crucial and can predict caregivers’ readiness for discharge, as they are positively correlated. This finding aligns with previous research on parents of hospitalized children, which demonstrated that nurses’ high-quality discharge teaching, particularly how information was delivered, significantly improved parental readiness for discharge [32,43]. Additionally, greater readiness was associated with fewer coping difficulties and a reduced need for post-hospitalization health services [18,32].
In addition to the quality of discharge teaching, several other predictors were identified in this study, addressing the third research question on factors influencing caregivers’ readiness for discharge. Caregiver age was positively correlated with caregiver readiness, suggesting that as the caregiver’s age increased, the personal status of the caregiver improved. This finding, which contradicts a previous study that found age-related differences causing challenges for discharge readiness, emphasizes the need for further research [44]. The earlier study specifically highlighted areas of concern like information retention and coping. Regardless, a study conducted by Ganefianty et al. [45] demonstrated a finding that aligns with the current research and reported that age was significantly linked to caregivers’ discharge readiness. Such a result indicates that age can pose challenges in some aspects, while older caregivers may express more confidence and ability due to their extended life experience or caregiver familiarity.
The child’s age was an identified predictor variable in estimating the level of readiness for discharge, and pediatric primary caregivers reported lower readiness levels when discharging infants compared with children of older ages, such as childhood or adolescence. This suggests that caregivers may feel increased apprehension or uncertainty in caring for younger children outside of the hospital environment, specifically infants. According to the study conducted by MacKay et al. [46], these parents are continuously in a grieving moment, which is stressful and tends to call for role adjustment, thus increasing their anxiety regarding how to manage care in the home setting. Holditch-Davis et al. [47] reported that caregivers of fragile babies in pediatric medical/surgical general units outside of intensive care often experience significant distress. The study highlighted the pressing need for additional support to help caregivers feel more comfortable in their caregiving role. With maturation, the caregiver is often more confident in managing the child’s needs within the comfort of their home and, thus, preparedness for discharge. Consequently, nurses bear significant importance in supporting the pediatric primary caregivers in general units, particularly those responsible for infants, through education, emotional support, and practical methods that improve caregivers’ confidence and competence to manage their infants’ health needs after discharge.
Hospital admission type strongly influences discharge readiness among pediatric primary caregivers, including acute admission, planned surgical admission, and medical admission. Caregivers of children with acute admissions demonstrated higher discharge readiness levels than children undergoing planned operations. According to Weiss et al. [18], acute cases are often uncomplicated, with fewer complications and care directives that may further emphasize a sense of control and empower caregivers to be confident in managing their child’s transition home. In contrast, caregivers whose children had undergone planned surgical procedures reported higher levels of stress and took longer to adapt and assume coping strategies, as identified by Poh et al. [48]. For these cases, critical predictors of discharge readiness included factors relating to family integration and communication, which would suggest that scheduled surgeries, by their very nature, require more prolonged support and individualized discharge planning to prepare caregivers adequately. Medical admissions did not show significant variations in readiness for discharge, demonstrating that such cases might carry different levels of complexity, neither hindering nor facilitating the transition home as much as acute or surgical cases do. It is thus important to provide personalized discharge education and support the caregivers with approaches to enhance their preparedness, especially for those patients with planned surgeries, since this can reduce readmission rates [49,50].
Interestingly, in this study, it was found that prolonged hospital stays were associated with reduced caregiver knowledge and coping ability. The caregivers of patients with long-term impairments requiring extended hospital stays often experience escalating emotional distress over time, alongside a decline in social support and difficulties in developing effective coping strategies. Research indicates that caregivers managing prolonged hospitalizations require enhanced support systems, such as psychological counseling and customized education, to improve coping skills and retain critical information effectively [51].
Moreover, the results of this study are consistent with the previous ones, pointing out that an extended period of hospitalization decreases caregivers’ knowledge and coping potential. It was documented in particular that long-term impairments of the patients with extended periods of admittance to hospitals are usually followed by a growth in the emotional stress of their caregivers, loss of social support, and an inability to develop coping measures effectively [52]. This stress may also arise due to other duties and changes in caregivers’ lives. To limit these effects, the evidence from previous research argues that increased support networks, including psychological guidance and individualized teaching, are fundamental in empowering caregivers to better cope with challenges and efficiently retain information at the prolonged duration of care [51]. Nurses are vital in guiding patients and their families through the transition process, offering personalized support, building trust, and empowering individuals to navigate their new care environment with confidence and autonomy [53]. In addition to prolonged hospital stays, the current study also determined that caregivers of other nationalities reported lower expectations of post-discharge support compared to Saudi participants. This is partially linked to the challenges faced by non-Saudi caregivers in the Saudi Arabian health system. Being from a different culture than the country of residence, navigating the healthcare system, and managing post-discharge care has become far more complex. Non-Saudi caregivers are specifically in a situation where there is a barrier with the language, unfamiliarity with local healthcare processes, and a general lack of support networks. Thus, their expectations of post-discharge care are lower than those of Saudi caregivers. As expected, the findings reflected this, where non-Saudi caregivers expressed lower confidence in receiving adequate support. It was also similarly concluded by Alotaibi et al. [54], where cultural and language differences hindered effective communication between individuals from different backgrounds, ultimately impacting the quality of care.
4.4. Strengths
This study is among the first on discharge readiness among pediatric caregivers in Saudi Arabia. It offers a good insight into this population, which needs to be well-researched. The use of the Pediatric Readiness for Hospital Discharge Scale and the Quality of Discharge Teaching Scale provides a comprehensive view of caregivers’ preparedness, and the quality of education received post-discharge. Additionally, comparing university and Ministry of Health hospitals adds value to the paper, while using rigorous statistical methods enhances the reliability of the findings. Moreover, the sample size was sufficient, ensuring robust and reliable results.
4.5. Weaknesses
Purposive sampling, upon which this study is based, may be subject to selection bias, limiting generalization to the broader population. The cross-sectional design captures data at one point, preventing analysis of outcomes such as readmissions. Cultural and language barriers might influence responses from non-Saudi caregivers. Lastly, self-reported data could introduce response bias, as caregivers may overestimate their preparedness or satisfaction with discharge teaching.
4.6. Future Recommendations
In light of these limitations, and as a way forward for future studies, we propose the following: Future studies should make use of random sampling methods so that generalization can be enhanced by diversifying samples. Longitudinal follow-up would allow more valuable insights; it would quantify long-term outcomes and the impact of discharge readiness on readmissions and complications. Individualized discharge plans should be developed for infant caregivers and those undergoing elective surgeries to enhance discharge education that meets specific needs. Training health professionals through appropriate training programs will also help provide respectful and professional services to overcome other cultural and language barriers of non-Saudi caregivers. And finally, support networks, including psychological counseling, need to be established to extend support to the caregivers during hospitalization.
Author Contributions
Conceptualization, M.A.A. and M.F.A.; methodology, M.A.A. and M.F.A.; software, M.A.A. and M.F.A.; validation, M.A.A. and M.F.A.; formal analysis, M.A.A.; investigation, M.A.A.; resources, M.A.A.; data curation, M.A.A.; writing—original draft preparation, M.A.A.; writing—review and editing, M.F.A.; visualization, M.F.A.; supervision, M.F.A.; project administration, M.A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Institutional Review Board of King Abdulaziz University Hospital (KAUH) (protocol code 624-23, approved on 6 December 2023) and by the Institutional Review Board for MOH hospitals at East Jeddah Hospital and King Abdulaziz Hospital (IRB Log No. A01714, approved on 4 September 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author. The data are not publicly available due to information that could compromise the privacy of the research participants.
Acknowledgments
The project administrator, Maha Alzahrani, would like to acknowledge the valuable contributions of the nursing interns, Fai Aljohani, Manal Alsulami, Tethkar Bakor, and Roaa Basas, for their assistance and support throughout the data collection process.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of this study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
References
- Kim, M.E.; Kasparian, N.A.; Zang, H.; Pater, C.; Chlebowski, M.M.; Marcuccio, E.; Florez, A.; Morales, D.L.; Madsen, N.; Moore, R.A. Are Parent Discharge Readiness Scores Effective for Patients With Congenital Heart Disease After Cardiac Surgery? J. Pediatr. 2023, 257, 113361. [Google Scholar] [CrossRef] [PubMed]
- Auger, K.A.; Kenyon, C.C.; Feudtner, C.; Davis, M.M. Pediatric hospital discharge interventions to reduce subsequent utilization: A systematic review. J. Hosp. Med. 2014, 9, 251–260. [Google Scholar] [CrossRef]
- McBride, M.; Andrews, G.J. The transition from acute care to home: A review of issues in discharge teaching and a framework for better practice. Can. J. Cardiovasc. Nurs. 2013, 23, 18–24. [Google Scholar] [CrossRef]
- Weiss, M.E.; Lerret, S.M.; Sawin, K.J.; Schiffman, R.F. Parent Readiness for Hospital Discharge Scale: Psychometrics and Association With Postdischarge Outcomes. J. Pediatr. Health Care 2020, 34, 30–37. [Google Scholar] [CrossRef]
- Al-Dhawyani, A.; Al-Hinai, K.; Chan, M.F.; Al-Azri, M. Factors Contributing to the Unmet Needs of Primary Caregivers of Omani Children Diagnosed with Leukemia. Oman Med. J. 2022, 37, e358. [Google Scholar] [CrossRef]
- Fenwick, A.M. An interdisciplinary tool for assessing patients’ readiness for discharge in the rehabilitation setting. J. Adv. Nurs. 1979, 4, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.-Y.; Lee, T.-T.; Lin, Y.-H.; Liu, C.-Y.; Wu, H.-C.; Huang, S.-H. Factors Related to Family Caregivers’ Readiness for the Hospital Discharge of Advanced Cancer Patients. Int. J. Environ. Res. Public Health 2022, 19, 8097. [Google Scholar] [CrossRef]
- Berry, J.G.; Ziniel, S.I.; Freeman, L.; Kaplan, W.; Antonelli, R.; Gay, J.; Coleman, E.A.; Porter, S.; Goldmann, D. Hospital readmission and parent perceptions of their child’s hospital discharge. Int. J. Qual. Health Care 2013, 25, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Lerret, S.M. Discharge readiness: An integrative review focusing on discharge following pediatric hospitalization. J. Spec. Pediatr. Nurs. 2009, 14, 245–255. [Google Scholar] [CrossRef]
- Weiss, M.E.; Lokken, L. Predictors and outcomes of postpartum mothers’ perceptions of readiness for discharge after birth. JOGNN—J. Obstet. Gynecol. Neonatal Nurs. 2009, 38, 406–417. [Google Scholar] [CrossRef]
- Galvin, E.C.; Wills, T.; Coffey, A. Readiness for hospital discharge: A concept analysis. J. Adv. Nurs. 2017, 73, 2547–2557. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.; Li, C.; Chen, P.; Guo, J.; Zhao, S. The Impact of Empowerment Education on Discharge Readiness and Care Burden of Caregivers of Children with Congenital Heart Disease. Altern. Ther. Health Med. 2024, v2n1, AT8532. [Google Scholar]
- Judha, M. Family Awareness and Willingness to Accept Discharge Planning According to Nursing Advocacy Program. Malays. J. Nurs. 2020, 11, 92–98. [Google Scholar] [CrossRef]
- Steele, N.F.; Sterling, Y.M. Application of the case study design: nursing interventions for discharge readiness. Clin. Nurse Spec. 1992, 6, 79–84. [Google Scholar] [CrossRef]
- Weiss, M.E.; Costa, L.L.; Yakusheva, O.; Bobay, K.L. Validation of Patient and Nurse Short Forms of the Readiness for Hospital Discharge Scale and Their Relationship to Return to the Hospital. Health Serv. Res. 2014, 49, 304. [Google Scholar] [CrossRef] [PubMed]
- Titler, M.G.; Pettit, D.M. Discharge Readiness Assessment. J. Cardiovasc. Nurs. 1995, 9, 64. [Google Scholar] [CrossRef]
- Marino, B.; Marino, E. Parents’ report of children’s hospital care: What it means for your practice. Pediatr. Nurs. 2000, 26, 195. Available online: https://pubmed.ncbi.nlm.nih.gov/12026276/ (accessed on 13 November 2022).
- Weiss, M.E.; Sawin, K.J.; Gralton, K.; Johnson, N.; Klingbeil, C.; Lerret, S.; Malin, S.; Yakusheva, O.; Schiffman, R. Discharge Teaching, Readiness for Discharge, and Post-discharge Outcomes in Parents of Hospitalized Children. J. Pediatr. Nurs. 2017, 34, 58–64. [Google Scholar] [CrossRef]
- Weiss, M.; Johnson, N.L.; Malin, S.; Jerofke, T.; Lang, C.; Sherburne, E. Readiness for Discharge in Parents of Hospitalized Children. J. Pediatr. Nurs. 2008, 23, 282–295. [Google Scholar] [CrossRef]
- Weiss, M.E.; Piacentine, L.B.; Lokken, L.; Ancona, J.; Archer, J.; Gresser, S.; Holmes, S.B.; Toman, S.; Toy, A.; Vega-Stromberg, T. Perceived readiness for hospital discharge in adult medical-surgical patients. Clin. Nurse Spec. 2007, 21, 31–42. [Google Scholar] [CrossRef]
- Levick, J.; Quinn, M.; Vennema, C. NICU parent-to-parent partnerships: A comprehensive approach. Neonatal Netw. 2014, 33, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Vaz, L.E.; Jungbauer, R.M.; Jenisch, C.; Austin, J.P.; Wagner, D.V.; Everist, S.J.; Libak, A.J.; Harris, M.A.; Zuckerman, K.E. Caregiver Experiences in Pediatric Hospitalizations: Challenges and Opportunities for Improvement. Hosp. Pediatr. 2022, 12, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Meleis, A.; Sawyer, L.; Eun-Ok, I.; Messias, H.; DeAnne, K.; Schumacher, K. Experiencing Transitions: An Emerging Middle-Range Theory. Adv. Nurs. Sci. 2000, 23, 12. Available online: https://oce.ovid.com/article/00012272-200009000-00006/HTML (accessed on 19 November 2022). [CrossRef] [PubMed]
- Polit, D.F.; Beck, C.T. Essentials of Nursing Research: Appraising Evidence for Nursing Practice; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2009. [Google Scholar]
- Bonett, D.G.; Wright, T.A. Sample size requirements for multiple regression interval estimation. J. Organ. Behav. 2011, 32, 822–830. [Google Scholar] [CrossRef]
- Kang, H. Sample size determination and power analysis using the G*Power software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef]
- McCrum-Gardner, E. Sample size and power calculations made simple. Int. J. Ther. Rehabil. 2010, 17, 10–14. [Google Scholar] [CrossRef]
- Polit, D.; Beck, C. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 10th ed.; Wolters Kluwer Health: Philadelphia, PA, USA, 2017. [Google Scholar]
- Acharya, A.S.; Prakash, A.; Saxena, P.; Nigam, A. Sampling: Why and How of it? Indian J. Med. Spéc. 2013, 4, 330–333. [Google Scholar] [CrossRef]
- Sharma, G. Pros and cons of different sampling techniques. Int. J. Appl. Res. 2017, 3, 749–752. Available online: www.allresearchjournal.com (accessed on 11 April 2023).
- O’Reilly-Shah, V.N. Factors influencing healthcare provider respondent fatigue answering a globally administered in-app survey. PeerJ 2017, 5, e3785. [Google Scholar] [CrossRef]
- Maloney, L.R.; Weiss, M.E. Patients’ perceptions of hospital discharge informational content. Clin. Nurs. Res. 2008, 17, 200–219. [Google Scholar] [CrossRef]
- Lerret, S.M.; Weiss, M.E. How ready are they? Parents of pediatric solid organ transplant recipients and the transition from hospital to home following transplant. Pediatr. Transpl. 2011, 15, 606–616. [Google Scholar] [CrossRef] [PubMed]
- Waltz, C.F.; Strickland, O.L.; Lenz, E.R. Measurement in Nursing and Health Research; Springer Publishing Company: New York, NY, USA, 2016. [Google Scholar] [CrossRef]
- Awang, Z.; Afthanorhan, A.; Mamat, M. The Likert scale analysis using parametric based Structural Equation Modeling (SEM). Comput. Methods Soc. Sci. 2016, 4, 13. [Google Scholar]
- Harpe, S.E. How to analyze Likert and other rating scale data. Curr. Pharm. Teach. Learn. 2015, 7, 836–850. [Google Scholar] [CrossRef]
- Hwang, J.S.; Hu, T.H. A stepwise regression algorithm for high-dimensional variable selection. J. Stat. Comput. Simul. 2015, 85, 1793–1806. [Google Scholar] [CrossRef]
- McDonald, J.H. Handbook of Biological Statistics—Paired T–Test; Sparky House Publishing: Baltimore, MD, USA, 2014. [Google Scholar]
- Malhotra, A.; Brady, D.; Kreys, E.; Silva, J.; Feng, X.; Yang, C. Development, implementation, and assessment of a comprehensive, integrated, and multimodal interprofessional education (CIM-IPE) program. J. Interprof. Educ. Pract. 2020, 21, 100356. [Google Scholar] [CrossRef]
- Luther, B.; Wilson, R.D.; Kranz, C.; Krahulec, M. Discharge Processes: What Evidence Tells Us Is Most Effective. Orthop. Nurs. 2019, 38, 328–333. [Google Scholar] [CrossRef]
- Xiong, L.; Liu, Y.; Chen, Q.; Tian, Y.; Yang, M. Readiness for hospital discharge of adult patients with major depressive disorder in China: A cross-sectional study. Patient Prefer. Adherence 2021, 15, 1681–1692. [Google Scholar] [CrossRef]
- Zhou, H.; Roberts, P.A.; Della, P.R. Nurse-Caregiver Communication of Hospital-To-Home Transition Information at a Tertiary Pediatric Hospital in Western Australia: A Multi-Stage Qualitative Descriptive Study. J. Pediatr. Nurs. 2021, 60, 83–91. [Google Scholar] [CrossRef]
- Hua, W.; Yuwen, W.; Simoni, J.M.; Yan, J.; Jiang, L. Parental readiness for hospital discharge as a mediator between quality of discharge teaching and parental self-efficacy in parents of preterm infants. J. Clin. Nurs. 2020, 29, 3754–3763. [Google Scholar] [CrossRef]
- Bobay, K.L.; Jerofke, T.A.; Weiss, M.E.; Yakusheva, O. Age-related differences in perception of quality of discharge teaching and readiness for hospital discharge. Geriatr. Nurs. 2010, 31, 178–187. [Google Scholar] [CrossRef]
- Ganefianty, A.; Songwathana, P.; Damkliang, J. Readiness for hospital discharge perceived by caregivers of patients with traumatic brain injury: A cross-sectional study. Belitung. Nurs. J. 2024, 10, 209–214. [Google Scholar] [CrossRef] [PubMed]
- MacKay, L.; Benzies, K.; Barnard, C.; Bouchal, S.R. Parental Experiences Caring for Their Hospitalized Medically Fragile Infants: A Description of Grief, Stress, and Coping. Can. J. Nurs. Res. 2021, 53, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Holditch-Davis, D.; Tesh, E.M.; Miles, M.S.; Burchinal, M. Early interactions between mothers and their medically fragile infants. Appl. Dev. Sci. 1999, 3, 155–167. [Google Scholar] [CrossRef]
- Poh, P.F.; Lee, J.H.; Loh, Y.J.; Tan, T.H.; Cheng, K.K.F. Readiness for Hospital Discharge, Stress, and Coping in Mothers of Children Undergoing Cardiac Surgeries: A Single-Center Prospective Study. Pediatr. Crit. Care Med. 2020, 21, e301–e310. [Google Scholar] [CrossRef] [PubMed]
- Patra, K.P.; Mains, N.; Dalton, C.; Welsh, J.; Iheonunekwu, C.; Dai, Z.; Murray, P.J.; Fisher, E.S. Improving discharge outcomes by using a standardized risk assessment and intervention tool facilitated by advanced pediatric providers. Hosp. Pediatr. 2020, 10, 173–180. [Google Scholar] [CrossRef]
- Uong, A.; Philips, K.; Hametz, P.; Dunbar, J.; Jain, P.; O’connor, K.; Offenbacher, R.; Eliezer, K.; Pilnick, C.; Kiely, V.; et al. SAFER care: Improving caregiver comprehension of discharge instructions. Pediatrics 2021, 147, e20200031. [Google Scholar] [CrossRef]
- Rennick, J.E.; St-Sauveur, I.; Knox, A.M.; Ruddy, M. Exploring the experiences of parent caregivers of children with chronic medical complexity during pediatric intensive care unit hospitalization: An interpretive descriptive study. BMC Pediatr. 2019, 19, 272. [Google Scholar] [CrossRef]
- Chiambretto, P.; Ferrario, S.R.; Zotti, A.M. Patients in a persistent vegetative state: Caregiver attitudes and reactions. Acta Neurol. Scand. 2001, 104, 364–368. [Google Scholar] [CrossRef]
- Gabay, G.; Tarabeih, M. “A Bridge Over Troubled Water”: Nurses’ Leadership in Establishing Young Adults’ Trust Upon the Transition to Adult Renal-Care—A Dual-Perspective Qualitative Study. J. Pediatr. Nurs. 2020, 53, e41–e48. [Google Scholar] [CrossRef]
- Alotaibi, K.; Higgins, I.; Chan, S. Culture, religion, language and the assessment and management of children’s pain by expatriate nurses in Saudi Arabia: A qualitative study. J. Spec. Pediatr. Nurs. 2023, 28, e12399. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).