Enhancing Effective Scanning Techniques for Digital Impression in Neonates with Cleft Lip and/or Palate: A Laboratory Study Investigating the Impact of Different Scanners, Scanning Tip Sizes, and Strategies
Abstract
1. Introduction
2. Materials and Methods
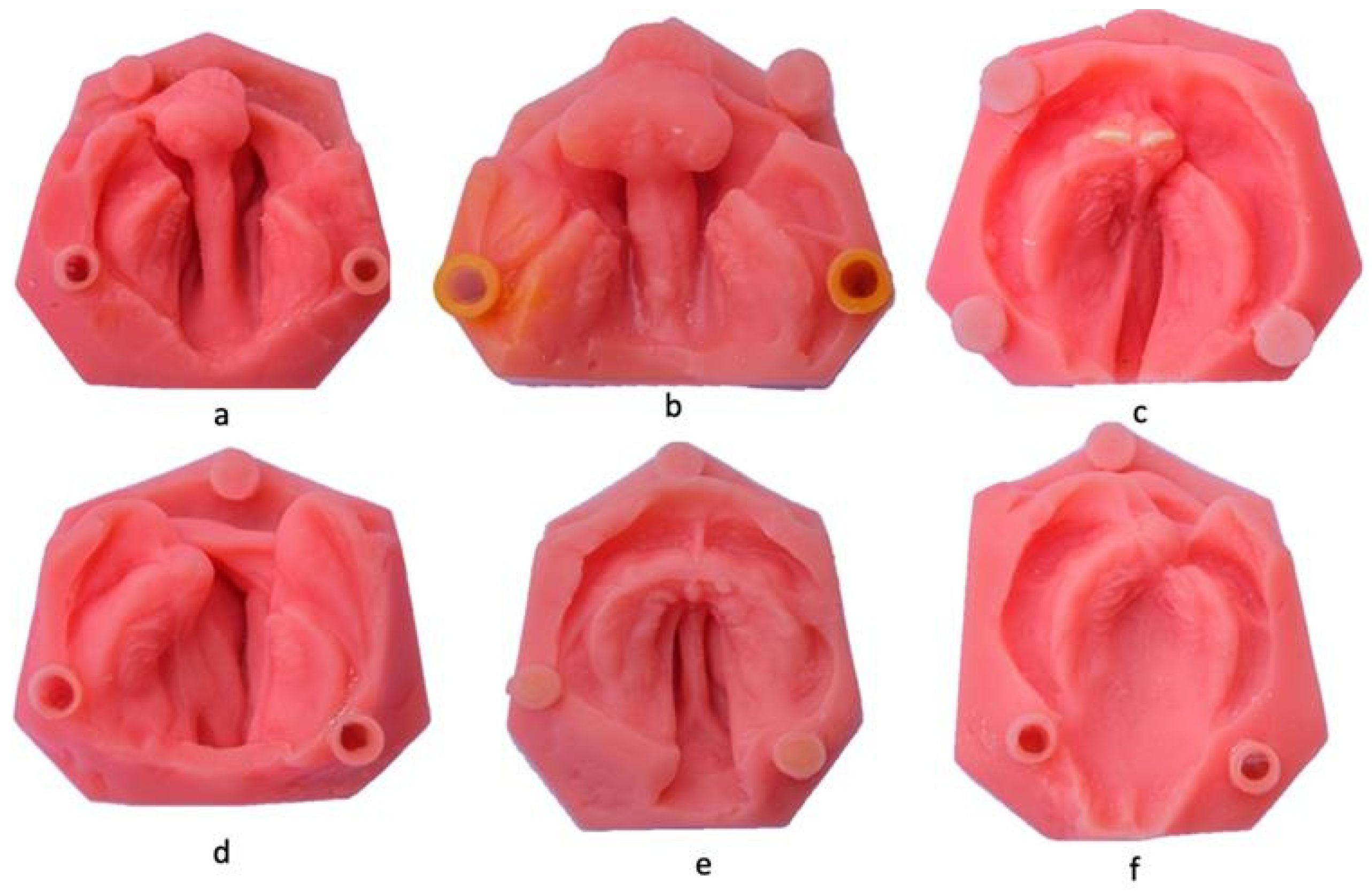
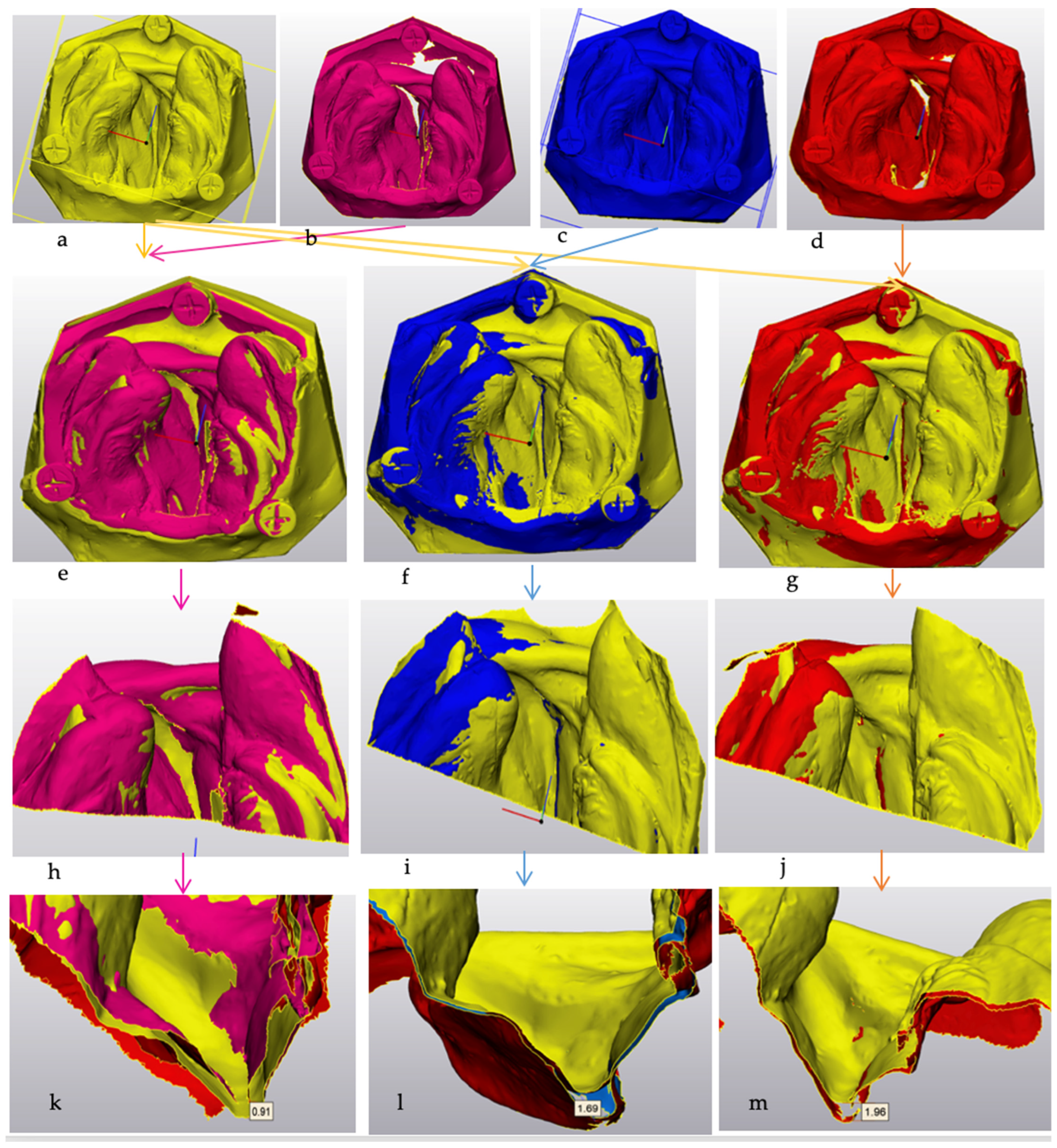
Cleft Lip and Palate Models
3. Results
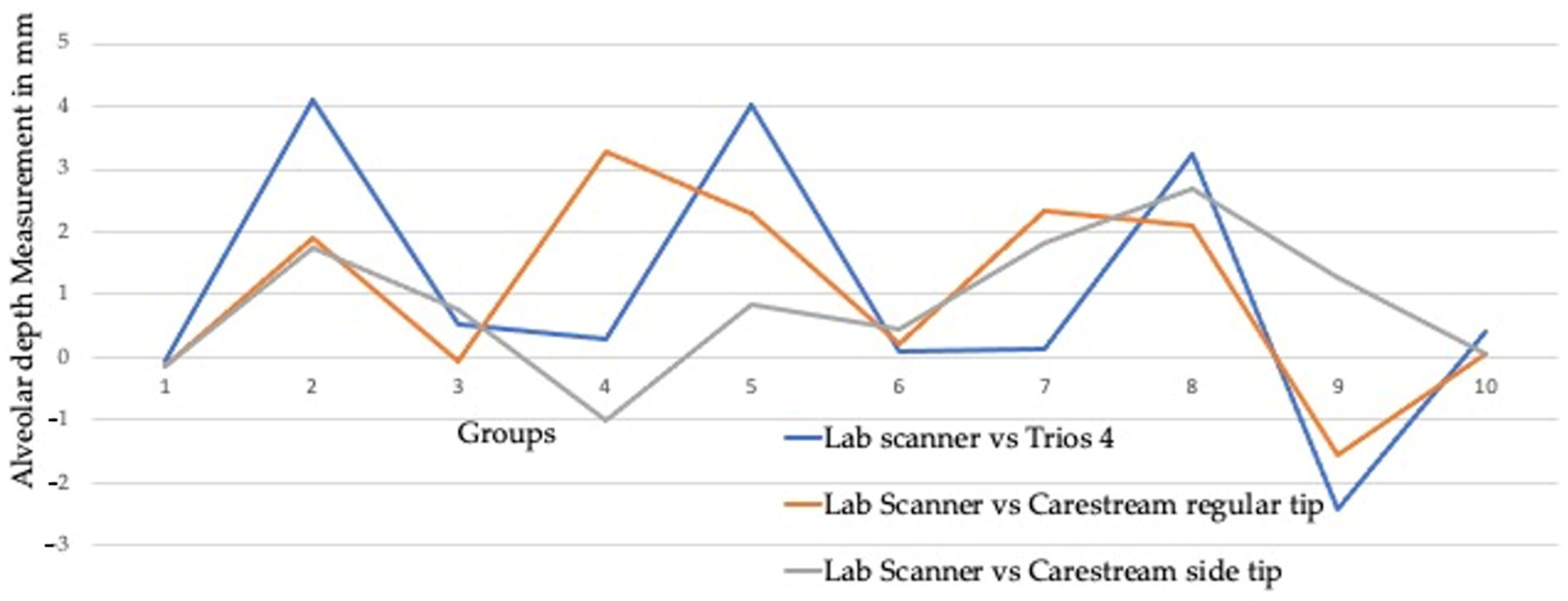
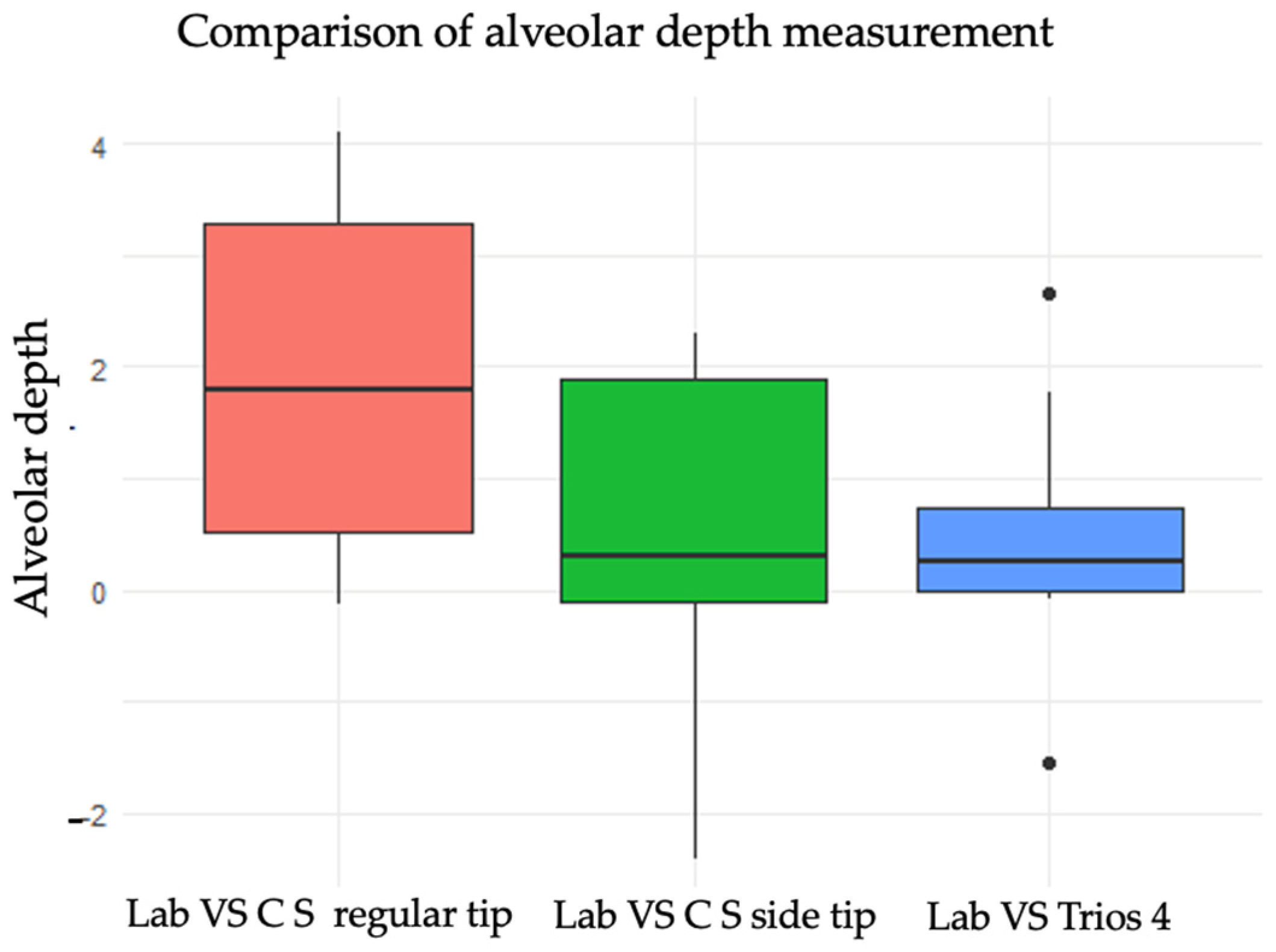
3.1. Effect of Scanning Tip Variation on Alveolar Cleft Depth Measurement
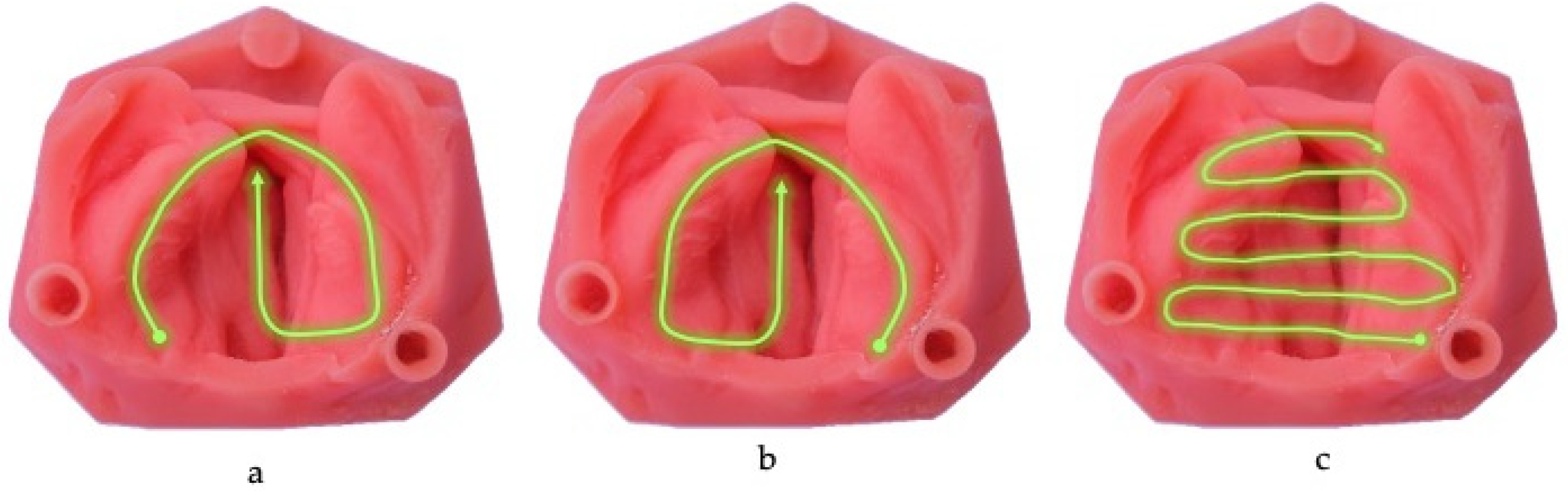
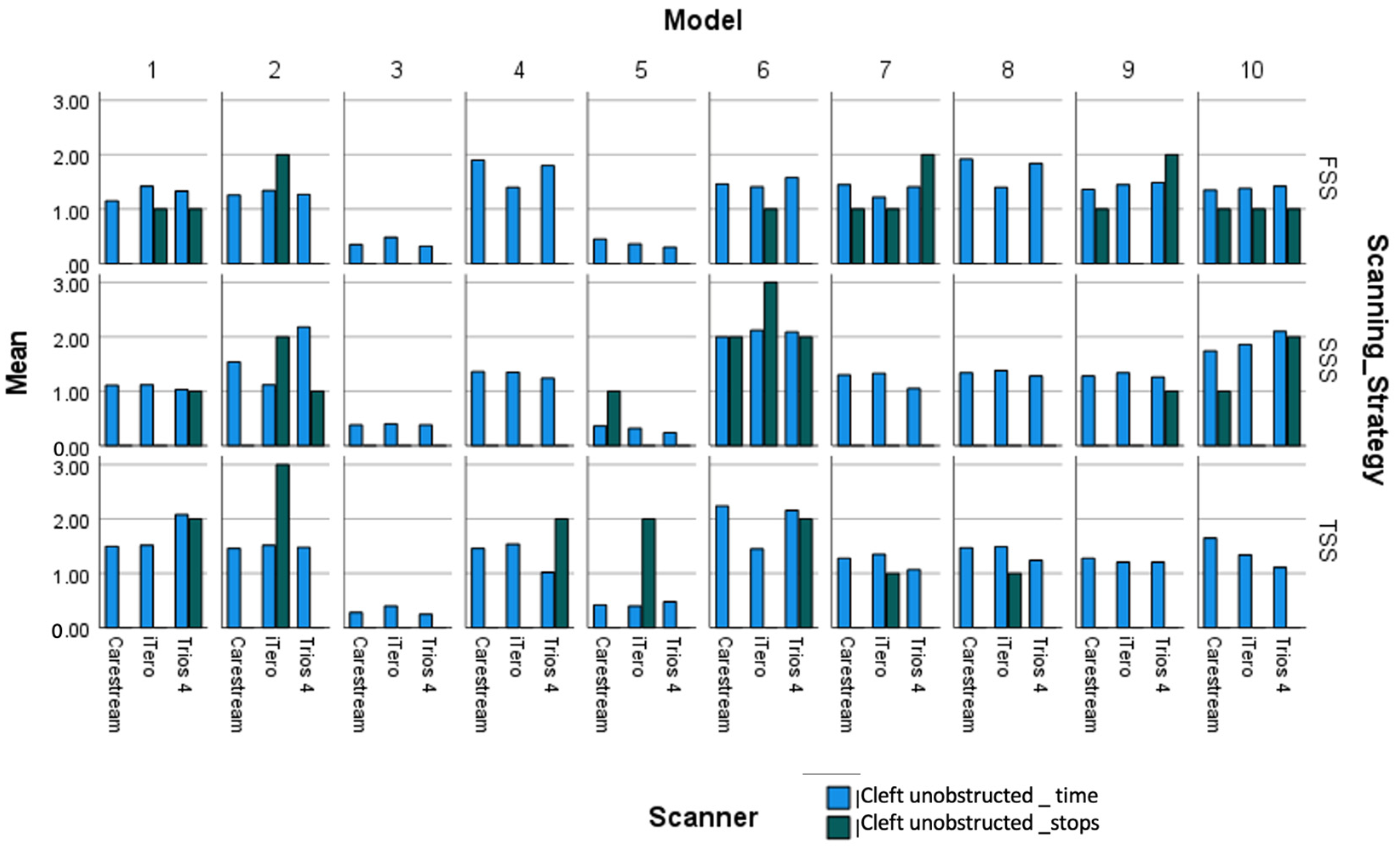
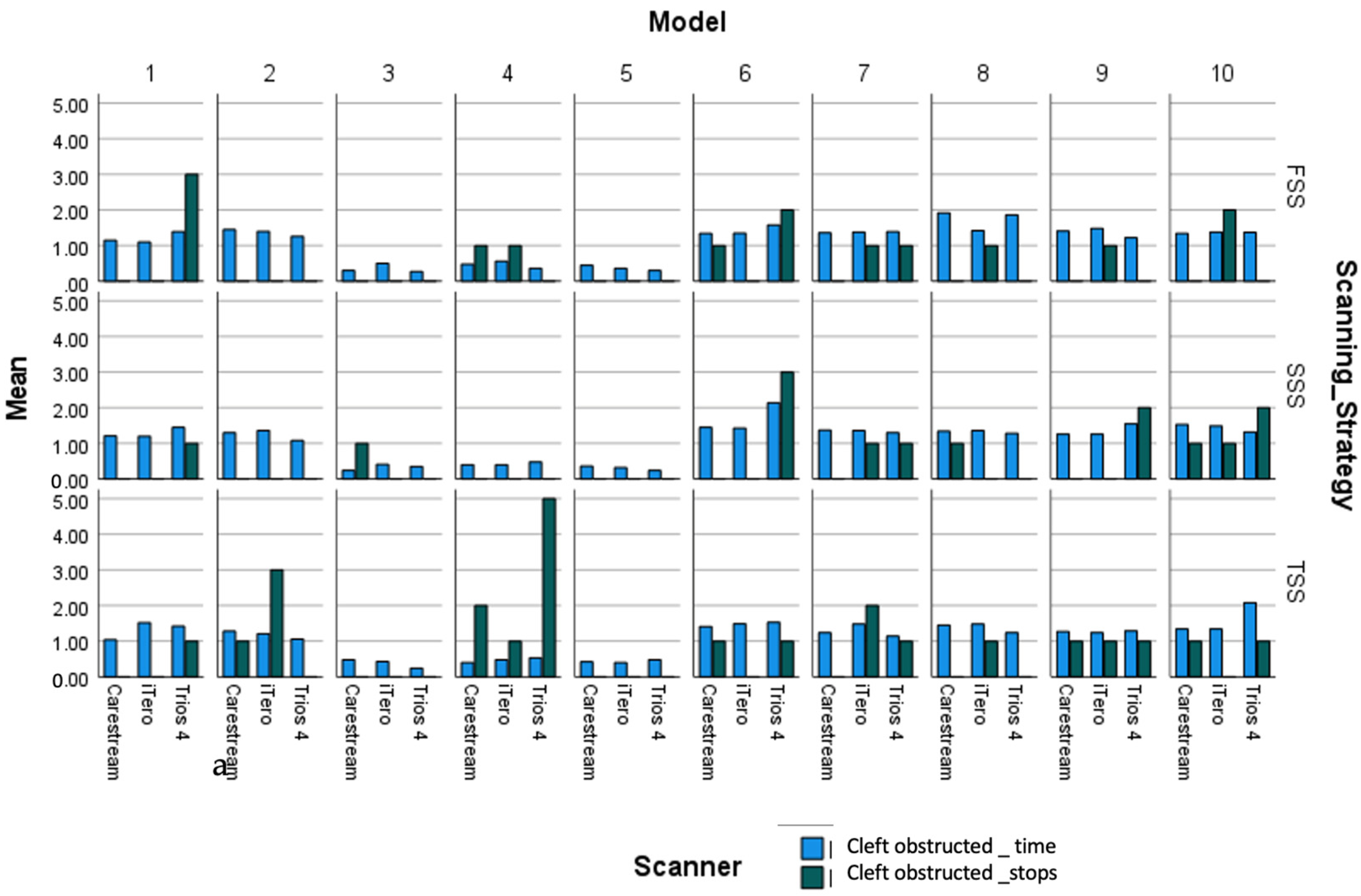
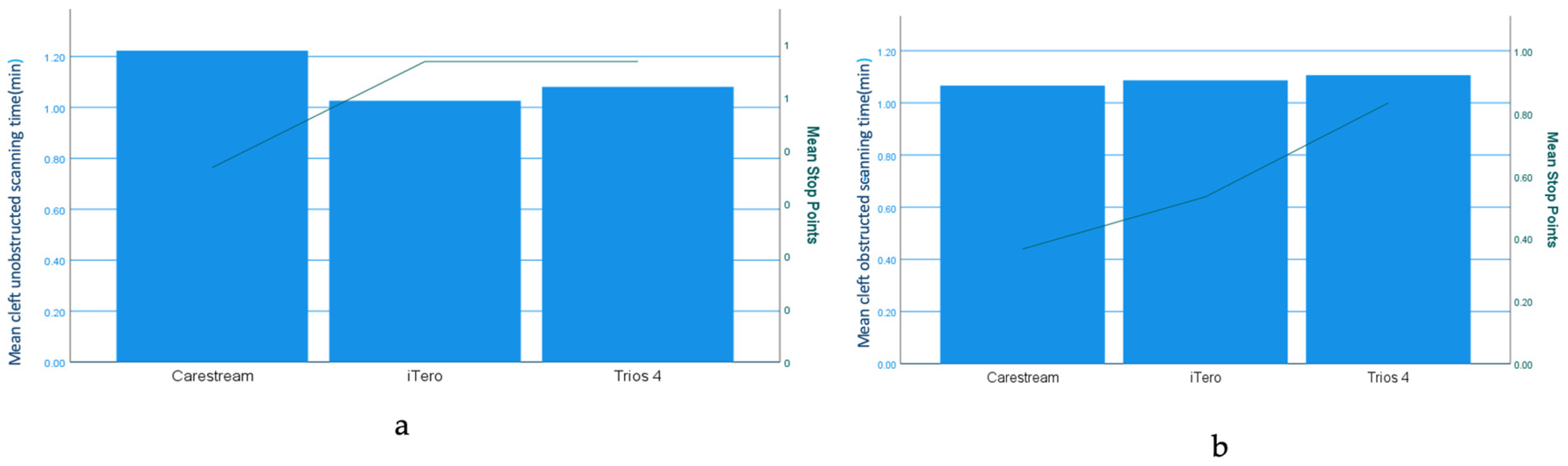
3.2. Different Scanners and Scanning Strategy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tanaka, S.A.; Mahabir, R.C.; Jupiter, D.C.; Menezes, J.M. Updating the epidemiology of cleft lip with or without cleft palate. Plast. Reconstr. Surg. 2012, 129, 511e–518e. [Google Scholar] [CrossRef] [PubMed]
- Shetye, P.R.; Gibson, T.L. Introduction to clinical provision of nasoalveolar molding. In Cleft Craniofacial Orthodontics; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2023; pp. 101–118. [Google Scholar] [CrossRef]
- Jacobson, B.N.; Rosenstein, S.W. Early maxillary orthopedics for the newborn cleft lip and palate patient. An impression and an appliance. Angle Orthod. 1984, 54, 247–263. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.S.; Shin, H.S. Preoperative Planning and Simulation in Patients with Cleft Palate Using Intraoral Three-Dimensional Scanning and Printing. J. Craniofacial Surg. 2019, 30, 2245–2248. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Hattori, M.; Akiyama, M.; Elbashti, M.E.; Liu, R.; Sumita, Y.I. Three-dimensional evaluation of the dental arch in cleft lip and palate after prosthetic treatment. J. Prosthodont. Res. 2023, 67, 87–92. [Google Scholar] [CrossRef]
- Ahmed, M.K.; Ahsanuddin, S.; Retrouvey, J.-M.; Koka, K.S.; Qureshi, H.; Bui, A.H.; Taub, P.J. Fabrication of Nasoalveolar Molding Devices for the Treatment of Cleft Lip and Palate, Using Stereolithography Additive Manufacturing Processes and Computer-Aided Design Manipulation Software. J. Craniofacial Surg. 2019, 30, 2604–2608. [Google Scholar] [CrossRef]
- Naveau, A.; Grémare, A.; Plaire, V.; Ducret, M.; Loot, M.; Noirrit-Esclassan, E. Digital management of low cost presurgical plates for young patients with palatal cleft. Fr. J. Dent. Med. 2021, 1–6. [Google Scholar] [CrossRef]
- Bous, R.M.; Kochenour, N.; Valiathan, M. A novel method for fabricating nasoalveolar molding appliances for infants with cleft lip and palate using 3-dimensional workflow and clear aligners. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 452–458. [Google Scholar] [CrossRef]
- Batra, P.; Raghavan, S. Technological advancements in presurgical infant orthopedics. In Cleft Craniofacial Orthodontics; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2023; pp. 149–157. [Google Scholar] [CrossRef]
- Dalessandri, D.; Tonni, I.; Laffranchi, L.; Migliorati, M.; Isola, G.; Bonetti, S.; Visconti, L.; Paganelli, C. Evaluation of a Digital Protocol for Pre-Surgical Orthopedic Treatment of Cleft Lip and Palate in Newborn Patients: A Pilot Study. Dent. J. 2019, 7, 111. [Google Scholar] [CrossRef]
- Chalmers, E.V.; Mcintyre, G.T.; Wang, W.; Gillgrass, T.; Martin, C.B.; Mossey, P.A. Intraoral 3D Scanning or Dental Impressions for the Assessment of Dental Arch Relationships in Cleft Care: Which is Superior? Cleft Palate Craniofacial J. 2016, 53, 568–577. [Google Scholar] [CrossRef]
- Carter, C.B.; Gallardo, F.F.; Colburn, H.E.; Schlieder, D.W. Novel Digital Workflow for Nasoalveolar Molding and Postoperative Nasal Stent for Infants with Cleft Lip and Palate. Cleft Palate Craniofacial J. 2022, 60, 1176–1181. [Google Scholar] [CrossRef]
- Fomenko, I.; Maslak, E.; Timakov, I.; Tsoy, T. Use of Virtual 3D-Model for the Assessment of Premaxilla Position in 3–4-Year-Olds with Complete Bilateral Cleft Lip and Palate—A Pilot Study. In Proceedings of the 2019 12th International Conference on Developments in eSystems Engineering (DeSE), Kazan, Russia, 7–10 October 2019; pp. 933–938. [Google Scholar] [CrossRef]
- Unnikrishnan, J.; Etemad Shahidi, Y.; Bakr, M.; Love, R.; Idris, G. Clinician- and Patient-Centred Outcomes of Digital Impressions in Infants with Cleft Lip and Palate: A Systematic Review. Children 2024, 11, 343. [Google Scholar] [CrossRef] [PubMed]
- Krey, K.-F.; Ratzmann, A.; Metelmann, P.H.; Hartmann, M.; Ruge, S.; Kordaß, B. Fully digital workflow for presurgical orthodontic plate in cleft lip and palate patients Vollständiger digitaler Workflow für die Herstellung von prächirurgischen kieferorthopädischen Platten bei Patienten mit Lippen-Kiefer-Gaumenspalten. Int. J. Comput. Dent. 2018, 21, 251–259. [Google Scholar] [PubMed]
- Weise, C.; Frank, K.; Wiechers, C.; Weise, H.; Reinert, S.; Koos, B.; Xepapadeas, A.B. Intraoral scanning of neonates and infants with craniofacial disorders: Feasibility, scanning duration, and clinical experience. Eur. J. Orthod. 2022, 44, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, T.; Kawanabe, H.; Fukui, K. Comparison of conventional impression making and intraoral scanning for the study of unilateral cleft lip and palate. Congenit. Anom. 2023, 63, 16–22. [Google Scholar] [CrossRef]
- Shanbhag, G.; Pandey, S.; Mehta, N.; Kini, Y.; Kini, A. A Virtual Noninvasive Way of Constructing a Nasoalveolar Molding Plate for Cleft Babies, Using Intraoral Scanners, CAD, and Prosthetic Milling. Cleft Palate Craniofacial J. 2020, 57, 263–266. [Google Scholar] [CrossRef]
- Batra, P.; Gribel, B.F.; Abhinav, B.A.; Arora, A.; Raghavan, S. OrthoAligner “NAM”: A Case Series of Presurgical Infant Orthopedics (PSIO) Using Clear Aligners. Cleft Palate Craniofacial J. 2020, 57, 646–655. [Google Scholar] [CrossRef]
- ElNaghy, R.; Amin, S.A.; Hasanin, M. Evaluating the accuracy of intraoral direct digital impressions in 2 infants with unilateral cleft lip and palate compared with digitized conventional impression. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 403–409. [Google Scholar] [CrossRef]
- Gong, X.; Dang, R.; Xu, T.; Yu, Q.; Zheng, J. Full Digital Workflow of Nasoalveolar Molding Treatment in Infants with Cleft Lip and Palate. J. Craniofacial Surg. 2020, 31, 367–371. [Google Scholar] [CrossRef]
- Patel, J.; Winters, J.; Walters, M. Intraoral Digital Impression Technique for a Neonate with Bilateral Cleft Lip and Palate. Cleft Palate Craniofacial J. 2019, 56, 1120–1123. [Google Scholar] [CrossRef]
- Soliman, I.; Sharaf, D.; Shawky, A.; Atteya, A. Diagnostic evaluation and guardian assessment of using digital impression in neonates versus the conventional techniques. Alex. Dent. J. 2023, 49, 129–133. [Google Scholar] [CrossRef]
- Unnikrishnan, J.; Bakr, M.; Love, R.; Idris, G. The Accuracy of Digital Impressions versus Conventional Impressions in Neonates with Cleft Lip and/or Palate: A Laboratory-Based Study. Children 2024, 11, 827. [Google Scholar] [CrossRef] [PubMed]
- Benitez, B.K.; Brudnicki, A.; Surowiec, Z.; Wieprzowski, Ł.; Rasadurai, A.; Nalabothu, P.; Lill, Y.; Mueller, A.A. Digital impressions from newborns to preschoolers with cleft lip and palate: A two-centers experience. J. Plast. Reconstr. Aesthetic Surg. 2022, 75, 4233–4242. [Google Scholar] [CrossRef] [PubMed]
- Zarean, P.; Zarean, P.; Thieringer, F.M.; Mueller, A.A.; Kressmann, S.; Erismann, M.; Sharma, N.; Benitez, B.K. A Point-of-Care Digital Workflow for 3D Printed Passive Presurgical Orthopedic Plates in Cleft Care. Children 2022, 9, 1261. [Google Scholar] [CrossRef]
- Vafaee, F.; Firouz, F.; Mohajeri, M.; Hashemi, R.; Ghorbani Gholiabad, S. In Vitro Comparison of the Accuracy (Precision and Trueness) of Seven Dental Scanners. J. Dent. 2021, 22, 8–13. [Google Scholar] [CrossRef]
- Kang, B.; Son, K.; Lee, K. Accuracy of Five Intraoral Scanners and Two Laboratory Scanners for a Complete Arch: A Comparative In Vitro Study. Appl. Sci. 2020, 10, 74. [Google Scholar] [CrossRef]
- Ender, A.; Attin, T.; Mehl, A. In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J. Prosthet. Dent. 2016, 115, 313–320. [Google Scholar] [CrossRef]
- Amornvit, P.; Rokaya, D.; Sanohkan, S. Comparison of Accuracy of Current Ten Intraoral Scanners. BioMed Res. Int. 2021, 2021, 2673040. [Google Scholar] [CrossRef]
- Uhm, S.-H.; Kim, J.-H.; Jiang, H.B.; Woo, C.-W.; Chang, M.; Kim, K.-N.; Bae, J.M.; Oh, S. Evaluation of the accuracy and precision of four intraoral scanners with 70% reduced inlay and four-unit bridge models of international standard. Dent. Mater. J. 2017, 36, 27–34. [Google Scholar] [CrossRef]
- An, H.; Langas, E.E.; Gill, A.S. Effect of scanning speed, scanning pattern, and tip size on the accuracy of intraoral digital scans. J. Prosthet. Dent. 2024, 131, 1160–1167. [Google Scholar] [CrossRef]
- Ender, A.; Mehl, A. Influence of scanning strategies on the accuracy of digital intraoral scanning systems. Int. J. Comput. Dent. 2013, 16, 11–21. [Google Scholar]
- Gavounelis, N.A.; Gogola, C.-M.C.; Halazonetis, D.J. The Effect of Scanning Strategy on Intraoral Scanner’s Accuracy. Dent. J. 2022, 10, 123. [Google Scholar] [CrossRef] [PubMed]
- Rapone, B.; Palmisano, C.; Ferrara, E.; Di Venere, D.; Albanese, G.; Corsalini, M. The Accuracy of Three Intraoral Scanners in the Oral Environment with and without Saliva: A Comparative Study. Appl. Sci. 2020, 10, 7762. [Google Scholar] [CrossRef]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral scanners in dentistry: A review of the current literature. BMC Oral. Health 2017, 17, 149. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.G.; Veronesi, G.; Hauschild, U.; Mijiritsky, E.; Mangano, C. Trueness and Precision of Four Intraoral Scanners in Oral Implantology: A Comparative in Vitro Study. PLoS ONE 2016, 11, e0163107. [Google Scholar] [CrossRef]
- Anh, J.; Park, J.-M.; Chun, Y.-S.; Kim, M.; Kim, M. A comparison of the precision of three-dimensional images acquired by 2 digital intraoral scanners: Effects of tooth irregularity and scanning direction. Korean J. Orthod. 2016, 46, 3–12. [Google Scholar] [CrossRef]
- Zhang, Y.-J.; Shi, J.; Qian, S.; Qiao, S.-C.; Lai, H.-C. Accuracy of full-arch digital implant impressions taken using intraoral scanners and related variables: A systematic review. Int. J. Oral. Implantol. 2021, 14, 157–179. [Google Scholar]
- Renne, W.; Ludlow, M.; Fryml, J.; Schurch, Z.; Mennito, A.; Kessler, R.; Lauer, A. Evaluation of the accuracy of 7 digital scanners: An in vitro analysis based on 3-dimensional comparisons. J. Prosthet. Dent. 2017, 118, 36–42. [Google Scholar] [CrossRef]
- Iturrate, M.; Eguiraun, H.; Etxaniz, O.; Solaberrieta, E. Accuracy analysis of complete-arch digital scans in edentulous arches when using an auxiliary geometric device. J. Prosthet. Dent. 2019, 121, 447–454. [Google Scholar] [CrossRef]
- Sorrentino, R.; Ruggiero, G.; Leone, R.; Ferrari, M.; Zarone, F. Area accuracy gradient and artificial markers: A three-dimensional analysis of the accuracy of IOS scans on the completely edentulous upper jaw. J. Osseointeg. 2021, 13, S257–S264. [Google Scholar] [CrossRef]
- Fang, J.-H.; An, X.; Jeong, S.-M.; Choi, B.-H. Digital intraoral scanning technique for edentulous jaws. J. Prosthet. Dent. 2018, 119, 733–735. [Google Scholar] [CrossRef]
- Jamjoom, F.Z.; Aldghim, A.; Aldibasi, O.; Yilmaz, B. Impact of intraoral scanner, scanning strategy, and scanned arch on the scan accuracy of edentulous arches: An in vitro study. J. Prosthet. Dent. 2023, 131, 1218–1225. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Caradonna, G.; Troiano, G.; Salamini, A.; Guida, L.; Ciavarella, D. Three-dimensional differences between intraoral scans and conventional impressions of edentulous jaws: A clinical study. J. Prosthet. Dent. 2020, 123, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Chebib, N.; Kalberer, N.; Srinivasan, M.; Maniewicz, S.; Perneger, T.; Müller, F. Edentulous jaw impression techniques: An in vivo comparison of trueness. J. Prosthet. Dent. 2019, 121, 623–630. [Google Scholar] [CrossRef]
- Patzelt, S.B.M.; Vonau, S.; Stampf, S.; Att, W. Assessing the feasibility and accuracy of digitizing edentulous jaws. J. Am. Dent. Assoc. 2013, 144, 914–920. [Google Scholar] [CrossRef]
- Osman, R.B.; Alharbi, N.M. Influence of scan technology on the accuracy and speed of intraoral scanning systems for the edentulous maxilla: An in vitro study. J. Prosthodont. 2023, 32, 821–828. [Google Scholar] [CrossRef]
- Resende, C.C.D.; Barbosa, T.A.Q.; Moura, G.F.; Tavares, L.D.N.; Rizzante, F.A.P.; George, F.M.; das Neves, F.D.; Mendonça, G. Influence of operator experience, scanner type, and scan size on 3D scans. J. Prosthet. Dent. 2021, 125, 294–299. [Google Scholar] [CrossRef]
- Revell, G.; Simon, B.; Mennito, A.; Evans, Z.P.; Renne, W.; Ludlow, M.; Vág, J. Evaluation of complete-arch implant scanning with 5 different intraoral scanners in terms of trueness and operator experience. J. Prosthet. Dent. 2022, 128, 632–638. [Google Scholar] [CrossRef]
- Lim, J.-H.; Park, J.-M.; Kim, M.; Heo, S.-J.; Myung, J.-Y. Comparison of digital intraoral scanner reproducibility and image trueness considering repetitive experience. J. Prosthet. Dent. 2018, 119, 225–232. [Google Scholar] [CrossRef]
- Ma, Y.; Guo, Y.; Jiang, L.; Yu, H. Influence of intraoral conditions on the accuracy of digital and conventional implant impression techniques for two-implant-supported fixed dental prostheses. J. Prosthodont. Res. 2023, 67, 633–640. [Google Scholar] [CrossRef]
| Sum of Squares | df | Mean Square | F | Sig. | |
|---|---|---|---|---|---|
| Between Groups | 0.26 | 2 | 0.128 | 0.05 | 0.95 |
| Within Groups | 70.93 | 27 | 2.63 | ||
| Total | 71.18 | 29 |
| Sum of Squares | df | Mean Square | F | Sig. | ||
|---|---|---|---|---|---|---|
| Time_Taken | Between Groups | 0.030 | 2 | 0.01 | 0.06 | 0.94 |
| Within Groups | 46.52 | 177 | 0.26 | |||
| Total | 46.54 | 179 | ||||
| Scan_stops | Between Groups | 5.733 | 2 | 2.86 | 4.123 | 0.02 |
| Within Groups | 123.06 | 177 | 0.69 | |||
| Total | 128.80 | 179 | ||||
| Dependent Variable | (I) Scanner | (J) Scanner | Mean Difference (I-J) | Std. Error | Sig. | 95% Confidence Interval | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Time_Taken | Trios 4 | iTero | 0.032 | 0.093 | 0.939 | −0.18 | 0.25 |
| Carestream | 0.014 | 0.093 | 0.988 | −0.20 | 0.23 | ||
| iTero | Trios 4 | −0.032 | 0.093 | 0.939 | −0.25 | 0.19 | |
| Carestream | −0.02 | 0.093 | 0.980 | −0.23 | 0.20 | ||
| Carestream | Trios 4 | −0.014 | 0.093 | 0.988 | −0.23 | 0.21 | |
| iTero | 0.02 | 0.093 | 0.980 | −0.20 | 0.24 | ||
| Scan_stops | Trios 4 | iTero | 0.17 | 0.15 | 0.519 | −0.19 | 0.52 |
| Carestream | 0.43 | 0.15 | 0.014 | 0.07 | 0.79 | ||
| iTero | Trios 4 | −0.16 | 0.15 | 0.519 | −0.52 | 0.19 | |
| Carestream | 0.26 | 0.15 | 0.189 | −0.09 | 0.63 | ||
| Carestream | Trios 4 | −0.43 | 0.15 | 0.014 | −0.79 | −0.07 | |
| iTero | −0.26 | 0.15 | 0.189 | −0.63 | 0.09 | ||
| Dependent Variable: Time_Taken | |||||
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
| Corrected Model | 0.070 a | 8 | 0.009 | 0.032 | 1.000 |
| Intercept | 244.961 | 1 | 244.96 | 901.26 | 0.000 |
| Scanner | 0.030 | 2 | 0.015 | 0.056 | 0.946 |
| Strategy | 0.002 | 2 | 0.001 | 0.003 | 0.997 |
| Scanner Strategy | 0.038 | 4 | 0.009 | 0.035 | 0.998 |
| Error | 46.477 | 171 | 0.272 | ||
| Total | 291.570 | 180 | |||
| Corrected Total | 46.547 | 179 | |||
| a. R Squared = 0.002 (Adjusted R Squared = −0.045) | |||||
| Dependent Variable: Scan_Stops | |||||
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
| Corrected Model | 7.949 a | 8 | 0.994 | 1.406 | 0.197 |
| Intercept | 51.097 | 1 | 51.097 | 72.300 | 0.000 |
| Scanner | 5.761 | 2 | 2.880 | 4.076 | 0.019 |
| Strategy | 0.632 | 2 | 0.316 | 0.447 | 0.640 |
| Scanner Strategy | 1.589 | 4 | 0.397 | 0.562 | 0.691 |
| Error | 120.851 | 171 | 0.707 | ||
| Total | 180.000 | 180 | |||
| Corrected Total | 128.800 | 179 | |||
| a. R Squared = 0.062 (Adjusted R Squared = 0.018) | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Unnikrishnan, J.; Bakr, M.; Love, R.; Idris, G. Enhancing Effective Scanning Techniques for Digital Impression in Neonates with Cleft Lip and/or Palate: A Laboratory Study Investigating the Impact of Different Scanners, Scanning Tip Sizes, and Strategies. Children 2024, 11, 1435. https://doi.org/10.3390/children11121435
Unnikrishnan J, Bakr M, Love R, Idris G. Enhancing Effective Scanning Techniques for Digital Impression in Neonates with Cleft Lip and/or Palate: A Laboratory Study Investigating the Impact of Different Scanners, Scanning Tip Sizes, and Strategies. Children. 2024; 11(12):1435. https://doi.org/10.3390/children11121435
Chicago/Turabian StyleUnnikrishnan, Jyotsna, Mahmoud Bakr, Robert Love, and Ghassan Idris. 2024. "Enhancing Effective Scanning Techniques for Digital Impression in Neonates with Cleft Lip and/or Palate: A Laboratory Study Investigating the Impact of Different Scanners, Scanning Tip Sizes, and Strategies" Children 11, no. 12: 1435. https://doi.org/10.3390/children11121435
APA StyleUnnikrishnan, J., Bakr, M., Love, R., & Idris, G. (2024). Enhancing Effective Scanning Techniques for Digital Impression in Neonates with Cleft Lip and/or Palate: A Laboratory Study Investigating the Impact of Different Scanners, Scanning Tip Sizes, and Strategies. Children, 11(12), 1435. https://doi.org/10.3390/children11121435







