The Diagnosis and Management of Infraoccluded Deciduous Molars: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Processing
2.2. Effect Measures
- -
- Prevalence: Percentage of infraoccluded primary molars in study populations.
- -
- Severity: Depth of infraocclusion classified as mild, moderate, or severe.
- -
- Dental Anomalies: Odds ratios (ORs) for associations with conditions like agenesis and tipping.
- -
- Occlusal Impact: Measurements of adjacent tooth tipping and space loss.
- -
- Treatment Outcomes: Success rates of interventions, such as spontaneous eruption.
2.3. Inclusion and Exclusion Criteria
- Studies with open access written in English;
- Studies that performed the research “in vivo” or in “humans”;
- Case–control studies, cohort studies, RCTs;
- Studies that were published in the last 15 years;
- Only IODMs.
- -
- Screening: Studies that did not fit the fundamental inclusion criteria were first weeded out of the titles and abstracts.
- -
- Full-Text Review: Following that, two impartial reviewers looked over the entire text to make sure it met all inclusion and exclusion requirements.
- -
- Resolution of Discrepancies: Any disputes were settled by dialogue or the advice of a third reviewer.
2.4. PICo Question
- I.
- Population (P):
- II.
- Phenomenon of Interest (I):
- III.
- Context (Co):
2.5. Data Processing
3. Results
3.1. Characteristics of Included Articles
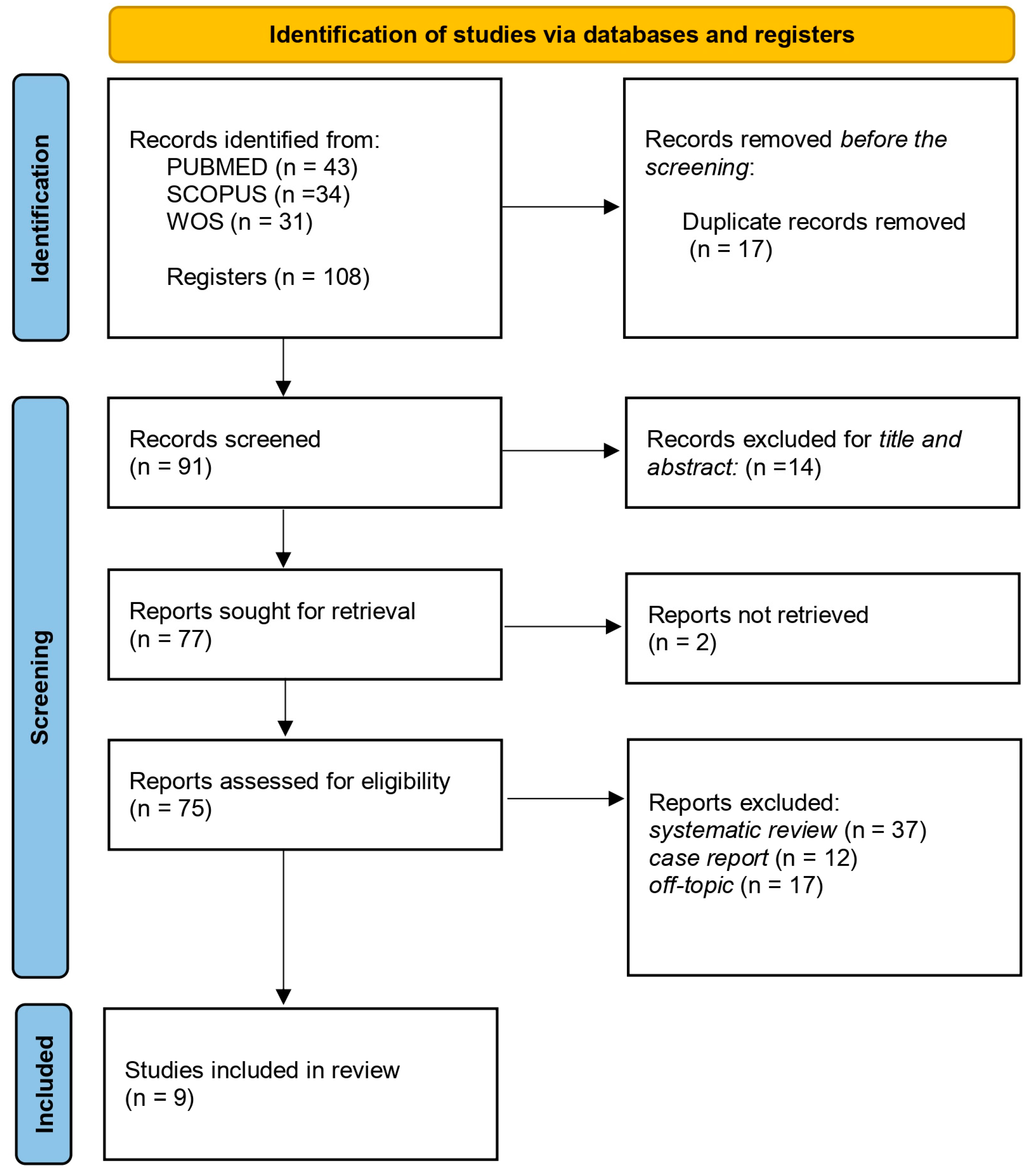
3.2. Descriptive Summary of Item Selection
3.3. Quality Assessment and Risk of Bias of Included Articles
3.4. Implications for Practice, Policy, and Research
- -
- Practice: Routine screening for infraoccluded molars in children’s dental exams is essential for early intervention and preventing complications like tooth tipping and space loss.
- -
- Policy: Standardized diagnostic and intervention guidelines are needed to improve detection and management across different regions.
- -
- Research: Future studies should focus on the long-term outcomes of IO treatments, the genetic factors involved, and developing consistent diagnostic criteria to guide treatment.
4. Discussion
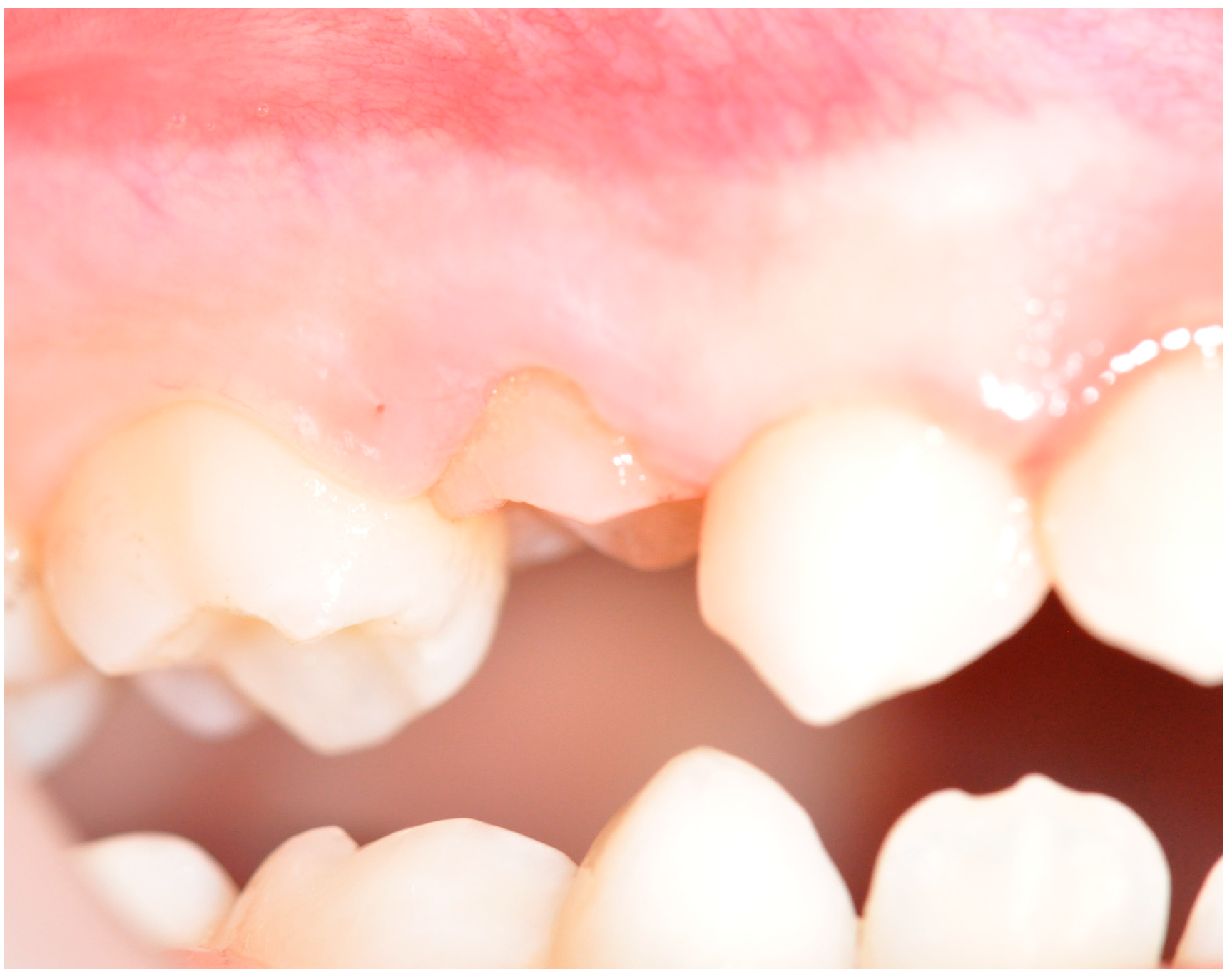
4.1. IO and Causes
- -
- environmental
- -
- developmental
- -
- hereditary
4.2. IO Diagnosis Techniques
- -
- Panoramic Radiographs: This is a widely accessible, quick, and cost-effective option for identifying infraocclusion, especially in initial assessments. However, panoramic radiographs offer limited resolution and can distort tooth size and position, which may hinder precise measurements of the infraocclusion depth or subtle structural changes [80].
- -
- Periapical Radiographs: These provide greater detail for IO teeth in specific areas, allowing for clearer visualization of root resorption, periodontal ligament (PDL) status, and bone structure around the infraoccluded tooth. While useful for localized diagnostics, periapical radiographs lack the full-arch perspective that panoramic radiographs offer, which can be limiting for treatment planning [26].
- -
- Cone-Beam Computed Tomography (CBCT): CBCT provides a 3D view, offering highly detailed visualization of the tooth structure, root morphology, surrounding bone, and PDL space, which is ideal for evaluating ankylosis and precise measurements of IO depth. Despite its accuracy, CBCT is often more costly and has a higher radiation dose than 2D techniques, so it is generally reserved for complex cases or when conventional radiographs are inconclusive [17].
- -
- Intraoral Photography: Though not technically a radiographic technique, intraoral photography allows clinicians to document the occlusal relationship visually, providing an additional reference point for infraocclusion’s impact on aesthetics and functionality. This method, however, cannot visualize underlying bone or root conditions and is generally used as a supplementary tool alongside radiographic technique [71].
4.3. IO Prevalence
4.4. IO and Root Resorption
4.5. Severe IO and Associated Anomalies
4.6. Dental Variations and Developmental Impact
4.7. IO Management
- -
- For mild cases without progressive infraocclusion or complications, periodic observation is often sufficient, especially if successor teeth are expected to erupt normally;
- -
- When IO teeth affect occlusion, restorations like composite resin build-ups can raise the tooth’s occlusal height to align with the dental arch, preserving space and function temporarily;
- -
- In severe cases, or when significant tipping or space loss occurs, extraction followed by space maintenance (e.g., a space maintainer) is recommended. This approach prevents adjacent teeth from shifting into the gap, allowing space for future dental implants or orthodontic treatment;
- -
- For cases involving significant space loss, orthodontic appliances may be used to regain lost space or to guide the alignment of impacted permanent teeth;
- -
- In adults or in cases where there is no permanent successor, implants or prosthetic replacements can be considered after extraction, particularly to restore function and esthetics in the long term.
5. Conclusions
- Prevalence: IO of primary molars is a common condition in children, requiring early diagnosis to prevent further dental complications.
- Causes and Complications: It results from disruptions in tooth eruption, leading to misalignment, root resorption, and space loss, affecting oral function and aesthetics.
- Diagnosis: Clinical and radiographic evaluations are essential to detect IO early and prevent complications like tooth tilting and impacted premolars.
- Treatment: Management depends on the severity, with mild cases monitored and severe ones requiring intervention like extraction or space maintenance.
- Genetic Factors: IO is linked to other dental anomalies, suggesting a genetic component that requires tailored treatment strategies.
- Long-term Impact: Untreated IO can cause delayed tooth eruption and increase the risk of caries, stressing the importance of timely treatment.
6. Limitations of the Study and Future Directions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AG | Agenesis |
| DAP | Dental Anomaly Pattern |
| FPM | First permanent molar |
| IO | Infraocclusion |
| IODM | Infraoccluded deciduous/primary molars |
| M2P | Mandibular second premolar |
| MIH | Molar–incisor hypomineralization |
| OPT | Orthopantomography |
| 2pm | Second primary molar |
| SPM | Second permanent molar |
References
- Webby, M.N.; Sullivan, M.P.; Yegambaram, K.M.; Radjainia, M.; Keown, J.R.; Kingston, R.L. A Method for Analyzing the Composition of Viral Nucleoprotein Complexes, Produced by Heterologous Expression in Bacteria. Virology 2019, 527, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Bergendal, B.; Bergendal, T.; Hallonsten, A.-L.; Koch, G.; Kurol, J.; Kvint, S. A Multidisciplinary Approach to Oral Rehabilitation with Osseointegrated Implants in Children and Adolescents with Multiple Aplasia. Eur. J. Orthod. 1996, 18, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Lygidakis, N.A.; Chatzidimitriou, K.; Lygidakis, N.N. A Novel Approach for Building up Infraoccluded Ankylosed Primary Molars in Cases of Missing Premolars: A Case Report. Eur. Arch. Paediatr. Dent. 2015, 16, 425–429. [Google Scholar] [CrossRef]
- Mancini, A.; Chirico, F.; Inchingolo, A.M.; Piras, F.; Colonna, V.; Marotti, P.; Carone, C.; Inchingolo, A.D.; Inchingolo, F.; Dipalma, G. Osteonecrosis of the Jaws Associated with Herpes Zoster Infection: A Systematic Review and a Rare Case Report. Microorganisms 2024, 12, 1506. [Google Scholar] [CrossRef] [PubMed]
- Contaldo, M.; Itro, A.; Lajolo, C.; Gioco, G.; Inchingolo, F.; Serpico, R. Overview on Osteoporosis, Periodontitis and Oral Dysbiosis: The Emerging Role of Oral Microbiota. Appl. Sci. 2020, 10, 6000. [Google Scholar] [CrossRef]
- Caliskan, S.; Tuloglu, N.; Celik, O.; Ozdemir, C.; Kizilaslan, S.; Bayrak, S. A Pilot Study of a Deep Learning Approach to Submerged Primary Tooth Classification and Detection. Int. J. Comput. Dent. 2021, 24, 1–9. [Google Scholar] [CrossRef]
- Farret, M.M.; Farret, M.M.B. Absence of Multiple Premolars and Ankylosis of Deciduous Molar with Cant of the Occlusal Plane Treated Using Skeletal Anchorage. Angle Orthod. 2015, 85, 134–141. [Google Scholar] [CrossRef]
- Dokova, A.F.; Lee, J.Y.; Mason, M.; Moretti, A.; Reside, G.; Christensen, J. Advancements in Tooth Autotransplantation. J. Am. Dent. Assoc. 2024, 155, 475–483. [Google Scholar] [CrossRef]
- Laudadio, C.; Inchingolo, A.D.; Malcangi, G.; Limongelli, L.; Marinelli, G.; Coloccia, G.; Montenegro, V.; Patano, A.; Inchingolo, F.; Bordea, I.R.; et al. Management of Anterior Open-Bite in the Deciduous, Mixed and Permanent Dentition Stage: A Descriptive Review. J. Biol. Regul. Homeost. Agents 2021, 35, 271–281. [Google Scholar] [CrossRef]
- Laforgia, A.; Inchingolo, A.D.; Piras, F.; Colonna, V.; Giorgio, R.V.; Carone, C.; Rapone, B.; Malcangi, G.; Inchingolo, A.M.; Inchingolo, F. Therapeutic Strategies and Genetic Implications for Periodontal Disease Management: A Systematic Review. Int. J. Mol. Sci. 2024, 25, 7217. [Google Scholar] [CrossRef]
- Bjerklin, K.; Bennett, J. The Long-Term Survival of Lower Second Primary Molars in Subjects with Agenesis of the Premolars. Eur. J. Orthod. 2000, 22, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Jaikaria, A.; Thakur, S. Alveolar Ridge Preservation in a Growing Patient with Decoronation: One-Year Follow-Up. J. Indian. Soc. Pedod. Prev. Dent. 2019, 37, 214–217. [Google Scholar] [CrossRef] [PubMed]
- Aktan, A.M.; Kara, I.; Şener, I.; Bereket, C.; Çelik, S.; Kirtay, M.; Çifti, M.E.; Arici, N. An Evaluation of Factors Associated with Persistent Primary Teeth. Eur. J. Orthod. 2012, 34, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Inchingolo, A.D.; Palumbo, I.; Guglielmo, M.; Balestriere, L.; Casamassima, L.; Ciccarese, D.; Marotti, P.; Mancini, A.; Palermo, A.; et al. Management of Physiological Gingival Melanosis by Diode Laser Depigmentation versus Surgical Scalpel: A Systematic Review. Dent. Rev. 2024, 4, 100146. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ferrara, I.; Viapiano, F.; Netti, A.; Campanelli, M.; Buongiorno, S.; Latini, G.; Carpentiere, V.; Ciocia, A.M.; Ceci, S.; et al. Rapid Maxillary Expansion on the Adolescent Patient: Systematic Review and Case Report. Children 2022, 9, 1046. [Google Scholar] [CrossRef]
- Selz, C.F.; Jung, B.A.; Guess, P.C. An Interdisciplinary Noninvasive All-Ceramic Treatment Concept for Nonsyndromic Oligodontia in Adolescence. Quintessence Int. 2015, 46, 111–118. [Google Scholar] [CrossRef]
- Demirel, A.; Sarı, Ş. Are Increased Masticatory Forces Risk for Primary 2nd Molars without Successors? A 3D FEA Study. J. Clin. Pediatr. Dent. 2019, 43, 64–68. [Google Scholar] [CrossRef]
- Kolokitha, O.-E.; Balli, D.; Zarkadi, A.-E.; Gizani, S. Association between Maxillary Canine Impaction and Other Dental Anomalies: Radiological Study of a Mixed Dentition Children’s Cohort from an Orthodontic Clinic. Eur. Arch. Paediatr. Dent. 2023, 24, 401–407. [Google Scholar] [CrossRef]
- Bambini, F.; Memè, L.; Pellecchia, M.; Sabatucci, A.; Selvaggio, R. Comparative Analysis of Deformation of Two Implant/Abutment Connection Systems during Implant Insertion. An in Vitro Study. Minerva Stomatol. 2005, 54, 129–138. [Google Scholar]
- Giorgini, E.; Sabbatini, S.; Conti, C.; Rubini, C.; Rocchetti, R.; Fioroni, M.; Memè, L.; Orilisi, G. Fourier Transform Infrared Imaging Analysis of Dental Pulp Inflammatory Diseases. Oral Dis. 2017, 23, 484–491. [Google Scholar] [CrossRef]
- Bilińska, M.; Burzykowski, T.; Plakwicz, P.; Zadurska, M.; Czochrowska, E.M. Availability of Third Molars as Donor Teeth for Autotransplantation to Replace Congenitally Absent Second Premolars in Children and Young Adults. Diagnostics 2023, 13, 1874. [Google Scholar] [CrossRef]
- Bhuyan, L.; Dhull, K.S.; Pattnaik, S.; Devraj, I.M.; Nishat, R.; Panda, A. CAD—CAM in Pediatric Dentistry: A Brief Insight. Bangladesh J. Med. Sci. 2024, 23, S38–S42. [Google Scholar] [CrossRef]
- Nessa, K.; Anwar, N.; Ghosh, R.; Mondal, S.; Alam, M.K. Case Report: Utilization of Residual Space of Deciduous Second Molar to Align Teeth in a Crowded Arch. Bangladesh J. Med. Sci. 2020, 19, 763–768. [Google Scholar] [CrossRef]
- Kjær, I.; Fink-Jensen, M.; Andreasen, J.O. Classification and Sequelae of Arrested Eruption of Primary Molars. Int. J. Paediatr. Dent. 2008, 18, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Dipalma, G.; Ferrara, I.; Viapiano, F.; Netti, A.; Ciocia, A.M.; Mancini, A.; Malcangi, G.; Palermo, A.; Inchingolo, A.M.; et al. Clear Aligners in the Growing Patient: A Systematic Review. Children 2024, 11, 385. [Google Scholar] [CrossRef]
- Dipalma, G.; Inchingolo, A.D.; Inchingolo, A.M.; Piras, F.; Carpentiere, V.; Garofoli, G.; Azzollini, D.; Campanelli, M.; Paduanelli, G.; Palermo, A.; et al. Artificial Intelligence and Its Clinical Applications in Orthodontics: A Systematic Review. Diagnostics 2023, 13, 3677. [Google Scholar] [CrossRef]
- Rossi, R.; Memè, L.; Strappa, E.M.; Bambini, F. Restoration of Severe Bone and Soft Tissue Atrophy by Means of a Xenogenic Bone Sheet (Flex Cortical Sheet): A Case Report. Appl. Sci. 2023, 13, 692. [Google Scholar] [CrossRef]
- Wong, M.L.; Awang, C.F.; Ng, L.K.; Norlian, D.; Burhanudin, R.D.; Gere, M.J. Role of Interceptive Orthodontics in Early Mixed Dentition. Singap. Dent. J. 2004, 26, 10–14. [Google Scholar]
- Al-Abdallah, M.; AlHadidi, A.; Hammad, M.; Al-Ahmad, H.; Saleh, R. Prevalence and Distribution of Dental Anomalies: A Comparison between Maxillary and Mandibular Tooth Agenesis. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 793–798. [Google Scholar] [CrossRef]
- Kurol, J. Infraocclusion of Primary Molars. An Epidemiological, Familial, Longitudinal Clinical and Histological Study. Swed. Dent. J. Suppl. 1984, 21, 1–67. [Google Scholar]
- Noble, J.; Karaiskos, N.; Wiltshire, W.A. Diagnosis and Management of the Infraerupted Primary Molar. Br. Dent. J. 2007, 203, 632–634. [Google Scholar] [CrossRef] [PubMed]
- Heggie, C.; Gartshore, L. Diagnosis, Management and Follow-Up of a Rare Regional Developmental Disorder: Segmental Odontomaxillary Dysplasia. J. Dent. Child 2020, 87, 39–43. [Google Scholar]
- Weinstein, C.; Hirschhaut, M.; Flores-Mir, C. Clinical Pearls for the Management of Maxillary Impacted Canines: Lessons Learned from 14 Patients. AJO-DO Clin. Companion 2024, 4, 376–415. [Google Scholar] [CrossRef]
- Cantekin, K.; Celikoglu, M. Comparison of the Dental Anomaly Frequency in Patients with and without Mandibular Second Premolar Agenesis. J. Dent. Sci. 2015, 10, 185–189. [Google Scholar] [CrossRef]
- Laskowska, J.; Paradowska-Stolarz, A.; Miralles-Jordá, L.; Schutty, D.; Mikulewicz, M. Complication of Orthodontic Treatment: A Case Report on Severe Apical Root Resorption (ARR) in a Patient with Turner Syndrome. Children 2024, 11, 358. [Google Scholar] [CrossRef]
- Oh, N.-Y.; Nam, S.-H.; Lee, J.-S.; Kim, H.-J. Delayed Spontaneous Eruption of Severely Infraoccluded Primary Second Molar: Two Case Reports. J. Clin. Pediatr. Dent. 2020, 44, 185–189. [Google Scholar] [CrossRef]
- Laganà, G.; Venza, N.; Borzabadi-Farahani, A.; Fabi, F.; Danesi, C.; Cozza, P. Dental Anomalies: Prevalence and Associations between Them in a Large Sample of Non-Orthodontic Subjects, a Cross-Sectional Study. BMC Oral Health 2017, 17. [Google Scholar] [CrossRef]
- Shalish, M.; Gal, A.; Brin, I.; Zini, A.; Ben-Bassat, Y. Prevalence of Dental Features That Indicate a Need for Early Orthodontic Treatment. Eur. J. Orthod. 2013, 35, 454–459. [Google Scholar] [CrossRef]
- Wotjiuk, F.; Hyon, I.; Dajean-Trutaud, S.; Badran, Z.; Prud’homme, T. Dental Management of Neurofibromatosis Type 1: A Case Report and Literature Review. Int. J. Clin. Pediatr. Dent. 2019, 12, 577–581. [Google Scholar] [CrossRef]
- Cherian, J.M.; Samuel, S.; Sabu, A.M.; Thomas, A.M.; Injety, R.J. Dental Implants in Growing Patients: A Quality Assessment of Systematic Reviews. J. Oral Biol. Craniofacial Res. 2023, 13, 610–615. [Google Scholar] [CrossRef]
- Torlińska-Walkowiak, N.; Tuczyńska, M.; Kucharska, K.; Wyzga, S.; Singh, N.; Łukomska-Pochylska, M.; Fudalej, O.; Opydo-Szymaczek, J. Infraocclusion—An Anomaly in Primary Dentition. Pediatr. I. Med. Rodz. 2022, 18, 341–344. [Google Scholar] [CrossRef]
- Alanzi, A.; Bufersen, N.; Haider, S.; Abdulrahim, M. Prevalence and Distribution of Dental Anomalies in Schoolchildren in Kuwait. Int. Dent. J. 2024, 74, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Renugalakshmi, A.; Vinothkumar, T.S.; Bokhari, A.M.; Almahdi, S.; Almalki, A.; Balla, S.B.; Tadakamadla, S.K.; Hakami, Z. Prevalence of Dental Anomalies and Its Role in Sex Estimation among Children of Jazan Region, Saudi Arabia. Children 2023, 10, 759. [Google Scholar] [CrossRef] [PubMed]
- Haghighi, S.; Gharekhani, S.; Abesi, F.; Ghasempour, M.; Hajian-Tilaki, K. Prevalence of Ectopic Maxillary Canine and Its Association With Other Dental Anomalies In Children: An Observational Study. East. J. Med. 2023, 28, 133–138. [Google Scholar] [CrossRef]
- Inchingolo, F.; Ferrara, I.; Viapiano, F.; Ciocia, A.M.; Palumbo, I.; Guglielmo, M.; Inchingolo, A.D.; Palermo, A.; Bordea, I.R.; Inchingolo, A.M.; et al. Primary Failure Eruption: Genetic Investigation, Diagnosis and Treatment: A Systematic Review. Children 2023, 10, 1781. [Google Scholar] [CrossRef]
- Hanisch, M.; Hanisch, L.; Kleinheinz, J.; Jung, S. Primary Failure of Eruption (PFE): A Systematic Review. Head Face Med. 2018, 14, 1–9. [Google Scholar] [CrossRef]
- Cardoso Silva, C.; Maroto Edo, M.; Soledad Alvaro Llorente, M.; Barbería Leache, E. Primary Molar Infraocclusion: Frequency, Magnitude, Root Resorption and Premolar Agenesis in a Spanish Sample. Eur. J. Paediatr. Dent. 2014, 15, 258–264. [Google Scholar]
- Rasidi, M.Q.Z.B.M.; Bhagya Lakhsmi, T.; Prabu, D. Pulpectomy in Maxillary First Molars with Distal Caries. Int. J. Res. Pharm. Sci. 2020, 11, 447–451. [Google Scholar] [CrossRef]
- Ristaniemi, J.; Karjalainen, T.; Kujasalo, K.; Rajala, W.; Pesonen, P.; Lähdesmäki, R. Radiological Features and Treatment of Erupting Maxillary Canines in Relation to the Occurrence of Dental Developmental Abnormalities. Acta Odontol. Scand. 2024, 83, 197–203. [Google Scholar] [CrossRef]
- Caleya, A.M.; Gallardo, N.E.; Feijoo, G.; Mourelle-Martínez, M.R.; Martín-Vacas, A.; Maroto, M. Relationship between Physiological Resorption of Primary Molars with Its Permanent Successors, Dental Age and Chronological Age. Children 2022, 9, 941. [Google Scholar] [CrossRef]
- De Moura, M.S.; Pontes, A.S.; Brito, M.H.S.F.; de Deus Moura, L.; de Deus Moura de Lima, M.; de Melo Simplício, A.H. Restorative Management of Severely Ankylosed Primary Molars. J. Dent. Child 2015, 82, 41–46. [Google Scholar]
- Pereira, P.M.; Ferreira, A.P.; Tavares, P.; Braga, A.C. Different Manifestations of Class II Division 2 Incisor Retroclination and Their Association with Dental Anomalies. J. Orthod. 2013, 40, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Janosy, A.-M.; Moca, A.E.; Juncar, R.I. Early Diagnosis and Treatment of Mandibular Second Premolar Impaction: A Case Report. Diagnostics 2024, 14, 1610. [Google Scholar] [CrossRef] [PubMed]
- Bauman, J.M.; Souza, J.G.S.; Bauman, C.D.; Flório, F.M. Epidemiological Pattern of Malocclusion in Brazilian Preschoolers. Cienc. E Saude Coletiva 2018, 23, 3861–3868. [Google Scholar] [CrossRef] [PubMed]
- Meade, M.J.; Dreyer, C.W. Eruption Disturbances in the Mixed Dentition: Orthodontic Considerations for Primary Dental Care. Aust. Dent. J. 2022, 67, S14–S23. [Google Scholar] [CrossRef]
- Zhou, C.; Duan, P.; He, H.; Song, J.; Hu, M.; Liu, Y.; Liu, Y.; Guo, J.; Jin, F.; Cao, Y.; et al. Expert Consensus on Pediatric Orthodontic Therapies of Malocclusions in Children. Int. J. Oral Sci. 2024, 16, 32. [Google Scholar] [CrossRef]
- Sigler, L.M.; Baccetti, T.; McNamara, J.A. Effect of Rapid Maxillary Expansion and Transpalatal Arch Treatment Associated with Deciduous Canine Extraction on the Eruption of Palatally Displaced Canines: A 2-Center Prospective Study. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e235–e244. [Google Scholar] [CrossRef]
- Malcangi, G.; Patano, A.; Ciocia, A.M.; Netti, A.; Viapiano, F.; Palumbo, I.; Trilli, I.; Guglielmo, M.; Inchingolo, A.D.; Dipalma, G.; et al. Benefits of Natural Antioxidants on Oral Health. Antioxidants 2023, 12, 1309. [Google Scholar] [CrossRef]
- Malcangi, G.; Patano, A.; Morolla, R.; De Santis, M.; Piras, F.; Settanni, V.; Mancini, A.; Di Venere, D.; Inchingolo, F.; Inchingolo, A.D.; et al. Analysis of Dental Enamel Remineralization: A Systematic Review of Technique Comparisons. Bioengineering 2023, 10, 472. [Google Scholar] [CrossRef]
- Inchingolo, F.; Inchingolo, A.M.; Latini, G.; Palmieri, G.; Di Pede, C.; Trilli, I.; Ferrante, L.; Inchingolo, A.D.; Palermo, A.; Lorusso, F.; et al. Application of Graphene Oxide in Oral Surgery: A Systematic Review. Materials 2023, 16, 6293. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Dipalma, G.; Viapiano, F.; Netti, A.; Ferrara, I.; Ciocia, A.M.; Mancini, A.; Di Venere, D.; Palermo, A.; Inchingolo, A.M.; et al. Celiac Disease-Related Enamel Defects: A Systematic Review. J. Clin. Med. 2024, 13, 1382. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.M.; Patano, A.; De Santis, M.; Del Vecchio, G.; Ferrante, L.; Morolla, R.; Pezzolla, C.; Sardano, R.; Dongiovanni, L.; Inchingolo, F.; et al. Comparison of Different Types of Palatal Expanders: Scoping Review. Children 2023, 10, 1258. [Google Scholar] [CrossRef] [PubMed]
- Dewhurst, S.N.; Harris, J.C.; Bedi, R. Infraocclusion of Primary Molars in Monozygotic Twins: Report of Two Cases. Int. J. Paediatr. Dent. 1997, 7, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Altay, N.; Cengiz, S.B. Space-Regaining Treatment for a Submerged Primary Molar: A Case Report. Int. J. Paediatr. Dent. 2002, 12, 286–289. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Avantario, P.; Azzollini, D.; Buongiorno, S.; Viapiano, F.; Campanelli, M.; Ciocia, A.M.; Leonardis, N.D.; et al. Effects of Resveratrol, Curcumin and Quercetin Supplementation on Bone Metabolism—A Systematic Review. Nutrients 2022, 14, 3519. [Google Scholar] [CrossRef]
- Schneider-Moser, U.E.M.; Moser, L.; Perakis, N. Esthetic and Periodontal Management of Missing Lower Anterior Teeth. Semin. Orthod. 2024, 30, 206–219. [Google Scholar] [CrossRef]
- Yuan, G.H.; Wang, Y. Etiology and clinical treatment strategies for second primary molars without permanent tooth germs. Zhonghua Kou Qiang Yi Xue Za Zhi 2024, 59, 738–744. [Google Scholar] [CrossRef]
- Tian, X.; Yuan, G.H. Etiology, diagnosis and treatment of infraoccluded primary second molars. Zhonghua Kou Qiang Yi Xue Za Zhi 2022, 57, 192–195. [Google Scholar] [CrossRef]
- Arhakis, A.; Boutiou, E. Etiology, Diagnosis, Consequences and Treatment of Infraoccluded Primary Molars. Open Dent. J. 2016, 10, 714–719. [Google Scholar] [CrossRef]
- Ishizuka, K.; Kato, C.; Fujita, A.; Misawa-Omori, E.; Ono, T. Factors Influencing Root Resorption in Retained Mandibular Second Deciduous Molars with Congenital Absence of Second Premolars: A Cross-Sectional Study. Prog. Orthod. 2024, 25, 14. [Google Scholar] [CrossRef]
- Hvaring, C.L.; Øgaard, B.; Stenvik, A.; Birkeland, K. The Prognosis of Retained Primary Molars without Successors: Infraocclusion, Root Resorption and Restorations in 111 Patients. Eur. J. Orthod. 2014, 36, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Shalish, M.; Har-Zion, G.; Zini, A.; Harari, D.; Chaushu, S. Deep Submersion: Severe Phenotype of Deciduous-Molar Infraocclusion with Biological Associations. Angle Orthod. 2014, 84, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Odeh, R.; Townsend, G.; Mihailidis, S.; Lähdesmäki, R.; Hughes, T.; Brook, A. Infraocclusion: Dental Development and Associated Dental Variations in Singletons and Twins. Arch. Oral Biol. 2015, 60, 1394–1402. [Google Scholar] [CrossRef] [PubMed]
- Díaz Schiappacasse, F.; Aguilera-Muñoz, F.; Cayo-Parra, V.; Guido-Garay, K. Prevalence of Infraocclusion in Primary Molars of Children 7 and 8 Years Old, Valdivia, Chile, 2019. Odontoestomatología 2020, 22, 4–11. [Google Scholar] [CrossRef]
- Alshaya, S.I.; Alanazi, A.F.; Aldawish, S.S.; Alsuhaim, M.M.; Alomar, M.S.; Almuaytiq, Y.M.; Alfahad, S.A.; Almousa, A.A.S.; Alassaf, A.; Mallineni, S.K. Infraocclusion: Prevalence, Characteristics, and Associated Dental Anomalies in Arabian Children. BioMed Res. Int. 2022, 2022, 4804. [Google Scholar] [CrossRef]
- Eşian, D.; Bica, C.I.; Stoica, O.E.; Dako, T.; Vlasa, A.; Bud, E.S.; Salcudean, D.; Beresescu, L. Prevalence and Manifestations of Dental Ankylosis in Primary Molars Using Panoramic X-Rays: A Cross-Sectional Study. Children 2022, 9, 1188. [Google Scholar] [CrossRef]
- Calheiros-Lobo, M.J.; Costa, F.; Pinho, T. Infraocclusion Level and Root Resorption of the Primary Molar in Second Premolar Agenesis: A Retrospective Cross-Sectional Study in the Portuguese Population. Dent. Med. Probl. 2022, 59, 195–207. [Google Scholar] [CrossRef]
- Akgöl, B.B.; Üstün, N.; Bayram, M. Characterizing Infraocclusion in Primary Molars: Prevalence, Accompanying Findings, and Infraocclusion Severity and Treatment Implications. BMC Oral Health 2024, 24. [Google Scholar] [CrossRef]
- Marcianes, M.; Garcia-Camba, P.; Albaladejo, A.; Varela Morales, M. Potential Association of Molar-Incisor Hypomineralization (MIH) with Dental Agenesis and Infraoccluded Deciduous Molars: Is MIH Related to Dental Anomaly Pattern (DAP)? An Observational Cross-Sectional Study. J. Clin. Med. 2024, 13, 2445. [Google Scholar] [CrossRef]
- Williams, R.; Park, J.H.; Chae, J.-M.; Vaden, J.L. The Congenitally Missing Second Premolar: Space Closure. A Viable Option. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 571–583.e16. [Google Scholar] [CrossRef]
- Cavare, A.; Decaup, P.-H.; Boileau, M.-J.; Garot, E. Patterns and Sexual Dimorphism of Non-Syndromic Hypodontia among a French Orthodontic Population. Arch. Oral Biol. 2024, 159, 105894. [Google Scholar] [CrossRef]
- Grageda, E.; Grageda, E. Periodontal Plastic Surgery for the Management of an Ankylosed Permanent Maxillary Lateral Incisor: A Clinical Report with 5-Year Follow-Up. J. Prosthet. Dent. 2022, 127, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Schonberger, S.; Kadry, R.; Shapira, Y.; Finkelstein, T. Permanent Tooth Agenesis and Associated Dental Anomalies among Orthodontically Treated Children. Children 2023, 10, 596. [Google Scholar] [CrossRef] [PubMed]
- Ith-Hansen, K.; Kjær, I. Persistence of Deciduous Molars in Subjects with Agenesis of the Second Premolars. Eur. J. Orthod. 2000, 22, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Badrov, J.; Gašpar, G.; Tadin, A.; Galić, T.; Govorko, D.K.; Gavić, L.; Badrov, R.; Galić, I. Prevalence and Characteristics of Congenitally Missing Permanent Teeth among Orthodontic Patients in Southern Croatia. Acta Stomatol. Croat. 2017, 51, 290–299. [Google Scholar] [CrossRef]
- Souza-Silva, B.N.; Vieira, W.d.A.; Bernardino, Í.d.M.; Batista, M.J.; Bittencourt, M.A.V.; Paranhos, L.R. Non-Syndromic Tooth Agenesis Patterns and Their Association with Other Dental Anomalies: A Retrospective Study. Arch. Oral Biol. 2018, 96, 26–32. [Google Scholar] [CrossRef]
- Lochib, S.; Indushekar, K.R.; Saraf, B.G.; Sheoran, N.; Sardana, D. Occlusal Characteristics and Prevalence of Associated Dental Anomalies in the Primary Dentition. J. Epidemiol. Glob. Health 2015, 5, 151–157. [Google Scholar] [CrossRef]
- Fourneron, M.; Tourbah, B.; Scibilia, J.; Frapier, L. Ortho- Perio- Prosthetic Interdisciplinary Approach of an Adult Class II Division 2 with Multiple Premolar Agenesis: A Case Report. Int. Orthod. 2023, 21, 729. [Google Scholar] [CrossRef]
- Thilander, B.; Ödman, J.; Gröteborg, K.; Friberg, B. Osseointegrated Implants in Adolescents. An Alternative in Replacing Missing Teeth? Eur. J. Orthod. 1994, 16, 84–95. [Google Scholar] [CrossRef]
- Dhanrajani, P.J.; Al Abdulkarim, S. Management of Severe Hypodontia. Implant. Dent. 2002, 11, 338–342. [Google Scholar] [CrossRef]
- Tayab, T.; AlFardan, A.E.; Hasan, E.A.R. Management of Severe Infraocclusion of the Primary Second Molar Leading to Impaction of Second Premolar. J. Dent. Child 2023, 90, 96–101. [Google Scholar]
- Quevedo, B.; Miranda, F.; Pereira Lauris, J.R.; Ferrari Junior, F.M.; Garib, D. Mandibular Second Premolar Distoangulation: A Longitudinal Follow-up from the Mixed to the Permanent Dentition. Eur. J. Orthod. 2023, 45, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Walshaw, E.G.; Noble, F.; Conville, R.; Anne Lawson, J.; Hasmun, N.; Rodd, H. Molar Incisor Hypomineralisation and Dental Anomalies: A Random or Real Association? Int. J. Paediatr. Dent. 2020, 30, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Miyanaga, M.; Takei, K.; Maeda, T. Observation of a Child with Multiple Submerged Primary Teeth. ASDC J. Dent. Child. 1998, 65, 439, 495–498. [Google Scholar] [PubMed]
- Patano, A.; Malcangi, G.; Inchingolo, A.D.; Garofoli, G.; Leonardis, N.D.; Azzollini, D.; Latini, G.; Mancini, A.; Carpentiere, V.; Laudadio, C.; et al. Mandibular Crowding: Diagnosis and Management—A Scoping Review. J. Pers. Med. 2023, 13, 774. [Google Scholar] [CrossRef]
- Inchingolo, F.; Inchingolo, A.M.; Latini, G.; Ferrante, L.; Trilli, I.; Del Vecchio, G.; Palmieri, G.; Malcangi, G.; Inchingolo, A.D.; Dipalma, G. Oxidative Stress and Natural Products in Orthodontic Treatment: A Systematic Review. Nutrients 2023, 16, 113. [Google Scholar] [CrossRef]
- Roslan, A.A.; Rahman, N.A.; Alam, M.K. Dental Anomalies and Their Treatment Modalities/Planning in Orthodontic Patients. J. Orthod. Sci. 2018, 7, 16. [Google Scholar] [CrossRef]
- Stabryła, J.; Zadurska, M.; Plakwicz, P.; Kukuła, K.T.; Czochrowska, E.M. Comparisons of Dental Anomalies in Orthodontic Patients with Impacted Maxillary and Mandibular Canines. Diagnostics 2023, 13, 2766. [Google Scholar] [CrossRef]
- Zimmer, B.; Schelper, I.; Seifi-Shirvandeh, N. Localized Orthodontic Space Closure for Unilateral Aplasia of Lower Second Premolars. Eur. J. Orthod. 2007, 29, 210–216. [Google Scholar] [CrossRef][Green Version]
- Ng, A.; Ong, D.; Goh, P. Management of a Patient with a Severely Infraoccluded Primary Molar and Hypodontia. Clin. Case Rep. 2022, 10, e6482. [Google Scholar] [CrossRef]
- McGeown, M.; O’Connell, A. Management of Primary Molar Infraocclusion in General Practice. J. Ir. Dent. Assoc. 2014, 60, 192–198. [Google Scholar] [PubMed]
- Friedlander, L.; Choquet, R.; Galliani, E.; De Chalendar, M.; Messiaen, C.; Ruel, A.; Vazquez, M.-P.; Berdal, A.; Alberti, C.; De La Dure Molla, M. Management of Rare Diseases of the Head, Neck and Teeth: Results of a French Population-Based Prospective 8-Year Study. Orphanet J. Rare Dis. 2017, 12, 94. [Google Scholar] [CrossRef] [PubMed]
- Odeh, R.; Mihailidis, S.; Townsend, G.; Lähdesmäki, R.; Hughes, T.; Brook, A. Prevalence of Infraocclusion of Primary Molars Determined Using a New 2D Image Analysis Methodology. Aust. Dent. J. 2016, 61, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Nagayama, K.; Ogaya, Y.; Hamada, M.; Okawa, R.; Uzawa, N.; Nakano, K. Severe Dislocation of Mandibular Second Premolar Associated with Deep Ankylosis of Primary Molar. Pediatr. Dent. J. 2022, 32, 116–122. [Google Scholar] [CrossRef]
- Garcovich, D.; Aiuto, R.; Martin, M.A. Space Regaining Made Easy: The Case of a Severely Infraoccluded Primary Molar. Case Rep. Dent. 2019, 2019, 6916839. [Google Scholar] [CrossRef]
- Caldeira, A.V.; Souza, A.C.A.; Miguel, M.A.T.; Ribeiro, I.P.; Almeida Júnior, L.A.; Sakai, V.T.; Moretti, A.B.S. Surgical and Orthodontic Treatment after Incidental Radiographic Discovery of a Severely Infraoccluded Primary Molar. Gen. Dent. 2019, 67, 72–75. [Google Scholar]
- Angelopoulou, V.-A.; Pouliakis, A.; Alexiou, N.; Ioannidi, P.; Vagiona, D.; Ekmektzoglou, K.; Xanthos, T.; Boutsikou, T.; Iliodromiti, Z.; Iacovidou, N. The Effects of Dexmedetomidine on Children Undergoing Magnetic Resonance Imaging: A Systematic Review and Meta-Analysis. Children 2023, 10, 948. [Google Scholar] [CrossRef]
- Sharif, M.O.; Parker, K.; Lyne, A.; Chia, M.S.Y. The Orthodontic-Oral Surgery Interface. Part Two: Diagnosis and Management of Anomalies in Eruption and Transpositions. Br. Dent. J. 2018, 225, 491–496. [Google Scholar] [CrossRef]
- Sehra, B.; Johnson, J. The Prosthetic Management of an Infra-Occluded First Permanent Molar: Case Report. Dent. Update 2016, 43, 482–484, 486. [Google Scholar] [CrossRef]
- Naoumova, J.; Kjellberg, H. The Use of Panoramic Radiographs to Decide When Interceptive Extraction Is Beneficial in Children with Palatally Displaced Canines Based on a Randomized Clinical Trial. Eur. J. Orthod. 2018, 40, 565–574. [Google Scholar] [CrossRef]
- Patano, A.; Inchingolo, A.M.; Laudadio, C.; Azzollini, D.; Marinelli, G.; Ceci, S.; Latini, G.; Rapone, B.; Inchingolo, A.D.; Mancini, A.; et al. Therapeutic Strategies of Primary Molar Infraocclusion: A Systematic Review. Children 2023, 10, 582. [Google Scholar] [CrossRef] [PubMed]
- Hua, L.; Thomas, M.; Bhatia, S.; Bowkett, A.; Merrett, S. To Extract or Not to Extract? Management of Infraoccluded Second Primary Molars without Successors. Br. Dent. J. 2019, 227, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Adamska, P.; Pylińska-Dąbrowska, D.; Stasiak, M.; Sobczak-Zagalska, H.; Jusyk, A.; Zedler, A.; Studniarek, M. Tooth Autotransplantation, Autogenous Dentin Graft, and Growth Factors Application: A Method for Preserving the Alveolar Ridge in Cases of Severe Infraocclusion—A Case Report and Literature Review. J. Clin. Med. 2024, 13, 3902. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Chow, Y.-L.; Xu, K.; Hardiman, R.; Schneider, P.; Tan, S.-S. Transcriptome Analysis of Ankylosed Primary Molars with Infraocclusion. Int. J. Oral Sci. 2020, 12, 7. [Google Scholar] [CrossRef] [PubMed]
- Savoldi, F.; Dalessandri, D.; Gardoni, A.; Dianiskova, S.; Bonetti, S.; Visconti, L. Treatment of Ankylosed Deciduous Molars with or without Permanent Successors in Children and Adolescents: A Systematic Review. Minerva Dent. Oral Sci. 2021, 70, 276–285. [Google Scholar] [CrossRef]
- Medio, M.; de la Dure Molla, M. Treatment of infra-occluded primary molars in patients with dental ageneses. Int. Orthod. 2014, 12, 291–302. [Google Scholar] [CrossRef]
- Bartolo, A.; Camilleri, A.; Camilleri, S. Unerupted Incisors—Characteristic Features and Associated Anomalies. Eur. J. Orthod. 2010, 32, 297–301. [Google Scholar] [CrossRef]
- Tunc, E.S.; Bayrak, S. Usage of White Mineral Trioxide Aggregate in a Non-Vital Primary Molar with No Permanent Successor. Aust. Dent. J. 2010, 55, 92–95. [Google Scholar] [CrossRef]
- Dos Santos, C.C.O.; Melo, D.L.; Da Silva, P.P.; Normando, D. What Is the Survival Rate of Deciduous Molars in Cases with Agenesis of Premolar Successors? A Systematic Review. Angle Orthod. 2022, 92, 110–117. [Google Scholar] [CrossRef]
- Memè, L.; Notarstefano, V.; Sampalmieri, F.; Orilisi, G.; Quinzi, V. ATR-FTIR Analysis of Orthodontic Invisalign® Aligners Subjected to Various In Vitro Aging Treatments. Materials 2021, 14, 818. [Google Scholar] [CrossRef]
- Pasquale, P.; Gaetano, M.; Giovanni, D.O.; Luigi, C.; Gilberto, S. Autologous Fat Grafting in Facial Volumetric Restoration. J. Craniofac. Surg. 2015, 26, 756–759. [Google Scholar] [CrossRef] [PubMed]
- Gasparro, R.; Adamo, D.; Masucci, M.; Sammartino, G.; Mignogna, M.D. Use of Injectable Platelet-Rich Fibrin in the Treatment of Plasma Cell Mucositis of the Oral Cavity Refractory to Corticosteroid Therapy: A Case Report. Dermatol. Ther. 2019, 32, e13062. [Google Scholar] [CrossRef] [PubMed]
- Ristaniemi, J.; Kujasalo, K.; Rytkönen, E.; Melaluoto, E.; Iivari, J.; Pesonen, P.; Lähdesmäki, R. Features of Dental Anomaly Patterns in Finnish Children as Seen in Panoramic Radiographs at the Late Mixed Stage. Acta Odontol. Scand. 2023, 81, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Khare, V.; Nayak, P.A.; Khandelwal, V.; Nayak, U.A. Fixed Functional Space Maintainer: Novel Aesthetic Approach for Missing Maxillary Primary Anterior Teeth. BMJ Case Rep. 2013, 2013, bcr2013009585. [Google Scholar] [CrossRef]
- Thumbigere-Math, V.; Alqadi, A.; Chalmers, N.I.; Chavez, M.B.; Chu, E.Y.; Collins, M.T.; Ferreira, C.R.; FitzGerald, K.; Gafni, R.I.; Gahl, W.A.; et al. Hypercementosis Associated with ENPP1 Mutations and GACI. J. Dent. Res. 2018, 97, 432–441. [Google Scholar] [CrossRef]
- Barber, S.; Bekker, H.L.; Meads, D.; Pavitt, S.; Khambay, B. Identification and Appraisal of Outcome Measures Used to Evaluate Hypodontia Care: A Systematic Review. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 184–194.e18. [Google Scholar] [CrossRef]
- Shalish, M.; Peck, S.; Wasserstein, A.; Peck, L. Increased Occurrence of Dental Anomalies Associated with Infraocclusion of Deciduous Molars. Angle Orthod. 2010, 80, 440–445. [Google Scholar] [CrossRef]
- Nagpal, A.; Pai, K.M.; Sharma, G. Palatal and Labially Impacted Maxillary Canine-Associated Dental Anomalies: A Comparative Study. J. Contemp. Dent. Pr. 2009, 10, 67–74. [Google Scholar]
- Jacobs, S.G. The Impacted Maxillary Canine. Further Observations on Aetiology, Radiographic Localization, Prevention/Interception of Impaction, and When to Suspect Impaction. Aust. Dent. J. 1996, 41, 310–316. [Google Scholar] [CrossRef]
- Grassi, A.; Memè, L.; Strappa, E.M.; Martini, E.; Bambini, F. Modified Periosteal Inhibition (MPI) Technique for Extraction Sockets: A Case Series Report. Appl. Sci. 2022, 12, 12292. [Google Scholar] [CrossRef]
- Termine, N.; Panzarella, V.; Ciavarella, D.; Lo Muzio, L.; D’Angelo, M.; Sardella, A.; Compilato, D.; Campisi, G. Antibiotic Prophylaxis in Dentistry and Oral Surgery: Use and Misuse. Int. Dent. J. 2009, 59, 263–270. [Google Scholar]
- Compilato, D.; Cirillo, N.; Termine, N.; Kerr, A.R.; Paderni, C.; Ciavarella, D.; Campisi, G. Long-Standing Oral Ulcers: Proposal for a New “S-C-D Classification System. J. Oral Pathol. Med. 2009, 38, 241–253. [Google Scholar] [CrossRef]
- Bambini, F.; De Stefano, C.A.; Giannetti, L.; Memè, L.; Pellecchia, M. Influence of biphosphonates on the integration process of endosseous implants evaluated using single photon emission computerized tomography (SPECT). Minerva Stomatol. 2003, 52, 331–338. [Google Scholar]
- Scandurra, C.; Gasparro, R.; Dolce, P.; Bochicchio, V.; Muzii, B.; Sammartino, G.; Marenzi, G.; Maldonato, N.M. The Role of Cognitive and Non-Cognitive Factors in Dental Anxiety: A Mediation Model. Eur. J. Oral Sci. 2021, 129, e12793. [Google Scholar] [CrossRef]
- Sammartino, G.; Marenzi, G.; Tammaro, L.; Bolognese, A.; Calignano, A.; Costantino, U.; Califano, L.; Mastrangelo, F.; Tetè, S.; Vittoria, V. Anti-Inflammatory Drug Incorporation into Polymeric Nano-Hybrids for Local Controlled Release. Int. J. Immunopathol. Pharmacol. 2005, 18, 55–62. [Google Scholar]
- Sammartino, G.; Marenzi, G.; Howard, C.M.; Minimo, C.; Trosino, O.; Califano, L.; Claudio, P.P. Chondrosarcoma of the Jaw: A Closer Look at Its Management. J. Oral Maxillofac. Surg. 2008, 66, 2349–2355. [Google Scholar] [CrossRef]
- Lo Russo, L.; Ciavarella, D.; Salamini, A.; Guida, L. Alignment of Intraoral Scans and Registration of Maxillo-Mandibular Relationships for the Edentulous Maxillary Arch. J. Prosthet. Dent. 2019, 121, 737–740. [Google Scholar] [CrossRef]

| Article-screening strategy | KEYWORDS: “A”: molar IO; “B”: primary molar IO; “C”: infra-occluded molar; “D”: IO of primary molars. |
| Boolean Indicators: “A” OR “B” OR “C” OR “D”. | |
| Timespan: 1 September 2024 to 10 September 2024 | |
| Electronic databases: PubMed; Scopus; Web of Science. |
| Authors and Years | Type of Study | Aim of the Study | Materials | Outcomes |
|---|---|---|---|---|
| Hvaring, C.L. et al. (2014) [71] | Retrospective observational Study | To assess IO, root resorption, and restorations in retained primary mandibular molars without permanent successors in patients with severe hypodontia. | 111 patients, 188 retained primary mandibular second molars, OPT, Facad software for measurements. | IO was found in 43.6% of patients, with severe cases in 18.8%. A significant correlation was observed between IO and root resorption. Age also showed a weak correlation with both IO and root resorption. Restorations were not significant in prognosis. |
| Shalish, M. et al. (2014) [72] | Retrospective Study | To evaluate treatment modalities for deep submersion and its association with other dental anomalies. | 25 orthodontic patients with IODM, dental records, radiographs | Treatment resulted in spontaneous eruption in 95% of cases. Increased prevalence of dental anomalies in deep submersion cases. |
| Odeh, R. et al. (2015) [73] | Retrospective Study | To investigate the association between IO, dental variations, and dental development in singletons/twins | 1454 radiographs of singletons (8–11 years), and 202 twins (8–11 years) dental models. | Significant association of IO with canine eruption anomalies and lateral incisor complex. Delayed dental development and smaller mandibular canines in IO cases. |
| Díaz Schiappacasse, F. et al. (2020) [74] | Cross-sectional study | To determine the prevalence of IO in primary molars of children aged 7 and 8 in Valdivia, Chile | Examination of 359 children in educational institutions, using the Brearley and McKibben classification for IO evaluation. Statistical analyses with chi-square and ANOVA tests | 41.78% prevalence of IO. - 82.06% of cases were mild, 15.28% moderate, and 2.66% severe. - Statistically significant differences in IO location and severity. (p < 0.05) |
| Alshaya, S.I. (2022) [75] | Retrospective cross-sectional study | Analyze the prevalence, distribution, and characteristics of IO in primary dentition among Arabian children and its associated dental anomalies. | 542 children aged 4–12 years from the pediatric dental clinic at Majmaah University, Saudi Arabia | IO is common in mandibular second primary molars, predominantly mild, and associated with anomalies like hypodontia. Regular follow-up is advised. |
| Eşian, D. et al. (2022) [76] | Retrospective cross-sectional radiographic analysis | To analyze the prevalence, characteristics, and associated dental anomalies of IO among Arabian children in primary dentition | OPT of 542 children attending the pediatric dental clinic at Majmaah University, Saudi Arabia, from January 2019 to May 2021. | 7.38% prevalence of IODM. - IO was more common in males (90%) and mandibular second primary molars (58%). - Hypodontia (12.5%) and supernumerary teeth (5%) were the most frequently associated anomalies. |
| Calheiros-Lobo, M.J. et al. (2022) [77] | Retrospective cross-sectional | To evaluate the lifespan and functionality of retained second primary molars in cases of second premolar agenesis (AG), particularly the extent of IO and root resorption. | 2.949 OPTs were analyzed from patients aged 7–36 years. A sample of 61 patients was selected for analysis based on retention of second primary molars. | Second primary molars remained functional for up to 25 years. - IO and root resorption increased with age, with critical loss phases at ages 11–15 and 21–25. - Mesial movement of adjacent teeth was absent. - A non-intervention approach could be considered in cases without other complications. |
| Akgöl, B.B. et al. (2024) [78] | Retrospective cross-sectional study | To investigate the prevalence, classification, accompanying findings, and treatment interventions related to IODMs in children. | 4.828 OPT of children aged 3 to 15 years. | Prevalence of IO was 4.3%. - Most cases (84.8%) were classified as mild (Group I), with more severe cases requiring extraction. - Accompanying findings included tipping of adjacent teeth, midline shifts, and increased caries. - Premolar AG was identified in 2% of cases, and extraction was more frequent when the successor tooth was malpositioned. |
| Marcianes, M. et al. (2024) [79] | Observational cross-sectional study | To explore potential associations between molar–incisor hypomineralization (MIH) and two specific dental anomalies: AG and IODM | Sample of 574 children aged 8–14 years, 287 with MIH and 287 without MIH. OPT and standardized intraoral photographs were used. | - No significant association between MIH and dental AG (7% in MIH group vs. 8% in non-MIH group). - No significant association between MIH and IODM (27% vs. 19.2%, p = 0.082). |
| Authors (Year) | D1 | D2 | D3 | D4 | D5 | D6 | Overall |
|---|---|---|---|---|---|---|---|
| Hvaring, C.L. et al. (2014) [71] |  |  |  |  |  |  |  |
| Shalish, M. et al. (2014) [72] |  |  |  |  |  |  |  |
| Odeh, R. et al. (2015) [73] |  |  |  |  |  |  |  |
| Díaz Schiappacasse, F. et al. (2020) [74] |  |  |  |  |  |  |  |
| Alshaya, S.I. et al. (2022) [75] |  |  |  |  |  |  |  |
| Eşian, D. et al. (2022) [76] |  |  |  |  |  |  |  |
| Calheiros-Lobo, M.J. et al. (2022) [77] |  |  |  |  |  |  |  |
| Akgöl, B.B. et al. (2024) [78] |  |  |  |  |  |  |  |
| Marcianes, M. et al. (2024) [79] |  |  |  |  |  |  |  |
| Domains: | Judgement: | ||||||
| D1: Bias due to confounding. | Very High |  | |||||
| D2: Bias arising from the measurement of the exposure. | High |  | |||||
| D3: Bias in the selection of participants in the study (or in the analysis). | Some Concerns |  | |||||
| D4: Bias due to post-exposure interventions. | Low |  | |||||
| D5: Bias due to missing data. | No Information |  | |||||
| D6: Bias arising from measurement of the outcome. | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dipalma, G.; Inchingolo, A.D.; Memè, L.; Casamassima, L.; Carone, C.; Malcangi, G.; Inchingolo, F.; Palermo, A.; Inchingolo, A.M. The Diagnosis and Management of Infraoccluded Deciduous Molars: A Systematic Review. Children 2024, 11, 1375. https://doi.org/10.3390/children11111375
Dipalma G, Inchingolo AD, Memè L, Casamassima L, Carone C, Malcangi G, Inchingolo F, Palermo A, Inchingolo AM. The Diagnosis and Management of Infraoccluded Deciduous Molars: A Systematic Review. Children. 2024; 11(11):1375. https://doi.org/10.3390/children11111375
Chicago/Turabian StyleDipalma, Gianna, Alessio Danilo Inchingolo, Lucia Memè, Lucia Casamassima, Claudio Carone, Giuseppina Malcangi, Francesco Inchingolo, Andrea Palermo, and Angelo Michele Inchingolo. 2024. "The Diagnosis and Management of Infraoccluded Deciduous Molars: A Systematic Review" Children 11, no. 11: 1375. https://doi.org/10.3390/children11111375
APA StyleDipalma, G., Inchingolo, A. D., Memè, L., Casamassima, L., Carone, C., Malcangi, G., Inchingolo, F., Palermo, A., & Inchingolo, A. M. (2024). The Diagnosis and Management of Infraoccluded Deciduous Molars: A Systematic Review. Children, 11(11), 1375. https://doi.org/10.3390/children11111375











