The Impact of Parental Migration on Multidimensional Health of Children in Rural China: The Moderating Effect of Mobile Phone Addiction
Abstract
1. Introduction
1.1. Conceptual Framework and Hypotheses
1.2. Purpose
2. Materials and Methods
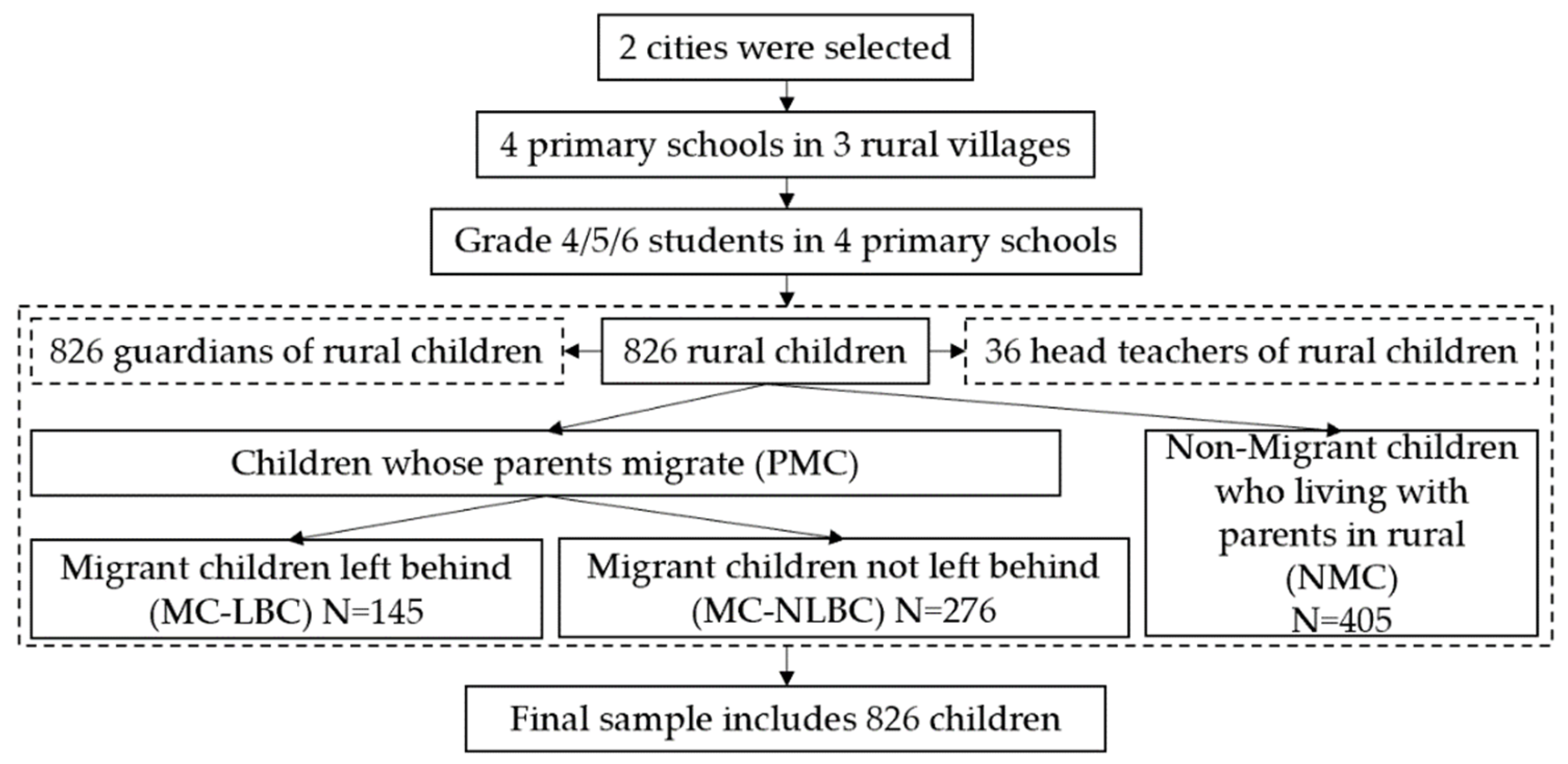
2.1. Data
2.2. Variable Measures
2.2.1. Multidimensional Health
2.2.2. Mobile Phone Addiction
2.3. Statistical Analysis and Model Specification
2.3.1. Statistical Analysis
2.3.2. Model Specification
3. Results
3.1. Descriptive Statistics Results
3.2. Baseline Regression Results
3.2.1. The Impact of Parental Migration on the Multidimensional Health of Rural Children
3.2.2. The Moderating Effect of Mobile Phone Addiction
3.3. Robustness Check
3.4. Heterogeneity Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Outcomes | Full Sample | Grade 4 | Grade 5 | Grade 6 |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Gender of child | −0.009 | −0.026 ** | −0.020 * | −0.016 ** |
| (0.005) | (0.006) | (0.007) | (0.002) | |
| Age of child | 0.037 ** | −0.014 | 0.029 | −0.007 |
| (0.018) | (0.010) | (0.031) | (0.010) | |
| Siblings | −0.006 | 0.002 | −0.008 | −0.018 *** |
| (0.006) | (0.026) | (0.005) | (0.001) | |
| Boarding | 0.000 | −0.019 * | 0.005 | −0.006 |
| (0.006) | (0.006) | (0.008) | (0.015) | |
| Left-behind Children | −0.001 | −0.013 | −0.001 | −0.015 * |
| (0.007) | (0.016) | (0.012) | (0.004) | |
| Age of guardian | 0.003 | −0.029 *** | −0.004 | −0.005 |
| (0.009) | (0.002) | (0.013) | (0.007) | |
| Education of guardian | 0.026 * | −0.010 | −0.022 ** | 0.026 * |
| (0.014) | (0.014) | (0.004) | (0.007) | |
| Annual family income | 0.018 * | −0.011 | −0.008 | −0.020 ** |
| (0.010) | (0.010) | (0.008) | (0.004) | |
| N | 826 | 826 | 826 | 826 |
| School FEs | Yes | Yes | Yes | Yes |
| Class FEs | Yes | Yes | Yes | Yes |
| Outcomes | Gender of Head Teacher | Age of Head Teacher | Teaching Age of Head Teacher |
| (1) | (2) | (3) | |
| Gender of child | 0.733 | −20.836 | −17.951 |
| (0.867) | (15.030) | (16.048) | |
| Age of child | 0.018 | −1.316 | −0.674 |
| (0.102) | (1.175) | (1.196) | |
| Siblings | −0.277 | −4.422 | −3.290 |
| (0.806) | (11.119) | (11.121) | |
| Boarding | −6.638 * | −48.649 | −38.335 |
| (3.705) | (41.426) | (41.538) | |
| Left-behind Children | −0.466 | 33.027 *** | 29.221 ** |
| (1.001) | (9.789) | (11.304) | |
| Age of guardian | −0.061 | 0.329 | 0.411 |
| (1.347) | (0.463) | (0.439) | |
| Education of guardian | −0.027 | 1.972 | 3.085 * |
| (0.063) | (1.636) | (1.607) | |
| Annual family income | 0.033 | −1.743 | −1.432 |
| (0.122) | (1.215) | (1.425) | |
| N | 826 | 826 | 826 |
| School FEs | Yes | Yes | Yes |
| Grade FEs | Yes | Yes | Yes |
| Class FEs | Yes | Yes | Yes |
References
- Wu, Y.; Guo, Z. An analysis of the nutritional status of left-behind children in rural China and the impact mechanisms of child malnutrition. Child. Youth Serv. Rev. 2020, 119, 105598. [Google Scholar] [CrossRef]
- Wang, H.; Zhu, R. Social spillovers of China’s left-behind children in the classroom. Labour Econ. 2021, 69, 101958. [Google Scholar] [CrossRef]
- Liang, Z.; Yue, Z.; Li, Y.; Li, Q.; Zhou, A. Choices or Constraints: Education of Migrant Children in Urban China. Popul. Res. Policy Rev. 2020, 39, 671–690. [Google Scholar] [CrossRef]
- Martínez-Montilla, J.M.; Mercken, L.; Lima-Serrano, M.; de Vries, H.; Lima-Rodríguez, J.S. Why are Spanish Adolescents Binge Drinkers? Focus Group with Adolescents and Parents. Int. J. Environ. Res. Public Health 2020, 17, 3551. [Google Scholar] [CrossRef] [PubMed]
- Schneiders, M.L.; Phou, M.; Tun, V.; Kelley, M.; Parker, M.; Turner, C. Grandparent caregiving in Cambodian skip-generation households: Roles and impact on child nutrition. Matern. Child Nutr. 2021, 17, 13269. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Wang, Y.; Gao, Y.; Wu, S.; Li, H.; Chen, Y.; Shi, Y. The Effect of Boarding on the Mental Health of Primary School Students in Western Rural China. Int. J. Environ. Res. Public Health 2020, 17, 8200. [Google Scholar] [CrossRef]
- Morinaga, M.; Hollander, A.-C.; Heuvelman, H.; Lundberg, M.; Dalman, C.; Rai, D.; Magnusson, C. Migration and risk of intellectual disability with and without autism: A population-based cohort study. Acta Psychiatr. Scand. 2021, 144, 487–500. [Google Scholar] [CrossRef]
- McKay, I.T.; Nadorff, D.K. The Impact of Custodial Grandparenting on Cognitive Performance in a Longitudinal Sample of Grandparents Raising Grandchildren. J. Fam. Issues 2021, 42, 2242–2262. [Google Scholar] [CrossRef]
- Min, S.; Hou, L.-L.; Hermann, W.; Huang, J.-K.; Mu, Y.-Y. The impact of migration on the food consumption and nutrition of left-behind family members: Evidence from a minority mountainous region of southwestern China. J. Integr. Agr. 2019, 18, 1780–1792. [Google Scholar] [CrossRef]
- Dong, Y.; Wang, W.; Li, S.; Zhang, L. The cumulative impact of parental migration on schooling of left-behind children in rural China. J. Rural Stud. 2021, 86, 527–541. [Google Scholar] [CrossRef]
- Topalovic, T.; Episkopou, M.; Schillberg, E.; Brcanski, J.; Jocic, M. Migrant children in transit: Health profile and social needs of unaccompanied and accompanied children visiting the MSF clinic in Belgrade, Serbia. Confl. Health 2021, 15, 32. [Google Scholar] [CrossRef]
- Liu, X.; Shi, X.; Chen, K. Inequality of opportunity in children’s nutritional outcomes in China. Glob. Food Sec. 2022, 33, 100635. [Google Scholar] [CrossRef]
- Gaskin, P.; Chami, P.; Ward, J.; Goodman, G.; Sing, B.; Jackson, M.; Broome, H. A practical model for identification of children at risk of excess energy intake in the developing world. Public Health Nutr. 2019, 22, 1979–1989. [Google Scholar] [CrossRef]
- Eiholzer, U.; Fritz, C.; Stephan, A. The increase in child obesity in Switzerland is mainly due to migration from Southern Europe—A cross-sectional study. BMC Public Health 2021, 21, 243. [Google Scholar] [CrossRef]
- Bohara, S.S.; Thapa, K.; Bhatt, L.D.; Dhami, S.S.; Wagle, S. Determinants of Junk Food Consumption Among Adolescents in Pokhara Valley, Nepal. Front. Nutr. 2021, 8, 109. [Google Scholar] [CrossRef]
- Fahrni, O.; Wilhelm-Bals, A.; Posfay-Barbe, K.M.; Wagner, N. Hypovitaminosis D in migrant children in Switzerland: A retrospective study. Eur. J. Pediatr. 2021, 180, 2637–2644. [Google Scholar] [CrossRef]
- Mao, M.; Zang, L.; Zhang, H. The Effects of Parental Absence on Children Development: Evidence from Left-Behind Children in China. Int. J. Environ. Res. Public Health 2020, 17, 6770. [Google Scholar] [CrossRef]
- Peng, C.; Wang, M.; Cheng, J.; Tan, Y.; Huang, Y.; Rong, F.; Kang, C.; Ding, H.; Yu, Y. Association between internet addiction and suicidal ideation, suicide plans, and suicide attempts among Chinese adolescents with and without parental migration. Comput. Hum. Behav. 2021, 125, 106949. [Google Scholar] [CrossRef]
- Cai, J.; Wang, Y.; Wang, F.; Lu, J.; Li, L.; Zhou, X. The Association of Parent-Child Communication with Internet Addiction in Left-Behind Children in China: A Cross-Sectional Study. Int. J. Public Health 2021, 66, 630700. [Google Scholar] [CrossRef]
- Bai, C.; Chen, X.; Han, K. Mobile phone addiction and school performance among Chinese adolescents from low-income families: A moderated mediation model. Child. Youth Serv. Rev. 2020, 118, 105406. [Google Scholar] [CrossRef]
- Zhen, R.; Li, L.; Ding, Y.; Hong, W.; Liu, R.-D. How does mobile phone dependency impair academic engagement among Chinese left-behind children? Child. Youth Serv. Rev. 2020, 116, 105169. [Google Scholar] [CrossRef]
- Chen, L.; Yan, Z.; Tang, W.; Yang, F.; Xie, X.; He, J. Mobile phone addiction levels and negative emotions among Chinese young adults: The mediating role of interpersonal problems. Comput. Hum. Behav. 2016, 55, 856–866. [Google Scholar] [CrossRef]
- Liu, Q.-Q.; Zhou, Z.-K.; Ynag, X.-J.; Kong, F.-C.; Niu, G.-F.; Fan, C.-Y. Mobile phone addiction and sleep quality among Chinese adolescents: A moderated mediation model. Comput. Hum. Behav. 2017, 72, 108–114. [Google Scholar] [CrossRef]
- Lissak, G. Adverse physiological and psychological effects of screen time on children and adolescents: Literature review and case study. Environ. Res. 2018, 164, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Lian, S.-L.; Sun, X.-J.; Niu, G.-F.; Yang, X.-J.; Zhou, Z.-K.; Yang, C. Mobile phone addiction and psychological distress among Chinese adolescents: The mediating role of rumination and moderating role of the capacity to be alone. J. Affect. Disord. 2021, 279, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Gao, T.; Li, J.; Zhang, H.; Gao, J.; Kong, Y.; Hu, Y.; Mei, S. The influence of alexithymia on mobile phone addiction: The role of depression, anxiety and stress. J. Affect. Disord. 2018, 225, 761–766. [Google Scholar] [CrossRef]
- Kühn, S.; Rieger, U.M. Health is a state of complete physical, mental and social well-being and not merely absence of disease or infirmity. Surg. Obes. Relat. Dis. 2017, 13, 887. [Google Scholar] [CrossRef]
- Lu, W.; Zhang, A.; Mossialos, E. Parental Migration and Self-Reported Health Status of Adolescents in China: A Cross-Sectional Study. eClinicalMedicine 2020, 22, 100371. [Google Scholar] [CrossRef]
- Gao, Y.; Li, L.P.; Kim, J.H.; Congdon, N.; Lau, J.; Griffiths, S. The impact of parental migration on health status and health behaviours among left behind adolescent school children in China. BMC Public Health 2010, 10, 56. [Google Scholar] [CrossRef]
- Janssen, M.F.; Szende, A.; Cabases, J.; Ramos-Goñi, J.M.; Vilagut, G.; König, H.H. Population norms for the EQ-5D-3L: A cross-country analysis of population surveys for 20 countries. Eur. J. Health Econ. 2019, 20, 205–216. [Google Scholar] [CrossRef]
- Schnittker, J.; Bacak, V. The Increasing Predictive Validity of Self-Rated Health. PLoS ONE 2014, 9, e84933. [Google Scholar] [CrossRef]
- Kang, E.; Grol-Prokopczyk, H. Comparing South Korean and US self-rated health using anchoring vignettes. Qual. Life Res. 2020, 29, 3213–3222. [Google Scholar] [CrossRef]
- Pacheco, J. Using Anchoring Vignettes to Reevaluate the Link between Self-Rated Health Status and Political Behavior. J. Health Polit. Policy Law 2019, 44, 533–558. [Google Scholar] [CrossRef]
- Au, N.; Lorgelly, P.K. Anchoring vignettes for health comparisons: An analysis of response consistency. Qual. Life Res. 2014, 23, 1721–1731. [Google Scholar] [CrossRef]
- Huang, L.; Chen, W.; Renzaho, A.M.N.; Hall, B.J. Validation of Obesity Status Based on Self-Reported Data among Filipina and Indonesian Female Migrant Domestic Workers in Macao (SAR), China. Int. J. Environ. Res. Public Health 2020, 17, 5927. [Google Scholar] [CrossRef]
- Yu, J.; Han, X.; Wen, H.; Ren, J.; Qi, L. Better Dietary Knowledge and Socioeconomic Status (SES), Better Body Mass Index? Evidence from China-An Unconditional Quantile Regression Approach. Nutrients 2020, 12, 1197. [Google Scholar] [CrossRef]
- Gutin, I. In BMI we trust: Reframing the body mass index as a measure of health. Soc. Theory Health 2018, 16, 256–271. [Google Scholar] [CrossRef]
- Carleton, R.N.; Thibodeau, M.A.; Teale, M.J.N.; Welch, P.G.; Abrams, M.P.; Robinson, T.; Asmundson, G.J.G. The Center for Epidemiologic Studies Depression Scale: A Review with a Theoretical and Empirical Examination of Item Content and Factor Structure. PLoS ONE 2013, 8, e58067. [Google Scholar] [CrossRef]
- Zhou, M.; Zhang, G.; Scott, R.; Kenny, K.; Xue, H. Depressive Symptoms of Chinese Children: Prevalence and Correlated Factors among Subgroups. Int. J. Environ. Res. Public Health 2018, 15, 283. [Google Scholar] [CrossRef]
- Dou, D.; Shek, D.T.L.; Zhu, X.; Zhao, L. Dimensionality of the Chinese CES-D: Is It Stable across Gender, Time, and Samples? Int. J. Environ. Res. Public Health 2021, 18, 11818. [Google Scholar] [CrossRef]
- Heckman, J.J.; Kautz, T. Fostering and Measuring Skills: Interventions that Improve Character and Cognition; Working Paper 19656; National Bureau of Economic Research: Cambridge, MA, USA, 2014. [Google Scholar]
- White, N.; Flannery, L.; McClintock, A.; Machado, L. Repeated computerized cognitive testing: Performance shifts and test–retest reliability in healthy older adults. J. Clin. Exp. Neuropsyc. 2019, 41, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Cheng, Z.; Smyth, R. Do migrant students affect local students’ academic achievements in urban China? Econ. Educ. Rev. 2018, 63, 64–77. [Google Scholar] [CrossRef]
- Sulik, M.J.; Obradović, J. Teachers’ rankings of children’s executive functions: Validating a methodology for school-based data collection. J. Exp. Child Psychol. 2018, 173, 136–154. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Wang, J.; Gan, L. Empower the Impoverished Students’ Education: A Randomized Controlled Field Experiment. Manag. World. 2022, 38, 63–82+112+83–84. [Google Scholar]
- Gong, J.; Yi, L.; Song, H. Gender Peer Effects on Students’ Academic and Noncognitive Outcomes: Evidence and Mechanisms. J. Hum. Resour. 2021, 56, 686–710. [Google Scholar] [CrossRef]
- Guo, Y.; Li, S.; Chen, S.; Tang, Y.; Liu, C. Health benefits of having more female classmates: Quasi-experimental evidence from China. Econ Educ Rev. 2022, 91, 102330. [Google Scholar] [CrossRef]
- Shen, X.; Wang, H.Z.; Rost, D.H.; Gaskin, J.; Wang, J.-L. State anxiety moderates the association between motivations and excessive smartphone use. Curr. Psychol. 2021, 40, 1937–1945. [Google Scholar] [CrossRef]
- Su, S.; Pan, T.T.; Liu, X.Q.; Chen, X.W.; Wang, Y.J.; Li, M.Y. Development of the smartphone addiction scale for college students. Chin. Ment. Health J. 2014, 28, 392–397. [Google Scholar]
- Yoshikawa, H.; Aber, J.L.; Beardslee, W.R. The effects of poverty on the mental, emotional, and behavioral health of children and youth: Implications for prevention. Am. Psychol. 2012, 67, 272–284. [Google Scholar] [CrossRef]
- Goodman, S.H. Intergenerational Transmission of Depression. Annu. Rev. Clin. Psycho. 2020, 16, 213–238. [Google Scholar] [CrossRef]
- Spruit, A.; Goos, L.; Weenink, N.; Rodenburg, R.; Niemeyer, H.; Stams, G.J.; Colonnesi, C. The Relation Between Attachment and Depression in Children and Adolescents: A Multilevel Meta-Analysis. Clin. Child Fam. Psychol. Rev. 2020, 23, 54–69. [Google Scholar] [CrossRef]
- Anger, S.; Heineck, G. Do smart parents raise smart children? The intergenerational transmission of cognitive abilities. J. Popul. Econ. 2010, 23, 1105–1132. [Google Scholar] [CrossRef]
- Grol-Prokopczyk, H.; Freese, J.; Hauser, R.M. Using anchoring vignettes to assess group differences in general selfrated health. J. Health Soc. Behav. 2011, 52, 246–261. [Google Scholar] [CrossRef]
- Li, M.; Zhu, N.; Zeng, L.; Wang, D.; Dang, S.; Watson, V.; Chen, T.; Hua, Z.; Li, Z.; Kang, Y.; et al. Effect of Parental Migration on the Intellectual and Physical Development of Early School-Aged Children in Rural China. Int. J. Environ. Res. Public Health 2020, 17, 339. [Google Scholar] [CrossRef]
- Griffith, M.; Mellor, D.; Green, J.; Renzaho, A.M. Migration and obesity. Nutr. Diet 2014, 71, 252–257. [Google Scholar] [CrossRef]
- Zhao, G.; Wang, M.; Xu, J.; Lu, J.; Akezhuoli, H.; Wang, F. Health Status and Association with Interpersonal Relationships Among Chinese Children from Urban Migrant to Rural Left-Behind. Front. Public Health 2022, 10, 862219. [Google Scholar] [CrossRef]
- Ye, J.; Pan, L. Differentiated childhoods: Impacts of rural labor migration on left-behind children in China. J. Peasant Stud. 2011, 38, 355–377. [Google Scholar]
- Wang, L.; Zheng, Y.; Li, G.; Li, Y.; Fang, Z.; Abbey, C.; Rozelle, S. Academic achievement and mental health of left-behind children in rural China: A causal study on parental migration. China Agric. Econ. Rev. 2019, 11, 569–582. [Google Scholar] [CrossRef]
- Zhen, R.; Li, L.; Liu, X.; Zhou, X. Negative life events, depression, and mobile phone dependency among left-behind adolescents in rural China: An interpersonal perspective. Child. Youth Serv. Rev. 2020, 109, 104688. [Google Scholar] [CrossRef]
- Martin, C.; Gilmore, L.; Apolzan, J.; Myers, C.; Thomas, D.; Redman, L. Smartloss: A Personalized Mobile Health Intervention for Weight Management and Health Promotion. JMIR Mhealth Uhealth 2016, 4, e18. [Google Scholar] [CrossRef]
- Shaw, M.P.; Satchell, L.P.; Thompson, S.; Harper, E.T. Smartphone and Tablet Software Apps to Collect Data in Sport and Exercise Settings: Cross-sectional International Survey. JMIR Mhealth Uhealth 2020. preprint. [Google Scholar] [CrossRef] [PubMed]
- Walsh, S.P.; White, K.M.; Young, R.M. Over-connected? A qualitative exploration of the relationship between Australian youth and their mobile phones. J. Adolescence 2008, 31, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.-Q.; Yang, X.-J.; Hu, Y.-T.; Zhang, C.-Y. Peer victimization, self-compassion, gender and adolescent mobile phone addiction: Unique and interactive effects. Child. Youth Serv. Rev. 2020, 118, 105397. [Google Scholar] [CrossRef]

| Dependent Variables | Variable Definition | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| Physical Health | |||||
| Self-rated health | 1–5 from “very unhealthy” to “very healthy” | 3.72 | 1.18 | 1 | 5 |
| BMI a | 1 = thin, 2 = normal, 3 = overweight, 4 = obese | 1.75 | 0.92 | 1 | 4 |
| Mental Health | |||||
| CES-D score | The higher the score, the more severe of depressive symptoms | 16.82 | 10.24 | 0 | 57 |
| Depression severity | |||||
| no depression | 1 = Yes, 0 = No | 0.575 | 0.495 | 0 | 1 |
| mild depression | 1 = Yes, 0 = No | 0.183 | 0.387 | 0 | 1 |
| Moderate depression | 1 = Yes, 0 = No | 0.111 | 0.315 | 0 | 1 |
| severe depression | 1 = Yes, 0 = No | 0.131 | 0.337 | 0 | 1 |
| Cognitive Ability | |||||
| Ranking of academic achievement | |||||
| Excellent | 1= Yes, 0 = No | 0.188 | 0.391 | 0 | 1 |
| Very good | 1 = Yes, 0 = No | 0.203 | 0.403 | 0 | 1 |
| Medium | 1 = Yes, 0 = No | 0.197 | 0.398 | 0 | 1 |
| Poor | 1 = Yes, 0 = No | 0.203 | 0.403 | 0 | 1 |
| Very poor | 1= Yes, 0 = No | 0.208 | 0.406 | 0 | 1 |
| Independent Variables | |||||
| Children whose parents migrate | 1 = Yes, 0 = No | 0.51 | 0.50 | 0 | 1 |
| Migrant children left-behind | 1 = Yes, 0 = No | 0.18 | 0.38 | 0 | 1 |
| Migrant children not left-behind | 1 = Yes, 0 = No | 0.33 | 0.47 | 0 | 1 |
| Moderator Variables | |||||
| Mobile phone addiction | The higher the score, the more severe mobile phone addiction | 48.82 | 15.91 | 22 | 110 |
| Control Variables | |||||
| Gender of child | 1 = male, 0 = female | 0.50 | 0.50 | 0 | 1 |
| Age of child | Years | 11.70 | 1.01 | 9 | 15 |
| Siblings | 1 = Yes, 0 = No | 0.46 | 0.50 | 0 | 1 |
| Boarding | 1 = Yes, 0 = No | 0.02 | 0.14 | 0 | 1 |
| Nutritious lunch | 1 = Yes, 0 = No | 0.81 | 0.39 | 0 | 1 |
| Age of guardian | Years | 40.85 | 7.62 | 30 | 81 |
| Guardian educational attainment | Years | 9.14 | 2.52 | 0 | 22 |
| Personality of guardians | |||||
| Conscientiousness | Measured by the Big Five Personality Scale | 11.28 | 2.52 | 3 | 15 |
| Agreeableness | Measured by the Big Five Personality Scale | 11.10 | 2.57 | 3 | 15 |
| Emotional stability | Measured by the Big Five Personality Scale | 7.70 | 2.54 | 3 | 15 |
| Extroversion | Measured by the Big Five Personality Scale | 9.87 | 2.61 | 3 | 15 |
| Openness | Measured by the Big Five Personality Scale | 9.73 | 3.16 | 3 | 15 |
| Nutritional knowledge | The higher the score, the greater the knowledge of nutritional intakes | 50.40 | 6.36 | 32 | 68 |
| Distance from home to school | km | 2.43 | 3.61 | 0.1 | 30 |
| Annual family income | 10,000 yuan | 4.57 | 3.76 | 1 | 20 |
| Variables | NMC a | PMC b | Diff e | MC-LBC c | Diff e | MC-NLBC d | Diff e |
|---|---|---|---|---|---|---|---|
| n = 405 | n = 421 | n = 145 | n = 276 | ||||
| (1) | (2) | (3) = (2) − (1) | (4) | (5) = (3) − (1) | (6) | (7) = (6) − (1) | |
| Anchored self-rated health | 3.8 | 3.63 | −0.17 ** | 3.55 | −0.25 ** | 3.67 | −0.13 |
| CES-D score | 15.96 | 17.64 | 1.68 ** | 18.87 | 2.91 *** | 16.99 | 1.03 |
| Depression severity | 0.72 | 0.87 | 0.16 ** | 0.94 | 0.23 ** | 0.84 | 0.12 |
| Chinese ranking | 2.91 | 3.17 | 0.26 *** | 3.04 | 0.14 | 3.24 | 0.33 *** |
| Mathematics ranking | 2.94 | 3.14 | 0.20 *** | 3.19 | 0.25 * | 3.11 | 0.17 |
| English ranking | 2.96 | 3.12 | 0.16 | 3.21 | 0.25 * | 3.07 | 0.11 |
| Variables | Physical Health | Mental Health | Cognitive Ability | ||||
|---|---|---|---|---|---|---|---|
| Anchored Self-Rated Health | Depression Level | Chinese Ranking | Mathematics Ranking | English Ranking | |||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Children whose parents migrate | −0.24 *** | −1.08 *** | 0.22 *** | 1.38 *** | 1.00 | 2.20 *** | 1.11 *** |
| (0.02) | (0.24) | (0.02) | (0.21) | (0.69) | (0.60) | (0.35) | |
| Migrant children not left-behind | 0.20 *** | 0.20 *** | −0.04 | −0.04 | −0.25 *** | −0.14 *** | −0.04 *** |
| (0.02) | (0.02) | (0.05) | (0.05) | (0.02) | (0.03) | (0.01) | |
| Mobile phone addiction | −0.17 *** | −0.28 *** | 1.00 *** | 1.16 *** | −0.45 *** | −0.30 *** | −0.41 *** |
| (0.06) | (0.01) | (0.11) | (0.05) | (0.03) | (0.04) | (0.02) | |
| Parental migration##Mobile phone addiction | 0.22 *** | −0.30 *** | −0.28 | −0.61 *** | −0.33 *** | ||
| (0.06) | (0.05) | (0.18) | (0.15) | (0.08) | |||
| Control variables | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Region dummies | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| School dummies | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Grade dummies | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 826 | 826 | 826 | 826 | 826 | 826 | 826 |
| Variables | BMI Abnormal | CES-D Score | Average Academic Ranking |
|---|---|---|---|
| Logit | OLS | Oprobit | |
| (1) | (2) | (3) | |
| Children whose parents migrate | −2.45 ** | 0.23 *** | 1.41 *** |
| (0.99) | (0.02) | (0.48) | |
| Migrant children not left-behind | 0.13 *** | −0.12 ** | −0.23 *** |
| (0.01) | (0.02) | (0.01) | |
| Mobile phone addiction | −0.31 *** | 0.63 *** | −0.49 *** |
| (0.10) | (0.03) | (0.01) | |
| Parental migration##Mobile phone addiction | 0.59 ** | −0.01 | −0.39 *** |
| (0.26) | (0.01) | (0.12) | |
| Control variables | Yes | Yes | Yes |
| Region dummies | Yes | Yes | Yes |
| School dummies | Yes | Yes | Yes |
| Grade dummies | Yes | Yes | Yes |
| Constant | 0.09 | 0.86 | |
| (1.13) | (0.44) | ||
| R-squared | 0.17 | ||
| Observations | 826 | 826 | 826 |
| Variables | BMI Abnormal | CES-D Score | Average Academic Ranking | |||
|---|---|---|---|---|---|---|
| Panel A: Child Gender | ||||||
| Boys | Girls | Boys | Girls | Boys | Girls | |
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Children whose parents migrate | −2.21 * | −1.96 ** | 0.23 *** | 0.15 ** | 1.12 *** | 1.60 *** |
| (1.21) | (0.99) | (0.02) | (0.02) | (0.17) | (0.56) | |
| Constant | −0.06 | 1.85 | 1.22 *** | 0.52 | ||
| (0.72) | (1.82) | (0.11) | (1.02) | |||
| Observations | 414 | 412 | 414 | 412 | 414 | 412 |
| R-squared | 0.16 | 0.23 | ||||
| Panel B: Family Income | ||||||
| High | Low | High | Low | High | Low | |
| Children whose parents migrate | −1.85 *** | −3.85 * | −0.48 | 0.57 ** | 1.61 *** | 1.47 |
| (0.56) | (2.25) | (0.25) | (0.07) | (0.17) | (1.02) | |
| Constant | 1.34 | 0.25 | 0.23 | 1.26 | ||
| (1.57) | (1.71) | (0.55) | (0.59) | |||
| Observations | 349 | 477 | 349 | 477 | 349 | 477 |
| R-squared | 0.25 | 0.14 | ||||
| Panel C: Nutrition Knowledge of Guardian | ||||||
| High | Low | High | Low | High | Low | |
| Children whose parents migrate | −1.56 ** | −3.54 *** | 0.44 | −0.05 | 1.24 *** | 1.15 *** |
| (0.78) | (0.74) | (0.32) | (0.18) | (0.40) | (0.34) | |
| Constant | 1.87 | 1.49 | 0.43 | 1.02 | ||
| (2.15) | (1.42) | (0.61) | (0.45) | |||
| Observations | 0.19 | 0.17 | ||||
| R-squared | 431 | 395 | 431 | 395 | 431 | 395 |
| Panel D: Education of Guardian | ||||||
| High | Low | High | Low | High | Low | |
| Children whose parents migrate | −1.56 | −2.72 ** | −1.02 ** | 0.61 ** | 4.96 *** | 0.37 |
| (1.47) | (1.23) | (0.23) | (0.09) | (1.23) | (1.02) | |
| Constant | −3.48 | 2.05 | 1.67 | 0.48 | ||
| (4.50) | (2.24) | (0.70) | (0.33) | |||
| Observations | 185 | 639 | 185 | 639 | 185 | 639 |
| R-squared | 0.29 | 0.16 | ||||
| Control variables | Yes | Yes | Yes | Yes | Yes | Yes |
| Region dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| School dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| Grade dummies | Yes | Yes | Yes | Yes | Yes | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, M.; Bian, B.; Zhu, W.; Huang, L. The Impact of Parental Migration on Multidimensional Health of Children in Rural China: The Moderating Effect of Mobile Phone Addiction. Children 2023, 10, 44. https://doi.org/10.3390/children10010044
Zhou M, Bian B, Zhu W, Huang L. The Impact of Parental Migration on Multidimensional Health of Children in Rural China: The Moderating Effect of Mobile Phone Addiction. Children. 2023; 10(1):44. https://doi.org/10.3390/children10010044
Chicago/Turabian StyleZhou, Mi, Biyu Bian, Weiming Zhu, and Li Huang. 2023. "The Impact of Parental Migration on Multidimensional Health of Children in Rural China: The Moderating Effect of Mobile Phone Addiction" Children 10, no. 1: 44. https://doi.org/10.3390/children10010044
APA StyleZhou, M., Bian, B., Zhu, W., & Huang, L. (2023). The Impact of Parental Migration on Multidimensional Health of Children in Rural China: The Moderating Effect of Mobile Phone Addiction. Children, 10(1), 44. https://doi.org/10.3390/children10010044






