Our Experiences with Asparaginase Activity Measurements in Children with Lymphoblastic Diseases
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
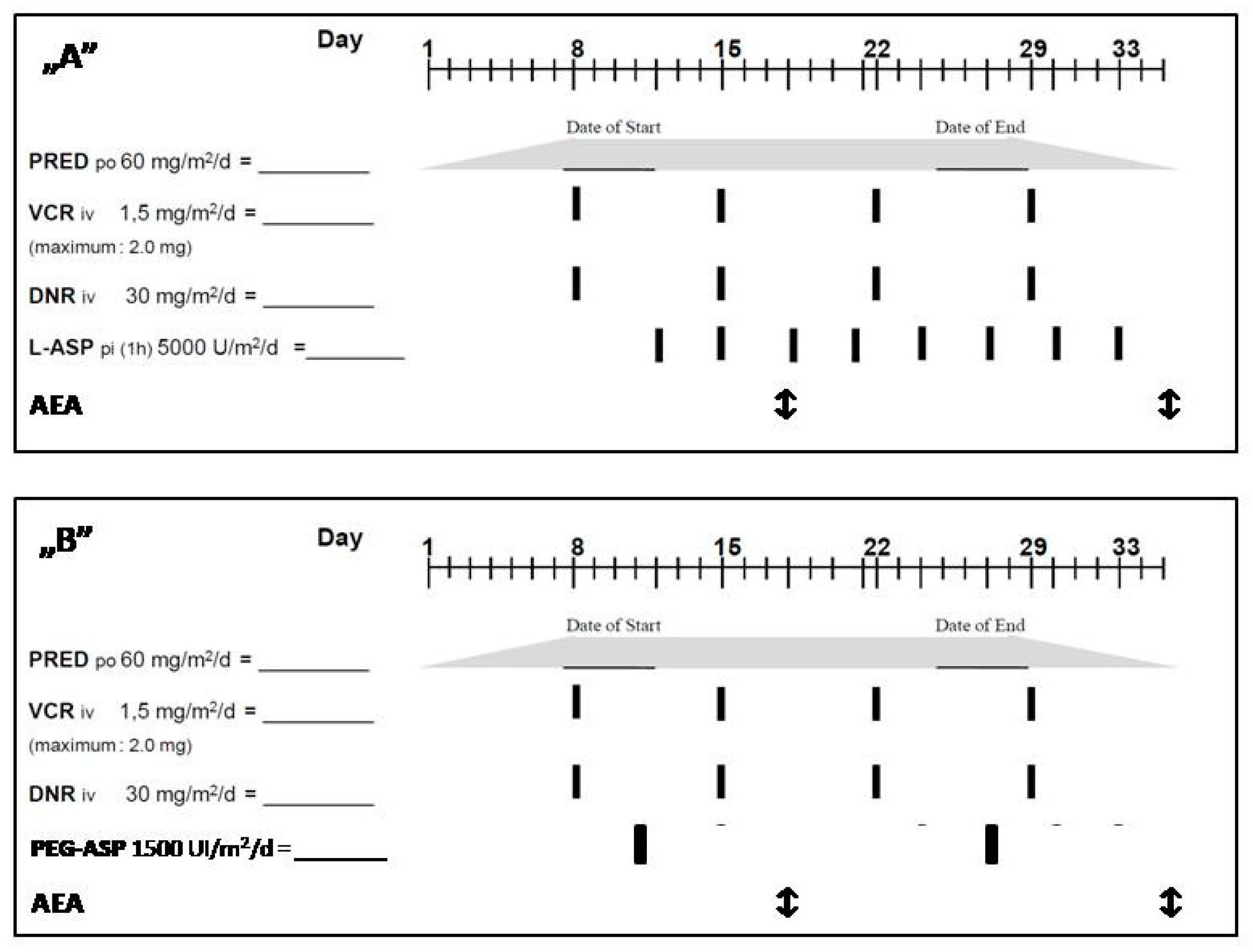
2.2. Asparaginase Treatment
2.3. Asparaginse Enzyme Activity Measurement
3. Results
3.1. Patient Characteristics
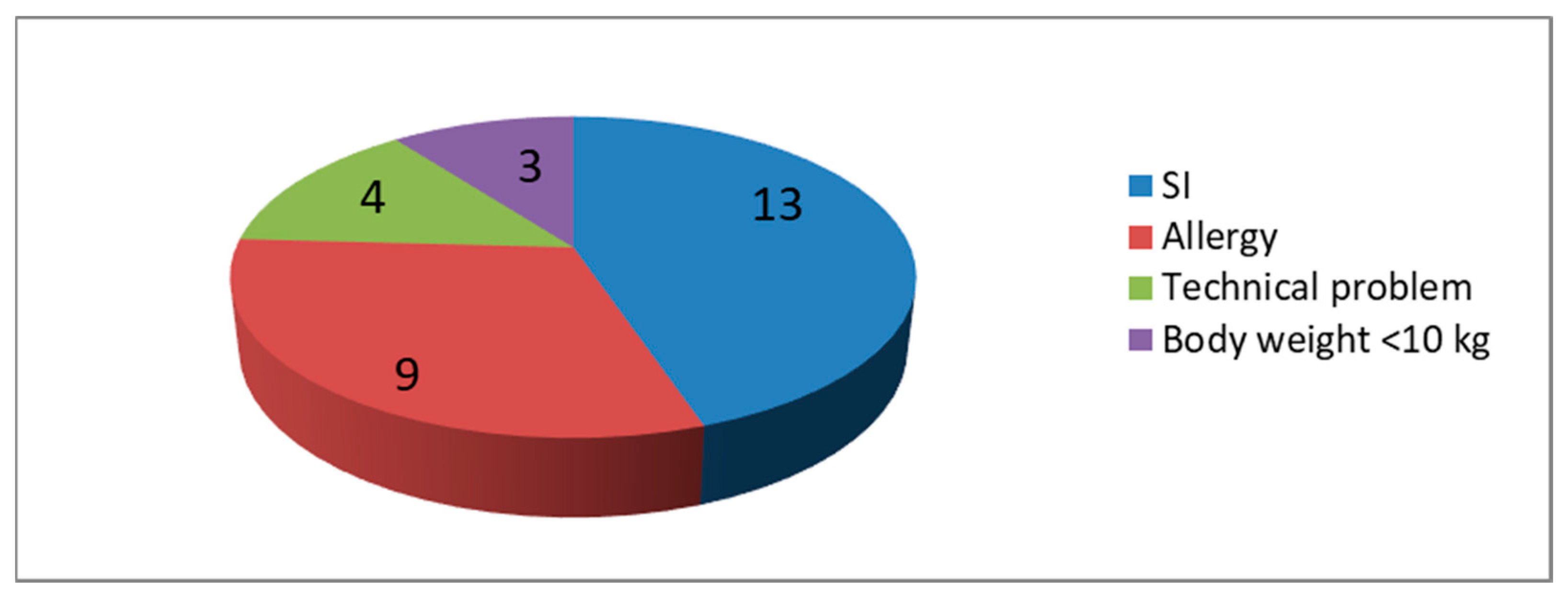
3.2. ASPnase Monitoring
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pieters, R.; de Groot-Kruseman, H.; van der Velden, V.; Fiocco, M.; Berg, H.V.D.; de Bont, E.; Egeler, R.M.; Hoogerbrugge, P.; Kaspers, G.; Van der Schoot, E.; et al. Successful Therapy Reduction and Intensification for Childhood Acute Lymphoblastic Leukemia Based on Minimal Residual Disease Monitoring: Study ALL10 from the Dutch Childhood Oncology Group. J. Clin. Oncol. 2016, 34, 2591–2601. [Google Scholar] [CrossRef]
- Reedijk, A.M.J.; Coebergh, J.W.W.; de Groot-Kruseman, H.A.; van der Sluis, I.M.; Kremer, L.C.; Karim-Kos, H.E.; Pieters, R. Progress against childhood and adolescent acute lymphoblastic leukaemia in the Netherlands, 1990–2015. Leukemia 2021, 35, 1001–1011. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, B.; Hermiston, M.L. Lymphoblastic lymphoma in children and adolescents: Review of current challenges and future opportunities. Br. J. Haematol. 2019, 185, 1158–1170. [Google Scholar] [CrossRef] [PubMed]
- Müller, H.J.; Boos, J. Use of L-asparaginase in childhood ALL. Crit. Rev. Oncol. Hematol. 1998, 28, 97–113. [Google Scholar] [CrossRef]
- Müller, H.-J.; Beier, R.; Löning, L.; Blütters-Sawatzki, R.; Dörffel, W.; Maass, E.; Müller-Weihrich, S.; Scheel-Walter, H.-G.; Scherer, F.; Stahnke, K.; et al. Pharmacokinetics of native Escherichia coli asparaginase (Asparaginase medac) and hypersensitivity reactions in ALL-BFM 95 reinduction treatment. Br. J. Haematol. 2001, 114, 794–799. [Google Scholar] [CrossRef] [PubMed]
- Boos, J.; Werber, G.; Ahlke, E.; Schulze-Westhoff, P.; Nowak-Göttl, U.; Würthwein, G.; Verspohl, E.; Ritter, J.; Jürgens, H. Monitoring of asparaginase activity and asparagine levels in children on different asparaginase preparations. Eur. J. Cancer 1996, 32, 1544–1550. [Google Scholar] [CrossRef]
- Avramis, V.I.; Panosyan, E.H. Pharmacokinetic/pharmacodynamic relationships of asparaginase formulations: The past, the present and recommendations for the future. Clin. Pharmacokinet. 2005, 44, 367–393. [Google Scholar] [CrossRef]
- Michalska, K.; Jaskolski, M. Structural aspects of L-asparaginases, their friends and relations. Acta Biochim. Pol. 2006, 53, 627–640. [Google Scholar] [CrossRef]
- van den Berg, H. Asparaginase revisited. Leuk. Lymphoma 2011, 52, 168–178. [Google Scholar] [CrossRef]
- Asselin, B.L. The three asparaginases. Comparative pharmacology and optimal use in childhood leukemia. Adv. Exp. Med. Biol. 1999, 457, 621–629. [Google Scholar]
- Asselin, B.L.; Whitin, J.C.; Coppola, D.J.; Rupp, I.P.; Sallan, E.S.; Cohen, H.J. Comparative pharmacokinetic studies of three asparaginase preparations. J. Clin. Oncol. 1993, 11, 1780–1786. [Google Scholar] [CrossRef]
- Pieters, R.; Hunger, S.P.; Boos, J.; Rizzari, C.; Silverman, L.; Baruchel, A.; Goekbuget, N.; Schrappe, M.; Pui, C.-H. L-asparaginase treatment in acute lymphoblastic leukemia: A focus on Erwinia asparaginase. Cancer 2011, 117, 238–249. [Google Scholar] [CrossRef] [PubMed]
- van der Sluis, I.M.; Vrooman, L.M.; Pieters, R.; Baruchel, A.; Escherich, G.; Goulden, N.; Mondelaers, V.; Sanchez de Toledo, J.; Rizzari, C.; Silverman, L.B.; et al. Consensus expert recommendations for identification and management of asparaginase hypersensitivity and silent inactivation. Haematologica 2016, 101, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Lanvers, C.; Pinheiro, J.P.V.; Hempel, G.; Wuerthwein, G.; Boos, J. Analytical validation of a microplate reader-based method for the therapeutic drug monitoring of L-asparaginase in human serum. Anal. Biochem. 2002, 309, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Tong, W.H.; Pieters, R.; Kaspers, G.J.L.; Loo, D.M.W.M.T.; Bierings, M.B.; Bos, C.V.D.; Kollen, W.J.W.; Hop, W.C.J.; Lanvers-Kaminsky, C.; Relling, M.V.; et al. A prospective study on drug monitoring of PEGasparaginase and Erwinia asparaginase and asparaginase antibodies in pediatric acute lymphoblastic leukemia. Blood 2014, 123, 2026–2033. [Google Scholar] [CrossRef]
- Panosyan, E.H.; Seibel, N.L.; Martin-Aragon, S.; Gaynon, P.S.; Avramis, I.A.; Sather, H.; Franklin, J.; Nachman, J.; Ettinger, L.J.; La, M.; et al. Asparaginase antibody and asparaginase activity in children with higher-risk acute lymphoblastic leukemia: Children’s Cancer Group Study CCG-1961. J. Pediatr. Hematol. Oncol. 2004, 26, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Avramis, V.I.; Martin-Aragon, S.; Avramis, E.V.; Asselin, B.L. Pharmacoanalytical assays of Erwinia asparaginase (erwinase) and pharmacokinetic results in high-risk acute lymphoblastic leukemia (HR ALL) patients: Simulations of erwinase population PK-PD models. Anticancer. Res. 2007, 27, 2561–2572. [Google Scholar]
- Pinheiro, J.P.V.; Ahlke, E.; Nowak-Göttl, U.; Hempel, G.; Müller, H.J.; Lümkemann, K.; Schrappe, M.; Rath, B.; Fleischhack, G.; Mann, G.; et al. Pharmacokinetic dose adjustment of Erwinia asparaginase in protocol II of the paediatric ALL/NHL-BFM treatment protocols. Br. J. Haematol. 1999, 104, 313–320. [Google Scholar] [CrossRef]
- Vrooman, L.M.; Stevenson, K.E.; Supko, J.G.; O’Brien, J.; Dahlberg, S.E.; Asselin, B.L.; Athale, U.H.; Clavell, L.A.; Kelly, K.M.; Kutok, J.L.; et al. Postinduction dexamethasone and individualized dosing of Escherichia Coli L-asparaginase each improve outcome of children and adolescents with newly diagnosed acute lymphoblastic leukemia: Results from a randomized study--Dana-Farber Cancer Institute ALL Consortium Protocol 00-01. J. Clin. Oncol. 2013, 31, 1202–1210. [Google Scholar] [CrossRef]
- Wetzler, M.; Sanford, B.L.; Kurtzberg, J.; DeOliveira, D.; Frankel, S.R.; Powell, B.L.; Kolitz, J.E.; Bloomfield, C.D.; Larson, R.A. Effective asparagine depletion with pegylated asparaginase results in improved outcomes in adult acute lymphoblastic leukemia: Cancer and Leukemia Group B Study 9511. Blood 2007, 109, 4164–4167. [Google Scholar] [CrossRef]
- Gupta, S.; Wang, C.; Raetz, E.A.; Schore, R.; Salzer, W.L.; Larsen, E.C.; Maloney, K.W.; Mattano, L.A., Jr.; Carroll, W.L.; Winick, N.J.; et al. Impact of Asparaginase Discontinuation on Outcome in Childhood Acute Lymphoblastic Leukemia: A Report from the Children’s Oncology Group. J. Clin. Oncol. 2020, 38, 1897–1905. [Google Scholar] [CrossRef] [PubMed]
- Højfeldt, S.G.; Grell, K.; Abrahamsson, J.; Lund, B.; Vettenranta, K.; Jónsson, Ó.G.; Frandsen, T.L.; Wolthers, B.O.; Marquart, H.V.H.; Vaitkeviciene, G.; et al. Relapse risk following truncation of pegylated asparaginase in childhood acute lymphoblastic leukemia. Blood 2021, 137, 2373–2382. [Google Scholar] [CrossRef] [PubMed]
- Batchelor, H.K.; Marriott, J.F. Paediatric pharmacokinetics: Key considerations. Br. J. Clin. Pharmacol. 2015, 79, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, J.P.; Murray, G.; Risler, L.; Chien, J.Y.; Dev, R.; Slattery, J.T. Age-dependent tetrahydrothiophenium ion formation in young children and adults receiving high-dose busulfan. Cancer Res. 1997, 57, 5509–5516. [Google Scholar] [PubMed]
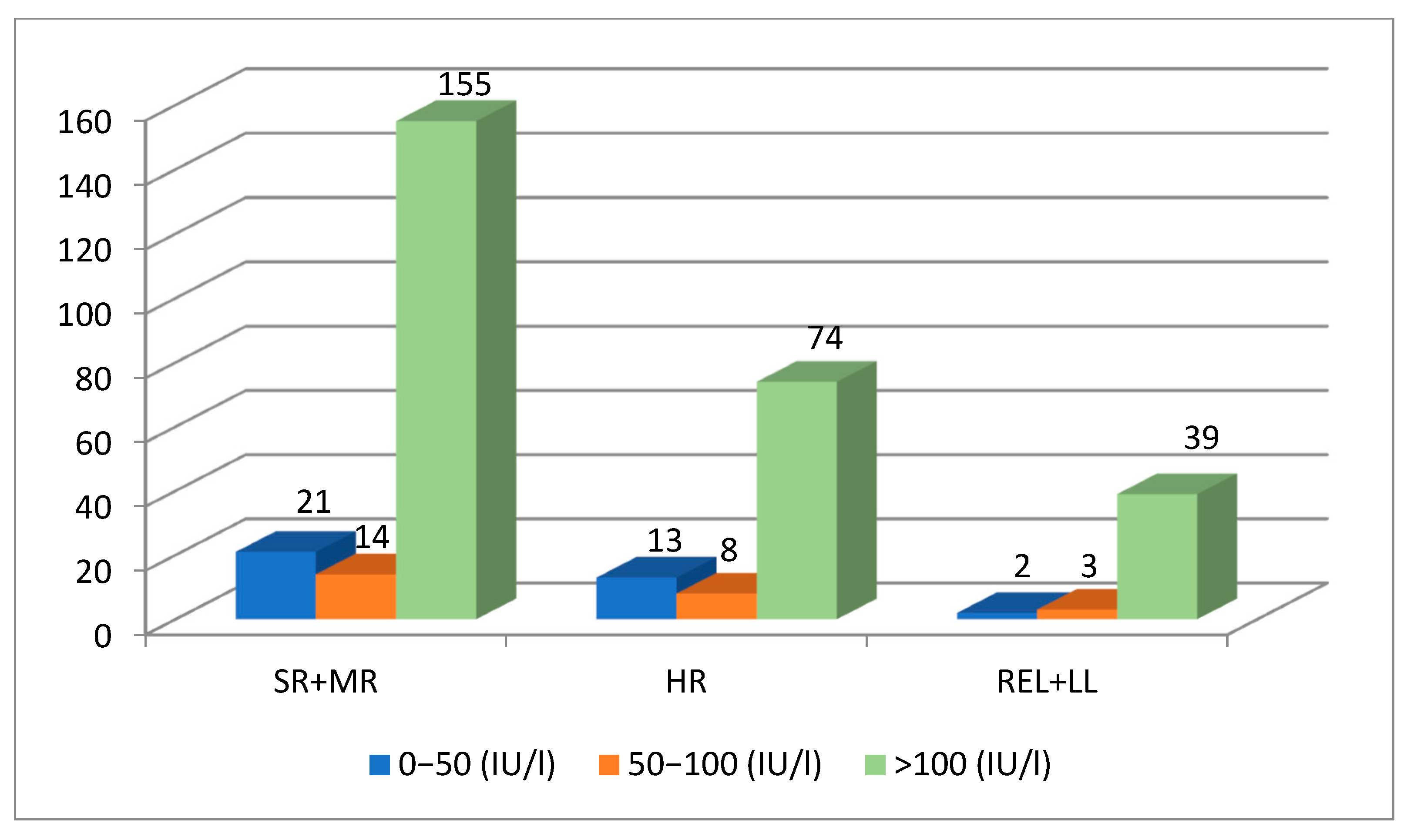
| SR + MR | HR | REL + LBL | ∑ | |
|---|---|---|---|---|
| No. of patients | 70 | 21 | 15 | 106 |
| Male/female | 1.59:1 | 1.33:1 | 2:1 | 1.58:1 |
| Median age (range) | 7.2 years (13 mo–17.9 y) | 6.9 years (1.5 y–16.9 y) | 13.2 years (4.7 y–17.5 y) | 8.0 years (13 mo–17.9 y) |
| No. of samples | 190 | 95 | 44 | 329 |
| Samples (no.)/patient mean | 1–4 2.7 | 1–7 4.5 | 1–5 2.9 | 1–7 3.4 |
| Mean AEA (IU/L) | 281 | 345 | 385 | 337 |
| 0–50 (IU/L) | 21 | 13 | 2 | 36 |
| 50–100 (IU/L) | 14 | 8 | 3 | 25 |
| >100 (IU/L) | 155 | 74 | 39 | 268 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müller, J.; Egyed, P.; Erdelyi, D.; Kovacs, K.; Mudra, K.; Szabo, S.; Egyed, B.; Gabor, K. Our Experiences with Asparaginase Activity Measurements in Children with Lymphoblastic Diseases. Children 2023, 10, 1160. https://doi.org/10.3390/children10071160
Müller J, Egyed P, Erdelyi D, Kovacs K, Mudra K, Szabo S, Egyed B, Gabor K. Our Experiences with Asparaginase Activity Measurements in Children with Lymphoblastic Diseases. Children. 2023; 10(7):1160. https://doi.org/10.3390/children10071160
Chicago/Turabian StyleMüller, Judit, Petra Egyed, Daniel Erdelyi, Krisztian Kovacs, Katalin Mudra, Sandor Szabo, Balint Egyed, and Kovacs Gabor. 2023. "Our Experiences with Asparaginase Activity Measurements in Children with Lymphoblastic Diseases" Children 10, no. 7: 1160. https://doi.org/10.3390/children10071160
APA StyleMüller, J., Egyed, P., Erdelyi, D., Kovacs, K., Mudra, K., Szabo, S., Egyed, B., & Gabor, K. (2023). Our Experiences with Asparaginase Activity Measurements in Children with Lymphoblastic Diseases. Children, 10(7), 1160. https://doi.org/10.3390/children10071160





