Comparing Patient Characteristics, Clinical Outcomes, and Biomarkers of Severe Asthma Patients in Taiwan
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. Data Collection and Outcome Measurement
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berry, A.; Busse, W.W. Biomarkers in asthmatic patients: Has their time come to direct treatment? J. Allergy Clin. Immunol. 2016, 137, 1317–1324. [Google Scholar] [CrossRef]
- Asthma, G.I.F. Global Strategy for Asthma Managment and Prevention. 28 August 2020. 2020. Available online: https://ginasthma.org/wp-content/uploads/2020/06/GINA-2020-report_20_06_04-1-wms.pdf (accessed on 28 August 2020).
- Tiotiu, A. Biomarkers in asthma: State of the art. Asthma Res. Pract. 2018, 4, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Vijverberg, S.J.; Hilvering, B.; Raaijmakers, J.A.; Lammers, J.W.J.; Maitland-van der Zee, A.H.; Koenderman, L. Clinical utility of asthma biomarkers: From bench to bedside. Biol. Targets Ther. 2013, 7, 199. [Google Scholar]
- World Health Organization. Asthma. 6 September 2020. 2020. Available online: https://www.who.int/news-room/q-a-detail/asthma#:~:text=Asthma%20is%20the%20most%20common,people%20are%20living%20with%20asthma (accessed on 28 August 2020).
- Hsiao, H.J.; Wang, L.C.; Yang, Y.H.; Lee, J.H.; Yu, H.H.; Lin, Y.T.; Chiang, B.L. A nationwide survey of the severity, comorbidity, and mortality of hospitalized patients with asthma in Taiwan. Pediatr. Neonatol. 2013, 54, 254–260. [Google Scholar] [CrossRef][Green Version]
- Lai, C.K.; de Guia, T.S.; Kim, Y.-Y.; Kuo, S.-H.; Mukhopadhyay, A.; Soriano, J.B.; Trung, P.L.; Zhong, N.S.; Zainudin, N.; Zainudin, B. Asthma control in the Asia-Pacific region: The asthma insights and reality in Asia-Pacific study. J. Allergy Clin. Immunol. 2003, 111, 263–268. [Google Scholar] [CrossRef]
- Ma, Y.-C.; Lin, C.-C.; Yang, S.-Y.; Chen, H.-J.; Li, T.-C.; Lin, J.-G. Time trend analysis of the prevalence and incidence of diagnosed asthma and traditional Chinese medicine use among adults in Taiwan from 2000 to 2011: A population-based study. PLoS ONE 2015, 10, e0140318. [Google Scholar] [CrossRef]
- Sun, H.-L.; Lue, K.-H. Health care utilization and costs of adult asthma in Taiwan. Allergy Asthma Proc. 2008, 29, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Strimbu, K.; Tavel, J.A. What are biomarkers? Curr. Opin. HIV Aids 2010, 5, 463. [Google Scholar] [CrossRef]
- Medrek, S.; Parulekar, A.D.; Hanania, N.A. Predictive biomarkers for asthma therapy. Curr. Allergy Asthma Rep. 2017, 17, 69. [Google Scholar] [CrossRef]
- Seys, S.F.; Scheers, H.; Brande, P.V.D.; Marijsse, G.; Dilissen, E.; Bergh, A.V.D.; Goeminne, P.C.; Hellings, P.W.; Ceuppens, J.L.; Dupont, L.J.; et al. Cluster analysis of sputum cytokine-high profiles reveals diversity in T (h) 2-high asthma patients. Respir. Res. 2017, 18, 39. [Google Scholar] [CrossRef]
- Peters, M.; Mekonnen, Z.; Yuan, S.; Bhakta, N.R.; Woodruff, P.G.; Fahy, J.V. Measures of gene expression in sputum cells can identify TH2-high and TH2-low subtypes of asthma. J. Allergy Clin. Immunol. 2014, 133, 388–394.e5. [Google Scholar] [CrossRef]
- Dunican, E.M.; Fahy, J.V. The role of type 2 inflammation in the pathogenesis of asthma exacerbations. Ann. Am. Thorac. Soc. 2015, 12 (Suppl. 2), S144–S149. [Google Scholar] [PubMed]
- Price, D.B.; Bosnic-Anticevich, S.; Pavord, I.D.; Roche, N.; Halpin, D.M.; Bjermer, L.; Usmani, O.S.; Brusselle, G.; Ming, S.W.Y.; Rastogi, S. Association of elevated fractional exhaled nitric oxide concentration and blood eosinophil count with severe asthma exacerbations. Clin. Transl. Allergy 2019, 9, 41. [Google Scholar] [CrossRef]
- Saito, J.; Gibeon, D.; Macedo, P.; Menzies-Gow, A.; Bhavsar, P.K.; Chung, K.F. Domiciliary diurnal variation of exhaled nitric oxide fraction for asthma control. Eur. Respir. J. 2014, 43, 474–484. [Google Scholar] [CrossRef]
- Wang, Z.; Pianosi, P.; Keogh, K.; Zaiem, F.; Alsawas, M.; Alahdab, F.; Almasri, J.; Mohammed, K.; Larrea-Mantilla, L.; Farah, W.; et al. The Clinical Utility of Fractional Exhaled Nitric Oxide (FeNO) in Asthma Management; Report No.: 17(18)-EHC030-EF; Agency for Healthcare Research and Quality (US): Rockville, ML, USA, 2017.
- Malinovschi, A.; Janson, C.; Borres, M.; Alving, K. Simultaneously increased fraction of exhaled nitric oxide levels and blood eosinophil counts relate to increased asthma morbidity. J. Allergy Clin. Immunol. 2016, 138, 1301–1308.e2. [Google Scholar] [CrossRef] [PubMed]
- Parulekar, A.; Diamant, Z.; Hanania, N.A. Role of T2 inflammation biomarkers in severe asthma. Curr. Opin. Pulm. Med. 2016, 22, 59–68. [Google Scholar] [CrossRef]
- Wu, L.C.; Zarrin, A.A. The production and regulation of IgE by the immune system. Nat. Rev. Immunol. 2014, 14, 247–259. [Google Scholar] [CrossRef] [PubMed]
- Korevaar, D.A.; Westerhof, G.A.; Wang, J.; Cohen, J.F.; Spijker, R.; Sterk, P.J.; Bel, E.H.; Bossuyt, P.M.M. Diagnostic accuracy of minimally invasive markers for detection of airway eosinophilia in asthma: A systematic review and meta-analysis. Lancet Respir. Med. 2015, 3, 290–300. [Google Scholar] [CrossRef]
- Asthma, G.I.F. Global Strategy for Asthma Management and Prevention 2019. Available online: https://ginasthma.org/wp-content/uploads/2019/06/GINA-2019-main-report-June-2019-wms.pdf (accessed on 28 August 2020).
- Busse, W.W. Biological treatments for severe asthma: A major advance in asthma care. Allergol. Int. 2019, 68, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Castro, M.; Corren, J.; Pavord, I.D.; Maspero, J.; Wenzel, S.; Rabe, K.F.; Busse, W.W.; Ford, L.; Sher, L.; Fitzgerald, J.M.; et al. Dupilumab efficacy and safety in moderate-to-severe uncontrolled asthma. N. Engl. J. Med. 2018, 378, 2486–2496. [Google Scholar] [CrossRef]
- Ortega, H.G.; Yancey, S.W.; Mayer, B.; Gunsoy, N.B.; Keene, O.N.; Bleecker, E.R.; Brightling, C.E.; Pavord, I.D. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: A secondary analysis of the DREAM and MENSA studies. Lancet Respir. Med. 2016, 4, 549–556. [Google Scholar] [CrossRef]
- Ko, H.K.; Cheng, S.L.; Lin, C.H.; Lin, S.H.; Hsiao, Y.H.; Su, K.C.; Yu, C.J.; Wang, H.C.; Sheu, C.C.; Chiu, K.C.; et al. Blood tryptase and thymic stromal lymphopoietin levels predict the risk of exacerbation in severe asthma. Sci. Rep. 2021, 11, 8425. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, R.H.; Sidhu, S.S.; Raman, K.; Solon, M.; Solberg, O.D.; Caughey, G.H.; Woodruff, P.G.; Fahy, J.V. Accumulation of intraepithelial mast cells with a unique protease phenotype in T (H)2-high asthma. J. Allergy Clin. Immunol. 2010, 125, 1046–1053. [Google Scholar] [CrossRef] [PubMed]
- Kraft, M.; Martin, R.J.; Lazarus, S.C.; Fahy, J.V.; Boushey, H.A.; Lemanske, R.F., Jr.; Szefler, S.J. Asthma Clinical Research Network. Asthma Clinical Research Network. Airway tissue mast cells in persistent asthma: Predictor of treatment failure when patients discontinue inhaled corticosteroids. Chest 2003, 124, 42–50. [Google Scholar] [CrossRef]
| All Patients | No Exacerbations | Exacerbations > 1 | p-Value | |
|---|---|---|---|---|
| (n = 132) | (n = 80) | (n = 52) | ||
| n (%) | n (%) | n (%) | ||
| Age, mean ± SD | 61.47 ± 13.12 | 62.19 ± 13.39 | 60.37 ± 12.74 | 0.4377 |
| Gender | 0.7980 | |||
| Male | 50 (37.88) | 31 (38.75) | 19 (36.54) | |
| Female | 82 (62.12) | 49 (61.25) | 33 (63.46) | |
| BMI, mean ± SD | 25.43 ± 4.83 | 25 ± 4.74 | 26.07 ± 4.95 | 0.2150 |
| Smoking History | 34 (25.76) | 19 (23.75) | 15 (28.85) | 0.5130 |
| Allergic Rhinitis (AR) | 95 (71.97) | 60 (75) | 35 (67.31) | 0.3363 |
| Nasal Polyps | 4 (3.03) | 2 (2.5) | 2 (3.85) | 0.6464 |
| Hypertension | 60 (45.45) | 35 (43.75) | 25 (48.08) | 0.6257 |
| GERD | 23 (17.42) | 13 (16.25) | 10 (19.23) | 0.6591 |
| Heart Failure (HF) | 12 (9.09) | 7 (8.75) | 5 (9.62) | 1.0000 |
| DM | 27 (20.45) | 17 (21.25) | 10 (19.23) | 0.7787 |
| Atopic | 72 (54.55) | 49 (61.25) | 23 (44.23) | 0.0550 |
| FEV1, mean ± SD | 1.54 ± 0.7 | 1.54 ± 0.7 | 1.55 ± 0.71 | 0.9408 |
| FEV1%, mean ± SD | 66.93 ± 23.51 | 68.2 ± 23.98 | 64.97 ± 22.85 | 0.4425 |
| FEV1/FVC, mean ± SD | 66.86 ± 12.14 | 66.82 ± 12.8 | 66.93 ± 11.18 | 0.9599 |
| Exacerbation(s), mean ± SD | 0.73 ± 1.35 |
| All Patients | No Exacerbations | Exacerbations > 1 | p-Value | |
|---|---|---|---|---|
| (n = 132) | (n = 80) | (n = 52) | ||
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| IL-5 | 2.42 ± 1.58 | 2.35 ± 1.37 | 2.53 ± 1.87 | 0.5603 |
| IL-13 | 59.37 ± 28.32 | 61.33 ± 25.7 | 56.39 ± 31.92 | 0.3528 |
| Tryptase | 1881.54 ± 2715.44 | 2270.33 ± 3228.42 | 1283.41 ± 1480.97 | 0.0191 |
| Periostin | 16.26 ± 10.43 | 15.56 ± 10.13 | 17.36 ± 10.9 | 0.3396 |
| IL-8 | 15.94 ± 52.69 | 18.81 ± 66.55 | 11.41 ± 12.99 | 0.3403 |
| IL-17 | 12.59 ± 4.4 | 12.68 ± 4.8 | 12.44 ± 3.76 | 0.7565 |
| TGF Beta | 30.81 ± 23.56 | 28.25 ± 15.3 | 34.86 ± 32.4 | 0.1816 |
| TNF Alpha | 6.17 ± 18.95 | 4.5 ± 11.23 | 8.87 ± 27.08 | 0.2865 |
| VEGF | 338.67 ± 296.96 | 346.33 ± 333.07 | 327.04 ± 234.27 | 0.6980 |
| PIGF | 7.31 ± 6.7 | 7.85 ± 7.23 | 6.47 ± 5.74 | 0.2563 |
| TSLP | 13.98 ± 14.33 | 11.59 ± 14.15 | 17.76 ± 13.93 | 0.0166 |
| IL-33 | 3.87 ± 4.24 | 4.01 ± 4.96 | 3.67 ± 2.85 | 0.6191 |
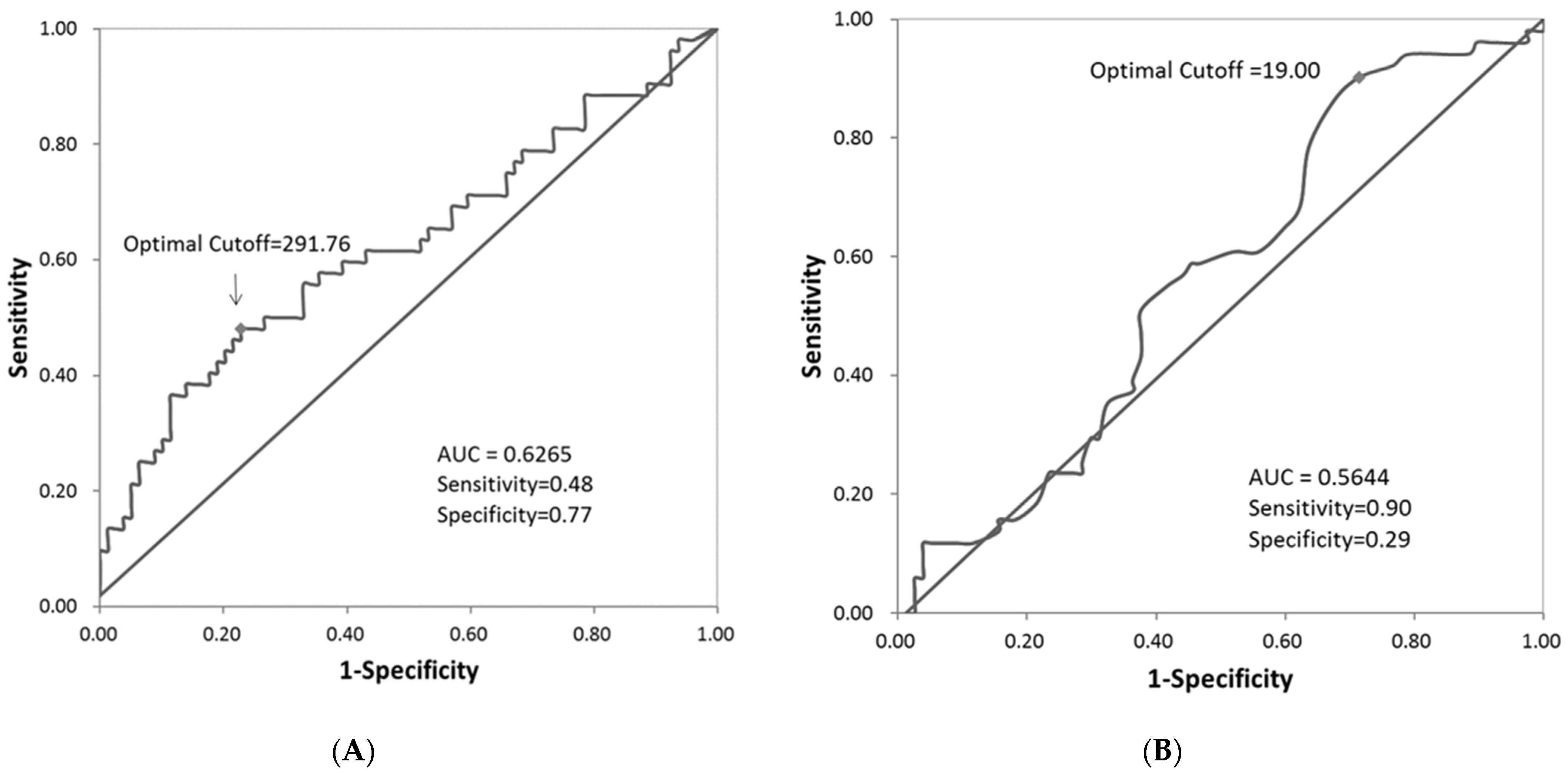
| EOS | 272.67 ± 272.91 | 210.05 ± 175.24 | 367.8 ± 357.18 | 0.0043 |
| FeNO | 34.12 ± 23.08 | 32.77 ± 22.99 | 36.16 ± 23.29 | 0.4190 |
| IgE Levels | 241.26 ± 331.20 | 239.13 ± 321.43 | 244.52 ± 348.84 | 0.9283 |
| All Patients | No Exacerbations | Exacerbations > 1 | p-Value | |
|---|---|---|---|---|
| (n = 132) | (n = 80) | (n = 52) | ||
| n (%) | n (%) | n (%) | ||
| Eosinophils Count | 0.0029 | |||
| <300 | 90 (68.70) | 62 (78.48) | 28 (53.85) | |
| ≥300 | 41 (31.30) | 17 (21.52) | 24 (46.15) | |
| missing | 1 | 1 | ||
| FeNO Measure | 0.0165 | |||
| <20 | 32 (25.00) | 25 (32.47) | 7 (13.73) | |
| ≥20 | 96 (75.00) | 52 (67.53) | 44 (86.27) | |
| missing | 4 | 3 | 1 | |
| IgE Levels | 0.9733 | |||
| <100 | 63 (48.84) | 38 (48.72) | 25 (49.02) | |
| ≥100 | 66 (51.16) | 40 (51.28) | 26 (50.98) | |
| missing | 3 | 2 | 1 |
| All Patients | No Exacerbations | Exacerbations > 1 | p-Value | |
|---|---|---|---|---|
| (n = 132) | (n = 80) | (n = 52) | ||
| n (%) | n (%) | n (%) | ||
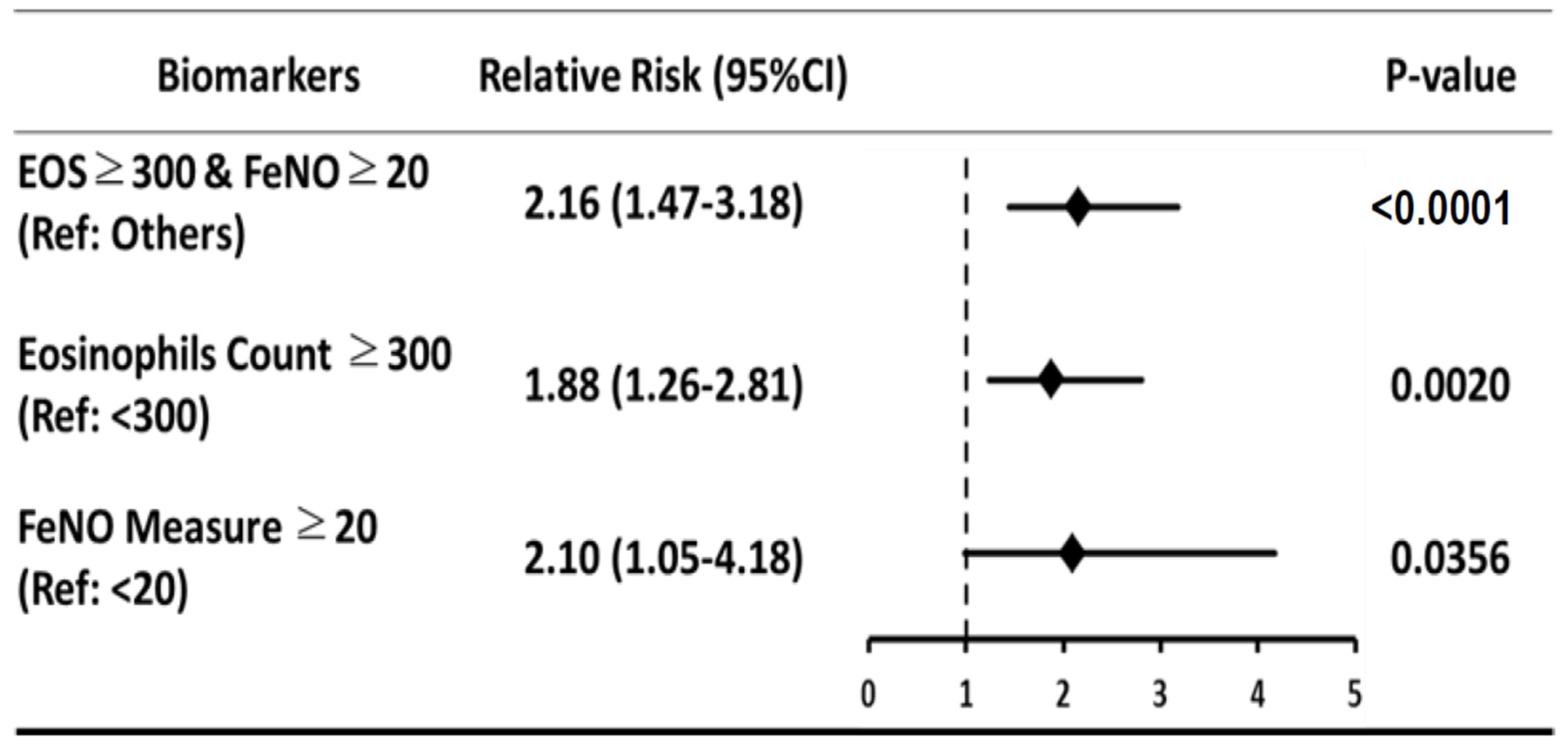
| Biomarker group #1 | 0.0019 | |||
| EOS <300 & FeNO < 20 | 26 (20.47) | 20 (26.32) | 6 (11.76) | |
| EOS ≥300 & FeNO < 20 | 6 (4.72) | 5 (6.58) | 1 (1.96) | |
| EOS <300 & FeNO ≥ 20 | 62 (48.82) | 40 (52.63) | 22 (43.14) | |
| EOS ≥300 & FeNO ≥ 20 | 33 (25.98) | 11 (14.47) | 22 (43.14) | |
| Missing | ||||
| Biomarker group #2 | <0.0001 | |||
| EOS ≥300 & FeNO ≥20 | 33 (20.47) | 11 (14.47) | 22 (43.14) | |
| Others | 94 (79.53) | 65 (85.53) | 29 (56.86) | |
| Missing | 5 | 4 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, S.-L.; Chiu, K.-C.; Ko, H.-K.; Perng, D.-W.; Wang, H.-C.; Yu, C.-J.; Sheu, C.-C.; Lin, S.-H.; Lin, C.-H. Comparing Patient Characteristics, Clinical Outcomes, and Biomarkers of Severe Asthma Patients in Taiwan. Biomedicines 2021, 9, 764. https://doi.org/10.3390/biomedicines9070764
Cheng S-L, Chiu K-C, Ko H-K, Perng D-W, Wang H-C, Yu C-J, Sheu C-C, Lin S-H, Lin C-H. Comparing Patient Characteristics, Clinical Outcomes, and Biomarkers of Severe Asthma Patients in Taiwan. Biomedicines. 2021; 9(7):764. https://doi.org/10.3390/biomedicines9070764
Chicago/Turabian StyleCheng, Shih-Lung, Kuo-Chin Chiu, Hsin-Kuo Ko, Diahn-Warng Perng, Hao-Chien Wang, Chong-Jen Yu, Chau-Chyun Sheu, Sheng-Hao Lin, and Ching-Hsiung Lin. 2021. "Comparing Patient Characteristics, Clinical Outcomes, and Biomarkers of Severe Asthma Patients in Taiwan" Biomedicines 9, no. 7: 764. https://doi.org/10.3390/biomedicines9070764
APA StyleCheng, S.-L., Chiu, K.-C., Ko, H.-K., Perng, D.-W., Wang, H.-C., Yu, C.-J., Sheu, C.-C., Lin, S.-H., & Lin, C.-H. (2021). Comparing Patient Characteristics, Clinical Outcomes, and Biomarkers of Severe Asthma Patients in Taiwan. Biomedicines, 9(7), 764. https://doi.org/10.3390/biomedicines9070764






