Trained Lifeguards Performing Pediatric Cardiopulmonary Resuscitation While Running: A Pilot Simulation Study
Abstract
1. Introduction
2. Materials and Methods
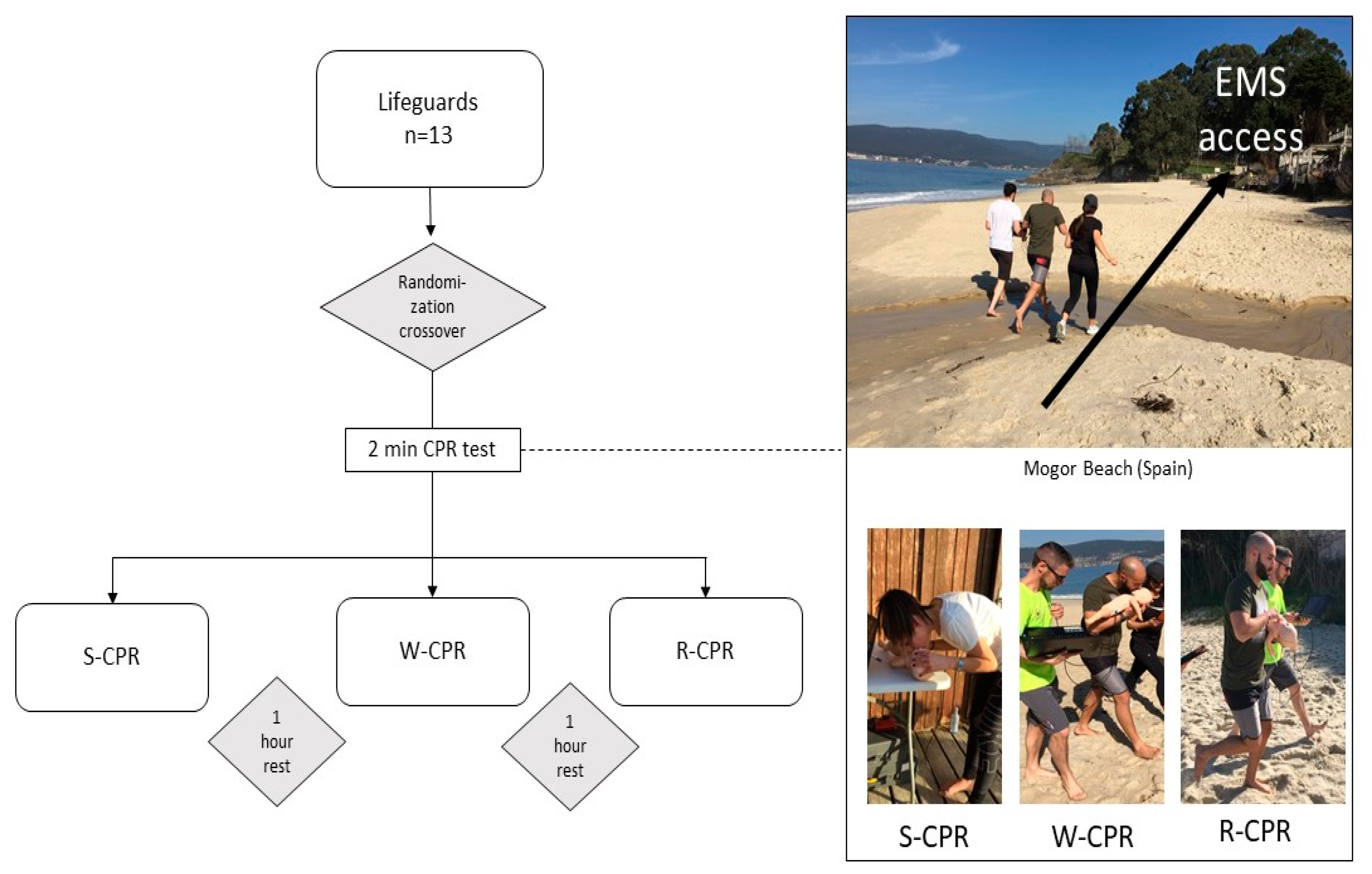
2.1. Study Design
2.2. Study Participants
2.3. Study Protocol
- (1)
- S-CPR/W-CPR/R-CPR
- (2)
- S-CPR/R-CPR/W-CPR
- (3)
- W-CPR/S-CPR/R-CPR
- (4)
- W-CPR/R-CPR/S-CPR
- (5)
- R-CPR/S-CPR/W-CPR
- (6)
- R-CPR/W-CPR/S-CPR
2.4. Conditions
2.5. Variables and Measuring Equipment
2.5.1. Cardiopulmonary Resuscitation Variables
- Chest Compressions (CC): Number of CC; Mean depth in mm; Mean rate in CC/min; Percentage of CC with adequate depth; Percentage of CC with adequate rate; Percentage of CC with adequate release; Percentage of CC with adequate hand position.
- Ventilations (V): Number of total V; Mean pause time for V in s; Number of effective V; Number of V with adequate volume; Number of V with excessive volume; Number of V with insufficient volume; Mean volume in ml.
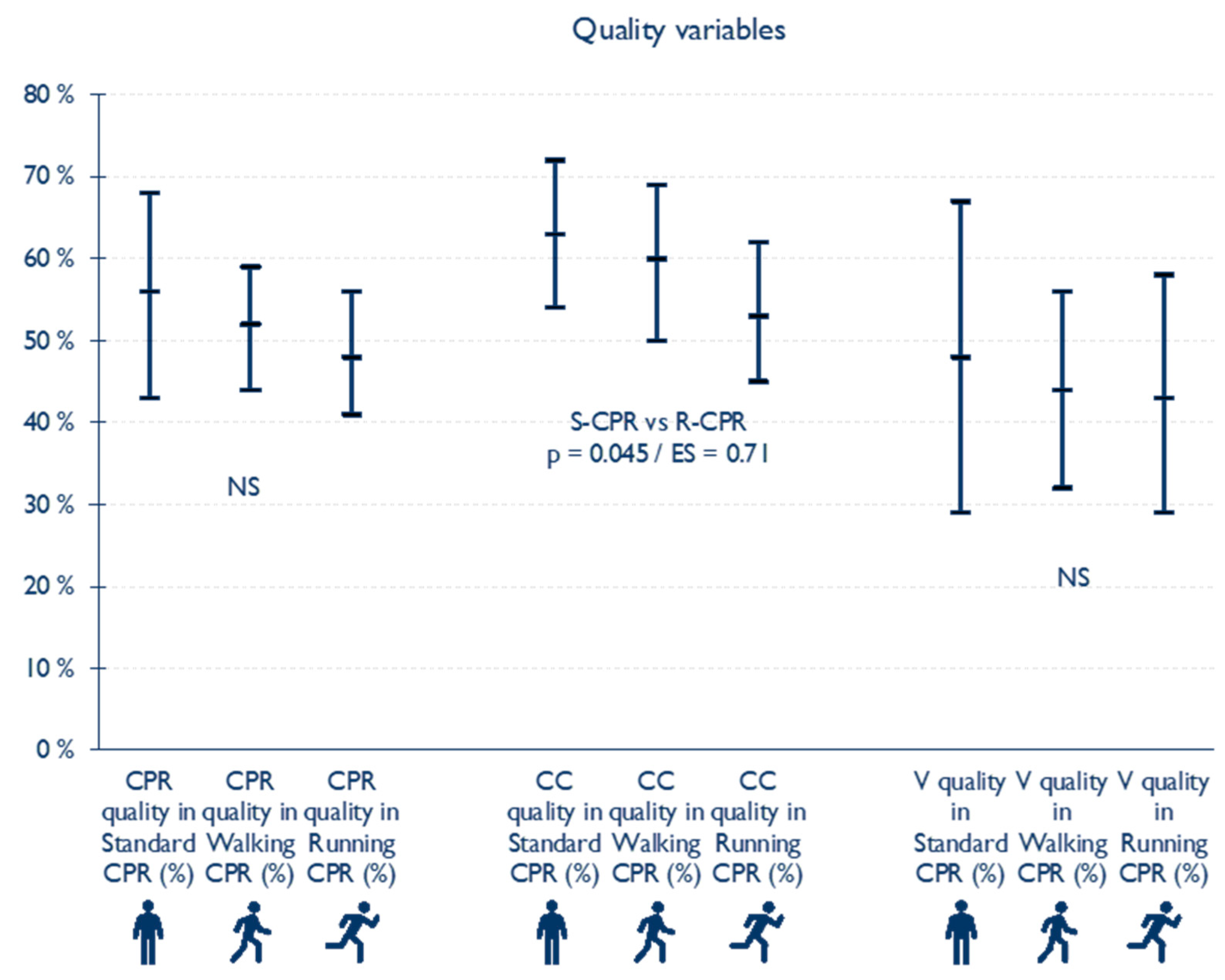
2.5.2. CPR Quality Variables
- CC quality, calculated using the formula: (CC with adequate depth + CC with correct chest recoil + CC with adequate rate) ÷ 3.
- V quality, calculated using the formula: Number of V with adequate volume ÷ Number of total V × 100.
- CPR quality, calculated using the formula: [(CC quality + V quality) ÷ 2].
2.5.3. Physiological and Effort Parameters
2.6. Statistical Analysis
3. Results
3.1. Cardiopulmonary Resuscitation Variables (Table 1)
3.2. Quality CPR Variables (Figure 2)
3.3. Physiological and Effort Parameters (Figure 3)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hasselqvist-Ax, I.; Riva, G.; Herlitz, J.; Rosenqvist, M.; Hollenberg, J.; Nordberg, P.; Ringh, M.; Jonsson, M.; Axelsson, C.; Lindqvist, J.; et al. Early Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac Arrest. New Engl. J. Med. 2015, 372, 2307–2315. [Google Scholar] [CrossRef]
- Wissenberg, M.; Lippert, F.K.; Folke, F.; Weeke, P.; Hansen, C.M.; Christensen, E.F.; Jans, H.; Hansen, P.A.; Lang-Jensen, T.; Olesen, J.B.; et al. Association of National Initiatives to Improve Cardiac Arrest Management With Rates of Bystander Intervention and Patient Survival After Out-of-Hospital Cardiac Arrest. JAMA 2013, 310, 1377–1384. [Google Scholar] [CrossRef]
- Perkins, G.D.; Graesner, J.-T.; Semeraro, F.; Olasveengen, T.; Soar, J.; Lott, C.; Van de Voorde, P.; Madar, J.; Zideman, D.; Mentzelopoulos, S.; et al. European Resuscitation Council Guidelines 2021: Executive Summary. Resuscitation 2021, 161, 1–60. [Google Scholar] [CrossRef]
- Topjian, A.A.; Raymond, T.T.; Atkins, D.; Chan, M.; Duff, J.P.; Joyner, B.L.; Lasa, J.J.; Lavonas, E.J.; Levy, A.; Mahgoub, M.; et al. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S469–S523. [Google Scholar] [CrossRef]
- Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part V. Pediatric Basic Life Support. JAMA 1992, 268, 2251–2261. [Google Scholar]
- Santos-Folgar, M.; Fernández-Méndez, F.; Otero-Agra, M.; Abelairas-Gómez, C.; Murciano, M.; Rodríguez-Núñez, A.; Barcala-Furelos, R. Infant Cardiopulmonary Resuscitation Quality While Walking Fast: A Simulation Study. Pediatr. Emerg. Care 2022, 38, e973–e977. [Google Scholar] [CrossRef]
- Perkins, G.D.; Colquhoun, M.; Simons, R. Training Manikins. In ABC of Resuscitation, 5th ed.; BMJ Books: London, UK, 2004; pp. 97–101. [Google Scholar]
- Van de Voorde, P.; Turner, N.M.; Djakow, J.; de Lucas, N.; Martinez-Mejias, A.; Biarent, D.; Bingham, R.; Brissaud, O.; Hoffmann, F.; Johannesdottir, G.B.; et al. European Resuscitation Council Guidelines 2021: Paediatric Life Support. Resuscitation 2021, 161, 327–387. [Google Scholar] [CrossRef]
- Maconochie, I.K.; Bingham, R.; Eich, C.; López-Herce, J.; Rodríguez-Núñez, A.; Rajka, T.; Van de Voorde, P.; Zideman, D.A.; Biarent, D. Paediatric life support section Collaborators European Resuscitation Council Guidelines for Resuscitation 2015: Section 6. Paediatric Life Support. Resuscitation 2015, 95, 223–248. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical Bases of Perceived Exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Nunez, A.R. Ventilation During Pediatric CPR. Curr. Pediatr. Rev. 2013, 9, 109–114. [Google Scholar] [CrossRef]
- Wilkins, L.W. Part 7.1: Adjuncts for Airway Control and Ventilation. Circulation 2005, 112, IV-51–IV-57. [Google Scholar] [CrossRef][Green Version]
- Santos-Folgar, M.; Otero-Agra, M.; Fernández-Méndez, F.; Hermo-Gonzalo, M.T.; Barcala-Furelos, R.; Rodríguez-Núñez, A. Ventilación durante la reanimación cardiopulmonar en el lactante: ¿boca a boca y nariz o con bolsa autoinflable? Un estudio cuasiexperimental. An. Pediatr. 2018, 89, 272–278. [Google Scholar] [CrossRef]
- Weight-for-Length/Height. Available online: https://www.who.int/tools/child-growth-standards/standards/weight-for-length-height (accessed on 3 April 2022).
- Barcala-Furelos, R.; Barcala-Furelos, M.; Cano-Noguera, F.; Otero-Agra, M.; Alonso-Calvete, A.; Martínez-Isasi, S.; Aranda-García, S.; López-García, S.; Rodríguez-Núñez, A. A Comparison between Three Different Techniques Considering Quality Skills, Fatigue and Hand Pain during a Prolonged Infant Resuscitation: A Cross-Over Study with Lifeguards. Children 2022, 9, 910. [Google Scholar] [CrossRef]
- Sousa, A.; Fernandes, R.J.; Rodríguez, N.; Abraldes, J.A. Influence of a 100-M Simulated In-Water Rescue on Cardiopulmonary Parameters. Prehosp. Emerg. Care 2017, 21, 301–308. [Google Scholar] [CrossRef]
- Liu, S.; Vaillancourt, C.; Kasaboski, A.; Taljaard, M. Bystander Fatigue and CPR Quality by Older Bystanders: A Randomized Crossover Trial Comparing Continuous Chest Compressions and 30:2 Compressions to Ventilations. CJEM 2016, 18, 461–468. [Google Scholar] [CrossRef]
- Perkins, G.D.; Lall, R.; Quinn, T.; Deakin, C.D.; Cooke, M.W.; Horton, J.; Lamb, S.E.; Slowther, A.-M.; Woollard, M.; Carson, A.; et al. Mechanical versus Manual Chest Compression for Out-of-Hospital Cardiac Arrest (PARAMEDIC): A Pragmatic, Cluster Randomised Controlled Trial. Lancet 2015, 385, 947–955. [Google Scholar] [CrossRef]
- Martin, P.S.; Kemp, A.M.; Theobald, P.S.; Maguire, S.A.; Jones, M.D. Do Chest Compressions during Simulated Infant CPR Comply with International Recommendations? Arch. Dis. Child. 2013, 98, 576–581. [Google Scholar] [CrossRef]
- Talikowska, M.; Tohira, H.; Finn, J. Cardiopulmonary Resuscitation Quality and Patient Survival Outcome in Cardiac Arrest: A Systematic Review and Meta-Analysis. Resuscitation 2015, 96, 66–77. [Google Scholar] [CrossRef]
- Aufderheide, T.P.; Sigurdsson, G.; Pirrallo, R.G.; Yannopoulos, D.; McKnite, S.; Von, B.; Sparks, C.W.; Conrad, C.J.; Provo, T.A.; Lurie, K.G. Hyperventilation-Induced Hypotension during Cardiopulmonary Resuscitation. Circulation 2004, 109, 1960–1965. [Google Scholar] [CrossRef]
- Aufderheide, T.P.; Pirrallo, R.G.; Yannopoulos, D.; Klein, J.P.; von Briesen, C.; Sparks, C.W.; Deja, K.A.; Kitscha, D.J.; Provo, T.A.; Lurie, K.G. Incomplete Chest Wall Decompression: A Clinical Evaluation of CPR Performance by Trained Laypersons and an Assessment of Alternative Manual Chest Compression-Decompression Techniques. Resuscitation 2006, 71, 341–351. [Google Scholar] [CrossRef]
- Aufderheide, T.P.; Lurie, K.G. Death by Hyperventilation: A Common and Life-Threatening Problem during Cardiopulmonary Resuscitation. Crit. Care Med. 2004, 32, S345–S351. [Google Scholar] [CrossRef] [PubMed]
- Yannopoulos, D.; McKnite, S.; Aufderheide, T.P.; Sigurdsson, G.; Pirrallo, R.G.; Benditt, D.; Lurie, K.G. Effects of Incomplete Chest Wall Decompression during Cardiopulmonary Resuscitation on Coronary and Cerebral Perfusion Pressures in a Porcine Model of Cardiac Arrest. Resuscitation 2005, 64, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Sutton, R.M.; Niles, D.; Nysaether, J.; Stavland, M.; Thomas, M.; Ferry, S.; Bishnoi, R.; Litman, R.; Allen, J.; Srinivasan, V.; et al. Effect of Residual Leaning Force on Intrathoracic Pressure during Mechanical Ventilation in Children. Resuscitation 2010, 81, 857–860. [Google Scholar] [CrossRef]
- Fried, D.A.; Leary, M.; Smith, D.A.; Sutton, R.M.; Niles, D.; Herzberg, D.L.; Becker, L.B.; Abella, B.S. The Prevalence of Chest Compression Leaning during In-Hospital Cardiopulmonary Resuscitation. Resuscitation 2011, 82, 1019. [Google Scholar] [CrossRef]
- Smereka, J.; Iskrzycki, Ł.; Makomaska-Szaroszyk, E.; Bielski, K.; Frass, M.; Robak, O.; Ruetzler, K.; Czekajło, M.; Rodríguez-Núnez, A.; López-Herce, J.; et al. The Effect of Chest Compression Frequency on the Quality of Resuscitation by Lifeguards. A Prospective Randomized Crossover Multicenter Simulation Trial. Cardiol. J. 2020, 26, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Donoghue, A.; Heard, D.; Griffin, R.; Abbadessa, M.K.; Gaines, S.; Je, S.; Hanna, R.; Erbayri, J.; Myers, S.; Niles, D.; et al. Longitudinal Effect of High Frequency Training on CPR Performance during Simulated and Actual Pediatric Cardiac Arrest. Resusc. Plus 2021, 6, 100117. [Google Scholar] [CrossRef]
- Nayak, V.R.; Babu, A.; Unnikrishnan, R.; Babu, A.S.; Krishna, H.M. Influence of Physical Activity of the Rescuer on Chest Compression Duration and Its Effects on Hemodynamics and Fatigue Levels of the Rescuer: A Simulation-Based Study. Indian J. Crit. Care Med. 2020, 24, 409–413. [Google Scholar] [CrossRef]
- Smereka, J.; Szarpak, L.; Rodríguez-Núñez, A.; Ladny, J.R.; Leung, S.; Ruetzler, K. A Randomized Comparison of Three Chest Compression Techniques and Associated Hemodynamic Effect during Infant CPR: A Randomized Manikin Study. Am. J. Emerg. Med. 2017, 35, 1420–1425. [Google Scholar] [CrossRef]
- Mühlbacher, J.; Pröbstl, C.; Granegger, M.; Schiefer, J.; Duma, A.; Hüpfl, M.; Herkner, H.; Röhrich, M.; Schebesta, K. Impact of Infant Positioning on Cardiopulmonary Resuscitation Performance During Simulated Pediatric Cardiac Arrest: A Randomized Crossover Study. Pediatr. Crit. Care Med. 2020, 21, e1076–e1083. [Google Scholar] [CrossRef]
- Barcala-Furelos, R.; Abelairas-Gomez, C.; Aranda-García, S.; Lorenzo-Martínez, M.; Martínez-Isasi, S.; Durán-Álvarez, C.; Palacios-Aguilar, J.; Rodríguez-Núñez, A. Is It Feasible “Scoop and Run While Playing” Resuscitation on a Rescue Water Craft? A Randomized Simulation Study with Lifeguards. Am. J. Emerg. Med. 2020, 38, 618–623. [Google Scholar] [CrossRef]
- Ashton, A.; McCluskey, A.; Gwinnutt, C.L.; Keenan, A.M. Effect of Rescuer Fatigue on Performance of Continuous External Chest Compressions over 3 Min. Resuscitation 2002, 55, 151–155. [Google Scholar] [CrossRef] [PubMed]
- McDonald, C.H.; Heggie, J.; Jones, C.M.; Thorne, C.J.; Hulme, J. Rescuer Fatigue under the 2010 ERC Guidelines, and Its Effect on Cardiopulmonary Resuscitation (CPR) Performance. Emerg. Med. J. 2013, 30, 623–627. [Google Scholar] [CrossRef]
- Santos-Folgar, M.; Otero-Agra, M.; Prada-Pérez, A.; Barcala-Furelos, R.; Rodríguez-Núñez, A.; Fernández-Méndez, F. Fatigue During Infant Cardiopulmonary Resuscitation: Is It Really a Problem for Quality Performance? Pediatr. Emerg. Care 2021, 37, e278–e279. [Google Scholar] [CrossRef]
- Jung, W.J.; Hwang, S.O.; Kim, H.I.; Cha, Y.S.; Kim, O.H.; Kim, H.; Lee, K.H.; Cha, K.-C. ‘Knocking-fingers’ chest compression technique in infant cardiac arrest: Single-rescuer manikin study. Eur. J. Emerg. Med. 2019, 26, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Jeon, W.; Kim, J.; Ko, Y.; Lee, J. New Chest Compression Method in Infant Resuscitation: Cross Thumb Technique. PLoS ONE 2022, 17, e0271636. [Google Scholar] [CrossRef] [PubMed]

| Variables | Standard CPR (S-CPR) | Walking CPR (W-CPR) | Running CPR (R-CPR) | Significance | |||
|---|---|---|---|---|---|---|---|
| Me | IQR | Me | IQR | Me | IQR | ||
| CC: Chest compressions | |||||||
| Number of CC | 180 | (169–190) | 199 | (170–212) | 191 | (174–243) | NS † |
| Mean depth (mm) | 42 | (41–43) | 41 | (37–43) | 42 | (41–43) | NS † |
| Mean rate (CC/min) | 129 | (121–142) | 130 | (119–154) | 133 | (115–176) | NS † |
| CC with adequate depth (%) | 99 | (98–100) | 96 | (64–99) | 95 | (77–96) | NS † |
| CC with adequate rate (%) | 1 | (0–46) | 8 | (2–29) | 7 | (1–37) | NS † |
| CC with adequate release (%) | 95 | (55–98) | 89 | (67–97) | 63 | (27–84) | S vs. R = 0.032 (0.50) † W vs. R = 0.018 (0.54) † |
| CC with adequate hand-position (%) | 100 | (93–100) | 92 | (68–99) | 85 | (63–91) | S vs. R = 0.005 (0.62) † |
| V: Ventilations | |||||||
| Mean pause time for V (s) | 5 | (5–7) | 4 | (4–5) | 4 | (4–5) | S vs. R = 0.024 (0.52) † |
| Number of effective V | 15 | (15–16) | 16 | (13–17) | 15 | (13–19) | NS † |
| Number of V with adequate volume | 7 | (4–10) | 7 | (5–10) | 7 | (3–13) | NS * |
| Number of V with excessive volume | 6 | (0–10) | 3 | (1–7) | 3 | (1–7) | NS † |
| Number of V with insufficient volume | 0 | (0–4) | 5 | (1–7) | 5 | (4–7) | NS † |
| Mean volume (mL) | 53 | (45–63) | 44 | (38–58) | 44 | (41–60) | S vs. R = 0.010 (0.58) † S vs. W = 0.010 (0.58) † |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos-Folgar, M.; Rodriguez-Nunez, A.; Barcala-Furelos, R.; Otero-Agra, M.; Martínez-Isasi, S.; Fernández-Méndez, F. Trained Lifeguards Performing Pediatric Cardiopulmonary Resuscitation While Running: A Pilot Simulation Study. Children 2023, 10, 1348. https://doi.org/10.3390/children10081348
Santos-Folgar M, Rodriguez-Nunez A, Barcala-Furelos R, Otero-Agra M, Martínez-Isasi S, Fernández-Méndez F. Trained Lifeguards Performing Pediatric Cardiopulmonary Resuscitation While Running: A Pilot Simulation Study. Children. 2023; 10(8):1348. https://doi.org/10.3390/children10081348
Chicago/Turabian StyleSantos-Folgar, Myriam, Antonio Rodriguez-Nunez, Roberto Barcala-Furelos, Martín Otero-Agra, Santiago Martínez-Isasi, and Felipe Fernández-Méndez. 2023. "Trained Lifeguards Performing Pediatric Cardiopulmonary Resuscitation While Running: A Pilot Simulation Study" Children 10, no. 8: 1348. https://doi.org/10.3390/children10081348
APA StyleSantos-Folgar, M., Rodriguez-Nunez, A., Barcala-Furelos, R., Otero-Agra, M., Martínez-Isasi, S., & Fernández-Méndez, F. (2023). Trained Lifeguards Performing Pediatric Cardiopulmonary Resuscitation While Running: A Pilot Simulation Study. Children, 10(8), 1348. https://doi.org/10.3390/children10081348






