Parental Access to Healthcare following Paediatric Surgery—The Precarious Role of Parents as Providers of Care in the Home
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Setting
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Family Characteristics
3.2. Dimensions of Access
3.2.1. Approachability
would have probably wished that … given a follow-up relatively quickly after so that … or at least so that you could talk and ask a few questions about what you are worried about. BKK3
I was, was sent around a little at first, a little back and forth, but then finally I got in touch with someone who had, who had been with, had something to do with, my son. BKK5
3.2.2. Acceptability
Well, it felt both really nice and really scary and really strange … well, mostly really good, but also a bit strange of course. BKK11
Er, and, you did not get any real input about when, like the actual length of the care and treatment in recovery. I would have liked more information about that. BKK97
Then, like… it becomes my task to search for the information although it is the same organisation… Like, it would have been better if the primary (paediatric) nurse could start off by saying ‘Yes, okay, where have you been hospitalised? Yes, you’ve been there. Yes, good, then I will contact them.’ BKK6
3.2.3. Affordability
… we chose to do it like this anyway, as we lived so near the hospital…very close… and we have another child at home, so we wanted to go home. BKK35
… it was partly to avoid travelling three times a week [to the hospital], so we sent pictures instead. BKK11
3.2.4. Appropriateness
I thought that both nurses, doctors, and surgeons followed up well. We got information and what we should … like that we shouldn’t bathe him, but showering should be done and dabbing, so to speak, the wound there, and … yes, like that, what we should think about, and so on. BKK16
… one doctor says ‘Yes, but this is how it is and it should be done in this way. And we will do this and this and this’ … And then two days later you talk to another doctor, and then it is, and then it is not the same message that is being delivered. BKK97
3.2.5. Availability
And then when we … changed the dressing on the wound ourselves at the Child Health Centre, or fixed the bandage at the Child Health Centre, and then we were even in XXX, and had … because he also had these bruises on his hips, so we were there once a week and like bathed him. BKK6
We were called for a follow-up visit to the person who performed the surgery. But besides that, we had no [hospital] contact that I remember, which I maybe thought was a little surprising. BKK3
3.2.6. Aperture
We always take pictures at ten o’clock in the kitchen. It’s never good to send pictures by e-mail. [laughs] I don’t think we can do that, [laughs] so but … and it’s … well, no, maybe it would have been better if … they said that maybe we could have had some kind of video call, that might be better. BKK 11
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kristensson-Hallström, I. Parental participation in pediatric surgical care. AORN J. 2000, 71, 1021–1024. [Google Scholar] [CrossRef] [PubMed]
- Chua, G.C.C.; Cyna, A.M. Satisfaction measures in pediatric anesthesia and perioperative care. Pediatr. Anesth. 2021, 31, 746–754. [Google Scholar] [CrossRef]
- Kristjánsdóttir, O.; Sjöström-Strand, A.; Kristjánsdóttir, G. Living with the Memories—Parents’ Experiences of Their Newborn Child Undergoing Heart Surgery Abroad: A Qualitative Study. Int. J. Environ. Res. Public Health 2020, 17, 8840. [Google Scholar] [CrossRef] [PubMed]
- Lindkvist, R.-M.; Sjöström-Strand, A.; Landgren, K.; Johnsson, B.A.; Stenström, P.; Hallström, I.K. “In a Way We Took the Hospital Home”—A Descriptive Mixed-Methods Study of Parents’ Usage and Experiences of eHealth for Self-Management after Hospital Discharge Due to Pediatric Surgery or Preterm Birth. Int. J. Environ. Res. Public Health 2021, 18, 6480. [Google Scholar] [CrossRef] [PubMed]
- Aydon, L.; Hauck, Y.; Murdoch, J.; Siu, D.; Sharp, M. Transition from hospital to home: Parents’ perception of their preparation and readiness for discharge with their preterm infant. J. Clin. Nurs. 2018, 27, 269–277. [Google Scholar] [CrossRef]
- Kampouroglou, G.; Velonaki, V.-S.; Pavlopoulou, I.D.; Kosmopoulos, M.; Kouvas, N.; Drakou, E.; Skoutelis, N.; Spinos, D.; Tsagkaris, S.; Tsoumakas, K. Health literacy of parents/caregivers of paediatric surgical patients: A study on 1000 individuals. Afr. J. Paediatr. Surg. 2021, 18, 85–89. [Google Scholar] [CrossRef]
- Batterham, R.W.; Hawkins, M.; Collins, P.A.; Buchbinder, R.; Osborne, R.H. Health literacy: Applying current concepts to improve health services and reduce health inequalities. Public Health 2016, 132, 3–12. [Google Scholar] [CrossRef]
- Morrison, A.K.; Glick, A.; Yin, H.S. Health Literacy: Implications for Child Health. Pediatr. Rev. 2019, 40, 263–277. [Google Scholar] [CrossRef]
- Lawrence, P.R.; Feinberg, I.; Spratling, R. The Relationship of Parental Health Literacy to Health Outcomes of Children with Medical Complexity. J. Pediatr. Nurs. 2021, 60, 65–70. [Google Scholar] [CrossRef]
- Vilhjalmsson, R. Failure to seek needed medical care: Results from a national health survey of Icelanders. Soc. Sci. Med. 2005, 61, 1320–1330. [Google Scholar] [CrossRef]
- Levesque, J.-F.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef] [PubMed]
- Hylén, M.; Nilsson, S.; Kristensson-Hallström, I.; Kristjánsdóttir, G.; Stenström, P.; Vilhjálmsson, R. Access to health care perceived by parents caring for their child at home supported by eHealth—A directed approach introducing aperture. BMC Health Serv. Res. 2022, 22, 1008. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, H.-F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Ryan, G.; Vyrostek, S.; Aminoff, D.; Booth, K.; Driesbach, S.; Fisher, M.; Gerberick, J.; Haanen, M.; Mullins, C.; Parker, L.; et al. Importance of education and the role of the patient and family in the care of anorectal malformations. Semin. Pediatr. Surg. 2020, 29, 150990. [Google Scholar] [CrossRef] [PubMed]
- Young, K.; Gupta, A.; Palacios, R. Impact of Telemedicine in Pediatric Postoperative Care. Telemed. J. E-Health 2019, 25, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, J.B.; Cahill, D.; Young, K.; Humphrey, K.; Campbell, J.; Schumann, C.; Nelson, C.P.; Gupta, A.; Estrada, C.R., Jr. Telemedicine for Pediatric Urological Postoperative Care is Safe, Convenient and Economical. J. Urol. 2020, 204, 144–148. [Google Scholar] [CrossRef]
- Kim, D.-W.; Choi, J.-Y.; Han, K.-H. Risk management-based security evaluation model for telemedicine systems. BMC Med. Inform. Decis. Mak. 2020, 20, 106. [Google Scholar] [CrossRef]
- Denning, N.-L.; Glick, R.D.; Rich, B.S. Outpatient follow-up after pediatric surgery reduces emergency department visits and readmission rates. J. Pediatr. Surg. 2020, 55, 1037–1042. [Google Scholar] [CrossRef]
- de Buhr, E.; Tannen, A. Parental health literacy and health knowledge, behaviours and outcomes in children: A cross-sectional survey. BMC Public Health 2020, 20, 1096. [Google Scholar] [CrossRef]
- Kristjansdottir, G.; Hallström, I.K.; Vilhjalmsson, R. Sociodemographic and health status predictors of parental role strain: A general population study. Scand. J. Public Health 2020, 48, 519–526. [Google Scholar] [CrossRef]
- Ridgway, L.; Hackworth, N.; Nicholson, J.M.; McKenna, L. Working with families: A systematic scoping review of family-centred care in universal, community-based maternal, child, and family health services. J. Child Health Care 2021, 25, 268–289. [Google Scholar] [CrossRef] [PubMed]
- Mann, S. The Research Interview. In Reflective Practice and Reflexivity in Research Processes; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Wolf, T.G.; Schulze, R.K.W.; Ramos-Gomez, F.; Campus, G. Effectiveness of Telemedicine and Teledentistry after the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 13857. [Google Scholar] [CrossRef] [PubMed]
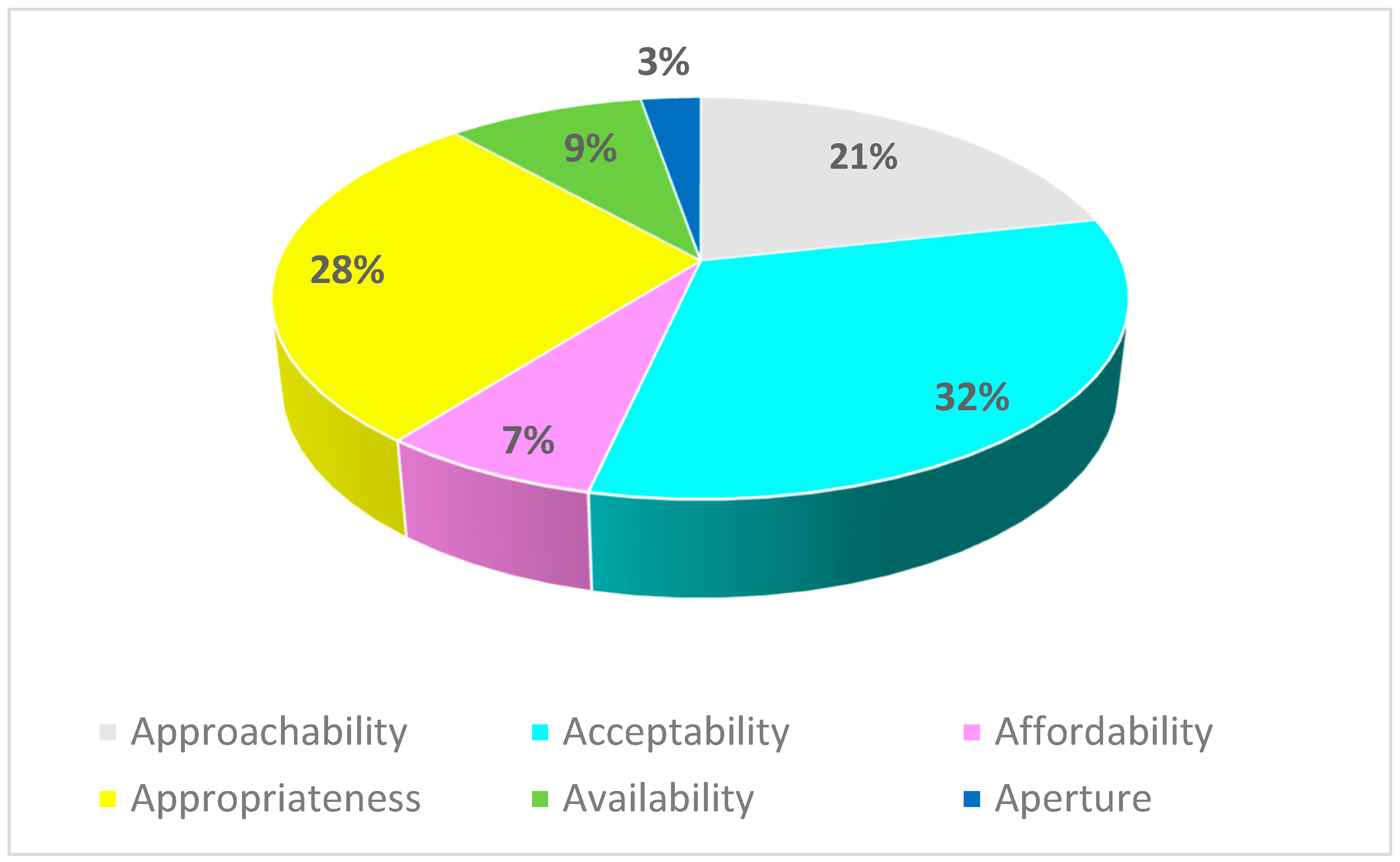
| Approachability | Parents in need of healthcare can identify their needs and are able to, and do, initiate contact with health services that could have an impact on their child’s health. |
| Acceptability | Parents accept the care offered, as well as their own role as providers of healthcare, and where, how, and what services are provided. |
| Affordability | Parents have the time and resources to use health services and find the use of those services worth the cost and effort. |
| Appropriateness | The coordination and continuity of care initiated by the health services (through virtual and onsite contacts with known providers) generate a fit between the services provided and the parents’ perceived needs. |
| Availability | Healthcare is obtained and reached either in the home or at the healthcare facilities. |
| Aperture | The pathways by which communication is transmitted in cyberspace are not easily visualised by parents submitting information to health professionals and, therefore, create uncertainty. |
| Age (in years) and gender of the interviewed parents and their child | |
| Gender of the parents: | |
| 10 (53) |
| 9 (47) |
| Age of the parents, median (range years) | 32 (24–40) |
| Age of the children, median (range months) | 12 (0.25–48) |
| Transportation to hospital | |
| 35 (15–180) |
| 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nilsson, S.; Hylén, M.; Kristensson-Hallström, I.; Kristjánsdóttir, G.; Stenström, P.; Vilhjálmsson, R. Parental Access to Healthcare following Paediatric Surgery—The Precarious Role of Parents as Providers of Care in the Home. Children 2023, 10, 1578. https://doi.org/10.3390/children10091578
Nilsson S, Hylén M, Kristensson-Hallström I, Kristjánsdóttir G, Stenström P, Vilhjálmsson R. Parental Access to Healthcare following Paediatric Surgery—The Precarious Role of Parents as Providers of Care in the Home. Children. 2023; 10(9):1578. https://doi.org/10.3390/children10091578
Chicago/Turabian StyleNilsson, Stefan, Mia Hylén, Inger Kristensson-Hallström, Gudrún Kristjánsdóttir, Pernilla Stenström, and Runar Vilhjálmsson. 2023. "Parental Access to Healthcare following Paediatric Surgery—The Precarious Role of Parents as Providers of Care in the Home" Children 10, no. 9: 1578. https://doi.org/10.3390/children10091578
APA StyleNilsson, S., Hylén, M., Kristensson-Hallström, I., Kristjánsdóttir, G., Stenström, P., & Vilhjálmsson, R. (2023). Parental Access to Healthcare following Paediatric Surgery—The Precarious Role of Parents as Providers of Care in the Home. Children, 10(9), 1578. https://doi.org/10.3390/children10091578










