Nutritional Supplementation Concurrent with Nutrition Education Accelerates the Wound Healing Process in Patients with Diabetic Foot Ulcers
Abstract
1. Introduction
2. Experimental Section
2.1. Screening and Recruitment
2.2. Study Design and Data Collection
2.3. Intervention/Treatment
2.4. Measurements
2.5. Dietary Assessment
2.6. Wound Measurement and Characterization
2.7. The Wound Healing Rate = (Current Area-Baseline Area)/Time (Number of Weeks) Endpoints
2.8. Statistical Analysis
2.9. Data and Resource Availability
3. Results
3.1. General Characteristics
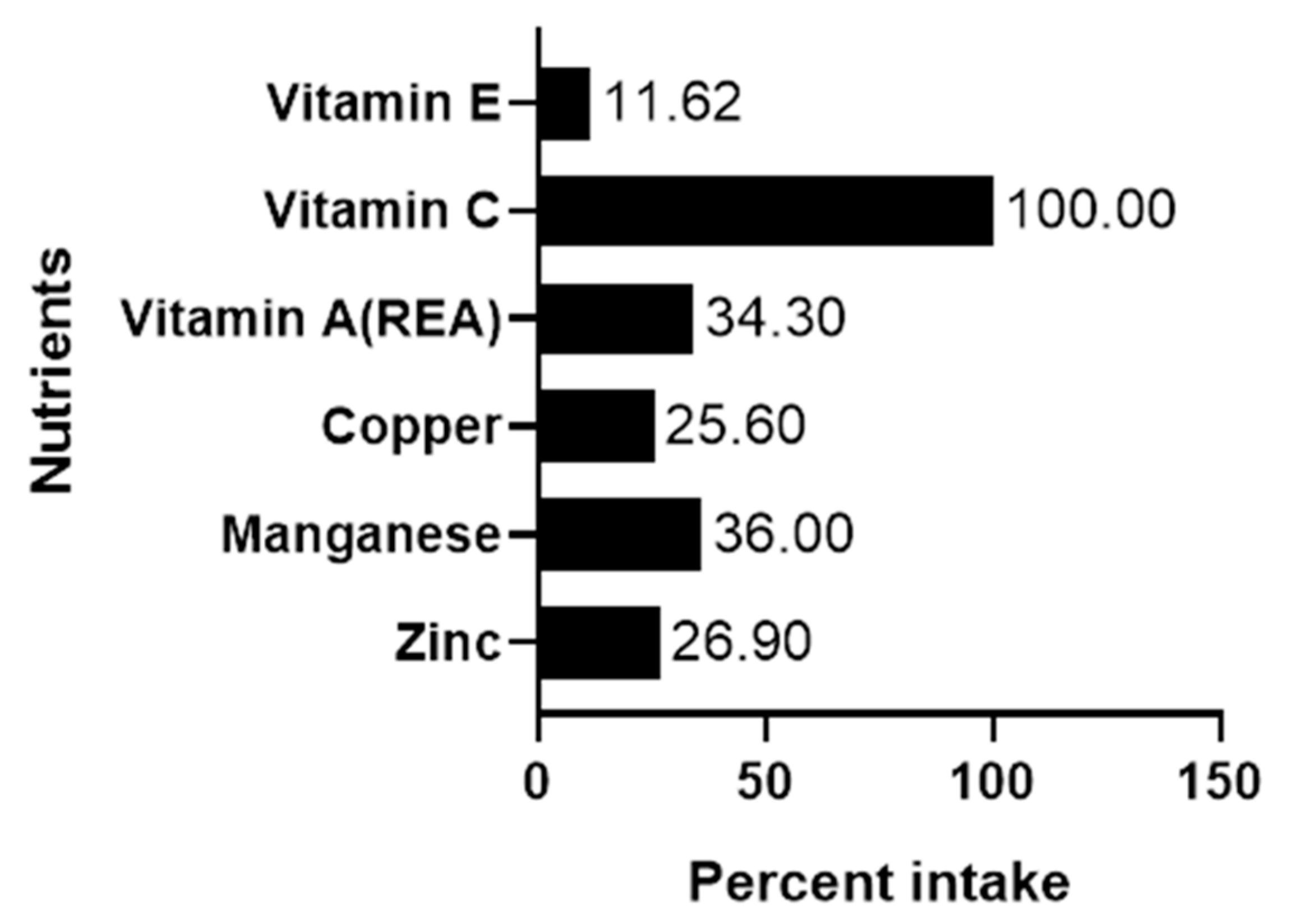
3.2. Dietary Intake of Participants at Baseline
3.3. Change in Dietary Intake of Participants During the Study
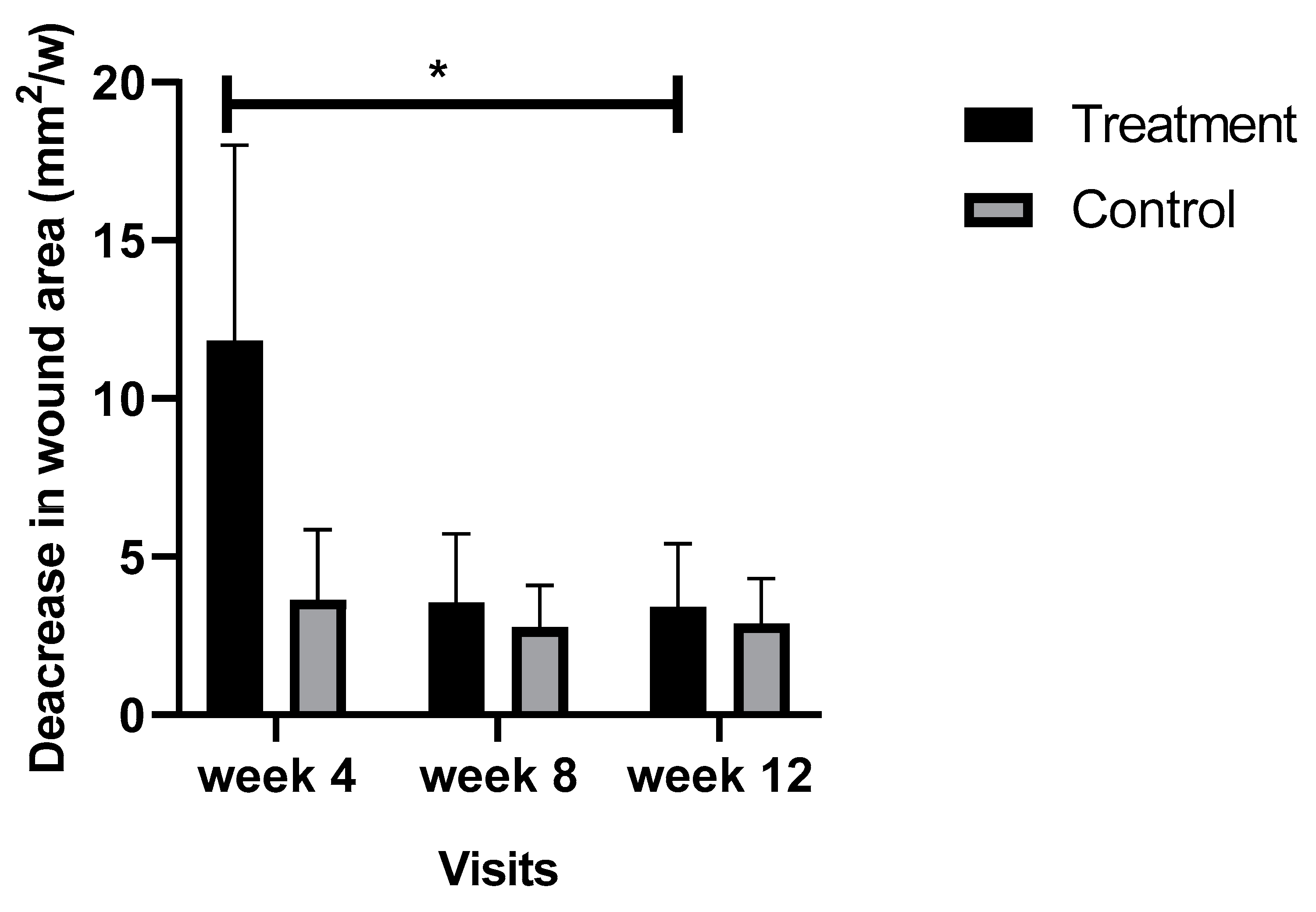
3.4. Comparison of the Wound Healing Rate between Groups
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Nutrient | Amount |
|---|---|
| Calories (kcal) | 250 |
| Calories from fat (kcal) | 110 |
| Total Fat (g) | 12 |
| Saturated Fat (g) | 1.5 |
| Trans Fat (g) | 0 |
| Cholesterol (mg) | <5 |
| Sodium (mg) | 270 |
| Potassium (mg) | 260 |
| Total Carbohydrate (g) | 23 |
| Dietary Fiber (g) | 3 |
| Sugars (g) | 6 |
| Protein * (g) | 14 |
| Vitamin A ** (IU) | 1250 |
| Vitamin C (mg) | 102 |
| Calcium (mg) | 250 |
| Iron (mg) | 3.6 |
| Vitamin D (IU) | 240 |
| Vitamin E (IU) | 33 |
| Vitamin K (mcg) | 16 |
| Thiamin (mg) | 0.3 |
| Riboflavin (mg) | 0.34 |
| Niacin (mg) | 4 |
| Vitamin B6 (mg) | 0.4 |
| Folic Acid (mcg) | 80 |
| Vitamin B12 (mcg) | 1.2 |
| Biotin (mcg) | 60 |
| Pantothenic Acid (mg) | 2 |
| Phosphorus (mg) | 200 |
| Iodine (mcg) | 30 |
| Magnesium (mg) | 80 |
| Zinc (mg) | 3 |
| Selenium (mcg) | 14 |
| Copper (mg) | 0.4 |
| Manganese (mg) | 0.4 |
| Chromium (mcg) | 24 |
| Molybdenum (mcg) | 15 |
| Chloride (mg) | 204 |
| L-carnitine (mg) | 25 |
| Taurine (mg) | 20 |
| Inositol (mg) | 200 |
References
- Zhang, P.; Lu, J.; Jing, Y.; Tang, S.; Zhu, D.; Bi, Y. Global epidemiology of diabetic foot ulceration: A systematic review and meta-analysis. Ann. Med. 2017, 49, 106–116. [Google Scholar] [CrossRef]
- CDC. CDC Press Releases. 2016. Available online: https://www.cdc.gov/media/releases/2017/p0718-diabetes-report.html (accessed on 7 March 2019).
- Raghav, A.; Khan, Z.A.; Labala, R.K.; Ahmad, J.; Noor, S.; Mishra, B.K. Financial burden of diabetic foot ulcers to world: A progressive topic to discuss always. Ther. Adv. Endocrinol. Metab. 2018, 9, 29–31. [Google Scholar] [CrossRef] [PubMed]
- Maier, H.M.; Ilich-Ernst, J.; Arjmandi, B.; Kim, J.-S.; Spicer, M. Deficiencies in Nutritional Intake in Patients with Diabetic Foot Ulcers. J. Nutr. Ther. 2016, 5, 85–92. [Google Scholar] [CrossRef]
- Sajid, N.; Miyan, Z.; Zaidi, S.I.H.; Jaffri, S.S.A.; AbdeAli, M. Protein requirement and its intake in subjects with diabetic foot ulcers at a tertiary care hospital. Pak. J. Med. Sci. 2018, 34, 886–890. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.-S.; Tang, Z.-Y.; Fang, P.; Qian, H.-J.; Xu, L.; Ning, G. Nutritional status deteriorates as the severity of diabetic foot ulcers increases and independently associates with prognosis. Exp. Ther. Med. 2013, 5, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Gau, B.-R.; Chen, H.-Y.; Hung, S.-Y.; Yang, H.M.; Yeh, J.T.; Huang, C.H.; Sun, J.H.; Huang, Y.Y. The impact of nutritional status on treatment outcomes of patients with limb-threatening diabetic foot ulcers. J. Diabetes Complicat. 2016, 30, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Tatti, P.; Barber, A.E. The Use of a Specialized Nutritional Supplement for Diabetic Foot Ulcers Reduces the Use of Antibiotics. J. Endocrinol. Metab. 2012, 2, 26–31. [Google Scholar] [CrossRef][Green Version]
- Sipahi, S.; Gungor, O.; Gunduz, M.; Cilci, M.; Demirci, M.C.; Tamer, A. The effect of oral supplementation with a combination of beta-hydroxy-beta-methylbutyrate, arginine and glutamine on wound healing: A retrospective analysis of diabetic haemodialysis patients. BMC Nephrol. 2013, 14, 8. [Google Scholar] [CrossRef]
- Afzali, H.; Jafari Kashi, A.H.; Momen-Heravi, M.; Razzaghi, R.; Amirani, E.; Bahmani, F.; Gilasi, H.R.; Asemi, Z. The effects of magnesium and vitamin E co-supplementation on wound healing and metabolic status in patients with diabetic foot ulcer: A randomized, double-blind, placebo-controlled trial. Wound Repair Regen. 2019, 27, 277–284. [Google Scholar] [CrossRef]
- Oyibo, S.O.; Jude, E.B.; Tarawneh, I.; Nguyen, H.C.; Harkless, L.B.; Boulton, A.J.M. A Comparison of Two Diabetic Foot Ulcer Classification Systems: The Wagner and the University of Texas wound classification systems. Diabetes Care 2001, 24, 84–88. [Google Scholar] [CrossRef]
- Arrendale, J.R.; Cherian, S.E.; Zineh, I.; Chirico, M.J.; Taylor, J.R. Assessment of Glycated Hemoglobin Using A1CNow+TM Point-of-Care Device as Compared to Central Laboratory Testing. J. Diabetes Sci. Technol. 2008, 2, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.; Fuhrman, M.P. Nutrients and Wound Healing: Still Searching for the Magic Bullet. Nutr. Clin. Pract. 2005, 20, 331–347. [Google Scholar] [CrossRef] [PubMed]
- Stechmiller, J.K. Understanding the role of nutrition and wound healing. Nutr. Clin. Pract. 2010, 25, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Haesler, E. (Ed.) National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. In Prevention and Treatment of Pressure Ulcers: Quick Reference Guide; Cambridge Media: Osborne Park, Australia, 2014. [Google Scholar]
- Razzaghi, R.; Pidar, F.; Momen-Heravi, M.; Bahmani, F.; Akbari, H.; Asemi, Z. Magnesium Supplementation and the Effects on Wound Healing and Metabolic Status in Patients with Diabetic Foot Ulcer: A Randomized, Double-Blind, Placebo-Controlled Trial. Biol. Trace Elem. Res. 2018, 181, 207–215. [Google Scholar] [CrossRef]
- Cereda, E.; Klersy, C.; Serioli, M.; Crespi, A.; D’Andrea, F. OligoElement Sore Trial Study Group. A nutritional formula enriched with arginine, zinc, and antioxidants for the healing of pressure ulcers: A randomized trial. Ann. Intern. Med. 2015, 162, 167–174. [Google Scholar] [CrossRef]
- Cereda, E.; Gini, A.; Pedrolli, C.; Vanotti, A. Disease-Specific, Versus Standard, Nutritional Support for the Treatment of Pressure Ulcers in Institutionalized Older Adults: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2009, 57, 1395–1402. [Google Scholar] [CrossRef]
- Calder, P.C.; Albers, R.; Antoine, J.-M.; Blum, S.; Bourdet-Sicard, R.; Ferns, G.A.; Folkerts, G.; Friedmann, P.S.; Frost, G.S.; Guarner, F. Inflammatory Disease Processes and Interactions with Nutrition. Br. J. Nutr. 2009, 101, 1–45. [Google Scholar] [CrossRef]
- Guo, S.; DiPietro, L.A. Factors Affecting Wound Healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar] [CrossRef]
- Langemo, D.; Anderson, J.; Hanson, D.; Hunter, S.; Thompson, P.; Posthauer, M.E. Nutritional considerations in wound care. Adv. Skin Wound Care 2006, 19, 297–303. [Google Scholar] [CrossRef]
- Nutrient Recommendations: Dietary Reference Intakes (DRI). Available online: https://ods.od.nih.gov/Health_Information/Dietary_Reference_Intakes.aspx (accessed on 18 September 2019).
- Gould, L.; Abadir, P.; Brem, H.; Carter, M.; Conner-Kerr, T.; Davidson, J.; DiPietro, L.; Falanga, V.; Fife, C.; Gardner, S. Chronic Wound Repair and Healing in Older Adults: Current Status and Future Research. J. Am. Geriatr. Soc. 2015, 63, 427–438. [Google Scholar] [CrossRef]
- Jeffcoate, W.J.; Vileikyte, L.; Boyko, E.J.; Armstrong, D.G.; Boulton, A.J.M. Current Challenges and Opportunities in the Prevention and Management of Diabetic Foot Ulcers. Diabetes Care 2018, 41, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Niedert, K.C. American Dietetic Association. Position of the American Dietetic Association: Liberalization of the diet prescription improves quality of life for older adults in long-term care. J. Am. Diet. Assoc. 2005, 105, 1955–1965. [Google Scholar] [CrossRef] [PubMed]
- Salgado, R.M.; Cruz-Castañeda, O.; Elizondo-Vázquez, F.; Pat, L.; De la Garza, A.; Cano-Colín, S.; Baena-Ocampo, L.; Krötzsch, E. Maltodextrin/ascorbic acid stimulates wound closure by increasing collagen turnover and TGF-β1 expression in vitro and changing the stage of inflammation from chronic to acute in vivo. J. Tissue Viability 2017, 26, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Musalmah, M.; Fairuz, A.H.; Gapor, M.T.; Wan Ngah, W.Z. Effect of vitamin E on plasma malondialdehyde, antioxidant enzyme levels and the rates of wound closures during wound healing in normal and diabetic rats. Asia Pac. J. Clin. Nutr. 2002, 11, S448–S451. [Google Scholar] [CrossRef]
- Aschner, J.L.; Aschner, M. Nutritional aspects of manganese homeostasis. Mol. Aspects Med. 2005, 26, 353–362. [Google Scholar] [CrossRef]
- Das, A.; Chen, G.-F.; Kim, H.W.; Youn, S.W.; Varadarajan, S.; McKinney, R.D.; Finney, L.; Ushio-Fukai, M.; Fukai, T. Abstract 16637: Antioxidant-1, a Novel Cu-Dependent Transcription Factor for NADPH Oxidase p47phox, Promotes Wound Healing by Regulating Inflammation and Angiogenesis. Circulation 2014, 130, A16637. [Google Scholar]
- Martin, F.; Linden, T.; Katschinski, D.M.; Oehme, F.; Flamme, I.; Mukhopadhyay, C.K.; Eckhardt, K. Copper-dependent activation of hypoxia-inducible factor (HIF)-1: Implications for ceruloplasmin regulation. Blood 2005, 105, 4613–4619. [Google Scholar] [CrossRef]
- Mirastschijski, U.; Haaksma, C.J.; Tomasek, J.J.; Agren, M.S. Matrix metalloproteinase inhibitor GM 6001 attenuates keratinocyte migration, contraction and myofibroblast formation in skin wounds. Exp. Cell Res. 2004, 299, 465–475. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Hanft, J.R.; Driver, V.R.; Smith, A.P.; Lazaro-Martinez, J.L.; Reyzelman, A.M.; Furst, G.J.; Vayser, D.J.; Cervantes, H.L.; Snyder, R.J. Effect of oral nutritional supplementation on wound healing in diabetic foot ulcers: A prospective randomized controlled trial. Diabet Med. 2014, 31, 1069–1077. [Google Scholar] [CrossRef]
- Rice, J.B.; Desai, U.; Cummings, A.K.G.; Birnbaum, H.G.; Skornicki, M.; Parsons, N.B. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care 2014, 37, 651–658. [Google Scholar] [CrossRef]
- Lantis, J.C.; Boone, D.; Gendics, C.; Todd, G. Analysis of patient cost for recombinant human platelet-derived growth factor therapy as the first-line treatment of the insured patient with a diabetic foot ulcer. Adv. Skin Wound Care 2009, 22, 167–171. [Google Scholar] [CrossRef] [PubMed]


| Nutrient | Total from Supplements/Day | RDA for Nutrient | % of RDA Provided; Men vs. Women if RDA Varied for Men vs. Women |
|---|---|---|---|
| Protein | 28 g | 56 g 46 g | 50% 61% |
| Vitamin C | 204 mg | 60 mg | 304% |
| Vitamin E | 66 IU | 33.3 IU | 200% |
| Vitamin A | 2500 IU | 3000 IU | 83% |
| Zinc | 6 mg | men: 11 mg women: 8 mg | 54% 75% |
| Copper | 0.8 mg | 0.9 mg | 88% |
| Manganese ** | 0.8 mg | men: 2.3 mg women: 1.8 mg | 35% 44% |
| Groups | Treatment | Control | p-Value |
|---|---|---|---|
| N | 15 | 14 | -- |
| Men/women | 8/7 | 11/3 | -- |
| Age (year) | |||
| Means ± SD | 52.93 ± 9.74 | 53.79 ± 12.84 | |
| Median | 54 | 55 | 0.84 |
| Interquartile range | 12 | 21 | |
| Ethnicity | |||
| African American | 4 | 3 | 0.75 |
| White | 11 | 11 | |
| BMI * (kg/m2) | |||
| Means ± SD | 33.54 ± 7.98 | 34.07 ± 6.04 | |
| Median | 31.1 | 34.5 | 0.84 |
| Interquartile range | 16.7 | 18.4 | |
| Diabetes duration (years) | |||
| Means ± SD | 14.40 ± 8.03 | 11.71 ± 6.17 | 0.32 |
| Median | 12 | 12 | |
| Interquartile range | 10 | 12 | |
| Wound age estimation (months) | |||
| Means ± SD | 10.97 ± 15.09 | 10.58 ± 18.27 | |
| Median | 6 | 6 | 0.95 |
| Interquartile range | 10 | 9.5 | |
| HbA1C ** | |||
| Means ± SD | 7.95 ± 2.06 | 8.40 ± 2.16 | |
| Median | 7.3 | 8.8 | 0.57 |
| Interquartile range | 2.5 | 4.4 | |
| Dietary restrictions (yes/no) | 2/13 | 1/13 | 1 |
| Appetite problem (yes/no) | 1/14 | 1/13 | 1 |
| Visited RD *** (yes/no) | 7/8 | 3/11 | 0.3 |
| Unintentional weight loss (yes/no) | 4/11 | 1/13 | 0.32 |
| living alone (yes/no) | 3/12 | 4/10 | 0.6 |
| Having financial support (yes/no) | 11/4 | 11/3 | 0.75 |
| Employed (yes/no) | 4/11 | 6/8 | 0.37 |
| Having financial concern (yes/no) | 6/9 | 3/11 | 0.3 |
| Need food (yes/no) | 2/13 | 1/13 | 0.6 |
| Smoke (yes/no) | 3/12 | 3/12 | 1 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basiri, R.; Spicer, M.T.; Levenson, C.W.; Ormsbee, M.J.; Ledermann, T.; Arjmandi, B.H. Nutritional Supplementation Concurrent with Nutrition Education Accelerates the Wound Healing Process in Patients with Diabetic Foot Ulcers. Biomedicines 2020, 8, 263. https://doi.org/10.3390/biomedicines8080263
Basiri R, Spicer MT, Levenson CW, Ormsbee MJ, Ledermann T, Arjmandi BH. Nutritional Supplementation Concurrent with Nutrition Education Accelerates the Wound Healing Process in Patients with Diabetic Foot Ulcers. Biomedicines. 2020; 8(8):263. https://doi.org/10.3390/biomedicines8080263
Chicago/Turabian StyleBasiri, Raedeh, Maria T. Spicer, Cathy W. Levenson, Michael J. Ormsbee, Thomas Ledermann, and Bahram H. Arjmandi. 2020. "Nutritional Supplementation Concurrent with Nutrition Education Accelerates the Wound Healing Process in Patients with Diabetic Foot Ulcers" Biomedicines 8, no. 8: 263. https://doi.org/10.3390/biomedicines8080263
APA StyleBasiri, R., Spicer, M. T., Levenson, C. W., Ormsbee, M. J., Ledermann, T., & Arjmandi, B. H. (2020). Nutritional Supplementation Concurrent with Nutrition Education Accelerates the Wound Healing Process in Patients with Diabetic Foot Ulcers. Biomedicines, 8(8), 263. https://doi.org/10.3390/biomedicines8080263






