Novel Medicine for Endometriosis and Its Therapeutic Effect in a Mouse Model
Abstract
:1. Introduction
2. Experimental Section
2.1. Animals
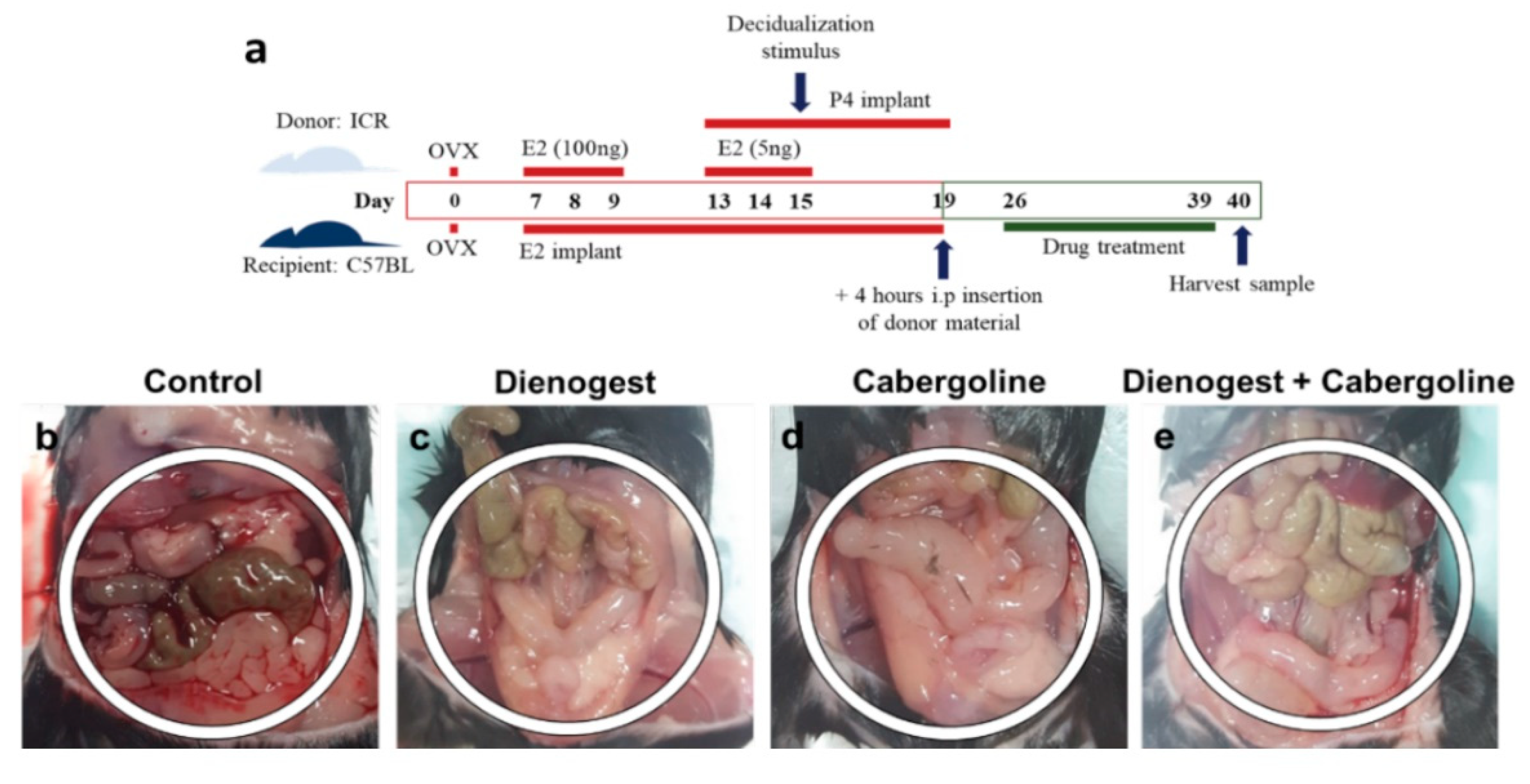
2.2. In Vivo Model of Endometriosis
2.3. Histological Study
2.4. Immunohistochemistry Study
2.5. RT-PCR and Real-Time qPCR for Gene Expression Analysis
2.6. Western Blotting for Protein Expression Analysis
2.7. Statistical Analyses
3. Results
3.1. Gross Findings of the Pelvic Cavity
3.2. Histological Study of the Endometriosis Animal Model
3.3. Immunohistochemistry Data
3.4. Gene Expression Analysis by RT-PCR and Real-Time qPCR
3.5. Protein Expression Analysis by Western Blotting
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Giudice, L.C. Clinical practice. Endometriosis. N. Engl. J. Med. 2010, 362, 2389–2398. [Google Scholar] [CrossRef]
- Giudice, L.C.; Kao, L.C. Endometriosis. Lancet 2004, 364, 1789–1799. [Google Scholar] [CrossRef]
- Bergqvist, A.; Bergquist, C.; Nordenskjold, F. Current aspects on the treatment of endometriosis. Lakartidningen 2000, 97, 818–822. [Google Scholar] [PubMed]
- Felberbaum, R.E.; Ludwig, M.; Diedrich, K. Clinical application of GnRH-antagonists. Mol. Cell Endocrinol. 2000, 166, 9–14. [Google Scholar] [CrossRef]
- Keckstein, J. Surgical therapy of endometriosis. Wien Med. Wochenschr. 1999, 149, 366–371. [Google Scholar] [PubMed]
- Rimbach, S.; Ulrich, U.; Schweppe, K.W. Surgical Therapy of Endometriosis: Challenges and Controversies. Geburtshilfe Frauenheilkd. 2013, 73, 918–923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Somigliana, E.; Busnelli, A.; Benaglia, L.; Viganò, P.; Leonardi, M.; Paffoni, A.; Vercellini, P. Postoperative hormonal therapy after surgical excision of deep endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 209, 77–80. [Google Scholar] [CrossRef]
- Somigliana, E.; Vercellini, P.; Vigano, P.; Benaglia, L.; Busnelli, A.; Fedele, L. Postoperative medical therapy after surgical treatment of endometriosis: From adjuvant therapy to tertiary prevention. J. Minim. Invasive Gynecol. 2014, 21, 328–334. [Google Scholar] [CrossRef]
- Vercellini, P.; Somigliana, E.; Vigano, P.; Abbiati, A.; Barbara, G.; Crosignani, P.G. Endometriosis: Current therapies and new pharmacological developments. Drugs 2009, 69, 649–675. [Google Scholar] [CrossRef]
- Ferrero, S.; Ragni, N.; Remorgida, V. Antiangiogenic therapies in endometriosis. Br. J. Pharmacol. 2006, 149, 133–135. [Google Scholar] [CrossRef] [Green Version]
- Parazzini, F.; Ferraroni, M.; Bocciolone, L.; Tozzi, L.; Rubessa, S.; La Vecchia, C. Contraceptive methods and risk of pelvic endometriosis. Contraception 1994, 49, 47–55. [Google Scholar] [CrossRef]
- Pavone, M.E.; Bulun, S.E. Aromatase inhibitors for the treatment of endometriosis. Fertil. Steril. 2012, 98, 1370–1379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prentice, A.; Deary, A.J.; Goldbeck-Wood, S.; Farquhar, C.; Smith, S.K. Gonadotrophin-releasing hormone analogues for pain associated with endometriosis. Cochrane Database Syst Rev. 2000, CD000346. [Google Scholar] [CrossRef] [PubMed]
- Roman, H. Oral contraceptives and endometriosis. Hum. Reprod. 2011, 26, 1600–1601. [Google Scholar] [CrossRef] [Green Version]
- Barra, F.; Scala, C.; Ferrero, S. Elagolix sodium for the treatment of women with moderate to severe endometriosis-associated pain. Drugs Today 2019, 55, 237–246. [Google Scholar] [CrossRef]
- Rice, V.M. Conventional medical therapies for endometriosis. Ann. N. Y. Acad. Sci. 2002, 955, 343–352. [Google Scholar] [CrossRef]
- Della Corte, L.; Noventa, M.; Ciebiera, M.; Magliarditi, M.; Sleiman, Z.; Karaman, E.; Catena, U.; Salvaggio, C.; Falzone, G.; Garzon, S. Phytotherapy in endometriosis: An up-to-date review. J. Complement. Integr. Med. 2020, 7. [Google Scholar] [CrossRef]
- Kobayashi, H.; Yamada, Y.; Morioka, S.; Niiro, E.; Shigemitsu, A.; Ito, F. Mechanism of pain generation for endometriosis-associated pelvic pain. Arch. Gynecol. Obstet. 2014, 289, 13–21. [Google Scholar] [CrossRef]
- Mechsner, S.; Kaiser, A.; Kopf, A.; Gericke, C.; Ebert, A.; Bartley, J. A pilot study to evaluate the clinical relevance of endometriosis-associated nerve fibers in peritoneal endometriotic lesions. Fertil. Steril. 2009, 92, 1856–1861. [Google Scholar] [CrossRef]
- Yao, H.J.; Huang, X.F.; Lu, B.C.; Zhou, C.Y.; Zhang, J.; Zhang, X.M. Protein gene product 9.5-immunoactive nerve fibers and its clinical significance in endometriotic peritoneal lesions. Zhonghua Fu Chan Ke Za Zhi 2010, 45, 256–259. [Google Scholar]
- Barcena de Arellano, M.L.; Arnold, J.; Vercellino, F.; Chiantera, V.; Schneider, A.; Mechsner, S. Overexpression of nerve growth factor in peritoneal fluid from women with endometriosis may promote neurite outgrowth in endometriotic lesions. Fertil. Steril. 2011, 95, 1123–1126. [Google Scholar] [CrossRef] [PubMed]
- Tokushige, N.; Markham, R.; Russell, P.; Fraser, I.S. Effects of hormonal treatment on nerve fibers in endometrium and myometrium in women with endometriosis. Fertil. Steril. 2008, 90, 1589–1598. [Google Scholar] [CrossRef] [PubMed]
- Tokushige, N.; Markham, R.; Russell, P.; Fraser, I.S. Effect of progestogens and combined oral contraceptives on nerve fibers in peritoneal endometriosis. Fertil. Steril. 2009, 92, 1234–1239. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, K.; Llarena, N.C.; Rehmer, J.M.; Richards, E.G.; Falcone, T. The role of pharmacotherapy in the treatment of endometriosis across the lifespan. Expert Opin. Pharmacother. 2020, 21, 893–903. [Google Scholar] [CrossRef]
- Vercellini, P.; Buggio, L.; Frattaruolo, M.P.; Borghi, A.; Dridi, D.; Somigliana, E. Medical treatment of endometriosis-related pain. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 51, 68–91. [Google Scholar] [CrossRef]
- Healy, D.L.; Rogers, P.A.; Hii, L.; Wingfield, M. Angiogenesis: A new theory for endometriosis. Hum. Reprod. Update 1998, 4, 736–740. [Google Scholar] [CrossRef] [Green Version]
- Rocha, A.L.; Reis, F.M.; Taylor, R.N. Angiogenesis and endometriosis. Obstet. Gynecol. Int. 2013, 2013, 859619. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.; He, Y.L. Study of an antiangiogenesis gene therapy with endostatin on endometriosis in the nude mouse model. Clin. Exp. Obstet. Gynecol. 2014, 41, 328–334. [Google Scholar]
- Zheng, W.; Cao, L.; Xu, Z.; Ma, Y.; Liang, X. Anti-Angiogenic Alternative and Complementary Medicines for the Treatment of Endometriosis: A Review of Potential Molecular Mechanisms. Evid. Based Complement. Altern. Med. 2018, 2018, 4128984. [Google Scholar] [CrossRef] [Green Version]
- Olivares, C.N.; Ricci, A.; Bilotas, M.; Barañao, R.I.; Meresman, G. The inhibitory effect of celecoxib and rosiglitazone on experimental endometriosis. Fertil. Steril. 2011, 96, 428–433. [Google Scholar] [CrossRef]
- Ercan, C.M.; Kayaalp, O.; Cengiz, M.; Keskin, U.; Yumusak, N.; Aydogan, U.; Ide, T.; Ergün, A. Comparison of efficacy of bromocriptine and cabergoline to GnRH agonist in a rat endometriosis model. Arch. Gynecol. Obstet. 2014, 291, 1103–1111. [Google Scholar] [CrossRef] [PubMed]
- McCormack, P.L. Dienogest: A review of its use in the treatment of endometriosis. Drugs 2010, 70, 2073–2088. [Google Scholar] [CrossRef] [PubMed]
- Tarjanne, S.; Ng, C.H.; Manconi, F.; Arola, J.; Mentula, M.; Maneck, B.; Fraser, I.S.; Heikinheimo, O. Use of hormonal therapy is associated with reduced nerve fiber density in deep infiltrating, rectovaginal endometriosis. Acta Obstet. Gynecol. Scand. 2015, 94, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Novella-Maestre, E.; Carda, C.; Noguera, I.; Ruiz-Saurí, A.; García-Velasco, J.A.; Simón, C.; Pellicer, A. Dopamine agonist administration causes a reduction in endometrial implants through modulation of angiogenesis in experimentally induced endometriosis. Hum. Reprod. 2009, 24, 1025–1035. [Google Scholar] [CrossRef] [Green Version]
- Delgado-Rosas, F.; Gómez, R.; Ferrero, H.; Gaytan, F.; Garcia-Velasco, J.; Simón, C.; Pellicer, A. The effects of ergot and non-ergot-derived dopamine agonists in an experimental mouse model of endometriosis. Reproduction 2011, 142, 745–755. [Google Scholar] [CrossRef] [Green Version]
- Laschke, M.W.; Menger, M.D. Anti-angiogenic treatment strategies for the therapy of endometriosis. Hum. Reprod. Update 2012, 18, 682–702. [Google Scholar] [CrossRef] [Green Version]
- Novella-Maestre, E.; Herraiz, S.; Vila-Vives, J.M.; Carda, C.; Ruiz-Sauri, A.; Pellicer, A. Effect of antiangiogenic treatment on peritoneal endometriosis-associated nerve fibers. Fertil. Steril. 2012, 98, 1209–1217. [Google Scholar] [CrossRef]
- Greaves, E.; Cousins, F.L.; Murray, A.; Esnal-Zufiaurre, A.; Fassbender, A.; Horne, A.W.; Saunders, P.T. A novel mouse model of endometriosis mimics human phenotype and reveals insights into the inflammatory contribution of shed endometrium. Am. J. Pathol. 2014, 184, 1930–1939. [Google Scholar] [CrossRef] [Green Version]
- Barra, F.; Laganà, A.S.; Scala, C.; Garzon, S.; Ghezzi, F.; Ferrero, S. Pretreatment with dienogest in women with endometriosis undergoing IVF after a previous failed cycle. Reprod. Biomed. Online 2020, 41, 859–868. [Google Scholar] [CrossRef]
- Andres, M.P.; Lopes, L.A.; Baracat, E.C.; Podgaec, S. Dienogest in the treatment of endometriosis: Systematic review. Arch. Gynecol. Obstet. 2015, 292, 523–529. [Google Scholar] [CrossRef]
- Hamid, A.M.S.A.; Madkour, W.A.I.; Moawad, A.; Elzaher, M.A.; Roberts, M.P. Does Cabergoline help in decreasing endometrioma size compared to LHRH agonist? A prospective randomized study. Arch. Gynecol. Obstet. 2014, 290, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Paterni, I.; Granchi, C.; Katzenellenbogen, J.A.; Minutolo, F. Estrogen receptors alpha (ER alpha) and beta (ERbeta): Subtype-selective ligands and clinical potential. Steroids 2014, 90, 13–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jia, M.; Dahlman-Wright, K.; Gustafsson, J.A. Estrogen receptor alpha and beta in health and disease. Best Pract. Res. Clin. Endocrinol. Metab. 2015, 29, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Trukhacheva, E.; Lin, Z.; Reierstad, S.; Cheng, Y.H.; Milad, M.; Bulun, S.E. Estrogen receptor (ER) beta regulates ER alpha expression in stromal cells derived from ovarian endometriosis. J. Clin. Endocrinol. Metab. 2009, 94, 615–622. [Google Scholar] [CrossRef]
- Bulun, S.E.; Monsavais, D.; Pavone, M.E.; Dyson, M.; Xue, Q.; Attar, E.; Tokunaga, H.; Su, E.J. Role of estrogen receptor-β in endometriosis. Semin Reprod. Med. 2012, 30, 39–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borghese, B.; Vaiman, D.; Mondon, F.; De Ziegler, D.; Chapron, C. Neurotrophins and pain in endometriosis. Gynecol. Obstet. Fertil. 2010, 38, 442–446. [Google Scholar] [CrossRef] [PubMed]
- Anaf, V.; Simon, P.; El Nakadi, I.; Fayt, I.; Simonart, T.; Buxant, F.; Noel, J.-C. Hyperalgesia, nerve infiltration and nerve growth factor expression in deep adenomyotic nodules, peritoneal and ovarian endometriosis. Hum. Reprod. 2002, 17, 1895–1900. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Fu, X.; Wu, T.; Yang, L.; Hu, C.; Wu, R. Role of Interleukin-6 and Its Receptor in Endometriosis. Med. Sci. Monit. 2017, 23, 3801–3807. [Google Scholar] [CrossRef] [Green Version]
- Margari, K.M.; Zafiropoulos, A.; Hatzidaki, E.; Giannakopoulou, C.; Arici, A.; Matalliotakis, I. Peritoneal fluid concentrations of beta-chemokines in endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 169, 103–107. [Google Scholar] [CrossRef]
- Garzon, S.; Laganà, A.S.; Barra, F.; Casarin, J.; Cromi, A.; Raffaelli, R.; Uccella, S.; Franchi, M.; Ghezzi, F.; Ferrero, S. Novel drug delivery methods for improving efficacy of endometriosis treatments. Expert Opin. Drug Deliv. 2020, 1–13. [Google Scholar] [CrossRef]




| Gene | Forward Primer | Reverse Primer |
|---|---|---|
| Er-α | TCC CTG ATG TCA ATT GCC CT | ATG GTG GGA TCT GTG AGG TG |
| Er-β | GCC AAC CTC CTG ATG CTT CT | TGT GAC TGG AGG TTC TGG GA |
| Ccl2 | AGC CAA CTC TCA CTG AAG CC | GGA CCC ATT CCT TCT TGG GG |
| Ccl5 | CAA GTG TGT GCC AAC CCA GA | CAA GCT GGC TAG GAC TAG AGC |
| Il-6 | CCC CAA TTT CCA ATG CTC TCC | CGC ACT AGG TTT GCC GAG TA |
| Gapdh | TGT GAA CGG ATT TGG CCG TA | ACT GTG CCG TTG AAT TTG CC |
| Positive Inflammatory Lesions Mice Ratio (%) | No Inflammatory Mice Ration (%) | |
|---|---|---|
| Control | 93.33 * | 6.66 |
| Dienogest | 6.66 * | 93.33 |
| Cabergoline | 0 * | 100 |
| Dienogest + Cabergoline | 0 * | 100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.S.; Kim, Y.J.; Kim, M.J.; Lee, S.J.; Kwon, H.; Lee, J.H. Novel Medicine for Endometriosis and Its Therapeutic Effect in a Mouse Model. Biomedicines 2020, 8, 619. https://doi.org/10.3390/biomedicines8120619
Kim YS, Kim YJ, Kim MJ, Lee SJ, Kwon H, Lee JH. Novel Medicine for Endometriosis and Its Therapeutic Effect in a Mouse Model. Biomedicines. 2020; 8(12):619. https://doi.org/10.3390/biomedicines8120619
Chicago/Turabian StyleKim, Young Sang, Yu Jin Kim, Myung Joo Kim, Sang Jin Lee, Hwang Kwon, and Jae Ho Lee. 2020. "Novel Medicine for Endometriosis and Its Therapeutic Effect in a Mouse Model" Biomedicines 8, no. 12: 619. https://doi.org/10.3390/biomedicines8120619
APA StyleKim, Y. S., Kim, Y. J., Kim, M. J., Lee, S. J., Kwon, H., & Lee, J. H. (2020). Novel Medicine for Endometriosis and Its Therapeutic Effect in a Mouse Model. Biomedicines, 8(12), 619. https://doi.org/10.3390/biomedicines8120619





