Professional Feeding Guidance Improved Infants’ Self-Feeding Proportion during Complementary Foods Introduction in Beijing, China: An Exploratory Study
(This article belongs to the Section Pediatric Neonatology)
Abstract
:1. Introduction
2. Materials and Methods
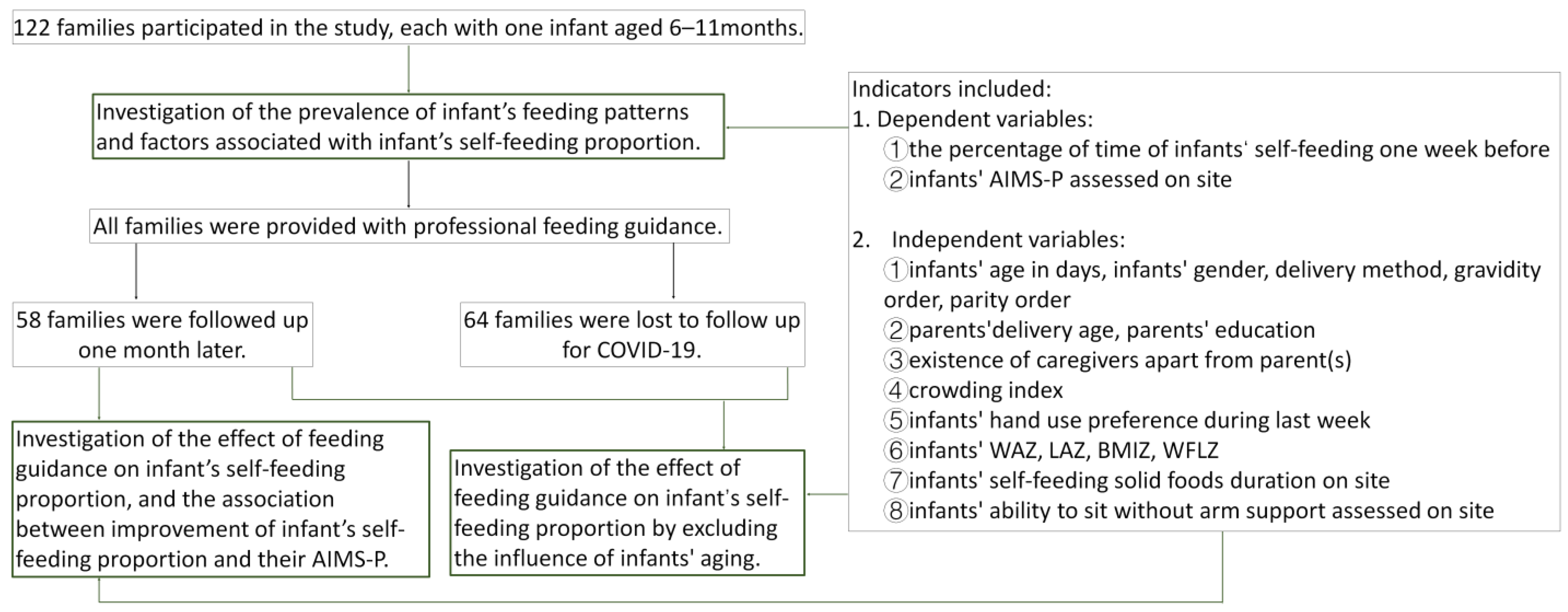
2.1. Participants
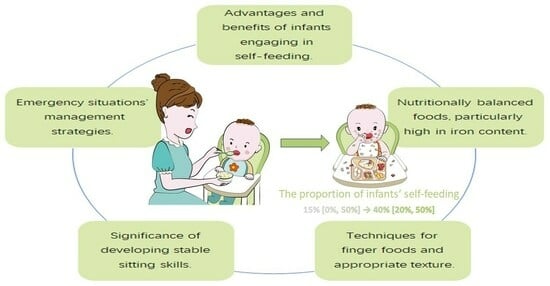
2.2. Procedures
2.2.1. Investigating the Prevalence of Infants’ Feeding Patterns and Associated Factors
2.2.2. Investigating the Influence of Professional Feeding Guidance on the Infants’ Self-Feeding Proportion
2.3. Statistical Analysis
3. Results
3.1. Basic Characteristics of the Families
3.2. The Factors Associated with the Proportion of Infants’ Self-Feeding
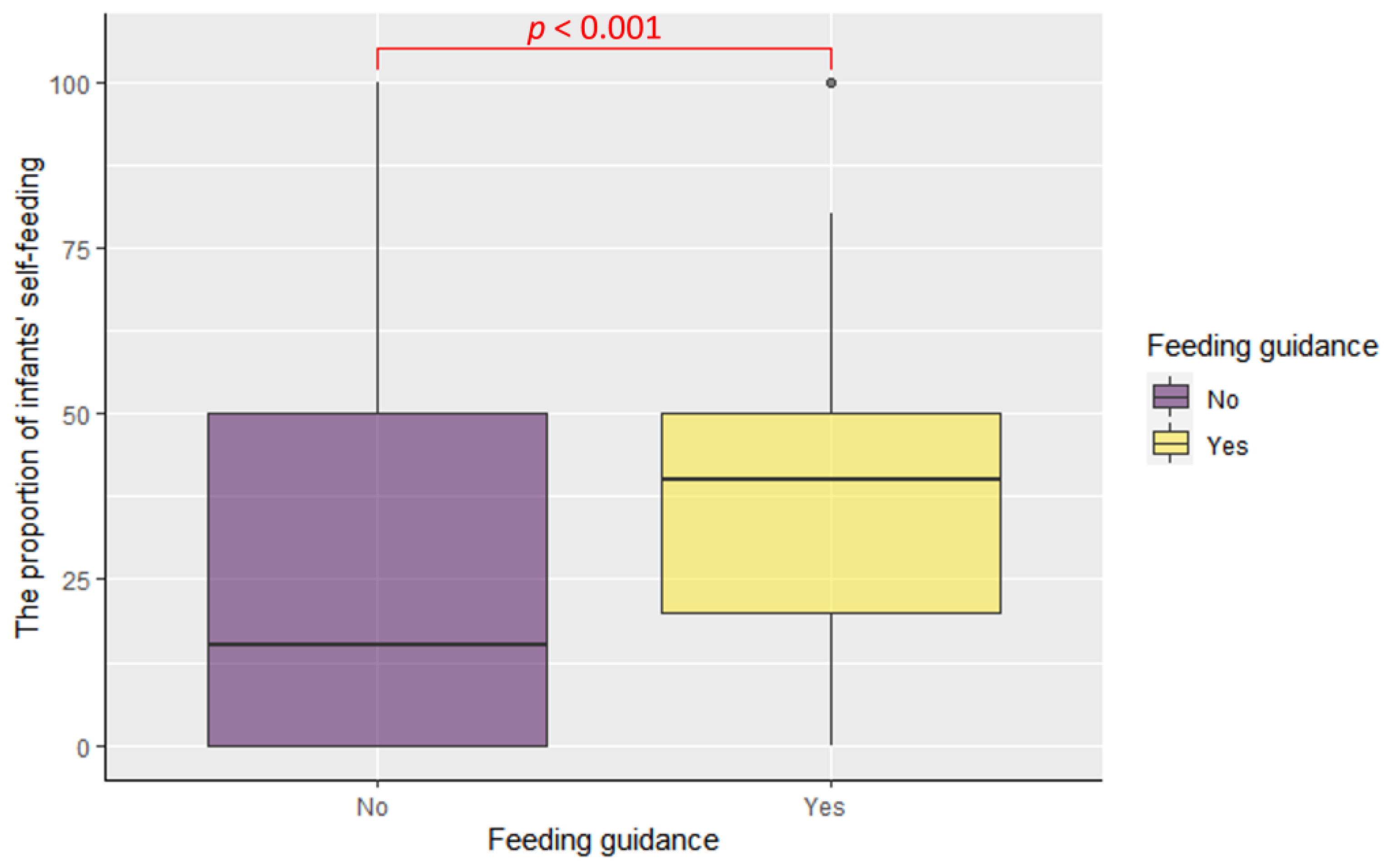
3.3. The Effect of Professional Feeding Guidance on the Proportion of Infants’ Self-Feeding
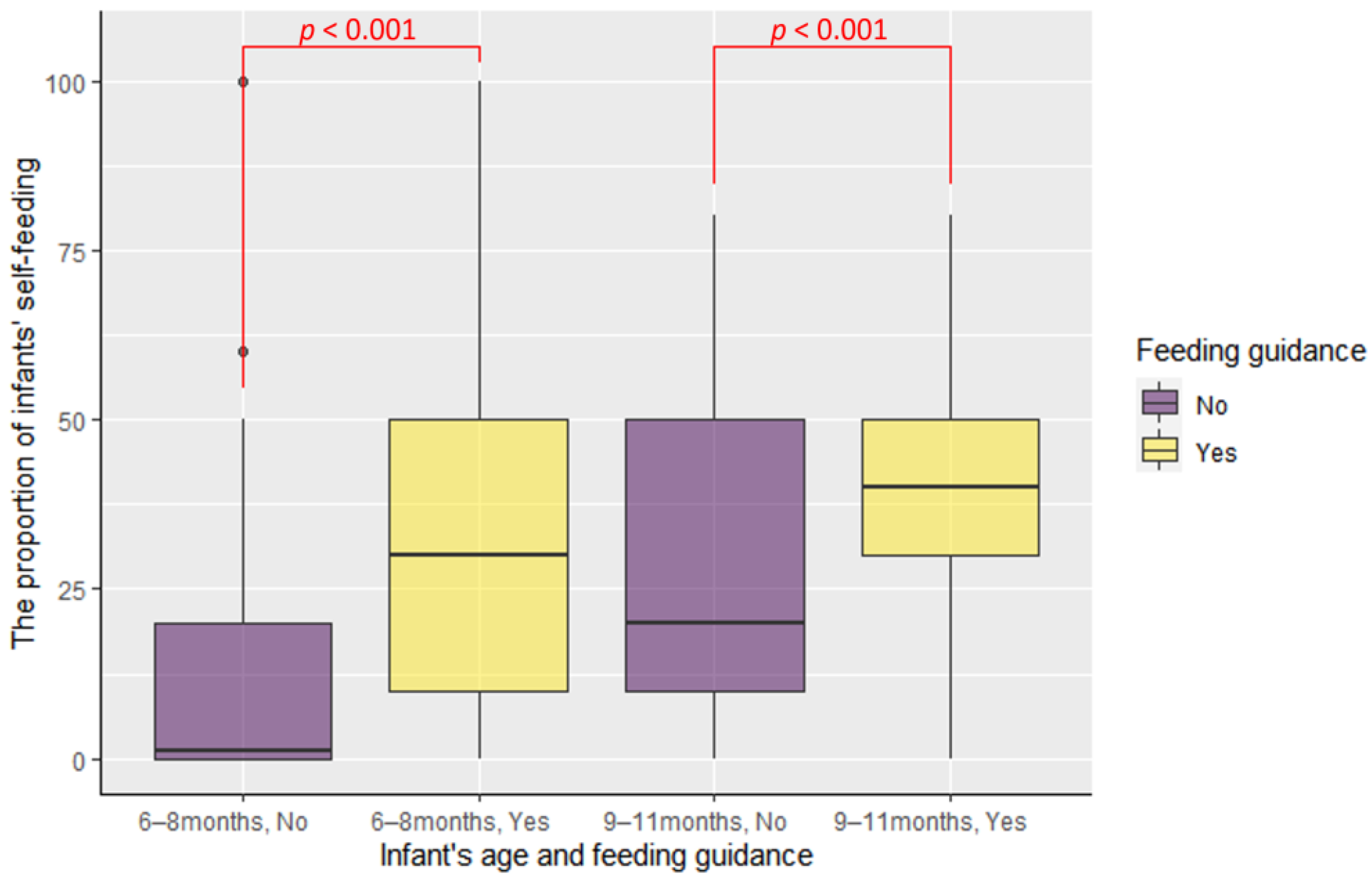
3.4. The Effect of Professional Feeding Guidance on the Infants’ Self-Feeding Proportion by Excluding the Influence of Infants’ Aging
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Complementary Feeding. Available online: https://www.who.int/health-topics/complementary-feeding#tab=tab_2 (accessed on 2 October 2023).
- Jackowska, M. Baby-led weaning—Co wiadomo o tym podejściu do żywienia niemowląt? Przegląd literatury. Pol. J. Nutr. 2016, 4, 65–72. [Google Scholar]
- Brown, A. Differences in eating behaviour, well-being and personality between mothers following baby-led vs. traditional weaning styles. Matern. Child. Nutr. 2016, 12, 826–837. [Google Scholar] [CrossRef]
- Brown, A.; Lee, M. Maternal control of child feeding during the weaning period: Differences between mothers following a baby-led or standard weaning approach. Matern. Child. Health J. 2011, 15, 1265–1271. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.; Lee, M. A descriptive study investigating the use and nature of baby-led weaning in a UK sample of mothers. Matern. Child. Nutr. 2011, 7, 34–47. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Conlon, C.A.; Haszard, J.J.; Beck, K.L.; von Hurst, P.R.; Taylor, R.W.; Heath, A.M. Food fussiness and early feeding characteristics of infants following Baby-Led Weaning and traditional spoon-feeding in New Zealand: An internet survey. Appetite 2018, 130, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Morison, B.J.; Heath, A.M.; Haszard, J.J.; Hein, K.; Fleming, E.A.; Daniels, L.; Erickson, E.W.; Fangupo, L.J.; Wheeler, B.J.; Taylor, B.J.; et al. Impact of a Modified Version of Baby-Led Weaning on Dietary Variety and Food Preferences in Infants. Nutrients 2018, 10, 1092. [Google Scholar] [CrossRef]
- Rapley, G. Baby-led weaning: Transitioning to solid foods at the baby’s own pace. Community Pract. 2011, 84, 20–23. [Google Scholar]
- Quintiliano-Scarpelli, D.; Lehmann, N.; Castillo, B.; Blanco, E. Infant Feeding and Information Sources in Chilean Families Who Reported Baby-Led Weaning as a Complementary Feeding Method. Nutrients 2021, 13, 2707. [Google Scholar] [CrossRef]
- Addessi, E.; Galloway, A.T.; Wingrove, T.; Brochu, H.; Pierantozzi, A.; Bellagamba, F.; Farrow, C.V. Baby-led weaning in Italy and potential implications for infant development. Appetite 2021, 164, 105286. [Google Scholar] [CrossRef]
- Webber, C.; Blissett, J.; Addessi, E.; Galloway, A.T.; Shapiro, L.; Farrow, C. An infant-led approach to complementary feeding is positively associated with language development. Matern. Child. Nutr. 2021, 17, e13206. [Google Scholar] [CrossRef]
- Białek-Dratwa, A.; Soczewka, M.; Grajek, M.; Szczepańska, E.; Kowalski, O. Use of the Baby-Led Weaning (BLW) Method in Complementary Feeding of the Infant-A Cross-Sectional Study of Mothers Using and Not Using the BLW Method. Nutrients 2022, 14, 2372. [Google Scholar] [CrossRef]
- Rapley, G. Spoon-Feeding or Self-Feeding? The Infant’s First Experience of Solid Food. Ph.D. Thesis, Canterbury Christ Church University, Canterbury, UK, 2015. [Google Scholar]
- Wright, C.M.; Cameron, K.; Tsiaka, M.; Parkinson, K.N. Is baby-led weaning feasible? When do babies first reach out for and eat finger foods? Matern. Child. Nutr. 2011, 7, 27–33. [Google Scholar] [CrossRef]
- Nantel, A.; Gingras, V. Are Complementary Feeding Practices Aligned with Current Recommendations? A Narrative Review. Children 2023, 10, 794. [Google Scholar] [CrossRef] [PubMed]
- Scottish Government. Scottish Maternal and Infant Nutrition Survey. 2017. Available online: https://www.gov.scot/publications/scottish-maternal-infant-nutrition-survey-2017/ (accessed on 21 February 2018).
- Kittisakmontri, K.; Fewtrell, M.; Roekworachai, K.; Phanpong, C.; Lanigan, J. Complementary feeding: Attitudes, knowledge and practices of urban families in northern Thailand. Nutr. Diet. 2019, 76, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Pries, A.M.; Huffman, S.L.; Adhikary, I.; Upreti, S.R.; Dhungel, S.; Champeny, M.; Zehner, E. High consumption of commercial food products among children less than 24 months of age and product promotion in Kathmandu Valley, Nepal. Matern. Child. Nutr. 2016, 12 (Suppl. S2), 22–37. [Google Scholar] [CrossRef] [PubMed]
- Stiller, C.K.; Golembiewski, S.K.E.; Golembiewski, M.; Mondal, S.; Biesalski, H.K.; Scherbaum, V. Maternal nutritional status and child feeding practices: A retrospective study in Santal communities, Birbhum District, West Bengal, India. Int. Breastfeed. J. 2020, 15, 50. [Google Scholar] [CrossRef]
- Cameron, S.L.; Heath, A.L.; Taylor, R.W. Healthcare professionals’ and mothers’ knowledge of, attitudes to and experiences with, Baby-Led Weaning: A content analysis study. BMJ Open 2012, 2, e001542. [Google Scholar] [CrossRef]
- Brown, A. No difference in self-reported frequency of choking between infants introduced to solid foods using a baby-led weaning or traditional spoon-feeding approach. J. Hum. Nutr. Diet. 2018, 31, 496–504. [Google Scholar] [CrossRef]
- Rowan, H.; Lee, M.; Brown, A. Estimated energy and nutrient intake for infants following baby-led and traditional weaning approaches. J. Hum. Nutr. Diet. 2022, 35, 325–336. [Google Scholar] [CrossRef]
- Guo, S.; Wang, Y.; Fries, L.R.; Li, Y.; Zhang, N.; Zhang, H.; Wei, H.; Jiang, X.; Shang, L. Infant and preschooler feeding behaviors in Chinese families: A systematic review. Appetite 2022, 168, 105768. [Google Scholar] [CrossRef]
- Historical Census of Housing Tables: Crowding. Available online: https://www.census.gov/data/tables/time-series/dec/coh-crowding.html (accessed on 8 October 2021).
- World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- WHOanthro. Available online: https://github.com/CDC-DNPAO/WHOanthro (accessed on 18 October 2022).
- China’s Nutrition Guidelines of Complementary Feeding for Infants and Toddlers (WS/T 678—2020). Available online: https://www.chinanutri.cn/yyzyxxpt/fgbzzx/xybz_112/202006/t20200615_217308.html (accessed on 15 June 2020).
- Better Health, Start for Life, What is Weaning? Available online: https://www.nhs.uk/start-for-life/baby/weaning/ (accessed on 2 October 2023).
- Briaux, J.; Fortin, S.; Kameli, Y.; Agboka, Y.; Romedenne, M.; Boko, J.; Martin-Prevel, Y.; Becquet, R.; Savy, M. Dissimilarities across age groups in the associations between complementary feeding practices and child growth: Evidence from rural Togo. Matern. Child. Nutr. 2019, 15, e12843. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Ríos, M.; Santiago-Pérez, M.I.; Butler, H.; Mourino, N.; Malvar, A.; Hervada, X. Baby-led weaning: Prevalence and associated factors in Spain. Eur. J. Pediatr. 2020, 179, 849–853. [Google Scholar] [CrossRef] [PubMed]
- Rapley, G. Baby-led weaning: The theory and evidence behind the approach. J. Health Visit. 2015, 3, 144–151. [Google Scholar] [CrossRef]
- Rapley, G.; Murkett, T. Baby-Led Weaning: Helping Your Baby to Love Good Food; Vermilion: Oxford, UK, 2008. [Google Scholar]
- Białek-Dratwa, A.; Kowalski, O.; Szczepańska, E. Traditional complementary feeding or BLW (Baby Led Weaning) method?—A cross-sectional study of Polish infants during complementary feeding. Front. Pediatr. 2022, 10, 992244. [Google Scholar] [CrossRef] [PubMed]
- Berthier, N.E.; Keen, R. Development of reaching in infancy. Exp. Brain Res. 2006, 169, 507–518. [Google Scholar] [CrossRef] [PubMed]
- Mulville, K.; Kai, J.; Kearney, J.M.; Ng-Osorio, J.; Boushey, C.J.; Fialkowski, M.K. A Qualitative Analysis of a Caregivers’ Experience of Complementary Feeding in a Population of Native Hawaiian, Other Pacific Islander and Filipino Infants: The Timing of the Introduction of Complementary Foods, and the Role of Transgenerational Experience. Nutrients 2022, 14, 3268. [Google Scholar] [CrossRef]
- Congiu, M.; Cimador, V.; Bettini, I.; Rongai, T.; Labriola, F.; Sbravati, F.; Marcato, C.; Alvisi, P. What Has Changed over Years on Complementary Feeding in Italy: An Update. Nutrients 2023, 15, 1280. [Google Scholar] [CrossRef]
- Bartkowski, J.P.; Kohler, J.; Xu, X.; Collins, T.; Roach, J.B.; Newkirk, C.; Klee, K. Racial Differences in Breastfeeding on the Mississippi Gulf Coast: Making Sense of a Promotion-Prevalence Paradox with Cross-Sectional Data. Healthcare 2022, 10, 2444. [Google Scholar] [CrossRef]
- Kostecka, M.; Kostecka-Jarecka, J. Knowledge on the Complementary Feeding of Infants Older than Six Months among Mothers Following Vegetarian and Traditional Diets. Nutrients 2021, 13, 3973. [Google Scholar] [CrossRef]

| Characteristic | n = 122 |
|---|---|
| Proportion of infants’ self-feeding (median [IQR]) | 10% [0%, 40%] |
| 6–8 months (n = 74) | 0% [0%, 30%] |
| 9–11 months (n = 48) | 20% [10%, 50%] |
| Infant age in days (median [IQR]) | 246.00 [205.75, 295.75] |
| Boys—no. (%) | 69 (56.6) |
| WAZ (mean (SD)) | 0.55 (0.95) |
| LAZ (mean (SD)) | 0.52 (1.10) |
| BMIZ (mean (SD)) | 0.35 (0.92) |
| WFLZ (mean (SD)) | 0.45 (0.91) |
| Maternal delivery age (median [IQR]) | 31.00 [29.00, 34.00] |
| Paternal delivery age (median [IQR]) | 32.00 [29.25, 36.00] |
| Vaginal delivery—no. (%) | 82 (67.2) |
| Gravidity ordered 1st—no. (%) | 92 (75.4) |
| Parity ordered 1st—no. (%) | 104 (85.2) |
| Mother with less than master’s degree—no. (%) | 71 (58.2) |
| Father with less than master’s degree—no. (%) | 80 (65.6) |
| Existence of caregivers apart from parent(s)—no. (%) | 112 (91.8) |
| Crowding index (median [IQR]) | 1.67 [1.33, 2.00] |
| Hand use preference | |
| No preference | 75 (61.5) |
| Left preference | 13 (10.7) |
| Right preference | 34 (27.9) |
| Self-feeding solid foods duration in the observation (median [IQR]) | 10.00 [8.00, 15.75] |
| The ability to sit without arm support—no. (%) | 97 (79.5) |
| AIMS-P | |
| <5th | 0 (0) |
| 5th~10th | 7 (5.7) |
| 10th~25th | 11 (9.0) |
| 25th~50th | 11 (9.0) |
| 50th~75th | 31 (25.4) |
| 75th~90th | 28 (23.0) |
| >90th | 34 (27.9) |
| Indicators | β | Standardized β | 95%CI | p |
|---|---|---|---|---|
| (Intercept) | 92.783 | <0.001 ** | ||
| Infants’ age in days | 0.098 | 0.200 | 0.01, 0.19 | 0.028 * |
| Caregivers apart from parent(s) | −11.457 | −0.128 | −27.46, 4.55 | 0.159 |
| No AIMS-P Increase | AIMS-P Increase | χ2 | p | |
|---|---|---|---|---|
| No improvement in infants’ self-feeding | 13 | 7 | 1.1657 | 0.2803 |
| Improvement in infants’ self-feeding | 31 | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, G.; Chang, J.; Guan, H.; Zhang, Y.; Zhang, T.; Zhang, Z. Professional Feeding Guidance Improved Infants’ Self-Feeding Proportion during Complementary Foods Introduction in Beijing, China: An Exploratory Study. Children 2023, 10, 1740. https://doi.org/10.3390/children10111740
Song G, Chang J, Guan H, Zhang Y, Zhang T, Zhang Z. Professional Feeding Guidance Improved Infants’ Self-Feeding Proportion during Complementary Foods Introduction in Beijing, China: An Exploratory Study. Children. 2023; 10(11):1740. https://doi.org/10.3390/children10111740
Chicago/Turabian StyleSong, Guochao, Jiahui Chang, Hongyan Guan, Yanfeng Zhang, Ting Zhang, and Zhaofeng Zhang. 2023. "Professional Feeding Guidance Improved Infants’ Self-Feeding Proportion during Complementary Foods Introduction in Beijing, China: An Exploratory Study" Children 10, no. 11: 1740. https://doi.org/10.3390/children10111740
APA StyleSong, G., Chang, J., Guan, H., Zhang, Y., Zhang, T., & Zhang, Z. (2023). Professional Feeding Guidance Improved Infants’ Self-Feeding Proportion during Complementary Foods Introduction in Beijing, China: An Exploratory Study. Children, 10(11), 1740. https://doi.org/10.3390/children10111740