Socio-Emotional Experiences and Wellbeing of Deaf and Hard of Hearing Children and Their Parents before and during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Recruitment, and Follow-Up: Overview of the VicCHILD Study
2.2. Data Analysis
3. Results
3.1. Demographics
3.2. COVID-19 Exposure
3.3. Daily Behaviors
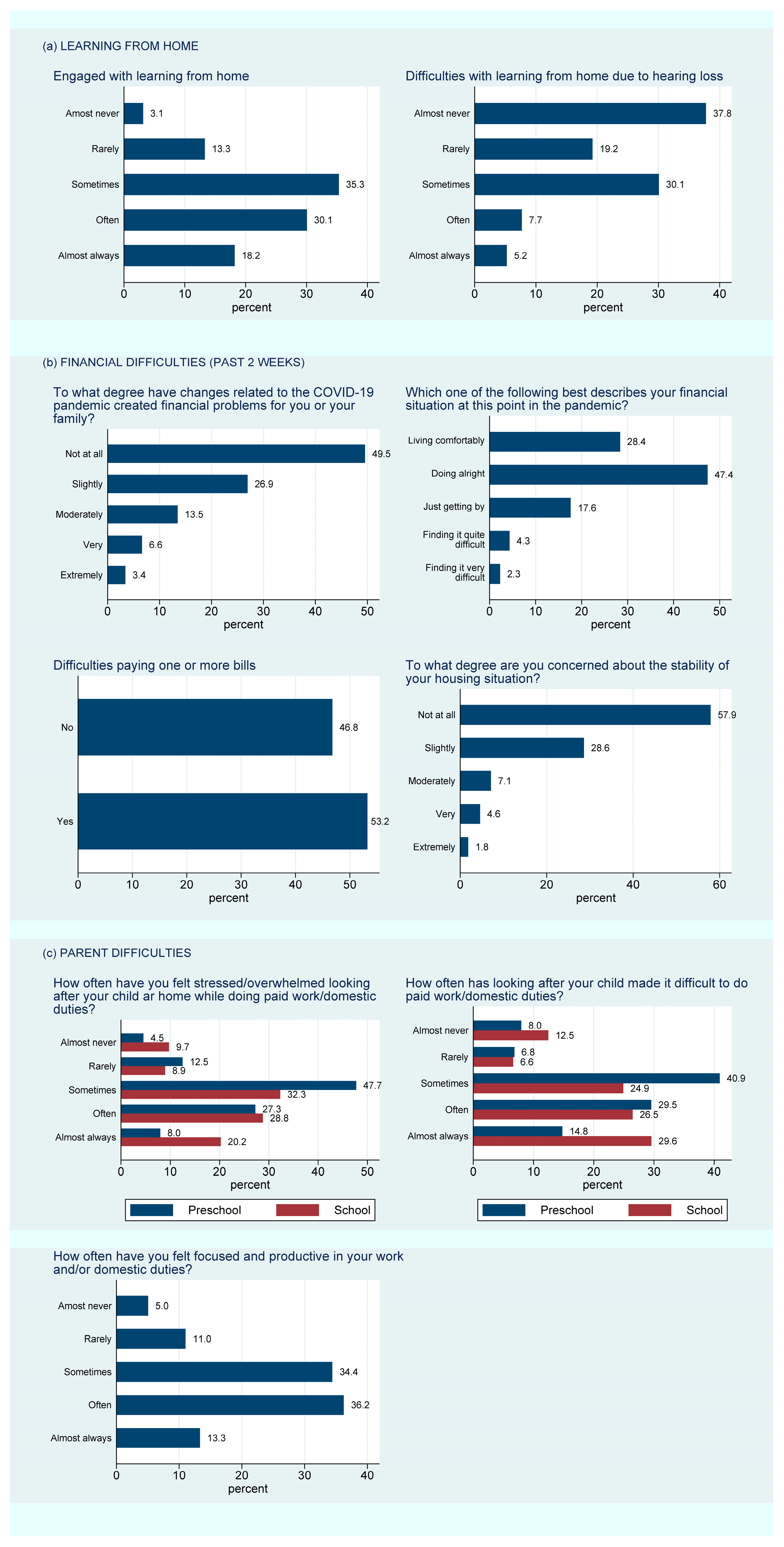
3.3.1. Changes to Child Learning or Care Arrangements
3.3.2. Changes to Parent Employment
3.3.3. Financial Problems
3.3.4. Daily Activities
3.4. Changes to Family Life
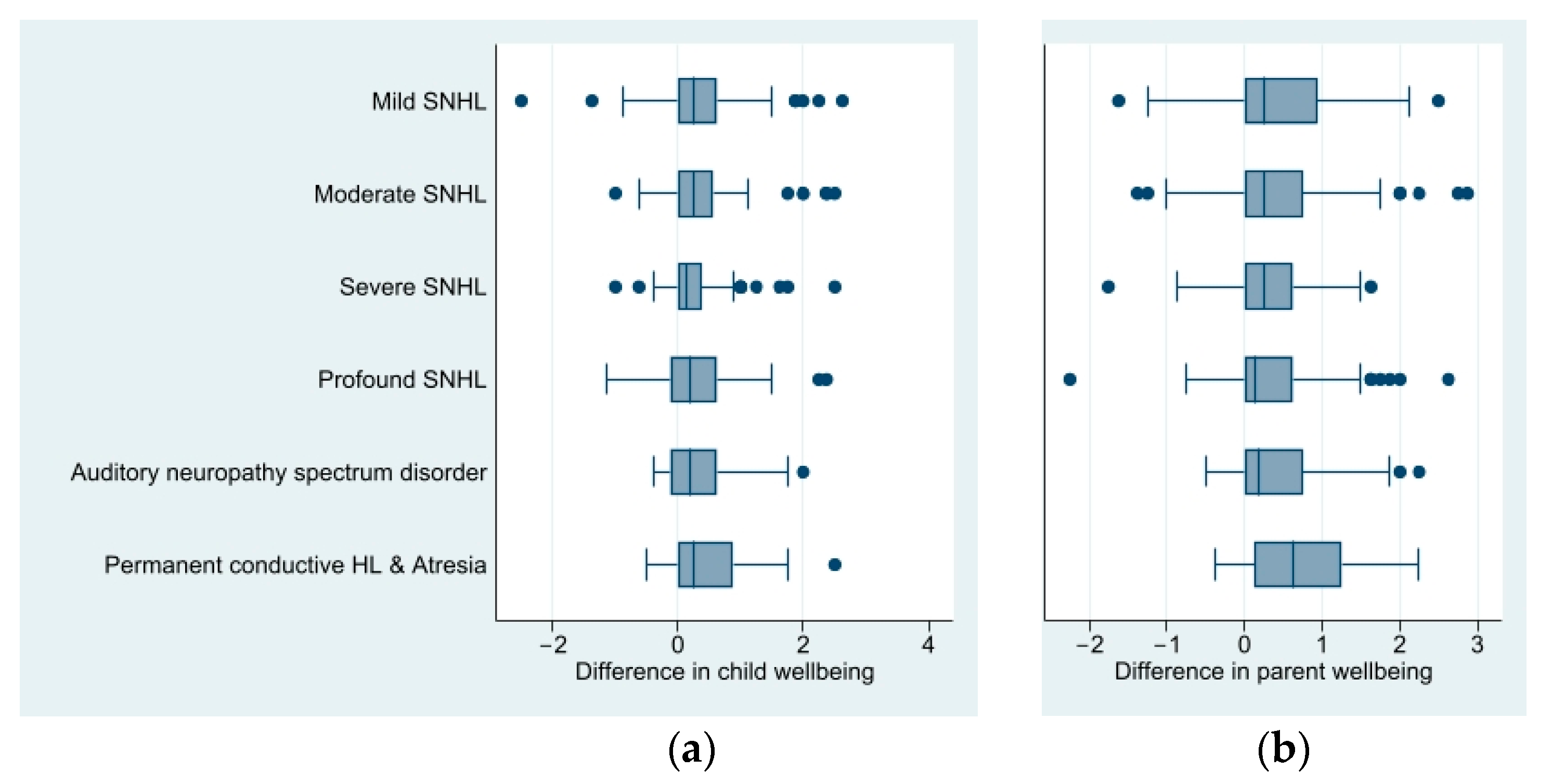
3.5. Socio-Emotional Wellbeing of DHH Children and Their Parents
4. Discussion
4.1. Principal Findings
4.2. Strengths and Limitations
4.3. Interpretation in Light of Other Studies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Long, G.C.; Umat, C.; Din, N.C. Socio-emotional development of children with cochlear implant: A systematic review. Malays. J. Med. Sci. MJMS 2021, 28, 10. [Google Scholar]
- Harris, L.G. Social-Emotional Development in Children with Hearing Loss. Master’s Thesis, University Press of Kentucky, Lexington, KY, USA, 2014. [Google Scholar]
- Wang, Y.; Su, Y.; Fang, P.; Zhou, Q. Facial expression recognition: Can preschoolers with cochlear implants and hearing aids catch it? Res. Dev. Disabil. 2011, 32, 2583–2588. [Google Scholar] [CrossRef]
- Hintermair, M. Socio-emotional problems among hearing-impaired children—Initial results of the German version of the Strengths and Difficulties Questionnaire (SDQ-D). Z. Fur Kinder-Jugendpsychiatrie Psychother. 2006, 34, 49–61. [Google Scholar] [CrossRef]
- Van Eldik, T.; Treffers, P.D.A.; Veerman, J.W.; Verhulst, F.C. Mental health problems of deaf Dutch children as indicated by parents’ responses to the child behavior checklist. Am. Ann. Deaf. 2004, 148, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Van Gent, T.; Goedhart, A.W.; Hindley, P.A.; Treffers, P.D. A Prevalence and correlates of psychopathology in a sample of deaf adolescents. J. Child Psychol. Psychiatry 2007, 48, 950–958. [Google Scholar] [CrossRef]
- Fellinger, J.; Holzinger, D.; Sattel, H.; Laucht, M. Mental health and quality of life in deaf pupils. Eur. Child Adolesc. Psychiatry 2008, 17, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Fellinger, J.; Holzinger, D.; Sattel, H.; Laucht, M.; Goldberg, D. Correlates of mental health disorders among children with hearing impairments. Dev. Med. Child Neurol. 2009, 51, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Dammeyer, J. Psychosocial development in a Danish population of children with cochlear implants and deaf and hard-of-hearing children. J. Deaf. Stud. Deaf. Educ. 2010, 15, 50–58. [Google Scholar] [CrossRef]
- Hindley, P.; Kitson, N. Mental health and deafness. In Child and Adolescent Psychiatry; Whurr Publishers: London, UK, 2000. [Google Scholar]
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. 2021. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 11 November 2020).
- McManus, M.A.; Ball, E. COVID-19 should be considered an Adverse Childhood Experience (ACE). J. Community Saf. Well-Being 2020, 5, 164–167. [Google Scholar] [CrossRef]
- Prime Minister of Australia. Border Restrictions. Available online: https://www.pm.gov.au/media/border-restrictions (accessed on 10 August 2020).
- Australian Government, Department of Health. Coronavirus (COVID-19) Case Numbers and Statistics. Available online: https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-case-numbers-and-statistics (accessed on 18 August 2021).
- Department of Health and Human Services. Victoria’s Restriction Levels. Available online: https://www.dhhs.vic.gov.au/victorias-restriction-levels-covid-19 (accessed on 15 November 2020).
- Australian Institute of Health and Welfare. The First Year of COVID-19 in Australia: Direct and Indirect Health Effects; Australian Institute of Health and Welfare: Canberra, Australia, 2021. [Google Scholar]
- Li, S.H.; Beames, J.R.; Newby, J.M.; Maston, K.; Christensen, H.; Werner-Seidler, A. The impact of COVID-19 on the lives and mental health of Australian adolescents. J. Eur. Child Adolesc. Psychiatry 2021, 31, 1465–1477. [Google Scholar] [CrossRef]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-analysis. JAMA Pediatr. 2021, 175, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Hoefnagels, J.W.; Schoen, A.B.; van der Laan, S.E.; Rodijk, L.H.; van der Ent, C.K.; van de Putte, E.M.; Dalmeijer, G.W.; Nijhof, S.L. The Impact of the COVID-19 Outbreak on Mental Wellbeing in Children with a Chronic Condition Compared to Healthy Peers. Int. J. Environ. Res. Public Health 2022, 19, 2953. [Google Scholar] [CrossRef] [PubMed]
- Alqraini, F.M.; Alasim, K.N. Distance Education for d/Deaf and Hard of Hearing Students during the COVID-19 Pandemic in Saudi Arabia: Challenges and Support. Res. Dev. Disabil. 2021, 117, 104059. [Google Scholar] [CrossRef] [PubMed]
- Patel, K. Mental health implications of COVID-19 on children with disabilities. Asian J. Psychiatry 2020, 54, 102273. [Google Scholar] [CrossRef]
- Schafer, E.C.; Dunn, A.; Lavi, A. Educational challenges during the pandemic for students who have hearing loss. Lang. Speech Hear. Serv. Sch. 2021, 52, 889–898. [Google Scholar] [CrossRef]
- Fellinger, J.; Holzinger, D.; Pollard, R. Mental health of deaf people. Lancet 2012, 379, 1037–1044. [Google Scholar] [CrossRef]
- Sung, V.; Smith, L.; Poulakis, Z.; Burt, R.A.; Carew, P.; Tobin, S.; Wake, M. Data Resource Profile: The Victorian Childhood Hearing Impairment Longitudinal Databank (VicCHILD). Int. J. Epidemiol. 2019, 48, 1409–1410h. [Google Scholar] [CrossRef]
- Nikolaidis, A.; Paksarian, D.; Alexander, L.; Derosa, J.; Dunn, J.; Nielson, D.M.; Droney, I.; Kang, M.; Douka, I.; Bromet, E. The Coronavirus Health and Impact Survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Sci. Rep. 2021, 11, 8139. [Google Scholar] [CrossRef]
- Sciberras, E.; Patel, P.; Stokes, M.A.; Coghill, D.; Middeldorp, C.M.; Bellgrove, M.A.; Becker, S.P.; Efron, D.; Stringaris, A.; Faraone, S.V. Physical health, media use, and mental health in children and adolescents with ADHD during the COVID-19 pandemic in Australia. J. Atten. Disord. 2022, 26, 549–562. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA). Available online: https://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa2011? (accessed on 21 May 2018).
- Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS): Volume 5 Remoteness Structure (1270.0.55.005). Available online: https://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/A277D01B6AF25F64CA257B03000D7EED/$File/1270055005_july%202011.pdf (accessed on 30 January 2023).
- Mardinli, A.; Weerasuriya, R.; Gillespie, A.; Smith, L.; Sung, V. Accessing hearing-health services for deaf and hard-of—Hearing children during the COVID-19 pandemic: Parent and child perspectives. Aust. J. Soc. Issues 2022, 58, 232–258. [Google Scholar] [CrossRef]
- O’Connor, M.; Greenwood, C.J.; Letcher, P.; Giallo, R.; Priest, N.; Goldfeld, S.; Hope, S.; Edwards, B.; Olsson, C.A. Inequalities in the distribution of COVID-19-related financial difficulties for Australian families with young children. Child Care Health Dev. 2022, 48, 1040–1051. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Xiao, Y.; Liu, Y.; Li, Q.; Shan, C.; Chang, S.; Jen, P.H.-S. Mental Health and Psychological Impact on Students with or without Hearing Loss during the Recurrence of the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 2021, 18, 1421. [Google Scholar] [CrossRef] [PubMed]
- Ariapooran, S.; Khezeli, M. Symptoms of anxiety disorders in Iranian adolescents with hearing loss during the COVID-19 pandemic. BMC Psychiatry 2021, 21, 114. [Google Scholar]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef]
- Santa-Cruz, C.; Espinoza, V.; Donoso, J.; Rosas, R.; Badillo, D. How did the pandemic affect the socio-emotional well-being of Chilean schoolchildren? A longitudinal study. Sch. Psychol. 2022, 37, 85–96. [Google Scholar] [CrossRef]
- Mete Yesil, A.; Sencan, B.; Omercioglu, E.; Ozmert, E.N. The Impact of the COVID-19 Pandemic on Children With Special Needs: A Descriptive Study. Clin. Pediatr. 2021, 61, 141–149. [Google Scholar] [CrossRef]

| Measure | Responders n = 497 (62%) | Non-Responders n = 309 (38%) |
|---|---|---|
| Demographics: parent | ||
| Sex: female—n (%) | 413 (93%) | - |
| Relationship to child: mother—n (%) | 414 (94%) | - |
| Partner living with parent—n (%) | 399 (90%) | - |
| Located within Australia—n (%) | 489 (98%) | - |
| Maternal education—n (%) a | ||
| High school not completed | 44 (11%) | 46 (19%) |
| High school completed | 126 (31%) | 86 (36%) |
| Tertiary qualification completed | 240 (59%) | 109 (45%) |
| Demographics: child | ||
| Age, years—mean (SD) | 6.5 (4.0) | 6.9 (3.7) |
| Sex: female—n (%) | 215 (43%) | 148 (48%) |
| Demographics: family | ||
| SEIFA disadvantage index—mean (SD) b | 1013.5 (65.1) | 1006 (68.5) |
| Remoteness area: regional or remote—n (%) c | 96 (19%) | 55 (18%) |
| Language spoken at home: English—n (%) | 363 (73%) | 214 (75%) |
| Hearing loss information of child | ||
| Hearing loss laterality—n (%) | ||
| Unilateral | 143 (29%) | 84 (27%) |
| Bilateral | 320 (64%) | 204 (66%) |
| Unknown | 34 (7%) | 21 (7%) |
| Hearing loss type—n (%) d | ||
| Sensorineural | 339 (68%) | 215 (70%) |
| Mixed | 49 (10%) | 30 (10%) |
| Auditory neuropathy sensory disorder | 39 (8%) | 27 (9%) |
| Atresia | 19 (4%) | 4 (1%) |
| Permanent conductive | 14 (3%) | 11 (4%) |
| Unknown | 37 (7%) | 22 (7%) |
| Degree of hearing loss—n (%) | ||
| Mild | 117 (24%) | 74 (24%) |
| Moderate | 145 (29%) | 83 (27%) |
| Severe | 84 (17%) | 55 (18%) |
| Profound | 109 (22%) | 76 (25%) |
| Missing/ANSD (not recorded) | 42 (8%) | 21 (7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gillespie, A.N.; Smith, L.; Shepherd, D.A.; Xu, J.; Khanal, R.; Sung, V. Socio-Emotional Experiences and Wellbeing of Deaf and Hard of Hearing Children and Their Parents before and during the COVID-19 Pandemic. Children 2023, 10, 1147. https://doi.org/10.3390/children10071147
Gillespie AN, Smith L, Shepherd DA, Xu J, Khanal R, Sung V. Socio-Emotional Experiences and Wellbeing of Deaf and Hard of Hearing Children and Their Parents before and during the COVID-19 Pandemic. Children. 2023; 10(7):1147. https://doi.org/10.3390/children10071147
Chicago/Turabian StyleGillespie, Alanna N., Libby Smith, Daisy A. Shepherd, Jessica Xu, Rija Khanal, and Valerie Sung. 2023. "Socio-Emotional Experiences and Wellbeing of Deaf and Hard of Hearing Children and Their Parents before and during the COVID-19 Pandemic" Children 10, no. 7: 1147. https://doi.org/10.3390/children10071147
APA StyleGillespie, A. N., Smith, L., Shepherd, D. A., Xu, J., Khanal, R., & Sung, V. (2023). Socio-Emotional Experiences and Wellbeing of Deaf and Hard of Hearing Children and Their Parents before and during the COVID-19 Pandemic. Children, 10(7), 1147. https://doi.org/10.3390/children10071147





