A Comparison between Endostatin and Conventional Biomarkers on 30-Day Mortality and Renal Replacement Therapy in Unselected Intensive Care Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
- Admission to the ICU at Östersund hospital;
- Documented informed consent verbally approved by the patient or trustee;
- Need for arterial blood sampling and/or monitoring;
- Age of 18 years or above.
2.2. Blood Sampling and Analyses
2.3. Statistics
3. Results
Study Cohort
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Folkman, J. Antiangiogenesis in cancer therapy—Endostatin and its mechanisms of action. Exp. Cell Res. 2006, 312, 594–607. [Google Scholar] [CrossRef]
- Tomono, Y.; Naito, I.; Ando, K.; Yonezawa, T.; Sado, Y.; Hirakawa, S.; Arata, J.; Okigaki, T.; Ninomiya, Y. Epitope-defined Monoclonal Antibodies against Multiplexin Collagens Demonstrate that Type XV and XVIII Collagens are Expressed in Specialized Basement Membranes. Cell Struct. Funct. 2002, 27, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Bellini, M.H.; Coutinho, E.L.; Filgueiras, T.C.; Maciel, T.; Schor, N. Endostatin expression in the murine model of ischaemia/reperfusion-induced acute renal failure. Nephrology 2007, 12, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Bellini, M.H.; Malpighi, T.F.; Calvo, F.B.; Miranda, A.R.; Spencer, P.J.; Cichy, M.C.; Simons, S.M.; Tavassi, A.M.C.; Santos, M.; Rodrigues, C.J.; et al. Immobilized Kidney 28-kDa Endostatin-Related (KES28kDa) Fragment Promotes Endothelial Cell Survival. Am. J. Nephrol. 2010, 31, 255–261. [Google Scholar] [CrossRef]
- Peng, Y.; Gao, M.; Jiang, Y.; Wang, K.; Zhang, H.; Xiao, Z.; Ou, H.; Yang, B.; Yang, M.; Xiao, X. Angiogenesis Inhibitor Endostatin Protects Mice with Sepsis from Multiple Organ Dysfunction Syndrome. Shock 2015, 44, 357–364. [Google Scholar] [CrossRef]
- Larsson, A.; Tydén, J.; Johansson, J.; Lipcsey, M.; Bergquist, M.; Kultima, K.; Mandic-Havelka, A. Calprotectin is superior to procalcitonin as a sepsis marker and predictor of 30-day mortality in intensive care patients. Scand. J. Clin. Lab. Investig. 2019, 80, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Moreno, R.P.; Metnitz, P.G.H.; Almeida, E.; Jordan, B.; Bauer, P.; Campos, R.A.; Iapichino, G.; Edbrooke, D.; Capuzzo, M.; Le Gall, J.-R. SAPS 3—From evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission. Intensiv. Care Med. 2005, 31, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Tydén, J.; Herwald, H.; Hultin, M.; Walldén, J.; Johansson, J. Heparin-binding protein as a biomarker of acute kidney injury in critical illness. Acta Anaesthesiol. Scand. 2017, 61, 797–803. [Google Scholar] [CrossRef]
- Martensson, J.; Jonsson, N.; Glassford, N.J.; Bell, M.; Martling, C.-R.; Bellomo, R.; Larsson, A. Plasma endostatin may improve acute kidney injury risk prediction in critically ill patients. Ann. Intensiv. Care 2016, 6, 6. [Google Scholar] [CrossRef]
- Jia, H.-M.; Zheng, Y.; Huang, L.-F.; Xin, X.; Ma, W.-L.; Jiang, Y.-J.; Zheng, X.; Guo, S.-Y.; Li, W.-X. Derivation and validation of plasma endostatin for predicting renal recovery from acute kidney injury: A prospective validation study. Crit. Care 2018, 22, 305. [Google Scholar] [CrossRef]
- Mårtensson, J.; Vaara, S.T.; Pettilä, V.; Ala-Kokko, T.; Karlsson, S.; Inkinen, O.; Uusaro, A.; Larsson, A.; Bell, M. Assessment of plasma endostatin to predict acute kidney injury in critically ill patients. Acta Anaesthesiol. Scand. 2017, 61, 1286–1295. [Google Scholar] [CrossRef] [PubMed]
- Ruge, T.; Carlsson, A.C.; Larsson, T.E.; Carrero, J.-J.; Larsson, A.; Lind, L.; Ärnlöv, J. Endostatin Level is Associated with Kidney Injury in the Elderly: Findings from Two Community-Based Cohorts. Am. J. Nephrol. 2014, 40, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Ärnlöv, J.; Ruge, T.; Ingelsson, E.; Larsson, A.; Sundström, J.; Lind, L. Serum Endostatin and Risk of Mortality in the Elderly: Findings from 2 community-based cohorts. Arter. Thromb. Vasc. Biol. 2013, 33, 2689–2695. [Google Scholar] [CrossRef] [PubMed]
- Ruge, T.; Carlsson, A.C.; Kjøller, E.; Hilden, J.; Kolmos, H.J.; Sajadieh, A.; Kastrup, J.; Jensen, G.B.; Larsson, A.; Nowak, C.; et al. Circulating endostatin as a risk factor for cardiovascular events in patients with stable coronary heart disease: A CLARICOR trial sub-study. Atherosclerosis 2019, 284, 202–208. [Google Scholar] [CrossRef]
- Ruge, T.; Carlsson, A.C.; Jansson, J.-H.; Söderberg, S.; Larsson, A.; Ärnlöv, J. The association between circulating endostatin levels and incident myocardial infarction. Scand. Cardiovasc. J. 2018, 52, 315–319. [Google Scholar] [CrossRef]
- Marneros, A.G.; Olsen, B.R. Physiological role of collagen XVIII and endostatin. FASEB J. 2005, 19, 716–728. [Google Scholar] [CrossRef]
- Lin, H.C.; Chang, J.H.; Jain, S.; Gabison, E.E.; Kure, T.; Kato, T.; Fukai, N.; Azar, D.T. Matrilysin cleavage of corneal collagen type XVIII NC1 domain and generation of a 28-kDa fragment. Investig. Ophthalmol. Vis. Sci. 2001, 42, 2517–2524. [Google Scholar]
- Hoste, E.A.J.; Bagshaw, S.M.; Bellomo, R.; Cely, C.M.; Colman, R.; Cruz, D.N.; Edipidis, K.; Forni, L.G.; Gomersall, C.D.; Govil, D.; et al. Epidemiology of acute kidney injury in critically ill patients: The multinational AKI-EPI study. Intensiv. Care Med. 2015, 41, 1411–1423. [Google Scholar] [CrossRef]
- Vijayan, A.; Abdel-Rahman, E.M.; Liu, K.D.; Goldstein, S.L.; Agarwal, A.; Okusa, M.D.; Cerda, J. Recovery after Critical Illness and Acute Kidney Injury. Clin. J. Am. Soc. Nephrol. 2021, 16, 1601–1609. [Google Scholar] [CrossRef]
- Endre, Z.H. Recovery from Acute Kidney Injury: The Role of Biomarkers. Nephron Clin. Pract. 2014, 127, 101–105. [Google Scholar] [CrossRef]
- Abedin, M.; King, N. Diverse evolutionary paths to cell adhesion. Trends Cell Biol. 2010, 20, 734–742. [Google Scholar] [CrossRef]
- Karsdal, M.A.; Nielsen, S.H.; Leeming, D.J.; Langholm, L.L.; Nielsen, M.J.; Manon-Jensen, T.; Siebuhr, A.; Gudmann, N.S.; Ronnow, S.; Sand, J.M.; et al. The good and the bad collagens of fibrosis—Their role in signaling and organ function. Adv. Drug Deliv. Rev. 2017, 121, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Jansen, T.C.; Van Bommel, J.; Schoonderbeek, F.J.; Visser, S.J.S.; Van Der Klooster, J.M.; Lima, A.P.; Willemsen, S.P.; Bakker, J. Early Lactate-Guided Therapy in Intensive Care Unit Patients: A multicenter, open-label, randomized controlled trial. Am. J. Respir. Crit. Care Med. 2010, 182, 752–761. [Google Scholar] [CrossRef]
- Mansour, S.G.; Zhang, W.R.; Moledina, D.; Coca, S.G.; Jia, Y.; Thiessen-Philbrook, H.; McArthur, E.; Inoue, K.; Koyner, J.L.; Shlipak, M.G.; et al. The Association of Angiogenesis Markers With Acute Kidney Injury and Mortality After Cardiac Surgery. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2019, 74, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Åkerfeldt, T.; Gunningberg, L.; Swenne, C.L.; Ronquist, G.; Larsson, A. Elective orthopedic and cardiopulmonary bypass surgery causes a reduction in serum endostatin levels. Eur. J. Med. Res. 2014, 19, 61. [Google Scholar] [CrossRef][Green Version]
- Jadhav, A.P.; Sadaka, F.G. Angiotensin II in septic shock. Am. J. Emerg. Med. 2019, 37, 1169–1174. [Google Scholar] [CrossRef] [PubMed]
- John, H.; Preissner, K.T.; Forssmann, W.-G.; Ständker, L. Novel Glycosylated Forms of Human Plasma Endostatin and Circulating Endostatin-Related Fragments of Collagen XV†. Biochemistry 1999, 38, 10217–10224. [Google Scholar] [CrossRef]
- Iribarren, C.; Herrinton, L.J.; Darbinian, J.A.; Tamarkin, L.; Malinowski, D.; Vogelman, J.H.; Orentreich, N.; Baer, D. Does the association between serum endostatin, an endogenous anti-angiogenic protein, and acute myocardial infarction differ by race? Vasc. Med. 2006, 11, 13–20. [Google Scholar] [CrossRef] [PubMed]
| Survivors | Non-Survivors | p-Value | |||
|---|---|---|---|---|---|
| Medican | IQR | Median | IQR | ||
| SAPS3 | 53 | 45–63 | 72 | 66–79 | p < 0.001 |
| Age | 64 | 49–79 | 72 | 68–79 | p < 0.001 |
| Creatinine | 80 | 61–115 | 109 | 75–164 | p < 0.001 |
| Endostatin | 39.8 | 27.8–63.2 | 67.6 | 47.4–94.4 | p < 0.001 |
| Non-AKI | AKI Day 7 | p-Value | |||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| SAPS3 | 55 | 45–66 | 64 | 53–74 | p < 0.001 |
| Age | 66 | 49–76 | 70 | 62–76 | n.s. |
| Creatinine | 81 | 60–92 | 132 | 107–186 | p < 0.001 |
| Endostatin | 38.4 | 27.4–59.2 | 60.5 | 35.7–92.3 | p < 0.001 |
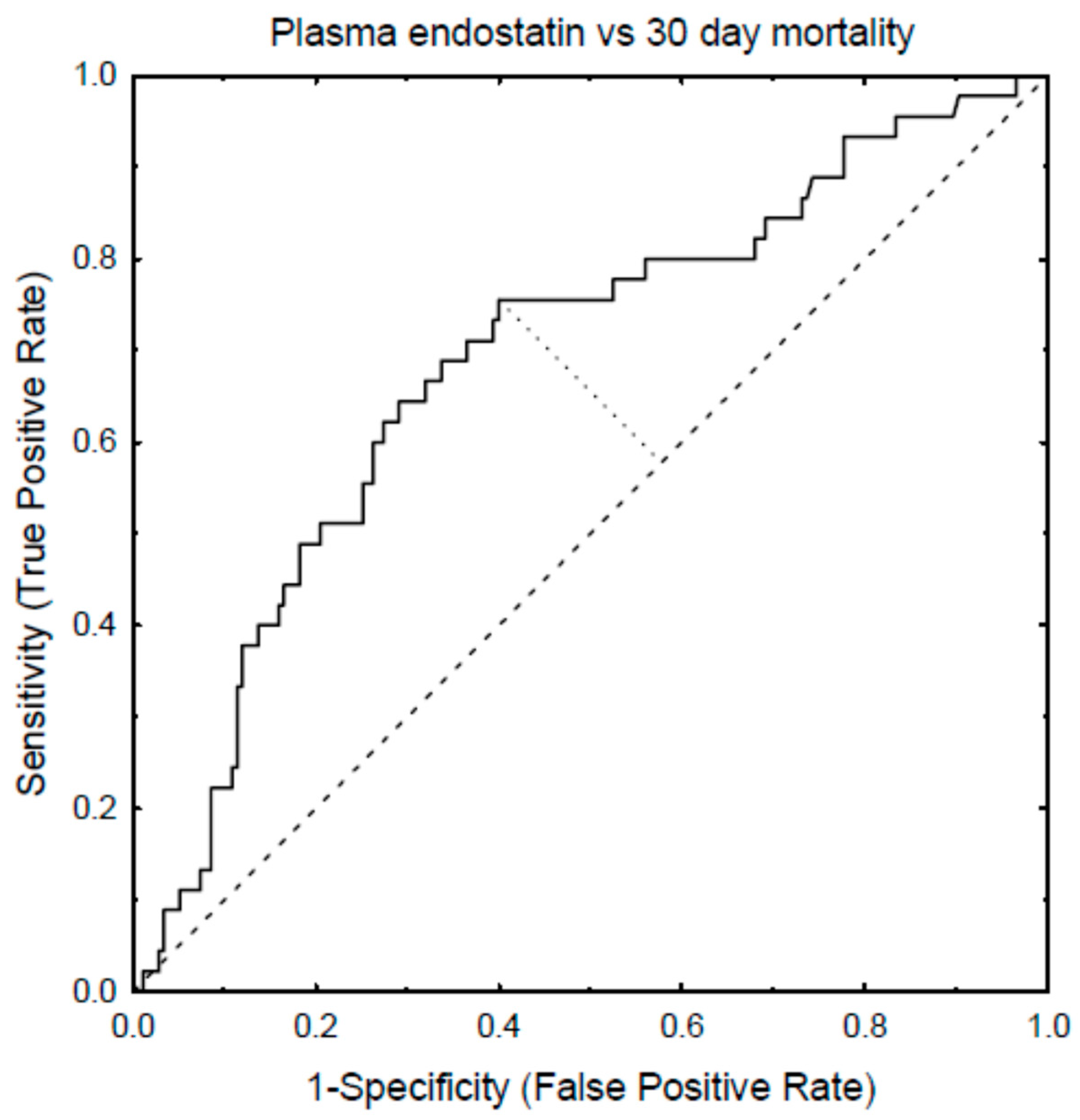
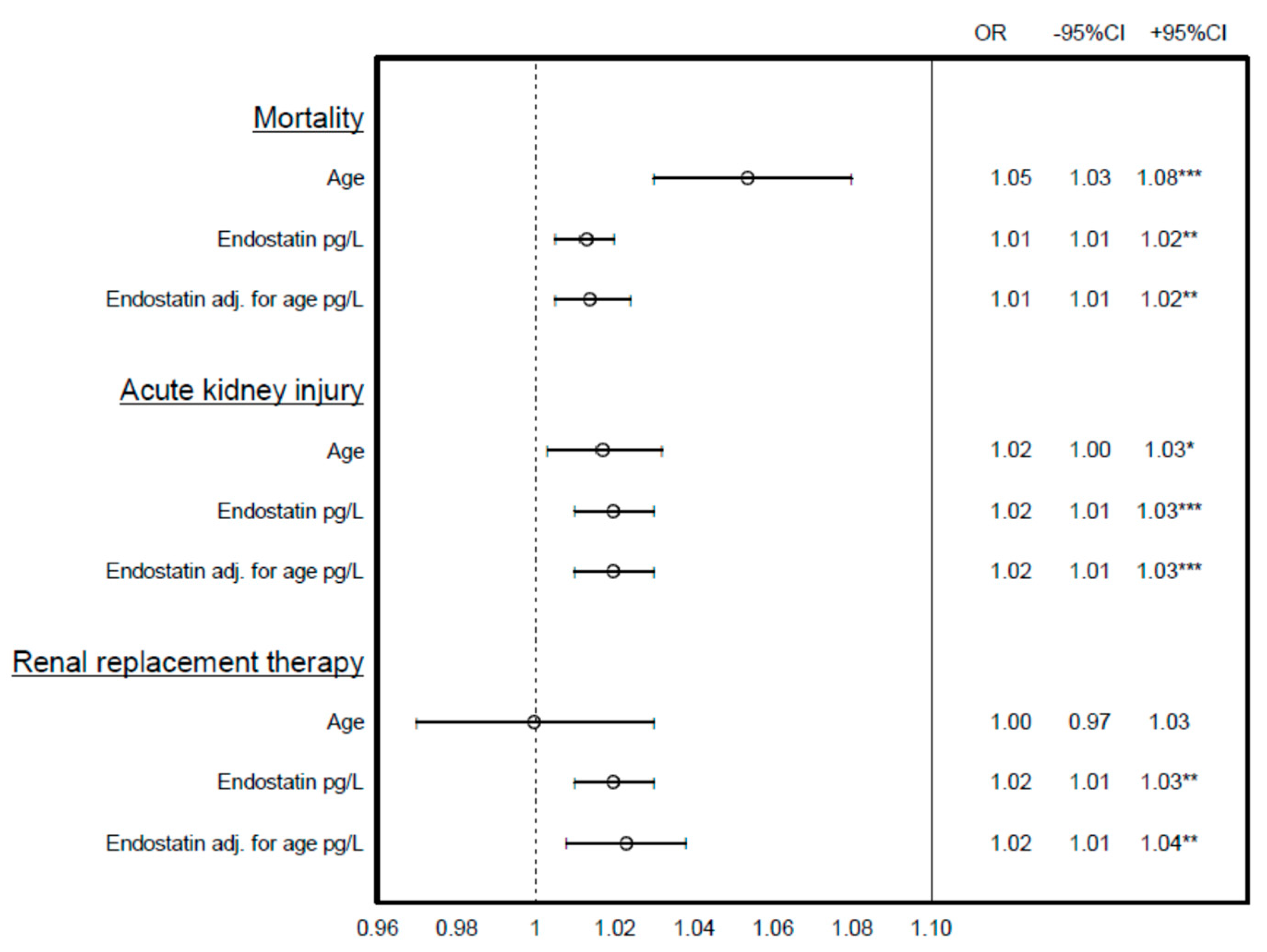
| Predictive Variable | 30-Day Mortality | AKI | RRT |
|---|---|---|---|
| Endostatin | 0.69 (0.62–0.77) | 0.68 (0.62–0.74) | 0.82 (0.72–0.91) |
| SAPS3 | 0.85 (0.80–0.90) | 0.65 (0.58–0.72) | 0.67 (0.52–0.82) |
| Age and Endostatin | 0.76 (0.70–0.82) | 0.70 (0.64–0.76) | 0.81 (0.71–0.91) |
| Age, Endostatin and creatinine | 0.76 (0.70–0.82) | 0.87 (0.83–0.91) | N.A. |
| Age and creatinine | 0.71 (0.64–0.78) | 0.86 (0.82–0.90) | N.A. |
| Age | 0.71 (0.64–0.77) | 0.57 (0.50–0.64) | 0.59 (0.42–0.76) |
| Creatinine | 0.64 (0.57–0.71) | 0.86 (0.82–0.90) | 0.91 (0.85–0.97) |
| Non-RRT | RRT | p-Value | |||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| SAPS3 | 58 | 48–69 | 71 | 56–75 | n.s. |
| Age | 68 | 54–76 | 66 | 53–72 | n.s. |
| Creatinine | 84 | 62–119 | 288 | 154–495 | p < 0.001 |
| Endostatin | 45.4 | 28.6–67.4 | 87.3 | 68.3–144.2 | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruge, T.; Larsson, A.; Lipcsey, M.; Tydén, J.; Johansson, J.; Eriksson, M. A Comparison between Endostatin and Conventional Biomarkers on 30-Day Mortality and Renal Replacement Therapy in Unselected Intensive Care Patients. Biomedicines 2021, 9, 1603. https://doi.org/10.3390/biomedicines9111603
Ruge T, Larsson A, Lipcsey M, Tydén J, Johansson J, Eriksson M. A Comparison between Endostatin and Conventional Biomarkers on 30-Day Mortality and Renal Replacement Therapy in Unselected Intensive Care Patients. Biomedicines. 2021; 9(11):1603. https://doi.org/10.3390/biomedicines9111603
Chicago/Turabian StyleRuge, Toralph, Anders Larsson, Miklós Lipcsey, Jonas Tydén, Joakim Johansson, and Mats Eriksson. 2021. "A Comparison between Endostatin and Conventional Biomarkers on 30-Day Mortality and Renal Replacement Therapy in Unselected Intensive Care Patients" Biomedicines 9, no. 11: 1603. https://doi.org/10.3390/biomedicines9111603
APA StyleRuge, T., Larsson, A., Lipcsey, M., Tydén, J., Johansson, J., & Eriksson, M. (2021). A Comparison between Endostatin and Conventional Biomarkers on 30-Day Mortality and Renal Replacement Therapy in Unselected Intensive Care Patients. Biomedicines, 9(11), 1603. https://doi.org/10.3390/biomedicines9111603








