Antibody-Based Immunotoxins for Colorectal Cancer Therapy
Abstract
1. Introduction
2. Immunotoxin Development
3. Cytotoxic, Non-Human Moieties
3.1. Bacterial and Plant Toxins
3.2. Fungal Ribotoxins
4. Human Cytotoxic Proteins
4.1. RNases
4.2. Microtubule-Associated Protein Tau (MAP-Tau)
4.3. Granzyme B
4.4. Granulysin
5. Targets in CRC
5.1. LewisY
5.2. CEA
5.3. EpCAM
5.4. Muc-1/Tn
5.5. GPA33
5.6. EGFR
6. Antibody-Based Immunotoxins in CRC Clinical Trials
6.1. Ricin-Based Immunotoxins
6.1.1. Ricin-Based ITX Targeting p72
6.1.2. Ricin-Based ITX Targeting CEA
6.2. PE-Based Immunotoxins
6.2.1. PE-Based ITX Targeting Anti-Lewis Y
6.2.2. PE-Based ITX Targeting EpCAM
6.2.3. PE-Based ITX Targeting Muc-1
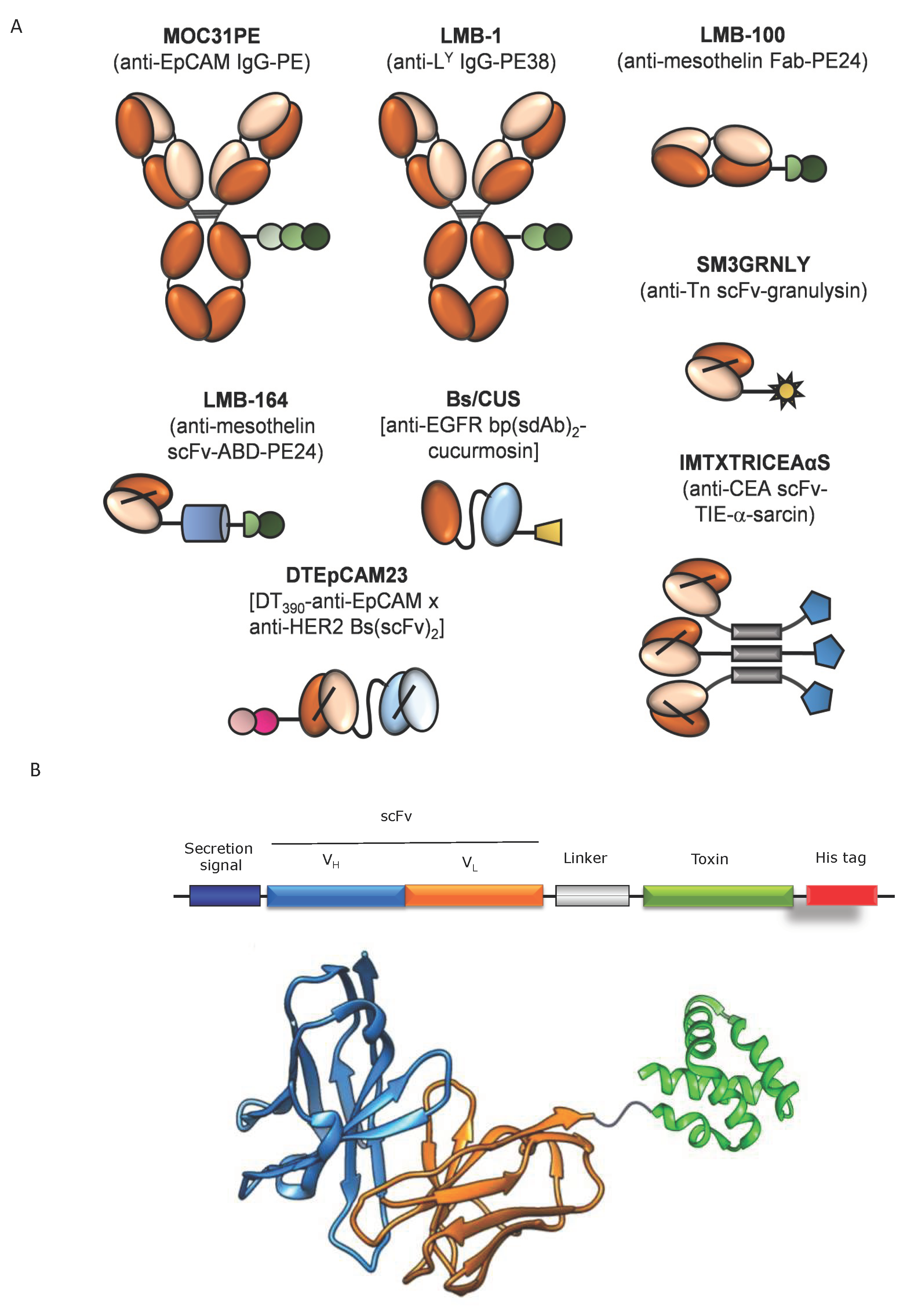
7. Antibody Fragment-Based Immunotoxins in CRC: Preclinical Developments
7.1. PE-Based Immunotoxins
7.1.1. PE-Based ITX Targeting CEA
7.1.2. PE-Based ITX Targeting CD71 (Transferrin Receptor 1)
7.1.3. PE-Based ITX Targeting Mesothelin
7.1.4. PE-Based ITX Targeting CD25
7.2. α-Sarcin-Based Immunotoxins
7.2.1. α-Sarcin-Based ITX Targeting GPA33
7.2.2. α-Sarcin-Based ITX Targeting CEA
7.3. Granulysin-Based Immunotoxins
7.3.1. Granulysin-Based ITX Targeting CEA
7.3.2. Granulysin-Based ITX Targeting the Tn Antigen
7.4. Cholera Exotoxin-Based Immunotoxin
7.5. Cucurmosin-Based Immunotoxin
8. Challenges and Future Directions in ITX Design
8.1. Immunogenicity of the Toxin Portion
8.2. Endosomal Retention of Toxins
8.3. Short Half–Life
8.4. Bispecific Immunotoxins
8.5. Gene Therapy for Immunotoxin In Vivo Production
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Biller, L.; Schrag, D. Diagnosis and Treatment of Metastatic Colorectal Cancer: A Review. JAMA 2021, 325, 669–685. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Chen, Y.; Fang, J. Comprehensive review of targeted therapy for colorectal cancer. Signal Transduct. Target. Ther. 2020, 5, 22. [Google Scholar] [CrossRef]
- Wilson, C.; Tolias, P. Recent advances in cancer drug discovery targeting RAS. Drug Discov. Today 2016, 21, 1915–1919. [Google Scholar] [CrossRef]
- Catalano, I.; Trusolino, L. The Stromal and Immune Landscape of Colorectal Cancer Progression during Anti-EGFR Therapy. Cancer Cell 2019, 36, 1–3. [Google Scholar] [CrossRef]
- Le, D.; Durham, J.; Smith, K.; Wang, H.; Bartlett, B.; Aulakh, L.; Lu, S.; Kemberling, H.; Wilt, C.; Luber, B.; et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science 2017, 357, 409–413. [Google Scholar] [CrossRef]
- Smaglo, B.; Aldeghaither, D.; Weiner, L. The development of immunoconjugates for targeted cancer therapy. Nat. Rev. Clin. Oncol. 2014, 11, 637–648. [Google Scholar] [CrossRef] [PubMed]
- Zuppone, S.; Fabbrini, M.; Vago, R. Hosts for Hostile Protein Production: The Challenge of Recombinant Immunotoxin Expression. Biomedicines 2019, 7, 38. [Google Scholar] [CrossRef]
- Hamamichi, S.; Fukuhara, T.; Hattori, N. Immunotoxin Screening System: A Rapid and Direct Approach to Obtain Functional Antibodies with Internalization Capacities. Toxins 2020, 12, 658. [Google Scholar] [CrossRef] [PubMed]
- Antignani, A.; Ho, E.; Bilotta, M.; Qiu, R.; Sarnvosky, R.; FitzGerald, D. Targeting Receptors on Cancer Cells with Protein Toxins. Biomolecules 2020, 10, 1331. [Google Scholar] [CrossRef]
- Thorpe, P.; Ross, W.; Cumber, A.; Hinson, C.; Edwards, D.; Davies, A. Toxicity of diphtheria toxin for lymphoblastoid cells is increased by conjugation to antilymphocytic globulin. Nature 1978, 271, 752–755. [Google Scholar] [CrossRef]
- Thorpe, P.; Mason, D.; Brown, A.; Simmonds, S.; Ross, W.; Cumber, A.; Forrester, J. Selective killing of malignant cells in a leukaemic rat bone marrow using an antibody-ricin conjugate. Nature 1982, 297, 594–596. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, D.; Waldmann, T.; Willingham, M.; Pastan, I. Pseudomonas exotoxin-anti-TAC. Cell-specific immunotoxin active against cells expressing the human T cell growth factor receptor. J. Clin. Investig. 1984, 74, 966–971. [Google Scholar] [CrossRef]
- Chaudhary, V.; Queen, C.; Junghans, R.; Waldmann, T.; FitzGerald, D.; Pastan, I. A recombinant immunotoxin consisting of two antibody variable domains fused to Pseudomonas exotoxin. Nature 1989, 339, 394–397. [Google Scholar] [CrossRef] [PubMed]
- Kreitman, R.; Dearden, C.; Zinzani, P.; Delgado, J.; Karlin, L.; Robak, T.; Gladstone, D.; le Coutre, P.; Dietrich, S.; Gotic, M.; et al. Moxetumomab pasudotox in relapsed/refractory hairy cell leukemia. Leukemia 2018, 32, 1768–1777. [Google Scholar] [CrossRef]
- Pastan, I.; Hassan, R.; Fitzgerald, D.; Kreitman, R. Immunotoxin therapy of cancer. Nat. Rev. Cancer 2006, 6, 559–565. [Google Scholar] [CrossRef]
- Pastan, I.; Hassan, R.; FitzGerald, D.; Kreitman, R. Immunotoxin treatment of cancer. Annu. Rev. Med. 2007, 58, 221–237. [Google Scholar] [CrossRef]
- Kim, J.; Jun, S.; Kim, Y. Critical Issues in the Development of Immunotoxins for Anticancer Therapy. J. Pharm. Sci. 2020, 109, 104–115. [Google Scholar] [CrossRef]
- Becker, N.; Benhar, I. Antibody-Based Immunotoxins for the Treatment of Cancer. Antibodies 2012, 1, 39–69. [Google Scholar] [CrossRef]
- Chowdhury, P.; Viner, J.; Beers, R.; Pastan, I. Isolation of a high-affinity stable single-chain Fv specific for mesothelin from DNA-immunized mice by phage display and construction of a recombinant immunotoxin with anti-tumor activity. Proc. Natl. Acad. Sci. USA 1998, 95, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Deckert, P. Current constructs and targets in clinical development for antibody-based cancer therapy. Curr. Drug Targets 2009, 10, 158–175. [Google Scholar] [CrossRef]
- Sanz, L.; Kristensen, P.; Blanco, B.; Facteau, S.; Russell, S.; Winter, G.; Alvarez-Vallina, L. Single-chain antibody-based gene therapy: Inhibition of tumor growth by in situ production of phage-derived human antibody fragments blocking functionally active sites of cell-associated matrices. Gene Ther. 2002, 9, 1049–1053. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Akbari, B.; Farajnia, S.; Khosroshahi, S.; Safari, F.; Yousefi, M.; Dariushnejad, H.; Rahbarnia, L. Immunotoxins in cancer therapy: Review and update. Int. Rev. Immunol. 2017, 36, 207–219. [Google Scholar]
- Mazor, R.; Onda, M.; Pastan, I. Immunogenicity of therapeutic recombinant immunotoxins. Immunol. Rev. 2016, 270, 152–164. [Google Scholar] [PubMed]
- Hlongwane, P.; Mungra, N.; Madheswaran, S.; Akinrinmade, O.; Chetty, S.; Barth, S. Human Granzyme B Based Targeted Cytolytic Fusion Proteins. Biomedicines 2018, 6, E72. [Google Scholar] [PubMed]
- Mathew, M.; Verma, R. Humanized immunotoxins: A new generation of immunotoxins for targeted cancer therapy. Cancer Sci. 2009, 100, 1359–1365. [Google Scholar] [PubMed]
- Mungra, N.; Jordaan, S.; Hlongwane, P.; Naran, K.; Chetty, S.; Barth, S. Targeted human cytolytic fusion proteins at the cutting edge: Harnessing the apoptosis-inducing properties of human enzymes for the selective elimination of tumor cells. Oncotarget 2019, 10, 897–915. [Google Scholar] [CrossRef]
- Guerrero-Ochoa, P.; Aguilar-Machado, D.; Ibáñez-Pérez, R.; Macías-León, J.; Hurtado-Guerrero, R.; Raso, J.; Anel, A. Production of a Granulysin-Based, Tn-Targeted Cytolytic Immunotoxin Using Pulsed Electric Field Technology. Int. J. Mol. Sci. 2020, 21, 6165. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez-Pérez, R.; Guerrero-Ochoa, P.; Al-Wasaby, S.; Navarro, R.; Tapia-Galisteo, A.; De Miguel, D.; Gonzalo, O.; Conde, B.; Martínez-Lostao, L.; Hurtado-Guerrero, R.; et al. Anti-tumoral potential of a human granulysinbased, CEA-targeted cytolytic immunotoxin. OncoImmunol 2019, 8, 1641392. [Google Scholar]
- Lu, J.; Zhu, Z.; Zheng, Y.; Shaw, P. Engineering of Ribosome-inactivating Proteins for Improving Pharmacological Properties. Toxins 2020, 12, 167. [Google Scholar] [CrossRef] [PubMed]
- Bortolotti, M.; Bolognesi, A.; Polito, L. Bouganin, an Attractive Weapon for Immunotoxins. Toxins 2018, 10, 323. [Google Scholar] [CrossRef]
- Giansanti, F.; Flavell, D.; Angelucci, F.; Fabbrini, M.; Ippoliti, R. Strategies to Improve the Clinical Utility of Saporin-Based Targeted Toxins. Toxins 2018, 10, 82. [Google Scholar] [CrossRef] [PubMed]
- Knödler, M.; Buyel, J. Plant-made immunotoxin building blocks: A roadmap for producing therapeutic antibody-toxin fusions. Biotechnol. Adv. 2021, 47, 107683. [Google Scholar] [CrossRef]
- Lacadena, J.; Alvarez-García, E.; Carreras-Sangrà, N.; Herrero-Galán, E.; Alegre-Cebollada, J.; García-Ortega, L.; Oñaderra, M.; Gavilanes, J.; Martínez del Pozo, A. Fungal ribotoxins: Molecular dissection of a family of natural killers. FEMS Microbiol. Rev. 2007, 31, 212–237. [Google Scholar] [CrossRef]
- Olombrada, M.; Lázaro-Gorines, R.; López-Rodríguez, J.; Martínez-Del-Pozo, Á.; Oñaderra, M.; Maestro-López, M.; Lacadena, J.; Gavilanes, J.; García-Ortega, L. Fungal Ribotoxins: A Review of Potential Biotechnological Applications. Toxins 2017, 9, 71. [Google Scholar] [CrossRef]
- De Lorenzo, C.; D’Alessio, G. From immunotoxins to immunoRNases. Curr. Pharm. Biotechnol. 2008, 9, 210–214. [Google Scholar] [CrossRef]
- Krauss, J.; Arndt, M.; Dübel, S.; Rybak, S. Antibody-targeted RNase fusion proteins (immunoRNases) for cancer therapy. Curr. Pharm. Biotechnol. 2008, 9, 231–234. [Google Scholar] [CrossRef]
- Jordaan, S.; Akinrinmade, O.; Nachreiner, T.; Cremer, C.; Naran, K.; Chetty, S.; Barth, S. Updates in the Development of ImmunoRNases for the Selective Killing of Tumor Cells. Biomedicines 2018, 6, 28. [Google Scholar] [CrossRef] [PubMed]
- Menzel, C.; Schirrmann, T.; Konthur, Z.; Jostock, T.; Dübel, S. Human antibody RNase fusion protein targeting CD30+ lymphomas. Blood 2008, 111, 3830–3837. [Google Scholar] [CrossRef]
- D’Avino, C.; Palmieri, D.; Braddom, A.; Zanesi, N.; James, C.; Cole, S.; Salvatore, F.; Croce, C.; De Lorenzo, C. A novel fully human anti-NCL immunoRNase for triple-negative breast cancer therapy. Oncotarget 2016, 7, 87016–87030. [Google Scholar] [CrossRef] [PubMed]
- Daniels, T.; Delgado, T.; Rodriguez, J.; Helguera, G.; Penichet, M. The transferrin receptor part I: Biology and targeting with cytotoxic antibodies for the treatment of cancer. Clin. Immunol. 2006, 121, 144–158. [Google Scholar] [CrossRef]
- Yoon, J.; Han, S.; Kown, O.; Kim, S.; Park, M.; Kim, B. Cloning and cytotoxicity of fusion proteins of EGF and angiogenin. Life Sci. 1999, 64, 1435–1445. [Google Scholar] [CrossRef]
- Arndt, M.; Krauss, J.; Vu, B.; Newton, D.; Rybak, S. A dimeric angiogenin immunofusion protein mediates selective toxicity toward CD22+ tumor cells. J. Immunother. 2005, 28, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Cremer, C.; Vierbuche, T.; Hein, L.; Fischer, R.; Barth, S.; Nachreiner, T. Angiogenin mutants as novel effector molecules for the generation of fusion proteins with increased cytotoxic potential. J. Immunother. 2015, 38, 85–95. [Google Scholar] [CrossRef]
- Gotte, G.; Menegazzi, M. Biological Activities of Secretory RNases: Focus on Their Oligomerization to Design Antitumor Drugs. Front. Immunol. 2019, 10, 2626. [Google Scholar] [CrossRef] [PubMed]
- Strong, L.; Kink, J.; Mei, B.; Shahan, M.; Raines, R. First in human phase I clinical trial of QBI-139, a human ribonuclease variant, in solid tumors. J. Clin. Oncol. 2012, 30, TPS3113. [Google Scholar] [CrossRef]
- Wezler, X.; Dübel, S.; Schirrmann, T. Antibody fusion proteins with human ribonucleases 1 to 8. Hum. Antibodies 2018, 26, 177–192. [Google Scholar] [CrossRef]
- Weidle, U.; Schneider, B.; Georges, G.; Brinkmann, U. Genetically engineered fusion proteins for treatment of cancer. Cancer Genom. Proteom. 2012, 9, 357–372. [Google Scholar]
- Hristodorov, D.; Mladenov, R.; Pardo, A.; Pham, A.; Huhn, M.; Fischer, R.; Thepen, T.; Barth, S. Microtubule-associated protein tau facilitates the targeted killing of proliferating cancer cells in vitro and in a xenograft mouse tumour model in vivo. Br. J. Cancer 2013, 109, 1570–1578. [Google Scholar] [CrossRef]
- Hristodorov, D.; Amoury, M.; Mladenov, R.; Niesen, J.; Arens, K.; Berges, N.; Hein, L.; Di Fiore, S.; Pham, A.; Huhn, M.; et al. EpCAM-selective elimination of carcinoma cells by a novel MAP-based cytolytic fusion protein. Mol. Cancer Ther. 2014, 13, 2194–2202. [Google Scholar] [CrossRef] [PubMed]
- Amoury, M.; Mladenov, R.; Nachreiner, T.; Pham, A.; Hristodorov, D.; Di Fiore, S.; Helfrich, W.; Pardo, A.; Fey, G.; Schwenkert, M. A novel approach for targeted elimination of CSPG4-positive triple-negative breast cancer cells using a MAP tau-based fusion protein. Int. J. Cancer 2016, 139, 916–927. [Google Scholar] [CrossRef]
- Martinez-Lostao, L.; Anel, A.; Pardo, J. How Do Cytotoxic Lymphocytes Kill Cancer Cells? Clin. Cancer Res. 2015, 21, 5047–5056. [Google Scholar] [CrossRef]
- Pardo, J.; Wallich, R.; Martin, P.; Urban, C.; Rongvaux, A.; Flavell, R.A.; Müllbacher, A.; Borner, C.; Simon, M.M. Granzyme B-induced cell death exerted by ex-vivo CTL: Discriminating requirements for cell death and some of its signs. Cell Death Differ. 2008, 15, 567–579. [Google Scholar] [CrossRef]
- Darmon, A.J.; Nicholson, D.W.; Bleackley, R.C. Activation of the apoptotic protease CPP32 by cytotoxic T-cell-derived granzyme B. Nature 1995, 377, 446–448. [Google Scholar] [CrossRef] [PubMed]
- Pardo, J.; Aguiló, J.; Anel, A.; Martin, P.; Joeckel, L.; Borner, C.; Wallich, R.; Müllbacher, A.; Froelich, C.; Simon, M. The biology of cytotoxic cell granule exocytosis pathway: Granzymes have evolved to induce cell death and inflammation. Microbes Infect. 2009, 11, 452–459. [Google Scholar] [CrossRef]
- Voskoboinik, I.; Whisstock, J.; Trapani, J. Perforin and granzymes: Function, dysfunction and human pathology. Nat. Rev. Immunol. 2015, 15, 388–400. [Google Scholar] [CrossRef] [PubMed]
- Froelich, C.J.; Oth, K.; Turbov, J.; Seth, P.; Gottlieb, R.; Babior, B.; Shah, G.M.; Bleackley, R.C.; Dixit, V.M.; Hanna, W. New paradigm for lymphocyte granule-mediated cytotoxicity. Target cells bind and internalize granzyme B, but an endosomolytic agent is necessary for cytosolic delivery and subsequent apoptosis. J. Biol. Chem. 1996, 271, 29073–29079. [Google Scholar] [CrossRef] [PubMed]
- Niesen, J.; Hehmann-Titt, G.; Woitok, M.; Fendel, R.; Barth, S.; Fischer, R.; Stein, C. A novel fully-human cytolytic fusion protein based on granzyme B shows in vitro cytotoxicity and ex vivo binding to solid tumors overexpressing the epidermal growth factor receptor. Cancer Lett. 2016, 374, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Clayberger, C.; Krensky, A.M. Granulysin. Curr. Opin. Immunol. 2003, 15, 560–565. [Google Scholar] [CrossRef]
- Dotiwala, F.; Mulik, S.; Polidoro, R.; Ansara, J.; Burleigh, B.; Walch, M.; Gazzinelli, R.; Lieberman, J. Killer lymphocytes use granulysin, perforin and granzymes to kill intracellular parasites. Nat. Med. 2016, 22, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Stenger, S.; Hanson, D.A.; Teitelbaum, R.; Dewan, P.; Niazi, K.R.; Froelich, C.J.; Ganz, T.; Thoma-Uszynski, S.; Melián, A.; Bogdan, C.; et al. An antimicrobial activity of cytolytic T cells mediated by granulysin. Science 1998, 282, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Aporta, A.; Catalán, E.; Galán-Malo, P.; Ramírez-Labrada, A.; Pérez, M.; Azaceta, G.; Palomera, L.; Naval, J.; Marzo, I.; Pardo, J.; et al. Granulysin induces apoptotic cell death and cleavage of the autophagy regulator Atg5 in human hematological tumors. Biochem. Pharmacol. 2014, 87, 410–423. [Google Scholar] [CrossRef] [PubMed]
- Gamen, S.; Hanson, D.A.; Kaspar, A.; Naval, J.; Krensky, A.M.; Anel, A. Granulysin-induced apoptosis. I. Involvement of at least two distinct pathways. J. Immunol. 1998, 161, 1758–1764. [Google Scholar]
- Peña, S.V.; Hanson, D.A.; Carr, B.A.; Goralski, T.J.; Krensky, A.M. Processing, subcellular localization, and function of 519 (granulysin), a human late T cell activation molecule with homology to small, lytic, granule proteins. J. Immunol. 1997, 158, 2680–2688. [Google Scholar] [PubMed]
- Anderson, D.H.; Sawaya, M.R.; Cascio, D.; Ernst, W.; Modlin, R.L.; Krensky, A.M.; Eisenberg, D. Granulysin crystal structure and a structure-derived lytic mechanism. J. Mol. Biol. 2003, 325, 355–365. [Google Scholar] [CrossRef]
- Barman, H.; Walch, M.; Latinovic-Golic, S.; Dumrese, C.; Dolder, M.; Groscurth, P.; Ziegler, U. Cholesterol in Negatively Charged Lipid Bilayers Modulates the Effect of the Antimicrobial Protein Granulysin. J. Membr. Biol. 2006, 212, 29–39. [Google Scholar] [CrossRef]
- Kaspar, A.A.; Okada, S.; Kumar, J.; Poulain, F.R.; Drouvalakis, K.A.; Kelekar, A.; Hanson, D.A.; Kluck, R.M.; Hitoshi, Y.; Johnson, D.E.; et al. A distinct pathway of cell-mediated apoptosis initiated by granulysin. J. Immunol. 2001, 167, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Lostao, L.; de Miguel, D.; Al-Wasaby, S.; Gallego-Lleyda, A.; Anel, A. Death ligands and granulysin: Mechanisms of tumor cell death induction and therapeutic opportunities. Immunotherapy 2015, 7, 883–892. [Google Scholar] [CrossRef] [PubMed]
- Pardo, J.; Pérez-Galán, P.; Gamen, S.; Marzo, I.; Monleón, I.; Kaspar, A.A.; Susín, S.A.; Kroemer, G.; Krensky, A.M.; Naval, J.; et al. A role of the mitochondrial apoptosis-inducing factor (AIF) in granulysin-induced apoptosis. J. Immunol. 2001, 167, 1222–1229. [Google Scholar] [CrossRef]
- Al-Wasaby, S.; de Miguel, D.; Aporta, A.; Naval, J.; Conde, B.; Martínez-Lostao, L.; Anel, A. In vivo potential of recombinant granulysin against human tumors. OncoImmunology 2015, 4, e1036213. [Google Scholar] [CrossRef]
- Al-Wasaby, S.; Guerrero-Ochoa, P.; Ibáñez-Pérez, R.; Soler, R.; Conde, B.; Martínez-Lostao, L.; Anel, A. In vivo potential of recombinant granulysin against human melanoma. Cancer Treat. Res. Commun. 2021, 27, 100355. [Google Scholar] [CrossRef]
- Pinho, S.; Reis, C. Glycosylation in cancer: Mechanisms and clinical implications. Nat. Rev. Cancer 2015, 15, 540–555. [Google Scholar] [CrossRef]
- Westwood, J.; Murray, W.; Trivett, M.; Haynes, N.; Solomon, B.; Mileshkin, L.; Ball, D.; Michael, M.; Burman, A.; Mayura-Guru, P.; et al. The Lewis-Y carbohydrate antigen is expressed by many human tumors and can serve as a target for genetically redirected T cells despite the presence of soluble antigen in serum. J. Immunother. 2009, 32, 292–301. [Google Scholar] [CrossRef]
- Blanas, A.; Sahasrabudhe, N.; Rodríguez, E.; van Kooyk, Y.; van Vliet, S. Fucosylated Antigens in Cancer: An Alliance toward Tumor Progression, Metastasis, and Resistance to Chemotherapy. Front. Oncol. 2018, 8, 39. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhang, H.; Cordon-Cardo, C.; Reuter, V.; Singhal, A.; Lloyd, K.; Livingston, P. Selection of tumor antigens as targets for immune attack using immunohistochemistry: II. Blood group-related antigens. Int. J. Cancer 1997, 73, 50–56. [Google Scholar] [CrossRef]
- Scott, A.; Tebbutt, N.; Lee, F.; Cavicchiolo, T.; Liu, Z.; Gill, S.; Poon, A.; Hopkins, W.; Smyth, F.; Murone, C.; et al. A phase I biodistribution and pharmacokinetic trial of humanized monoclonal antibody Hu3s193 in patients with advanced epithelial cancers that express the Lewis-Y antigen. Clin. Cancer Res. 2007, 13, 3286–3292. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Pan, Z.; Han, L.; Zhou, Y.; Zong, H.; Wang, L.; Sun, R.; Jiang, H.; Xie, Y.; Yuan, Y.; et al. A Novel Bispecific Antibody Targeting CD3 and Lewis Y with Potent Therapeutic Efficacy against Gastric Cancer. Biomedicines 2021, 9, 1059. [Google Scholar] [CrossRef] [PubMed]
- Beauchemin, N.; Draber, P.; Dveksler, G.; Gold, P.; Gray-Owen, S.; Grunert, F.; Hammarström, S.; Holmes, K.; Karlsson, A.; Kuroki, M.; et al. Redefined nomenclature for members of the carcinoembryonic antigen family. Exp. Cell Res. 1999, 252, 243–249. [Google Scholar]
- Gold, P.; Freedman, S. Demonstration of tumor specific antigen in human colon carcinoma by immunological tolerance and absorption techniques. J. Exp. Med. 1965, 121, 439–462. [Google Scholar] [CrossRef]
- Kammerer, R.; Zimmermann, W. Coevolution of activating and inhibitory receptors within mammalian carcinoembryonic antigen families. BMC Biol. 2010, 8, 12. [Google Scholar] [CrossRef]
- Kuespert, K.; Pils, S.; Hauck, C. CEACAMs: Their role in physiology and pathophysiology. Curr. Opin. Cell Biol. 2006, 18, 565–571. [Google Scholar] [CrossRef]
- Javaheri, A.; Kruse, T.; Moonens, K.; Mejías-Luque, R.; Debraekeleer, A.; Asche, C.; Tegtmeyer, N.; Kalali, B.; Bach, N.; Sieber, S.; et al. Helicobacter pylori adhesin HopQ engages in a virulence-enhancing interaction with human CEACAMs. Nat. Microbiol. 2016, 17, 16189. [Google Scholar] [CrossRef] [PubMed]
- Kinugasa, T.; Kuroki, M.; Yamanaka, T.; Matsuo, Y.; Oikawa, S.; Nakazato, H.; Matsuoka, Y. Non-proteolytic release of carcinoembryonic antigen from normal human colonic epithelial cells cultured in collagen gel. Int. J. Cancer 1994, 58, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Duffy, M.; van Dalen, A.; Haglund, C.; Hansson, L.; Holinski-Feder, E.; Klapdor, R.; Lamerz, R.; Peltomaki, P.; Sturgeon, C.; Topolcan, O. Clinical utility of biochemical markers in colorectal cancer: European Group on Tumour Markers (EGTM) guidelines. Eur. J. Cancer 2003, 39, 718–727. [Google Scholar] [CrossRef]
- Lutterbuese, R.; Raum, T.; Kischel, R.; Lutterbuese, P.; Schlereth, B.; Schaller, E.; Mangold, S.; Rau, D.; Meier, P.; Peter, A.K.; et al. Potent control of tumor growth by CEA/CD3-bispecific single-chain antibody constructs that are not competitively inhibited by soluble CEA. J. Immunother. 2009, 32, 341–352. [Google Scholar] [CrossRef]
- Gilham, D.; O’Neil, A.; Hughes, C.; Guest, R.; Kirillova, N.; Lehane, M.; Hawkins, R. Primary polyclonal human T lymphocytes targeted to carcino-embryonic antigens and neural cell adhesion molecule tumor antigens by CD3zeta-based chimeric immune receptors. J. Immunother. 2002, 25, 139–151. [Google Scholar] [CrossRef]
- Herlyn, M.; Steplewski, Z.; Herlyn, D.; Koprowski, H. Colorectal carcinoma-specific antigen: Detection by means of monoclonal antibodies. Proc. Natl. Acad. Sci. USA 1979, 76, 1438–1442. [Google Scholar] [CrossRef]
- Strnad, J.; Hamilton, A.; Beavers, L.; Gamboa, G.; Apelgren, L.; Taber, L.; Sportsman, J.; Bumol, T.; Sharp, J.; Gadski, R. Molecular cloning and characterization of a human adenocarcinoma/epithelial cell surface antigen complementary DNA. Cancer Res. 1989, 49, 314–317. [Google Scholar]
- Punt, C.; Nagy, A.; Douillard, J.; Figer, A.; Skovsgaard, T.; Monson, J.; Barone, C.; Fountzilas, G.; Riess, H.; Moylan, E.; et al. Edrecolomab alone or in combination with fluorouracil and folinic acid in the adjuvant treatment of stage III colon cancer: A randomised study. Lancet 2002, 360, 671–677. [Google Scholar] [CrossRef]
- Gires, O.; Pan, M.; Schinke, H.; Canis, M.; Baeuerle, P. Expression and function of epithelial cell adhesion molecule EpCAM: Where are we after 40 years? Cancer Metastasis Rev. 2020, 38, 969–987. [Google Scholar] [CrossRef]
- Ju, T.; Otto, V.; Cummings, R. The Tn antigen-structural simplicity and biological complexity. Angew. Chem. Int. Ed. Engl. 2011, 50, 1770–1791. [Google Scholar] [CrossRef]
- Loureiro, L.; Carrascal, M.; Barbas, A.; Ramalho, J.; Novo, C.; Delannoy, P.; Videira, P. Challenges in Antibody Development against Tn and Sialyl-Tn Antigens. Biomolecules 2015, 5, 1783–1809. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.; Zhao, H.; Wang, Y.; Cai, H.; Xiao, Y.; Zeng, Y.; Chen, H. Tumor-associated antigens: Tn antigen, sTn antigen, and T antigen. HLA 2016, 88, 275–286. [Google Scholar] [CrossRef]
- Martínez-Sáez, N.; Castro-López, J.; Valero-González, J.; Madariaga, D.; Compañón, I.; Somovilla, V.; Salvadó, M.; Asensio, J.; Jiménez-Barbero, J.; Avenoza, A.; et al. Deciphering the Non-Equivalence of Serine and Threonine O-Glycosylation Points: Implications for Molecular Recognition of the Tn Antigen by an anti-MUC1 Antibody. Angew. Chem. Int. Ed. Engl. 2015, 54, 9830–9834. [Google Scholar] [CrossRef] [PubMed]
- Posey, A.; Schwab, R.; Boesteanu, A.; Steentof, C.; Mandel, U.; Engels, B.; Stone, J.; Madsen, T.; Schreiber, K.; Haines, K.; et al. Engineered CAR T Cells Targeting the Cancer-Associated Tn-Glycoform of the Membrane Mucin MUC1 Control Adenocarcinoma. Immunity 2016, 44, 1444–1454. [Google Scholar] [CrossRef] [PubMed]
- Garinchesa, P.; Sakamoto, J.; Welt, S.; Real, F.; Rettig, W.; Old, L. Organ-specific expression of the colon cancer antigen A33, a cell surface target for antibody-based therapy. Int. J. Oncol. 1996, 9, 465–471. [Google Scholar] [CrossRef]
- Heath, J.; White, S.; Johnstone, C.; Catimel, B.; Simpson, R.; Moritz, R.; Tu, G.; Ji, H.; Whitehead, R.; Groenen, L.; et al. The human A33 antigen is a transmembrane glycoprotein and a novel member of the immunoglobulin superfamily. Proc. Natl. Acad. Sci. USA 1997, 94, 469–474. [Google Scholar] [CrossRef]
- Baptistella, A.; Salles Dias, M.; Aguiar Jr, S.; Begnami, M.; Martins, V. Heterogeneous expression of A33 in colorectal cancer: Possible explanation for A33 antibody treatment failure. Anticancer Drugs 2016, 27, 734–737. [Google Scholar] [CrossRef]
- Goetsch, L.; Haeuw, J.; Beau-Larvor, C.; Gonzalez, A.; Zanna, L.; Malissard, M.; Lepecquet, A.; Bailly, R.; Broussas, M.; Corvaia, N. A novel role for junctional adhesion molecule-A in tumor proliferation: Modulation by an anti-JAM-A monoclonal antibody. Int. J. Cancer 2013, 132, 1463–1474. [Google Scholar] [CrossRef]
- Pereira-Fantini, P.; Judd, L.; Kalantzis, A.; Peterson, A.; Ernst, M.; Heath, J.; Giraud, A. A33 antigen-deficient mice have defective colonic mucosal repair. Inflamm. Bowel Dis. 2010, 16, 604–612. [Google Scholar] [CrossRef]
- Johnstone, C.; Tebbutt, N.; Abud, H.; White, S.; Stenvers, K.; Hall, N.; Cody, S.; Whitehead, R.; Catimel, B.; Nice, E.; et al. Characterization of mouse A33 antigen, a definitive marker for basolateral surfaces of intestinal epithelial cells. Am. J. Physiol. 2000, 279, G500–G510. [Google Scholar] [CrossRef]
- Johnstone, C.; White, S.; Tebbutt, N.; Clay, F.; Ernst, M.; Biggs, W.; Viars, C.; Czekay, S.; Arden, K.; Heath, J. Analysis of the regulation of the A33 antigen gene reveals intestine-specific mechanisms of gene expression. J. Biol. Chem. 2002, 277, 34531–34539. [Google Scholar] [CrossRef]
- Ackerman, M.; Chalouni, C.; Schmidt, M.; Raman, V.; Ritter, G.; Old, L.; Mellman, I.; Wittrup, K. A33 antigen displays persistent surface expression. Cancer Immunol. Immunother. 2008, 57, 1017–1027. [Google Scholar] [CrossRef]
- King, D.; Antoniw, P.; Owens, R.; Adair, J.; Haines, A.; Farnsworth, A.; Finney, H.; Lawson, A.; Lyons, A.; Baker, T.; et al. Preparation and preclinical evaluation of humanised A33 immunoconjugates for radioimmunotherapy. Br. J. Cancer 1995, 72, 1364–1372. [Google Scholar] [CrossRef]
- Almqvist, Y.; Steffen, A.; Tolmachev, V.; Divgi, C.; Sundin, A. In vitro and in vivo characterization of 177Lu-huA33: A radioimmunoconjugate against colorectal cancer. Nucl. Med. Biol. 2006, 33, 991–998. [Google Scholar] [CrossRef]
- Panjideh, H.; Da Silva Coelho, V.; Dernedde, J.; Bachran, C.; Förster, G.; Franke, J.; Fasold, P.; Fuchs, H.; Thiel, E.; Deckert, P. Biodistribution and efficacy of [131I]A33scFv::CDy, a recombinant antibody-enzyme protein for colon cancer. Int. J. Oncol. 2008, 32, 925–930. [Google Scholar] [CrossRef]
- O’Donoghue, J.; Smith-Jones, P.; Humm, J.; Ruan, S.; Pryma, D.; Jungbluth, A.; Divgi, C.; Carrasquillo, J.; Pandit-Taskar, N.; Fong, Y.; et al. 124I-huA33 antibody uptake is driven by A33 antigen concentration in tissues from colorectal cancer patients imaged by immuno-PET. J. Nucl. Med. 2011, 52, 1878–1885. [Google Scholar] [CrossRef] [PubMed]
- Deckert, P.; Renner, C.; Cohen, L.; Jungbluth, A.; Ritter, G.; Bertino, J.; Old, L.; Welt, S. A33scFv-cytosine deaminase: A recombinant protein construct for antibody-directed enzyme-prodrug therapy. Br. J. Cancer 2003, 88, 937–939. [Google Scholar] [CrossRef][Green Version]
- Wei, D.; Tao, Z.; Shi, Q.; Wang, L.; Liu, L.; She, T.; Yi, Q.; Wen, X.; Liu, L.; Li, S.; et al. Selective Photokilling of Colorectal Tumors by Near-Infrared Photoimmunotherapy with a GPA33-Targeted Single-Chain Antibody Variable Fragment Conjugate. Mol. Pharm. 2020, 17, 2508–2517. [Google Scholar] [CrossRef]
- Moore, P.; Shah, K.; Yang, Y.; Alderson, R.; Roberts, P.; Long, V.; Liu, D.; Li, J.; Burke, S.; Ciccarone, V.; et al. Development of MGD007, a gpA33 x CD3-Bispecific DART Protein for T-Cell Immunotherapy of Metastatic Colorectal Cancer. Mol. Cancer Ther. 2018, 17, 1761–1772. [Google Scholar] [CrossRef] [PubMed]
- Simon, N.; FitzGerald, D. Immunotoxin Therapies for the Treatment of Epidermal Growth Factor Receptor-Dependent Cancers. Toxins 2016, 8, 137. [Google Scholar] [CrossRef] [PubMed]
- Vecchione, L.; Jacobs, B.; Normanno, N.; Ciardiello, F.; Tejpar, S. EGFR-targeted therapy. Exp. Cell Res. 2011, 317, 2765–2771. [Google Scholar] [CrossRef]
- Xie, H.; Ma, Y.; Li, J.; Chen, H.; Xie, Y.; Chen, M.; Zhao, X.; Tang, S.; Zhao, S.; Zhang, Y.; et al. WNT7A Promotes EGF-Induced Migration of Oral Squamous Cell Carcinoma Cells by Activating beta-Catenin/MMP9-Mediated Signaling. Front. Pharmacol. 2020, 11, 98. [Google Scholar] [CrossRef]
- Roskoski, R. The ErbB/HER family of protein-tyrosine kinases and cancer. Pharmacol. Res. 2014, 79, 34–74. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Jing, H.; Zhang, F. Epidermal growth factor receptor-targeted therapy in colorectal cancer. Front. Biosci. 2016, 21, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.; Valeri, N.; Dearman, C.; Rao, S.; Watkins, D.; Starling, N.; Chau, I.; Cunningham, D. Targeting EGFR pathway in metastatic colorectal cancer- tumour heterogeniety and convergent evolution. Crit. Rev. Oncol. Hematol. 2019, 143, 153–163. [Google Scholar] [CrossRef]
- Douillard, J.; Pirker, R.; O’Byrne, K.; Kerr, K.; Störkel, S.; von Heydebreck, A.; Grote, H.; Celik, I.; Shepherd, F. Relationship between EGFR expression, EGFR mutation status, and the efficacy of chemotherapy plus cetuximab in FLEX study patients with advanced non-small-cell lung cancer. J. Thorac. Oncol. 2014, 9, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Zhang, J.; Hu, H.; Cai, Y.; Wu, Z.; Ling, J.; Li, W.; Deng, Y. Efficacy and Safety of Regorafenib in Combination with Chemotherapy as Second-Line Treatment in Patients with Metastatic Colorectal Cancer: A Network Meta-Analysis and Systematic Literature Review. Adv. Ther. 2020, 37, 4233–4248. [Google Scholar] [CrossRef]
- Douillard, J.; Oliner, K.; Siena, S.; Tabernero, J.; Burkes, R.; Barugel, M.; Humblet, Y.; Bodoky, G.; Cunningham, D.; Jassem, J.; et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N. Eng. J. Med. 2013, 369, 1023–1034. [Google Scholar] [CrossRef] [PubMed]
- Dekker, E.; Tanis, P.; Vleugels, J.; Kasi, P.; Wallace, M. Colorectal cancer. Lancet 2019, 394, 1467–1480. [Google Scholar] [CrossRef]
- Byers, V.; Rodvien, R.; Grant, K.; Durrant, L.; Hudson, K.; Baldwin, R.; Scannon, P. Phase I study of monoclonal antibody-ricin A chain immunotoxin XomaZyme-791 in patients with metastatic colon cancer. Cancer Res. 1989, 49, 6153–6660. [Google Scholar]
- LoRusso, P.; Lomen, P.; Redman, B.; Poplin, E.; Bander, J.; Valdivieso, M. Phase I study of monoclonal antibody-ricin A chain immunoconjugate Xomazyme-791 in patients with metastatic colon cancer. Am. J. Clin. Oncol. 1995, 18, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Zalcberg, J.; Pietersz, G.; Toohey, B.; Laird, J.; Huggins, R.; Zimet, A.; Hennessy, O.; McKenzie, A.; McKenzie, I. A phase I/II study of the intralesional injection of ricin-monoclonal antibody conjugates in patients with hepatic metastases. Eur. J. Cancer 1994, 30A, 1227–1231. [Google Scholar] [CrossRef]
- Pai, L.; Wittes, R.; Setser, A.; Willingham, M.; Pastan, I. Treatment of advanced solid tumors with immunotoxin LMB-1: An antibody linked to Pseudomonas exotoxin. Nat. Med. 1996, 2, 350–353. [Google Scholar] [CrossRef] [PubMed]
- Posey, J.; Khazaeli, M.; Bookman, M.; Nowrouzi, A.; Grizzle, W.; Thornton, J.; Carey, D.; Lorenz, J.; Sing, A.; Siegall, C.; et al. A phase I trial of the single-chain immunotoxin SGN-10 (BR96 sFv-PE40) in patients with advanced solid tumors. Clin. Cancer Res. 2002, 8, 3092–3099. [Google Scholar]
- Andersson, Y.; Engebraaten, O.; Juell, S.; Aamdal, S.; Brunsvig, P.; Fodstad, Ø.; Dueland, S. Phase I trial of EpCAM-targeting immunotoxin MOC31PE, alone and in combination with cyclosporin. Br. J. Cancer 2015, 113, 1548–1555. [Google Scholar] [CrossRef]
- Andersson, Y.; Inderberg, E.; Kvalheim, G.; Herud, T.; Engebraaten, O.; Flatmark, K.; Dueland, S.; Fodstad, Ø. Immune stimulatory effect of anti-EpCAM immunotoxin—improved overall survival of metastatic colorectal cancer patients. Acta Oncol. 2020, 59, 404–409. [Google Scholar] [CrossRef]
- Frøysnes, I.; Andersson, Y.; Larsen, S.; Davidson, B.; Torset Øien, J.; Julsrud, L.; Fodstad, Ø.; Dueland, S.; Flatmark, K. ImmunoPeCa trial: Long-term outcome following intraperitoneal MOC31PE immunotoxin treatment in colorectal peritoneal metastasis. Eur. J. Surg. Oncol. 2021, 47, 134–138. [Google Scholar] [CrossRef]
- Frøysnes, I.; Andersson, Y.; Larsen, S.; Davidson, B.; Torset Øien, J.; Olsen, K.; Giercksky, K.; Julsrud, L.; Fodstad, Ø.; Dueland, S.; et al. Novel Treatment with Intraperitoneal MOC31PE Immunotoxin in Colorectal Peritoneal Metastasis: Results From the ImmunoPeCa Phase 1 Trial. Ann. Surg. Oncol. 2017, 24, 1916–1922. [Google Scholar] [CrossRef]
- Azemar, M.; Djahansouzi, S.; Jäger, E.; Solbach, C.; Schmidt, M.; Maurer, A.; Mross, K.; Unger, C.; von Minckwitz, G.; Dall, P.; et al. Regression of cutaneous tumor lesions in patients intratumorally injected with a recombinant single-chain antibody-toxin targeted to ErbB2/HER2. Breast Cancer Res. Treat. 2003, 82, 155–164. [Google Scholar] [CrossRef]
- von Minckwitz, G.; Harder, S.; Hövelmann, S.; Jäger, E.; Al-Batran, S.; Loibl, S.; Atmaca, A.; Cimpoiasu, C.; Neumann, A.; Abera, A.; et al. Phase I clinical study of the recombinant antibody toxin scFv(FRP5)-ETA specific for the ErbB2/HER2 receptor in patients with advanced solid malignomas. Breast Cancer Res. 2005, 7, R617–R626. [Google Scholar] [CrossRef]
- Andersson, Y.; Engebraaten, O.; Fodstad, Ø. Synergistic anti-cancer effects of immunotoxin and cyclosporin in vitro and in vivo. Br. J. Cancer 2009, 101, 1307–1315. [Google Scholar] [CrossRef] [PubMed]
- Engebraaten, O.; Sivam, G.; Juell, S.; Fodstad, O. Systemic immunotoxin treatment inhibits formation of human breast cancer metastasis and tumor growth in nude rats. Int. J. Cancer 2000, 88, 970–976. [Google Scholar] [CrossRef]
- Akamatsu, Y.; Murphy, J.; Nolan, K.; Thomas, P.; Kreitman, R.; Leung, S.; Junghans, R. A single-chain immunotoxin against carcinoembryonic antigen that suppresses growth of colorectal carcinoma cells. Clin. Cancer Res. 1998, 4, 2825–2832. [Google Scholar]
- Shinohara, H.; Fan, D.; Ozawa, S.; Yano, S.; Van Arsdell, M.; Viner, J.; Beers, R.; Pastan, I.; Fidler, I. Site-specific expression of transferrin receptor by human colon cancer cells directly correlates with eradication by antitransferrin recombinant immunotoxin. Int. J. Oncol. 2000, 17, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Traini, R.; Ben-Josef, G.; Pastrana, D.; Moskatel, E.; Sharma, A.; Antignani, A.; Fitzgerald, D. ABT-737 overcomes resistance to immunotoxin-mediated apoptosis and enhances the delivery of pseudomonas exotoxin-based proteins to the cell cytosol. Mol. Cancer Ther. 2010, 9, 2007–2015. [Google Scholar] [CrossRef]
- Cerise, A.; Bera, T.; Liu, X.; Wei, J.; Pastan, I. Anti-Mesothelin Recombinant Immunotoxin Therapy for Colorectal Cancer. Clin. Colorectal. Cancer 2019, 18, 192–199. [Google Scholar] [CrossRef]
- Onda, M.; Kobayashi, K.; Pastan, I. Depletion of regulatory T cells in tumors with an anti-CD25 immunotoxin induces CD8 T cell-mediated systemic antitumor immunity. Proc. Natl. Acad. Sci. USA 2019, 116, 4575–4582. [Google Scholar] [CrossRef]
- Rathore, D.; Nayak, S.; Batra, J. Overproduction of fungal ribotoxin alpha-sarcin in Escherichia coli: Generation of an active immunotoxin. Gene 1997, 190, 31–35. [Google Scholar] [CrossRef]
- Wawrzynczak, E.; Henry, R.; Cumber, A.; Parnell, G.; Derbyshire, E.; Ulbrich, N. Biochemical, cytotoxic and pharmacokinetic properties of an immunotoxin composed of a mouse monoclonal antibody Fib75 and the ribosome-inactivating protein alpha-sarcin from Aspergillus giganteus. Eur. J. Biochem. 1991, 196, 203–209. [Google Scholar] [CrossRef]
- Goyal, A.; Batra, J. Inclusion of a furin-sensitive spacer enhances the cytotoxicity of ribotoxin restrictocin containing recombinant single-chain immunotoxins. Biochem. J. 2000, 345, 247–254. [Google Scholar] [CrossRef]
- Carreras-Sangra, N.; Tomé-Amat, J.; García-Ortega, L.; Batt, C.; Oñaderra, M.; Martínez-del-Pozo, A.; Gavilanes, J.; Lacadena, J. Production and characterization of a colon cancer-specific immunotoxin based on the fungal ribotoxin α-sarcin. Protein Eng. Des. Sel. 2012, 25, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Tomé-Amat, J.; Olombrada, M.; Ruiz-de-la-Herrán, J.; Pérez-Gómez, E.; Andradas, C.; Sánchez, C.; Martínez, L.; Martínez-del-Pozo, A.; Gavilanes, J.; Lacadena, J. Efficient in vivo antitumor effect of an immunotoxin based on ribotoxin α-sarcin in nude mice bearing human colorectal cancer xenografts. SpringerPlus 2015, 4, 168. [Google Scholar] [CrossRef]
- Tomé-Amat, J.; Menéndez-Méndez, A.; García-Ortega, L.; Batt, C.; Oñaderra, M.; Martínez-del-Pozo, A.; Gavilanes, J.; Lacadena, J. Production and characterization of scFvA33T1, an immunoRNase targeting colon cancer cells. FEBS J. 2012, 279, 3022–3032. [Google Scholar] [CrossRef]
- Tomé-Amat, J.; Ruiz-de-la-Herrán, J.; Martínez-del-Pozo, A.; Gavilanes, J.; Lacadena, J. α-sarcin and RNase T1 based immunoconjugates: The role of intracellular trafficking in cytotoxic efficiency. FEBS J. 2015, 282, 673–684. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-de-la-Herrán, J.; Tomé-Amat, J.; Lázaro-Gorines, R.; Gavilanes, J.; Lacadena, J. Inclusion of a Furin Cleavage Site Enhances Antitumor Efficacy against Colorectal Cancer Cells of Ribotoxin α-Sarcin- or RNase T1-Based Immunotoxins. Toxins 2019, 11, 593. [Google Scholar] [CrossRef]
- Begent, R.; Verhaar, M.; Chester, K.; Casey, J.; Green, A.; Napier, M.; Hope-Stone, L.; Cushen, N.; Keep, P.; Johnson, C.; et al. Clinical evidence of efficient tumor targeting based on single-chain Fv antibody selected from a combinatorial library. Nat. Med. 1996, 2, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Boehm, M.; Corper, A.; Wan, T.; Sohi, M.; Sutton, B.; Thornton, J.; Keep, P.; Chester, K.; Begent, R.; Perkins, S. Crystal structure of the anti-(carcinoembryonic antigen) single-chain Fv antibody MFE-23 and a model for antigen binding based on intermolecular contacts. Biochem. J. 2000, 346, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Verhaar, M.; Chester, K.; Keep, P.; Robson, L.; Pedley, R.; Boden, J.; Hawkins, R.; Begent, R. A single chain Fv derived from a filamentous phage library has distinct tumor targeting advantages over one derived from a hybridoma. Int. J. Cancer 1995, 61, 497–501. [Google Scholar] [CrossRef]
- Lázaro-Gorines, R.; Ruiz-de-la-Herrán, J.; Navarro, R.; Sanz, L.; Álvarez-Vallina, L.; Martínez-Del-Pozo, A.; Gavilanes, J.; Lacadena, J. A novel Carcinoembryonic Antigen (CEA)-Targeted Trimeric Immunotoxin shows significantly enhanced Antitumor Activity in Human Colorectal Cancer Xenografts. Sci. Rep. 2019, 9, 11680. [Google Scholar] [CrossRef]
- Cuesta, A.; Sánchez-Martín, D.; Sanz, L.; Bonet, J.; Compte, M.; Kremer, L.; Blanco, F.; Oliva, B.; Alvarez-Vallina, L. In vivo tumor targeting and imaging with engineered trivalent antibody fragments containing collagen-derived sequences. PLoS ONE 2009, 4, e5381. [Google Scholar] [CrossRef]
- Sánchez-Arévalo Lobo, V.; Cuesta, A.; Sanz, L.; Compte, M.; García, P.; Prieto, J.; Blanco, F.; Alvarez-Vallina, L. Enhanced antiangiogenic therapy with antibody-collagen XVIII NC1 domain fusion proteins engineered to exploit matrix remodeling events. Int. J. Cancer 2006, 119, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Namba, M.; Hattori, N.; Hamada, H.; Yamaguchi, K.; Okamoto, Y.; Nakashima, T.; Masuda, T.; Sakamoto, S.; Horimasu, Y.; Miyamoto, S.; et al. Anti-KL-6/MUC1 monoclonal antibody reverses resistance to trastuzumab-mediated antibody-dependent cell-mediated cytotoxicity by capping MUC1. Cancer Lett. 2019, 442, 31–39. [Google Scholar] [CrossRef]
- Sarnovsky, R.; Tendler, T.; Makowski, M.; Kiley, M.; Antignani, A.; Traini, R.; Zhang, J.; Hassan, R.; FitzGerald, D. Initial characterization of an immunotoxin constructed from domains II and III of cholera exotoxin. Cancer Immunol. Immunother. 2010, 59, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Deng, C.; Xiong, J.; Gu, X.; Chen, X.; Wu, S.; Wang, Z.; Wang, D.; Tu, J.; Xie, J. Novel recombinant immunotoxin of EGFR specific nanobody fused with cucurmosin, construction and antitumor efficiency in vitro. Oncotarget 2017, 8, 38568–38580. [Google Scholar] [CrossRef]
- Zhang, C.; Cai, Y.; Dai, X.; Wu, J.; Lan, Y.; Zhang, H.; Lu, M.; Liu, J.; Xie, J. Novel EGFR-bispecific recombinant immunotoxin based on cucurmosin shows potent anti-tumor efficiency in vitro. Oncol. Rep. 2021, 45, 493–500. [Google Scholar] [CrossRef]
- Shapira, S.; Shapira, A.; Starr, A.; Kazanov, D.; Kraus, S.; Benhar, I.; Arber, N. An immunoconjugate of anti-CD24 and Pseudomonas exotoxin selectively kills human colorectal tumors in mice. Gastroenterology 2011, 140, 935–946. [Google Scholar] [CrossRef]
- Batra, J.; Fitzgerald, D.; Chaudhary, V.; Pastan, I. Single-chain immunotoxins directed at the human transferrin receptor containing Pseudomonas exotoxin A or diphtheria toxin: Anti-TFR(Fv)-PE40 and DT388-anti-TFR(Fv). Mol. Cell Biol. 1991, 11, 2200–2205. [Google Scholar] [PubMed]
- Lund, K.; Bostad, M.; Skarpen, E.; Braunagel, M.; Kiprijanov, S.; Krauss, S.; Duncan, A.; Høgset, A.; Selbo, P. The novel EpCAM-targeting monoclonal antibody 3-17I linked to saporin is highly cytotoxic after photochemical internalization in breast, pancreas and colon cancer cell lines. MAbs 2014, 6, 1038–1050. [Google Scholar] [CrossRef]
- Bostad, M.; Olsen, C.; Peng, Q.; Berg, K.; Høgset, A.; Selbo, P. Light-controlled endosomal escape of the novel CD133-targeting immunotoxin AC133-saporin by photochemical internalization—A minimally invasive cancer stem cell-targeting strategy. J. Control. Release 2015, 206, 37–48. [Google Scholar] [CrossRef]
- Stish, B.; Chen, H.; Shu, Y.; Panoskaltsis-Mortari, A.; Vallera, D. A bispecific recombinant cytotoxin (DTEGF13) targeting human interleukin-13 and epidermal growth factor receptors in a mouse xenograft model of prostate cancer. Clin. Cancer Res. 2007, 13, 6486–6493. [Google Scholar] [CrossRef]
- Tomé-Amat, J.; Herrero-Galán, E.; Oñaderra, M.; Martínez-Del-Pozo, A.; Gavilanes, J.; Lacadena, J. Preparation of an engineered safer immunotoxin against colon carcinoma based on the ribotoxin hirsutellin A. FEBS J. 2015, 282, 2131–2141. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.; Zhang, J.; Min, K.; Lee, K.; Moon, C.; Balthasar, J.; Yang, V. Combination of antibody targeting and PTD-mediated intracellular toxin delivery for colorectal cancer therapy. J. Control. Release 2014, 194, 197–210. [Google Scholar] [CrossRef]
- Tsai, L.; Chen, Y.; Lee, C.; Chen, H.; Chang, Z.; Hung, M.; Chao, P.; Lin, J. Growth suppression of human colorectal carcinoma in nude mice by monoclonal antibody C27-abrin A chain conjugate. Dis. Colon. Rectum. 1995, 38, 1067–1074. [Google Scholar] [CrossRef] [PubMed]
- Mazor, R.; Pastan, I. Immunogenicity of Immunotoxins Containing Pseudomonas Exotoxin A: Causes, Consequences, and Mitigation. Front. Immunol. 2020, 11, 1261. [Google Scholar] [CrossRef] [PubMed]
- Vallera, D.; Kreitman, R. Immunotoxins Targeting B cell Malignancy—Progress and Problems With Immunogenicity. Biomedicines 2019, 7, 1. [Google Scholar] [CrossRef]
- Onda, M.; Nagata, S.; FitzGerald, D.; Beers, R.; Fisher, R.; Vincent, J.; Lee, B.; Nakamura, M.; Hwang, J.; Kreitman, R.; et al. Characterization of the B cell epitopes associated with a truncated form of Pseudomonas exotoxin (PE38) used to make immunotoxins for the treatment of cancer patients. J. Immunol. 2006, 177, 8822–8834. [Google Scholar] [CrossRef]
- Onda, M.; Beers, R.; Xiang, L.; Nagata, S.; Wang, Q.; Pastan, I. An immunotoxin with greatly reduced immunogenicity by identification and removal of B cell epitopes. Proc. Natl. Acad. Sci. USA 2008, 105, 11311–11316. [Google Scholar] [CrossRef]
- Mazor, R.; Onda, M.; Park, D.; Addissie, S.; Xiang, L.; Zhang, J.; Hassan, R.; Pastan, I. Dual B- and T-cell de-immunization of recombinant immunotoxin targeting mesothelin with high cytotoxic activity. Oncotarget 2016, 7, 29916. [Google Scholar] [CrossRef]
- Guo, R.; Zhang, D.; Zhang, C.; Yang, Y.; Liu, H.; Yang, Y.; Lin, J. Immunotoxin IHP25-BT with low immunogenicity and off-target toxicity inhibits the growth and metastasis of trastuzumab-resistant tumor cells. Int. J. Pharm. 2021, 608, 121081. [Google Scholar] [CrossRef]
- Fuchs, H.; Weng, A.; Gilabert-Oriol, R. Augmenting the Efficacy of Immunotoxins and Other Targeted Protein Toxins by Endosomal Escape Enhancers. Toxins 2016, 8, 200. [Google Scholar] [CrossRef]
- Smith, W.; Johnston, D.; Wensley, H.; Holmes, S.; Flavell, S.; Flavell, D. The Role of Cholesterol on Triterpenoid Saponin-Induced Endolysosomal Escape of a Saporin-Based Immunotoxin. Int. J. Mol. Sci. 2020, 21, 8734. [Google Scholar] [CrossRef]
- Wei, J.; Bera, T.; Liu, X.; Zhou, Q.; Onda, M.; Ho, M.; Tai, C.; Pastan, I. Recombinant immunotoxins with albumin-binding domains have long half-lives and high antitumor activity. Proc. Natl. Acad. Sci. USA 2018, 115, E3501–E3508. [Google Scholar] [CrossRef]
- Nuñez-Prado, N.; Compte, M.; Harwood, S.; Álvarez-Méndez, A.; Lykkemark, S.; Sanz, L.; Álvarez-Vallina, L. The coming of age of engineered multivalent antibodies. Drug Discov. Today 2015, 20, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Mazor, Y.; Sachsenmeier, K.; Yang, C.; Hansen, A.; Filderman, J.; Mulgrew, K.; Wu, H.; Dall’Acqua, W. Enhanced tumor-targeting selectivity by modulating bispecific antibody binding affinity and format valence. Sci. Rep. 2017, 7, 40098. [Google Scholar] [CrossRef] [PubMed]
- Stish, B.; Chen, H.; Shu, Y.; Panoskaltsis-Mortari, A.; Vallera, D. Increasing anticarcinoma activity of an anti-erbB2 recombinant immunotoxin by the addition of an anti-EpCAM sFv. Clin. Cancer Res. 2007, 13, 3058–3067. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Yang, Y.; Zhang, D.; Du, J.; Zhu, X.; Liu, Y.; Yang, F.; Lin, J. A bispecific immunotoxin (IHPP) with a long half-life targeting HER2 and PDGFRβ exhibited improved efficacy against HER2-positive tumors in a mouse xenograft model. Int. J. Pharm. 2021, 592, 120037. [Google Scholar] [CrossRef] [PubMed]
- Guijarro-Muñoz, I.; Compte, M.; Alvarez-Vallina, L.; Sanz, L. Antibody gene therapy: Getting closer to clinical application? Curr. Gene Ther. 2013, 13, 282–290. [Google Scholar] [CrossRef]
- Compte, M.; Alonso-Camino, V.; Santos-Valle, P.; Cuesta, A.; Sánchez-Martín, D.; López, M.; Vicario, J.; Sanz, L.; Alvarez-Vallina, L. Factory neovessels: Engineered human blood vessels secreting therapeutic proteins as a new drug delivery system. Gene Ther. 2010, 17, 745–751. [Google Scholar] [CrossRef]
- Saenz del Burgo, L.; Compte, M.; Aceves, M.; Hernández, R.; Sanz, L.; Álvarez-Vallina, L.; Pedraz, J. Microencapsulation of therapeutic bispecific antibodies producing cells: Immunotherapeutic organoids for cancer management. J. Drug Target. 2015, 23, 170–179. [Google Scholar] [CrossRef]
- Pohl-Guimarães, F.; LB, H.-M.; Mitchell, D. RNA-electroporated T cells for cancer immunotherapy. OncoImmunology 2020, 9, 1792625. [Google Scholar] [CrossRef]
- Eggers, R.; Philippi, A.; Altmeyer, M.; Breinig, F.; Schmitt, M. Primary T cells for mRNA-mediated immunotoxin delivery. Gene Ther. 2018, 25, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Augusta Di Trani, C.; Fernandez-Sendin, M.; Cirella, A.; Segués, A.; Olivera, I.; Bolaños, E.; Melero, I.; Berraondo, P. Advances in mRNA-based drug discovery in cancer immunotherapy. Expert Opin. Drug Discov. 2021, 2021, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Deal, C.; Carfi, A.; Plante, O. Advancements in mRNA Encoded Antibodies for Passive Immunotherapy. Vaccines 2021, 9, 108. [Google Scholar] [CrossRef] [PubMed]
- Sanz, L.; Alvarez-Vallina, L. Engineered mRNA and the Rise of Next-Generation Antibodies. Antibodies 2021, 10, 37. [Google Scholar] [CrossRef]
| ITX | Toxin | Antibody Format | Target | Clinical Trial | Phase | Ref. |
|---|---|---|---|---|---|---|
| Xomazyme-791 | Ricin | mo IgG2b | 72kDa | N/A | Phase 1 | [120,121] |
| Anti-CEA-bR | Blocked ricin | mo IgG | CEA | N/A | Phase 1/2 | [122] |
| LMB-1 | PE38 | mo IgG1 | Lewis Y | NCT00001805 | Phase 2 | [123] |
| LMB-9 | PE38 | dsFv | Lewis Y | NCT00019435 NCT00005858 | Phase 1 Phase 1 | [16] |
| SGN-10 | PE40 | scFv | Lewis Y | N/A | Phase 1 | [124] |
| MOC31PE | PE | mo IgG1 | EpCAM (CD326) | NCT01061645 NCT02219893 | Phase 1 Phase 1/2 | [125,126,127,128] |
| BM7PE | PE | mo IgG1 | MUC-1 | NCT04550897 | Phase 1/2 | N/A |
| ITX | Toxin | Antibody Format | Target | Ref. |
|---|---|---|---|---|
| 2E4-PE38 | PE38 | scFv | CD25 | [137] |
| SWA11-ZZ-PE38 | PE38 | mo IgG2a | CD24 | [156] |
| HB21-PE40 | PE40 | scFv | TFR | [134,135,157] |
| LMB-12 LMB-100 LMB-164 | PE24 PE24 * PE24 | dsFv Hz Fab dsFv+ABD | Mesothelin | [136] |
| hMN14(Fv)-PE40 | PE40 | Hz scFv | CEA | [133] |
| HB21-CET40 | CET40 | scFv | TFR | [153] |
| 3-17I-saporin | saporin | hu IgG1 | EpCAM (CD326) | [158] |
| AC133-saporin | saporin | mo IgG1 | CD133 | [159] |
| DTEpCAM23 | DT | (scFv)2 | EpCAM x HER2 | [160] |
| MFE23-GRNLY | granulysin | scFv | CEA | [28] |
| SM3GRNLY | granulysin | scFv | Tn | [27] |
| IMTXA33αS IMTXA33furαS | α-sarcinE | scFv | GPA33 | [141,144,145] |
| IMTXCEAαS IMTXTRICEAαS | α-sarcin | scFv, trimerbody | CEA | [149] |
| scFvA33T1 scFvA33furT1 | RNase T1 | scFv | GPA33 | [144,145] |
| IMTXA33HtA3ΔW | hirsutellin A | scFv | GPA33 | [161] |
| T84.66-gelonin | gelonin | mo IgG1 | CEA | [162] |
| MAbC27-abrin A | abrin A | mo IgG1 | CEA | [163] |
| Bs/CUS | cucurmosin | bp (sdAb)2 | EGFR | [155] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanz, L.; Ibáñez-Pérez, R.; Guerrero-Ochoa, P.; Lacadena, J.; Anel, A. Antibody-Based Immunotoxins for Colorectal Cancer Therapy. Biomedicines 2021, 9, 1729. https://doi.org/10.3390/biomedicines9111729
Sanz L, Ibáñez-Pérez R, Guerrero-Ochoa P, Lacadena J, Anel A. Antibody-Based Immunotoxins for Colorectal Cancer Therapy. Biomedicines. 2021; 9(11):1729. https://doi.org/10.3390/biomedicines9111729
Chicago/Turabian StyleSanz, Laura, Raquel Ibáñez-Pérez, Patricia Guerrero-Ochoa, Javier Lacadena, and Alberto Anel. 2021. "Antibody-Based Immunotoxins for Colorectal Cancer Therapy" Biomedicines 9, no. 11: 1729. https://doi.org/10.3390/biomedicines9111729
APA StyleSanz, L., Ibáñez-Pérez, R., Guerrero-Ochoa, P., Lacadena, J., & Anel, A. (2021). Antibody-Based Immunotoxins for Colorectal Cancer Therapy. Biomedicines, 9(11), 1729. https://doi.org/10.3390/biomedicines9111729







