Trends and Prevalence of Hospital Admissions Related to Deliberate Self-Poisoning and Used Substances in Romanian Adolescents between 2016 and 2022
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants Selection
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Sample
3.2. Characteristics of Admissions Due to Self-Poisoning
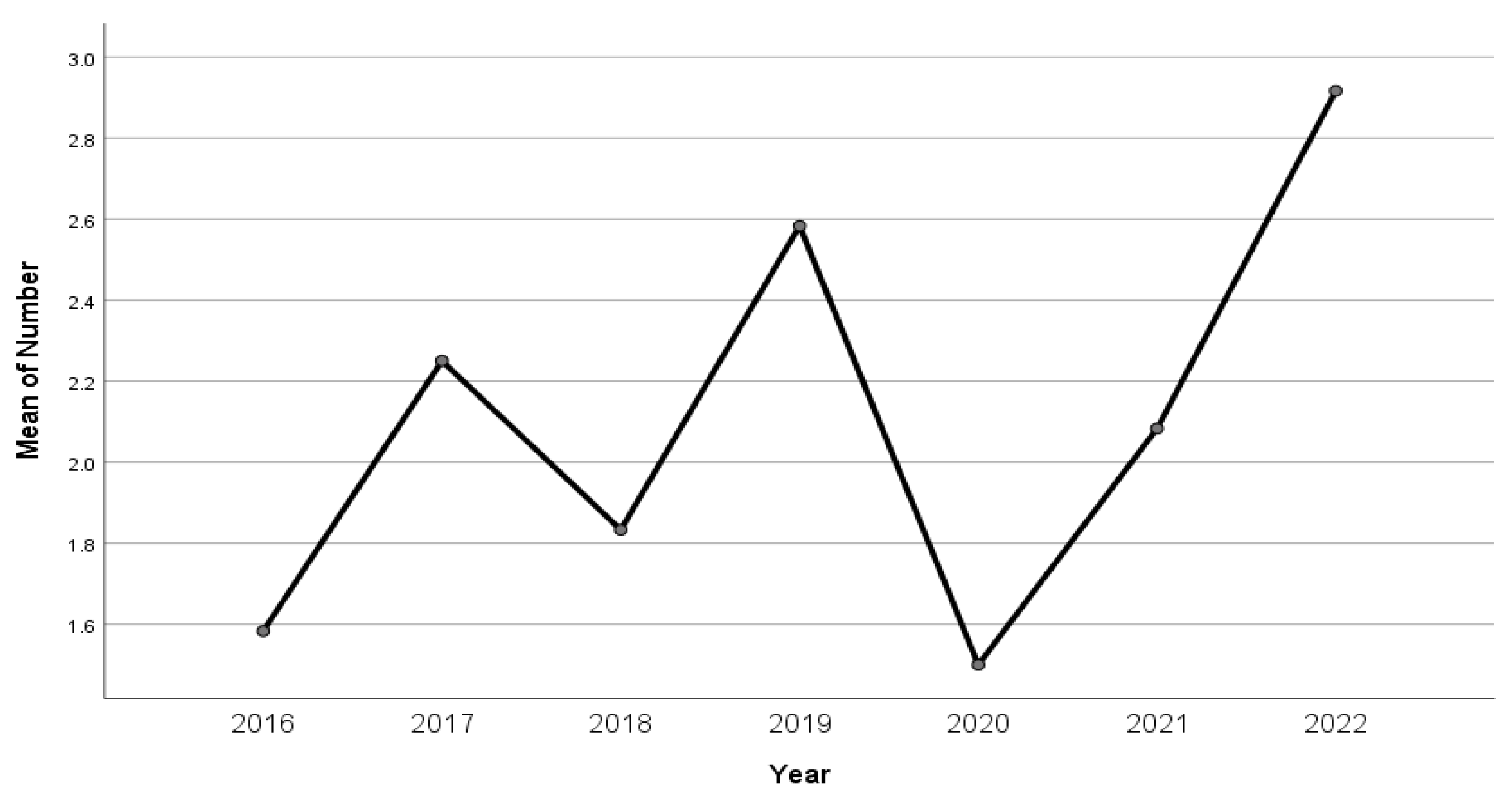
3.3. Trends in Self-Poisoning Episodes during the Period of 2016–2022
3.4. The Impact of COVID-19 Pandemic
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cairns, R.; Karanges, E.A.; Wong, A.; Brown, J.A.; Robinson, J.; Pearson, S.A.; Dawson, A.H.; Buckley, N.A. Trends in Self-Poisoning and Psychotropic Drug Use in People Aged 5–19 Years: A Population-Based Retrospective Cohort Study in Australia. BMJ Open 2019, 9, 2008–2015. [Google Scholar] [CrossRef] [PubMed]
- Gilley, M.; Sivilotti, M.L.A.; Juurlink, D.N.; Macdonald, E.; Yao, Z.; Finkelstein, Y. Trends of Intentional Drug Overdose among Youth: A Population-Based Cohort Study. Clin. Toxicol. 2020, 58, 711–715. [Google Scholar] [CrossRef] [PubMed]
- Spiller, H.A.; Ackerman, J.P.; Spiller, N.E.; Casavant, M.J. Sex- and Age-Specific Increases in Suicide Attempts by Self-Poisoning in the United States among Youth and Young Adults from 2000 to 2018. J. Pediatr. 2019, 210, 201–208. [Google Scholar] [CrossRef]
- Tyrrell, E.G.; Kendrick, D.; Sayal, K.; Orton, E. Poisoning substances taken by young people: A population-based cohort study. Br. J. Gen. Pract. 2018, 68, e703–e710. [Google Scholar] [CrossRef]
- Pawer, S.; Rajabali, F.; Zheng, A.; Smith, J.; Purssell, R.; Pike, I. Analyses of Child and Youth Self-Poisoning Hospitalizations by Substance and Socioeconomic Status. Int. J. Environ. Res. Public Health 2021, 18, 7003. [Google Scholar] [CrossRef]
- Wang, Y.J.; Li, X.; Ng, C.H.; Xu, D.W.; Hu, S.; Yuan, T.F. Risk Factors for Non-Suicidal Self-Injury (NSSI) in Adolescents: A Meta-Analysis. eClinicalMedicine 2022, 46, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bowes, L.; Wolke, D.; Joinson, C.; Lereya, S.T.; Lewis, G. Sibling Bullying and Risk of Depression, Anxiety, and Self-Harm: A Prospective Cohort Study. Pediatrics 2014, 134, e1032–e1039. [Google Scholar] [CrossRef]
- She, J.; Liu, L.; Liu, W. COVID-19 Epidemic: Disease Characteristics in Children. J. Med. Virol. 2020, 92, 747–754. [Google Scholar] [CrossRef]
- Pavone, P.; Ceccarelli, M.; Taibi, R.; Rocca, G.L.A.; Nunnari, G. Outbreak of COVID-19 Infection in Children: Fear and Serenity. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 4572–4575. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and Mental Health: A Review of the Existing Literature. Asian J. Psychiatr. 2020, 52, 102066. [Google Scholar] [CrossRef]
- Henry, N.; Parthiban, S.; Farroha, A. The Effect of COVID-19 Lockdown on the Incidence of Deliberate Self-Harm Injuries Presenting to the Emergency Room. Int. J. Psychiatry Med. 2021, 56, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-Analysis. JAMA Pediatr. 2021, 175, 1142–1150. [Google Scholar] [CrossRef]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J. Trop. Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef] [PubMed]
- Panchal, U.; Salazar de Pablo, G.; Franco, M.; Moreno, C.; Parellada, M.; Arango, C.; Fusar-Poli, P. The Impact of COVID-19 Lockdown on Child and Adolescent Mental Health: Systematic Review. Eur. Child Adolesc. Psychiatry 2021, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Amran, M.S. Psychosocial Risk Factors Associated with Mental Health of Adolescents amidst the COVID-19 Pandemic Outbreak. Int. J. Soc. Psychiatry 2022, 68, 6–8. [Google Scholar] [CrossRef]
- Cappa, C.; Jijon, I. COVID-19 and Violence against Children: A Review of Early Studies. Child Abus. Negl. 2021, 116, 105053. [Google Scholar] [CrossRef]
- Mourouvaye, M.; Bottemanne, H.; Bonny, G.; Fourcade, L.; Angoulvant, F.; Cohen, J.F.; Ouss, L. Association between Suicide Behaviours in Children and Adolescents and the COVID-19 Lockdown in Paris, France: A Retrospective Observational Study. Arch. Dis. Child. 2021, 106, 918–919. [Google Scholar] [CrossRef]
- Hawton, K.; Saunders, K.; Topiwala, A.; Haw, C. Psychiatric Disorders in Patients Presenting to Hospital Following Self-Harm: A Systematic Review. J. Affect. Disord. 2013, 151, 821–830. [Google Scholar] [CrossRef]
- Pirkis, J.; John, A.; Shin, S.; DelPozo-Banos, M.; Arya, V.; Analuisa-Aguilar, P.; Appleby, L.; Arensman, E.; Bantjes, J.; Baran, A.; et al. Suicide Trends in the Early Months of the COVID-19 Pandemic: An Interrupted Time-Series Analysis of Preliminary Data from 21 Countries. Lancet Psychiatry 2021, 8, 579–588. [Google Scholar] [CrossRef]
- Isumi, A.; Doi, S.; Yamaoka, Y.; Takahashi, K.; Fujiwara, T. Do Suicide Rates in Children and Adolescents Change during School Closure in Japan? The Acute Effect of the First Wave of COVID-19 Pandemic on Child and Adolescent Mental Health. Child Abuse Negl. 2020, 110 Pt 2, 104680. [Google Scholar] [CrossRef]
- Bruns, N.; Willemsen, L.; Stang, A.; Kowall, B.; Holtkamp, K.; Kamp, O.; Dudda, M.; Hey, F.; Hoffmann, F.; Blankenburg, J.; et al. Pediatric ICU Admissions after Adolescent Suicide Attempts during the Pandemic. Pediatrics 2022, 150, e2021055973. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision ICD-10: Tabular List; World Health Organization: Geneva, Switzerland, 2016; Volume 1, pp. 33–95. [Google Scholar]
- Hawton, K.; Saunders, K.E.A.; O’Connor, R.C. Self-Harm and Suicide in Adolescents. Lancet 2012, 379, 2373–2382. [Google Scholar] [CrossRef] [PubMed]
- Rahman, F.; Webb, R.T.; Wittkowski, A. Risk Factors for Self-Harm Repetition in Adolescents: A Systematic Review. Clin. Psychol. Rev. 2021, 88, 102048. [Google Scholar] [CrossRef]
- Daly, M. Prevalence of Depression among Adolescents in the U.S. from 2009 to 2019: Analysis of Trends by Sex, Race/Ethnicity, and Income. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2022, 70, 496–499. [Google Scholar] [CrossRef]
- Tørmoen, A.J.; Myhre, M.; Walby, F.A.; Grøholt, B.; Rossow, I. Change in Prevalence of Self-Harm from 2002 to 2018 among Norwegian Adolescents. Eur. J. Public Health 2020, 30, 688–692. [Google Scholar] [CrossRef] [PubMed]
- Chou, I.-C.; Lin, C.-C.; Sung, F.-C.; Kao, C.-H. Attention-Deficit Hyperactivity Disorder Increases the Risk of Deliberate Self-Poisoning: A Population-Based Cohort. Eur. Psychiatry 2014, 29, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.T.; Trout, Z.M.; Hernandez, E.M.; Cheek, S.M.; Gerlus, N. A Behavioral and Cognitive Neuroscience Perspective on Impulsivity, Suicide, and Non-Suicidal Self-Injury: Meta-Analysis and Recommendations for Future Research. Neurosci. Biobehav. Rev. 2017, 83, 440–450. [Google Scholar] [CrossRef]
- Ward, J.H.; Curran, S. Self-Harm as the First Presentation of Attention Deficit Hyperactivity Disorder in Adolescents. Child Adolesc. Ment. Health 2021, 26, 303–309. [Google Scholar] [CrossRef]
- Breslin, K.; Balaban, J.; Shubkin, C.D. Adolescent Suicide: What Can Pediatricians Do? Curr. Opin. Pediatr. 2020, 32, 595–600. [Google Scholar] [CrossRef]
- Spiller, H.A.; Ackerman, J.P.; Smith, G.A.; Kistamgari, S.; Funk, A.R.; McDermott, M.R.; Casavant, M.J. Suicide Attempts by Self-Poisoning in the United States among 10–25 Year Olds from 2000 to 2018: Substances Used, Temporal Changes and Demographics. Clin. Toxicol. 2020, 58, 676–687. [Google Scholar] [CrossRef]
- Chitty, K.M.; Raubenheimer, J.; Cairns, R.; Kirby, K.A.; Buckley, N.A. Deliberate Self-Poisoning in Australian Adolescents Is Increased on School Days. J. Psychiatr. Res. 2022, 148, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Burešová, I.; Bartošová, K.; Čerňák, M. Connection between Parenting Styles and Self-Harm in Adolescence. Procedia Soc. Behav. Sci. 2015, 171, 1106–1113. [Google Scholar] [CrossRef]
- Moe, C.A.; Villaveces, A.; Rivara, F.P.; Rowhani-Rahbar, A. Self-Harming Behavior in Relation to Exposure to Inter-Personal Violence among Youth and Young Adults in Colombia. Int. J. Inj. Contr. Saf. Promot. 2022, 29, 76–85. [Google Scholar] [CrossRef]
- Miranda-Mendizabal, A.; Castellví, P.; Parés-Badell, O.; Alayo, I.; Almenara, J.; Alonso, I.; Blasco, M.J.; Cebrià, A.; Gabilondo, A.; Gili, M.; et al. Gender Differences in Suicidal Behavior in Adolescents and Young Adults: Systematic Review and Meta-Analysis of Longitudinal Studies. Int. J. Public Health 2019, 64, 265–283. [Google Scholar] [CrossRef]
- Ilia, S.; Sakapeti, E.; Briassoulis, P.; Gerostergios, G.; Vgontzas, A.; Briassoulis, G. Suicidality Prevalence in a Pediatric Psychiatric Clinic: Relation to Social and Environmental Risk Factors. Children 2023, 1, 558. [Google Scholar] [CrossRef]
- Rheinheimer, B.; Kunz, M.; Nicolella, A.; Bastos, T. Trends in Self-Poisoning in Children and Adolescents in Southern Brazil between 2005 and 2013. Eur. Psychiatry 2015, 30, S136. [Google Scholar] [CrossRef]
- Hawton, K.; Casey, D.; Bale, E.; Brand, F.; Ness, J.; Waters, K.; Kelly, S.; Geulayov, G. Self-Harm during the Early Period of the COVID-19 Pandemic in England: Comparative Trend Analysis of Hospital Presentations. J. Affect. Disord. 2021, 282, 991–995. [Google Scholar] [CrossRef]
- Pignon, B.; Gourevitch, R.; Tebeka, S.; Dubertret, C.; Cardot, H.; Dauriac-Le Masson, V.; Trebalag, A.-K.; Barruel, D.; Yon, L.; Hemery, F.; et al. Dramatic Reduction of Psychiatric Emergency Consultations during Lockdown Linked to COVID-19 in Paris and Suburbs. Psychiatry Clin. Neurosci. 2020, 74, 557–559. [Google Scholar] [CrossRef]
- Smalley, C.M.; Malone, D.A.J.; Meldon, S.W.; Borden, B.L.; Simon, E.L.; Muir, M.R.; Fertel, B.S. The Impact of COVID-19 on Suicidal Ideation and Alcohol Presentations to Emergency Departments in a Large Healthcare System. Am. J. Emerg. Med. 2021, 41, 237–238. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Calle, D.; Martínez-Alés, G.; Mediavilla, R.; Aguirre, P.; Rodríguez-Vega, B.; Bravo-Ortiz, M.F. Trends in Psychiatric Emergency Department Visits Due to Suicidal Ideation and Suicide Attempts during the COVID-19 Pandemic in Madrid, Spain. J. Clin. Psychiatry 2020, 81, 21721. [Google Scholar] [CrossRef]
- Fortea, A.; Fortea, L.; Gómez-Ramiro, M.; Fico, G.; Giménez-Palomo, A.; Sagué-Vilavella, M.; Pons-Cabrera, M.; Radua, J.; Vázquez, M.; Baldaquí, N.; et al. The Aftermath of COVID-19 Lockdown: Self-Harm and Suicide-Related Behavior among Children and Adolescents Admitted to the Psychiatric Emergency Department. Neurosci. Appl. 2022, 1, 100966. [Google Scholar] [CrossRef]
- Steinhausen, H.-C. Recent International Trends in Psychotropic Medication Prescriptions for Children and Adolescents. Eur. Child Adolesc. Psychiatry 2015, 24, 635–640. [Google Scholar] [CrossRef]
- Friedrich, J.M.; Sun, C.; Geng, X.; Calello, D.P.; Gillam, M.; Medeiros, K.L.; Smith, M.; Ruck, B.; Mazer-Amirshahi, M. Child and Adolescent Benzodiazepine Exposure and Overdose in the United States: 16 Years of Poison Center Data. Clin. Toxicol. 2020, 58, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Cipriani, A.; Zhou, X.; Del Giovane, C.; Hetrick, S.E.; Qin, B.; Whittington, C.; Coghill, D.; Zhang, Y.; Hazell, P.; Leucht, S.; et al. Comparative Efficacy and Tolerability of Antidepressants for Major Depressive Disorder in Children and Adolescents: A Network Meta-Analysis. Lancet 2016, 388, 881–890. [Google Scholar] [CrossRef]
- Sheridan, D.C.; Hendrickson, R.G.; Lin, A.L.; Fu, R.; Horowitz, B.Z. Adolescent Suicidal Ingestion: National Trends Over a Decade. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2017, 60, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Hiremath, M.; Craig, S.; Graudins, A. Adolescent Deliberate Self-Poisoning in South-East Melbourne. Emerg. Med. Australas. 2016, 28, 704–710. [Google Scholar] [CrossRef]
- Diggins, E.; Kelley, R.; Cottrell, D.; House, A.; Owens, D. Age-Related Differences in Self-Harm Presentations and Subsequent Management of Adolescents and Young Adults at the Emergency Department. J. Affect. Disord. 2017, 208, 399–405. [Google Scholar] [CrossRef]
- Buckley, N.A.; Whyte, I.M.; Dawson, A.H.; Isbister, G.K. A Prospective Cohort Study of Trends in Self-Poisoning, Newcastle, Australia, 1987–2012: Plus Ça Change, plus c’est La Même Chose. Med. J. Aust. 2015, 202, 438–442. [Google Scholar] [CrossRef]



| Characteristics | F (N = 147) | M (N = 31) | Total (N = 178) | |
|---|---|---|---|---|
| Age | 14.94 (SD 1.52) | 15.61 (SD 1.38) | 15.06 (SD 1.52) | |
| Living with both parents | 78 | 20 | 98 (55.05%) | |
| Divorced parents | 60 | 11 | 71 (39.88%) | |
| Foster home | 9 | 0 | 9 (5.05%) | |
| Family psychiatric history | 33 | 2 | 35 (19.66%) | |
| Family suicide history | 7 | 0 | 7 (3.93%) | |
| Psychiatric diagnosis Depression/anxiety | 112 | 22 | 134 (75.28%) | |
| Psychiatric diagnosis ADHD/ODD/CD | 29 | 9 | 38 (21.34%) | |
| Psychiatric treatment | 77 | 18 | 95 (53.37%) | |
| History of psychiatric treatment | 68 | 17 | 85 (47.75%) | |
| History of previous suicide attempts | 48 | 5 | 53 (29.77%) | |
| Substances used for self-poisoning | Paracetamol | 16 | 3 | 19 (10.67%) |
| Analgesics, excluding paracetamol | 8 | 2 | 10 (5.61%) | |
| Psychotropic drugs | 45 | 10 | 55 (30.89%) | |
| Multiple substances | 50 | 12 | 62 (34.83%) | |
| Other substances | 28 | 4 | 17.97%) | |
| School difficulties | 105 | 22 | 127 (71.34%) | |
| Family conflicts | 70 | 15 | 85 (47.75%) |
| Year of Admission | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | Total |
|---|---|---|---|---|---|---|---|---|
| Total admissions | 830 | 914 | 959 | 998 | 489 | 723 | 760 | 5673 |
| Total admissions due to self-poisoning, N (%) | 19 (2.28%) | 27 (2.9%) | 22 (2.29%) | 31 (3.1%) | 18 (3.68%) | 25 (3.45%) | 36 (4.73%) | 178 (3.14%) |
| First-time admission N (%) due to self-poisoning | 13 (68.42%) | 23 (85.18%) | 18 (81.81%) | 11 (35.48%) | 10 (55.55%) | 12 (48%) | 23 (63.88%) | 110 (61.79%) |
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Psychiatric diagnosis | 1 | ||||
| 2. History of psychiatric treatment | 0.012 | 1 | |||
| 3. History of previous suicide attempts | 0.001 | 0.435 ** | 1 | ||
| 4. First admission due to self-poisoning | 0.171 * | −0.637 ** | −0.449 ** | 1 | |
| 5. Duration of hospitalization (shorter/longer than 2 weeks) | −0.25 | −0.179 * | −0.093 | 0.215 ** | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Predescu, E.; Calugar, I.; Bibu-Monus, C.; Sipos, R. Trends and Prevalence of Hospital Admissions Related to Deliberate Self-Poisoning and Used Substances in Romanian Adolescents between 2016 and 2022. Children 2023, 10, 790. https://doi.org/10.3390/children10050790
Predescu E, Calugar I, Bibu-Monus C, Sipos R. Trends and Prevalence of Hospital Admissions Related to Deliberate Self-Poisoning and Used Substances in Romanian Adolescents between 2016 and 2022. Children. 2023; 10(5):790. https://doi.org/10.3390/children10050790
Chicago/Turabian StylePredescu, Elena, Iulia Calugar, Cristian Bibu-Monus, and Roxana Sipos. 2023. "Trends and Prevalence of Hospital Admissions Related to Deliberate Self-Poisoning and Used Substances in Romanian Adolescents between 2016 and 2022" Children 10, no. 5: 790. https://doi.org/10.3390/children10050790
APA StylePredescu, E., Calugar, I., Bibu-Monus, C., & Sipos, R. (2023). Trends and Prevalence of Hospital Admissions Related to Deliberate Self-Poisoning and Used Substances in Romanian Adolescents between 2016 and 2022. Children, 10(5), 790. https://doi.org/10.3390/children10050790





