SARS-CoV-2 Infection during Pregnancy Followed by Thalamic Neonatal Stroke—Case Report
Abstract
1. Introduction
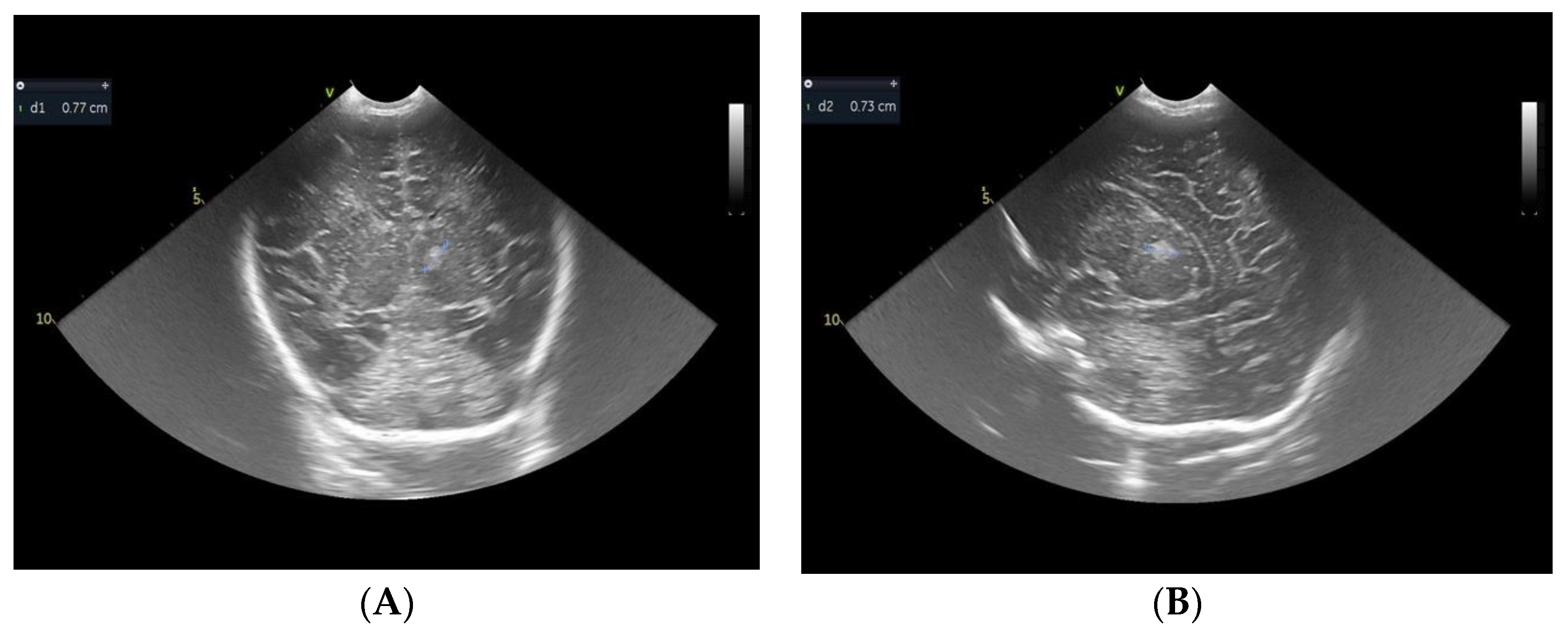
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raju, T.N.; Nelson, K.B.; Ferriero, D.; Lynch, J.K.; NICHD-NINDS Perinatal Stroke Workshop Participants. Ischemic perinatal stroke: Summary of a workshop sponsored by the National Institute of Child Health and Human Development and the National Institute of Neurological Disorders and Stroke. Pediatrics 2007, 120, 609–616. [Google Scholar] [CrossRef][Green Version]
- Martin, R.J.; Walsh, M.C.F.A. Fanaroff and Martin’s Neonatal-Perinatal Medicine, Diseases of Fetus and Infant, 10th ed.; Intracranial Hemorrhage and Vascular lesions in the Neonate; Elsevier Saunders: Philadelphia, PA, USA, 2015; Volume 2, pp. 886–903. [Google Scholar]
- Mineyko, A.; Kirton, A. The black box of perinatal ischemic stroke pathogenesis. J. Child Neurol. 2011, 26, 1154–1162. [Google Scholar] [CrossRef]
- Dunbar, M.; Kirton, A. Perinatal stroke: Mechanisms, management, and outcomes of early cerebrovascular brain injury. Lancet Child Adolesc. Health 2018, 2, 666–676. [Google Scholar] [CrossRef]
- Brogna, C.; Brogna, B.; De Biase, M.; Sini, F.; Mirra, F.; Moro, M.; Romeo, D.M. Perinatal Cerebral Ischemic Lesion and SARS-CoV-2 Infection during Pregnancy: A Case Report and a Review of the Literature. J. Clin. Med. 2022, 11, 6827. [Google Scholar] [CrossRef] [PubMed]
- Revuelta, M.; Elicegui, A.; Moreno-Cugnon, L.; Bührer, C.; Matheu, A.; Schmitz, T. Ischemic stroke in neonatal and adult astrocytes. Mech. Ageing Dev. 2019, 183, 111147. [Google Scholar] [CrossRef] [PubMed]
- Kirton, A.; Deveber, G. Stroke in the fetus and neonate. Future Cardiol. 2006, 2, 593–604. [Google Scholar] [CrossRef]
- Berfelo, F.J.; Kersbergen, K.J.; van Ommen, C.H.; Govaert, P.; van Straaten, H.L.; Poll-The, B.T.; van Wezel-Meijler, G.; Vermeulen, R.J.; Groenendaal, F.; de Vries, L.S.; et al. Neonatal cerebral sinovenous thrombosis from symptom to outcome. Stroke 2010, 41, 1382–1388. [Google Scholar] [CrossRef][Green Version]
- Herz, J.; Bendix, I.; Felderhoff-Müser, U. Peripheral immune cells and perinatal brain injury: A double-edged sword? Pediatr. Res. 2022, 91, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Kentab, A.Y. Unilateral Basal Ganglia Infarction in a Neonate Born to a Mother with Gestational Diabetes: Case Report. J. Neurol. Stroke 2016, 5, 00180. [Google Scholar] [CrossRef][Green Version]
- Chabrier, S.; Husson, B.; Dinomais, M.; Landrieu, P.; Nguyen The Tich, S. New insights (and new interrogations) in perinatal arterial ischemic stroke. Thromb. Res. 2011, 127, 13–22. [Google Scholar] [CrossRef][Green Version]
- Lynch, J.K.; Han, C.J.; Nee, L.E.; Nelson, K.B. Prothrombotic factors in children with stroke or porencephaly. Pediatrics 2005, 116, 447–453. [Google Scholar] [CrossRef]
- Jankovic, M.; Petrovic, B.; Novakovic, I.; Brankovic, S.; Radosavljevic, N.; Nikolic, D. The Genetic Basis of Strokes in Pediatric Populations and Insight into New Therapeutic Options. Int. J. Mol. Sci. 2022, 23, 1601. [Google Scholar] [CrossRef]
- Gelfand, A.A.; Croen, L.A.; Torres, A.R.; Wu, Y.W. Genetic risk factors for perinatal arterial ischemic stroke. Pediatr. Neurol. 2013, 48, 36–41. [Google Scholar] [CrossRef][Green Version]
- Heath, P.T.; Nik Yusoff, N.K.; Baker, C.J. Neonatal meningitis. Arch. Dis. Child.-Fetal Neonatal Ed. 2003, 88, F173–F178. [Google Scholar] [CrossRef][Green Version]
- Chang, C.J.; Chang, W.N.; Huang, L.T.; Chang, Y.C.; Huang, S.C.; Hung, P.L. Outcomes of bacterial meningitis in children. Med. Mal. Infect. 2016, 46, 177–187. [Google Scholar]
- Choi, S.Y.; Kim, J.W.; Ko, J.W.; Lee, Y.S.; Chang, Y.P. Patterns of ischemic injury on brain images in neonatal group B Streptococcal meningitis. Korean J. Pediatr. 2018, 61, 245–252. [Google Scholar] [CrossRef]
- Brum, A.C.; Glasman, M.P.; De Luca, M.C.; Rugilo, C.A.; Urquizu Handal, M.I.; Picon, A.O.; Cook, C.; Vain, N.E. Ischemic Lesions in the Brain of a Neonate with SARS-CoV-2 Infection. Pediatr. Infect. Dis. J. 2021, 40, e340–e343. [Google Scholar] [CrossRef] [PubMed]
- Engert, V.; Siauw, C.; Stock, A.; Rehn, M.; Wöckel, A.; Härtel, C.; Wirbelauer, J. Severe Brain Damage in a Moderate Preterm Infant as Complication of Post-COVID-19 Response during Pregnancy. Neonatology 2021, 118, 505–508. [Google Scholar] [CrossRef] [PubMed]
- Vivanti, A.J.; Vauloup-Fellous, C.; Prevot, S.; Zupan, V.; Suffee, C.; Do Cao, J.; Benachi, A.; De Luca, D. Transplacental transmission of SARS-CoV-2 infection. Nat. Commun. 2020, 11, 3572. [Google Scholar] [CrossRef]
- Maury, A.; Lyoubi, A.; Peiffer-Smadja, N.; de Broucker, T.; Meppiel, E. Neurological manifestations associated with SARS-CoV-2 and other coronaviruses: A narrative review for clinicians. Rev. Neurol. 2021, 177, 51–64. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, M.A.; Ramenghi, L.A.; Cowan, F.M. Neonatal stroke. Arch. Dis. Child.-Fetal Neonatal Ed. 2012, 97, F377–F384, Erratum in Arch. Dis. Child.-Fetal Neonatal Ed. 2013, 98, F180. [Google Scholar] [CrossRef] [PubMed]
- Mercuri, E.; Cowan, F.; Rutherford, M.; Acolet, D.; Pennock, J.; Dubowitz, L. Ischaemic and haemorrhagic brain lesions in newborns with seizures and normal Apgar scores. Arch. Dis. Child.-Fetal Neonatal Ed. 1995, 73, F67–F74. [Google Scholar] [CrossRef][Green Version]
- Srinivasan, J.; Miller, S.P.; Phan, T.G.; Mackay, M.T. Delayed recognition of initial stroke in children: Need for increased awareness. Pediatrics 2009, 124, e227–e234. [Google Scholar] [CrossRef]
- de Vries, L.S.; Groenendaal, F.; Eken, P.; van Haastert, I.C.; Rademaker, K.J.; Meiners, L.C. Infarcts in the vascular distribution of the middle cerebral artery in preterm and fullterm infants. Neuropediatrics 1997, 28, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Schmahmann, J.D. Vascular syndromes of the thalamus. Stroke 2003, 34, 2264–2278. [Google Scholar] [CrossRef] [PubMed]
- Núñez, C.; Stephan-Otto, C.; Arca, G.; Agut, T.; Arnaez, J.; Cordeiro, M.; Benavente-Fernández, I.; Boronat, N.; Lubián-López, S.P.; Valverde, E.; et al. Neonatal arterial stroke location is associated with outcome at 2 years: A voxel-based lesion-symptom mapping study. Arch. Dis. Child.-Fetal Neonatal Ed. 2022, 107, 45–50. [Google Scholar] [CrossRef]
- Dinomais, M.; Hertz-Pannier, L.; Groeschel, S.; Chabrier, S.; Delion, M.; Husson, B.; Kossorotoff, M.; Renaud, C.; Nguyen The Tich, S.; AVCnn Study Group. Long term motor function after neonatal stroke: Lesion localization above all. Hum. Brain Mapp. 2015, 36, 4793–4807. [Google Scholar] [CrossRef]
- Oberhuber, M.; Hope, T.M.H.; Seghier, M.L.; Parker Jones, O.; Prejawa, S.; Green, D.W.; Price, C.J. Four Functionally Distinct Regions in the Left Supramarginal Gyrus Support Word Processing. Cereb. Cortex 2016, 26, 4212–4226. [Google Scholar] [CrossRef][Green Version]
- Peterson, R.K.; Williams, T.S.; McDonald, K.P.; Dlamini, N.; Westmacott, R. Cognitive and Academic Outcomes Following Childhood Cortical Stroke. J. Child Neurol. 2019, 34, 897–906. [Google Scholar] [CrossRef]
- Pierrat, V.; Marchand-Martin, L.; Arnaud, C.; Kaminski, M.; Resche-Rigon, M.; Lebeaux, C.; Bodeau-Livinec, F.; Morgan, A.S.; Goffinet, F.; Marret, S.; et al. Neurodevelopmental outcome at 2 years for preterm children born at 22 to 34 weeks’ gestation in France in 2011: EPIPAGE-2 cohort study. BMJ 2017, 358, j3448. [Google Scholar] [CrossRef][Green Version]
- Basu, A.P. Early intervention after perinatal stroke: Opportunities and challenges. Dev. Med. Child Neurol. 2014, 56, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Elgendy, M.M.; Puthuraya, S.; LoPiccolo, C.; Liu, W.; Aly, H.; Karnati, S. Neonatal stroke: Clinical characteristics and neurodevelopmental outcomes. Pediatr. Neonatol. 2022, 63, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Rattani, A.; Lim, J.; Mistry, A.M.; Prablek, M.A.; Roth, S.G.; Jordan, L.C.; Shannon, C.N.; Naftel, R.P. Incidence of Epilepsy and Associated Risk Factors in Perinatal Ischemic Stroke Survivors. Pediatr. Neurol. 2019, 90, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Wagenaar, N.; van den Berk, D.J.M.; Lemmers, P.M.A.; van der Aa, N.E.; Dudink, J.; van Bel, F.; Groenendaal, F.; de Vries, L.S.; Benders, M.J.N.L.; Alderliesten, T. Brain Activity and Cerebral Oxygenation After Perinatal Arterial Ischemic Stroke Are Associated With Neurodevelopment. Stroke 2019, 50, 2668–2676. [Google Scholar] [CrossRef]
- van Buuren, L.M.; van der Aa, N.E.; Dekker, H.C.; Vermeulen, R.J.; van Nieuwenhuizen, O.; van Schooneveld, M.M.; de Vries, L.S. Cognitive outcome in childhood after unilateral perinatal brain injury. Dev. Med. Child Neurol. 2013, 55, 934–940. [Google Scholar] [CrossRef]
- Joma, M.; Fovet, C.M.; Seddiki, N.; Gressens, P.; Laforge, M. COVID-19 and Pregnancy: Vertical Transmission and Inflammation Impact on Newborns. Vaccines 2021, 9, 391. [Google Scholar] [CrossRef]
- Shanes, E.D.; Mithal, L.B.; Otero, S.; Azad, H.A.; Miller, E.S.; Goldstein, J.A. Placental Pathology in COVID-19. Am. J. Clin. Pathol. 2020, 154, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Ren, J.; Xu, L.; Ke, X.; Xiong, L.; Tian, X.; Fan, C.; Yan, H.; Yuan, J. Placental pathology of the third trimester pregnant women from COVID-19. Diagn. Pathol. 2021, 16, 8. [Google Scholar] [CrossRef]
- Sehgal, A. Perinatal stroke: A case-based review. Eur. J. Pediatr. 2012, 171, 225–234. [Google Scholar] [CrossRef]
- Grau, A.J.; Buggle, F.; Heindl, S.; Steichen-Wiehn, C.; Banerjee, T.; Maiwald, M.; Rohlfs, M.; Suhr, H.; Fiehn, W.; Becher, H.; et al. Recent infection as a risk factor for cerebrovascular ischemia. Stroke 1995, 26, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Grau, A.J. Infection, inflammation, and cerebrovascular ischemia. Neurology 1997, 49 (Suppl. 4), S47–S51. [Google Scholar] [CrossRef]
- Mercuri, E.; Cowan, F.; Gupte, G.; Manning, R.; Laffan, M.; Rutherford, M.; Edwards, A.D.; Dubowitz, L.; Roberts, I. Prothrombotic disorders and abnormal neurodevelopmental outcome in infants with neonatal cerebral infarction. Pediatrics 2001, 107, 1400–1404. [Google Scholar] [CrossRef] [PubMed]
- Hagstrom, J.N.; Walter, J.; Bluebond-Langner, R.; Amatniek, J.C.; Manno, C.S.; High, K.A. Prevalence of the factor V leiden mutation in children and neonates with thromboembolic disease. J. Pediatr. 1998, 133, 777–781. [Google Scholar] [CrossRef]
- Schwartz, E.S.; Barkovich, A.J. Brain and Spine Injuries in Infancy and Childhood. In Pediatric Neuroimaging, 6th ed.; Barkovich, A.J., Raybaud, C., Eds.; Wolters Kluver: Alphen aan den Rijn, The Netherlands, 2019; p. 236. [Google Scholar]
- Kirton, A.; Deveber, G.; Pontigon, A.M.; Macgregor, D.; Shroff, M. Presumed perinatal ischemic stroke: Vascular classification predicts outcomes. Ann Neurol. 2008, 63, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Adams, K.V.; Mahmud, N.; Green-Holland, M.; Vonderwalde, I.; Umebayashi, D.; Sachewsky, N.; Coles, B.L.; van der Kooy, D.; Morshead, C.M. Constraint–induced movement therapy promotes motor recovery after neonatal stroke in the absence of neural precursor activation. Eur. J. Neurosci. 2021, 53, 1334–1349. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vasilescu, D.I.; Rosoga, A.M.; Vasilescu, S.; Dragomir, I.; Dima, V.; Dan, A.M.; Cirstoiu, M.M. SARS-CoV-2 Infection during Pregnancy Followed by Thalamic Neonatal Stroke—Case Report. Children 2023, 10, 958. https://doi.org/10.3390/children10060958
Vasilescu DI, Rosoga AM, Vasilescu S, Dragomir I, Dima V, Dan AM, Cirstoiu MM. SARS-CoV-2 Infection during Pregnancy Followed by Thalamic Neonatal Stroke—Case Report. Children. 2023; 10(6):958. https://doi.org/10.3390/children10060958
Chicago/Turabian StyleVasilescu, Diana Iulia, Ana Maria Rosoga, Sorin Vasilescu, Ion Dragomir, Vlad Dima, Adriana Mihaela Dan, and Monica Mihaela Cirstoiu. 2023. "SARS-CoV-2 Infection during Pregnancy Followed by Thalamic Neonatal Stroke—Case Report" Children 10, no. 6: 958. https://doi.org/10.3390/children10060958
APA StyleVasilescu, D. I., Rosoga, A. M., Vasilescu, S., Dragomir, I., Dima, V., Dan, A. M., & Cirstoiu, M. M. (2023). SARS-CoV-2 Infection during Pregnancy Followed by Thalamic Neonatal Stroke—Case Report. Children, 10(6), 958. https://doi.org/10.3390/children10060958





