Tissue-Cultured Chondrocytes Survive After Irradiation in 1300 Gy Dose
Abstract
1. Introduction
2. Materials and Methods
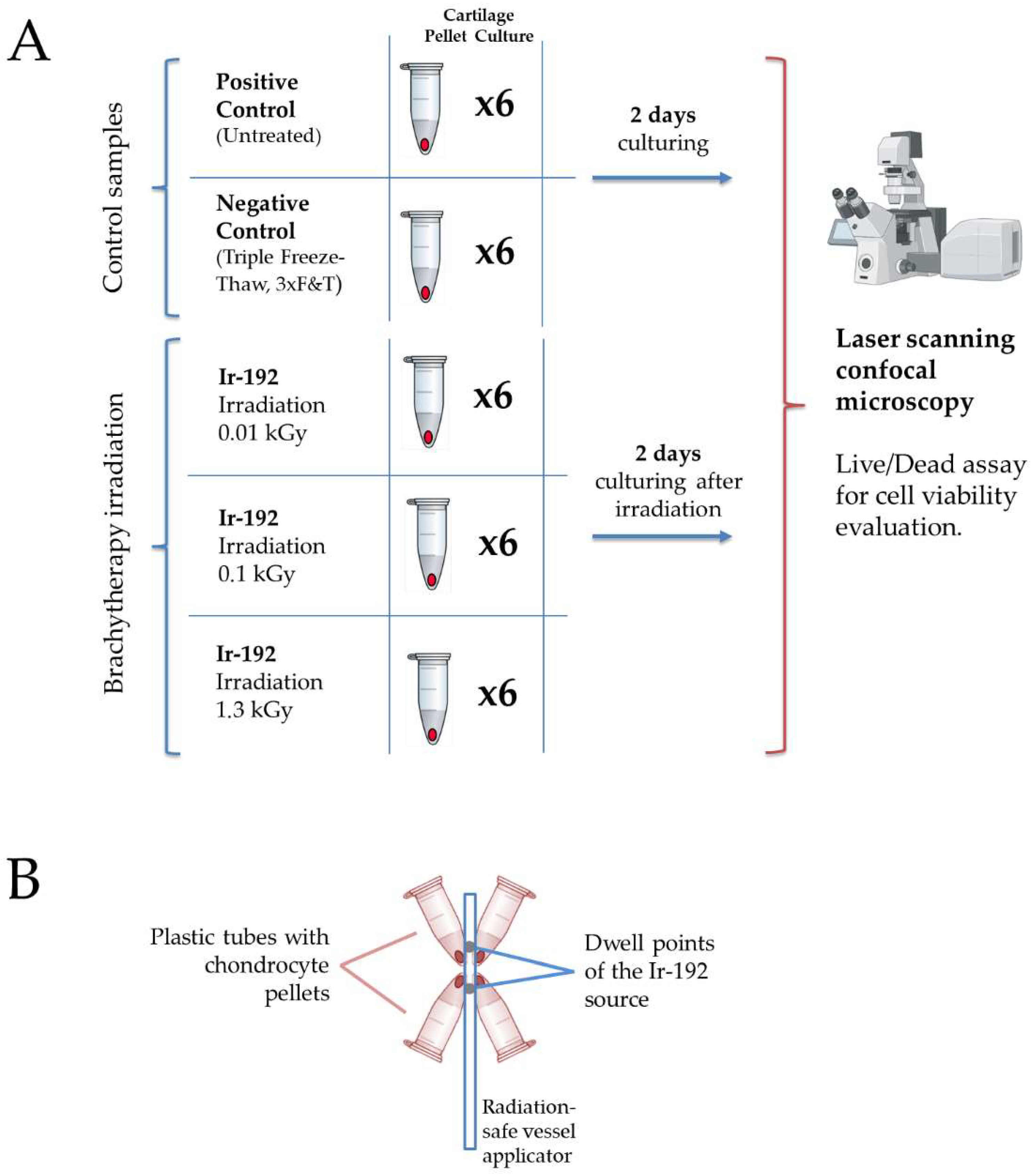
2.1. Study Design
2.2. Ionizing Irradiation
2.3. Chondrocyte Sample Derivation
2.4. Pellet Culture Chondrocytes
2.5. Cell Viability
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DNA | Deoxyribonucleic acid |
| ECM | Extracellular matrix |
References
- Datta, R.; Saha, S. Quantitative determination of tolerance doses for preoperative and postoperative radiotherapy of bones. Med. Phys. 1983, 10, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Minafra, L.; Bravatà, V. Cell and molecular response to IORT treatment. Transl. Cancer Res. 2014, 3, 32–47. [Google Scholar] [CrossRef]
- Chen, Y.; Sun, X.; Peng, Y.; Eichenbaum, J.V.; Ren, L.; Liu, Y. Effects of different radiation sources on the performance of collagen-based corneal repair materials and macrophage polarization. ACS Omega 2022, 7, 22559–22566. [Google Scholar] [CrossRef]
- Dombrowsky, A.C.; Schauer, J.; Sammer, M.; Blutke, A.; Walsh, D.W.M.; Schwarz, B.; Bartzsch, S.; Feuchtinger, A.; Reindl, J.; Combs, S.E.; et al. Acute Skin Damage and Late Radiation-Induced Fibrosis and Inflammation in Murine Ears after High-Dose Irradiation. Cancers 2019, 11, 727. [Google Scholar] [CrossRef]
- Acheva, A.; Aerts, A.; Rombouts, C.; Baatout, S.; Salomaa, S.; Manda, K.; Kämäräinen, M. Human 3-D tissue models in radiation biology: Current status and future perspectives. Int. J. Radiat. Res. 2014, 12, 81–98. [Google Scholar]
- Jones, G.D.; Symonds, P. Molecular, cellular and tissue effects of radiotherapy. In Walter and Miller’s Textbook of Radiotherapy: Radiation Physics, Therapy and Oncology; Churchill Livingstone-Elsevier: London, UK, 2012; pp. 279–292. [Google Scholar]
- Daly, M.J. A new perspective on radiation resistance based on Deinococcus radiodurans. Nat. Rev. Microbiol. 2009, 7, 237–245. [Google Scholar] [CrossRef]
- Slade, D.; Radman, M. Oxidative stress resistance in Deinococcus radiodurans. Microbiol. Mol. Biol. Rev. 2011, 75, 133–191. [Google Scholar] [CrossRef]
- Zivanovic, Y.; Armengaud, J.; Lagorce, A.; Leplat, C.; Guérin, P.; Dutertre, M.; Anthouard, V.; Forterre, P.; Wincker, P.; Confalonieri, F. Genome analysis and genome-wide proteomics of Thermococcus gammatolerans, the most radioresistant organism known amongst the Archaea. Genome Biol. 2009, 10, R70. [Google Scholar] [CrossRef]
- Yakimova, A.O.; Nikolaeva, A.; Galanova, O.; Shestakova, V.A.; Smirnova, E.I.; Levushkina, A.; Baranovskii, D.S.; Smirnova, A.N.; Stepanenko, V.N.; Kudlay, D.A.; et al. Microbiota-Induced Radioprotection: A Novel Approach to Enhance Human Radioresistance with In-Situ Genetically Engineered Gut Bacteria. Appl. Microbiol. 2025, 5, 1. [Google Scholar] [CrossRef]
- Busato, F.; Khouzai, B.E.; Mognato, M. Biological mechanisms to reduce radioresistance and increase the efficacy of radiotherapy: State of the art. Int. J. Mol. Sci. 2022, 23, 10211. [Google Scholar] [CrossRef] [PubMed]
- White, L.J.; Keane, T.J.; Smoulder, A.; Zhang, L.; Castleton, A.A.; Reing, J.E.; Turner, N.J.; Dearth, C.L.; Badylak, S.F. The impact of sterilization upon extracellular matrix hydrogel structure and function. J. Immunol. Regen. Med. 2018, 2, 11–20. [Google Scholar] [CrossRef]
- Matsumoto, T.; Iwasaki, K.; Sugihara, H. Effects of radiation on chondrocytes in culture. Bone 1994, 15, 97–100. [Google Scholar] [CrossRef]
- Sugrue, T.; Lowndes, N.F.; Ceredig, R. Mesenchymal stromal cells: Radio-resistant members of the bone marrow. Immunol. Cell Biol. 2013, 91, 5–11. [Google Scholar] [CrossRef]
- Saintigny, Y.; Cruet-Hennequart, S.; Hamdi, D.H.; Chevalier, F.; Lefaix, J.L. Impact of therapeutic irradiation on healthy articular cartilage. Radiat. Res. 2015, 183, 135–146. [Google Scholar] [CrossRef]
- Gilbert, A.; Tudor, M.; Montanari, J.; Commenchail, K.; Savu, D.I.; Lesueur, P.; Chevalier, F. Chondrosarcoma resistance to radiation therapy: Origins and potential therapeutic solutions. Cancers 2023, 15, 1962. [Google Scholar] [CrossRef]
- Eke, I.; Cordes, N. Radiobiology goes 3D: How ECM and cell morphology impact on cell survival after irradiation. Radiother. Oncol. 2011, 99, 271–278. [Google Scholar] [CrossRef]
- Shestakova, V.; Smirnova, A.; Yakimova, A.; Koryakin, S.; Baranovskii, D.; Saburov, V.; Yatsenko, E.; Moiseev, A.; Ivanov, S.; Smirnova, E.; et al. Biological Efficacy of Ionizing Radiation Sources on 3D Organotypic Tissue Slices Assessed by Fluorescence Microscopy. Curr. Radiopharm. 2025, 18, 64–72. [Google Scholar] [CrossRef]
- Zschenker, O.; Streichert, T.; Hehlgans, S.; Cordes, N. Genome-wide gene expression analysis in cancer cells reveals 3D growth to affect ECM and processes associated with cell adhesion but not DNA repair. PLoS ONE 2012, 7, e34279. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Sharma, D. Therapeutic response differences between 2D and 3D tumor models of magnetic hyperthermia. Nanoscale Adv. 2021, 3, 3663–3680. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Zhou, P.K. HIF-1 signaling: A key orchestrator of cancer radioresistance. Radiat. Med. Prot. 2020, 1, 7–14. [Google Scholar] [CrossRef]
- Babu, B.; Pawar, S.; Mittal, A.; Kolanthai, E.; Neal, C.J.; Coathup, M.; Seal, S. Nanotechnology enabled radioprotectants to reduce space radiation-induced reactive oxidative species. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2023, 15, e1896. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Roman, N.; Chong, M.Y.; Chahal, S.K.; Caragher, S.P.; Jackson, M.R.; Stevenson, K.H.; Dongre, S.A.; Chalmers, A.J. Radiation responses of 2D and 3D glioblastoma cells: A novel, 3D-specific radioprotective role of VEGF/Akt signaling through functional activation of NHEJ. Mol. Cancer Ther. 2020, 19, 575–589. [Google Scholar] [CrossRef]
- Kheir, E.; Stapleton, T.; Shaw, D.; Jin, Z.; Fisher, J.; Ingham, E. Development and characterization of an acellular porcine cartilage bone matrix for use in tissue engineering. J. Biomed. Mater. Res. Part A 2011, 99, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Suto, K.; Urabe, K.; Naruse, K.; Uchida, K.; Matsuura, T.; Mikuni-Takagaki, Y.; Itoman, M.; Suto, M.; Nemoto, N.; Kamiya, K.; et al. Repeated freeze–thaw cycles reduce the survival rate of osteocytes in bone-tendon constructs without affecting the mechanical properties of tendons. Cell Tissue Bank. 2012, 13, 71–80. [Google Scholar] [CrossRef]
- Roth, S.P.; Glauche, S.M.; Plenge, A.; Erbe, I.; Heller, S.; Burk, J. Automated freeze-thaw cycles for decellularization of tendon tissue-a pilot study. BMC Biotechnol. 2017, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Ninomiya, Y.; Cui, X.; Yasuda, T.; Wang, B.; Yu, D.; Sekine-Suzuki, E.; Nenoi, M. Arsenite induces premature senescence via p53/p21 pathway as a result of DNA damage in human malignant glioblastoma cells. BMB Rep. 2014, 47, 575–580. [Google Scholar] [CrossRef]
- Suckert, T.; Rassamegevanon, T.; Müller, J.; Dietrich, A.; Graja, A.; Reiche, M.; Löck, S.; Krause, M.; Beyreuther, E.; von Neubeck, C. Applying Tissue Slice Culture in Cancer Research—Insights from Preclinical Proton Radiotherapy. Cancers 2020, 12, 1589. [Google Scholar] [CrossRef]
- Drayson, O.G.G.; Melemenidis, S.; Katila, N.; Viswanathan, V.; Kramár, E.A.; Zhang, R.; Kim, R.; Ru, N.; Petit, B.; Dutt, S.; et al. A Multi-Institutional Study to Investigate the Sparing Effect after Whole Brain Electron FLASH in Mice: Reproducibility and Temporal Evolution of Functional, Electrophysiological, and Neurogenic Endpoints. Radiother. Oncol. 2024, 201, 110534. [Google Scholar] [CrossRef]
- Essers, J.; van Steeg, H.; de Wit, J.; Swagemakers, S.M.; Vermeij, M.; Hoeijmakers, J.H.; Kanaar, R. Homologous and non-homologous recombination differentially affect DNA damage repair in mice. EMBO J. 2000, 19, 1703–1710. [Google Scholar] [CrossRef]
- Maity, A.; Kao, G.D.; Muschel, R.J.; McKenna, W.G. Potential molecular targets for manipulating the radiation response. Int. J. Radiat. Oncol. Biol. Phys. 1997, 37, 639–653. [Google Scholar] [CrossRef]
- Fuks, Z.; Persauld, R.S.; Alfieri, A.; McLoughlin, M.; Ehleiter, C.; Schwartz, J.L.; Seddon, A.P.; Cordon-Cardo, C.; Haimovitz-Friedman, A. Basic fibroblast growth factor growth factor protects endothelial cells against radiation induced programmed cell death in vitro and in vivo. Cancer Res. 1994, 54, 2582–2590. [Google Scholar] [PubMed]
- Russell, J.; Wheldon, T.W.; Stanton, P.A. Radio resistant variant derived from a human neuroblastoma cell line is less prone to radiation-induced apoptosis. Cancer Res. 1995, 55, 4915–4921. [Google Scholar]
- Shrivastava, V.; Mishra, A.K.; Dwarakanath, B.S.; Ravindranath, T. Enhancement of radionuclide induced cytotoxicity by 2-deoxy-D-glucose in human tumor cell lines. J. Cancer Res. Ther. 2006, 2, 57–64. [Google Scholar]
- Barbero, A.; Grogan, S.; Schäfer, D.; Heberer, M.; Mainil-Varlet, P.; Martin, I. Age related changes in human articular chondrocyte yield, proliferation and post-expansion chondrogenic capacity. Osteoarthr. Cartil. 2004, 12, 476–484. [Google Scholar] [CrossRef]
- Babel, L.; Grunewald, M.; Lehn, R.; Langhans, M.; Meckel, T. Direct evidence for cell adhesion-mediated radioresistance (CAM-RR) on the level of individual integrin β1 clusters. Sci. Rep. 2017, 7, 3393. [Google Scholar] [CrossRef]
- Swamy, C.S.U.S.; Boothby, T.C. Surviving extreme radiation. eLife 2024, 13, e100219. [Google Scholar] [CrossRef] [PubMed]
- Clark-Hachtel, C.M.; Hibshman, J.D.; De Buysscher, T.; Stair, E.R.; Hicks, L.M.; Goldstein, B. The tardigrade Hypsibius exemplaris dramatically upregulates DNA repair pathway genes in response to ionizing radiation. Curr. Biol. 2024, 34, 1819–1830. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Liang, S.; Gao, J.; Wang, Z.; Li, C.; Wang, R.; Yu, W. Extracellular matrix stiffness mediates radiosensitivity in a 3D nasopharyngeal carcinoma model. Cancer Cell Int. 2022, 22, 364. [Google Scholar] [CrossRef]
- La Verde, G.; Artiola, V.; Panzetta, V.; Pugliese, M.; Netti, P.A.; Fusco, S. Cytoskeleton response to ionizing radiation: A brief review on adhesion and migration effects. Biomedicines 2021, 9, 1102. [Google Scholar] [CrossRef]
- Hehlgans, S.; Haase, M.; Cordes, N. Signalling via integrins: Implications for cell survival and anticancer strategies. Biochim. Biophys. Acta Rev. Cancer 2007, 1775, 163–180. [Google Scholar] [CrossRef]
- Mao, X.W.; Mekonnen, T.; Kennedy, A.R.; Gridley, D.S. Differential expression of oxidative stress and extracellular matrix remodeling genes in low- or high-dose-rate photon-irradiated skin. Radiat. Res. 2011, 176, 187–197. [Google Scholar] [CrossRef]
- Shestakova, V.A.; Smirnova, E.I.; Rao, L.; Kolobaev, I.V.; Atiakshin, D.A.; Ignatyuk, M.A.; Krasheninnikov, M.E.; Ahmedov, B.G.; Ivanov, S.A.; Baranovskii, D.S.; et al. Nasal Chondrocytes Intensively Invade and Repair Pathologically Altered Cartilage Through Intrinsic Genomic Mechanisms: A Narrative Review. Curr. Rheumatol. Rev. 2025. [Google Scholar] [CrossRef] [PubMed]
- Kabakov, A.E.; Yakimova, A.O. Hypoxia-induced cancer cell responses driving radioresistance of hypoxic tumors: Approaches to targeting and radiosensitizing. Cancers 2021, 13, 1102. [Google Scholar] [CrossRef] [PubMed]
- Prise, K.M.; Schettino, G.; Folkard, M.; Held, K.D. New insights on cell death from radiation exposure. Lancet Oncol. 2005, 6, 520–528. [Google Scholar] [CrossRef]
- International Atomic Energy Agency. Instructive Surfaces and Scaffolds for Tissue Engineering Using Radiation Technology; IAEA CRP F23030-E31007; International Atomic Energy Agency: Vienna, Austria, 2014; Available online: https://www.iaea.org/projects/crp/f23030 (accessed on 20 February 2025).
- Bustamante, P.; Anessi, C.; Santoro, N.; Ciavaro, N.; Horak, C. Synthesis and characterization of hydrogels cross-linked with gamma radiation for use as wound dressings. In VIII Latin American Conference on Biomedical Engineering and XLII National Conference on Biomedical Engineering, Proceedings of the CLAIB-CNIB 2019, Cancún, México, 2–5 October 2019; Springer International Publishing: Cham, Switzerland, 2020; pp. 643–651. [Google Scholar] [CrossRef]
- Yan, G.E.; Elbadawi, M.; Efferth, T. Multiple cell death modalities and their key features. World Acad. Sci. J. 2020, 2, 39–48. [Google Scholar] [CrossRef]
- Kudryavtsev, V.A.; Khokhlova, A.V.; Mosina, V.A.; Selivanova, E.I.; Kabakov, A.E. Induction of Hsp70 in tumor cells treated with inhibitors of the Hsp90 activity: A predictive marker and promising target for radiosensitization. PLoS ONE 2017, 12, e0173640. [Google Scholar] [CrossRef]
- Cortese, F.; Klokov, D.; Osipov, A.; Stefaniak, J.; Moskalev, A.; Schastnaya, J.; Cantor, C.; Aliper, A.; Mamoshina, P.; Ushakov, I.; et al. Vive la radiorésistance!: Converging research in radiobiology and biogerontology to enhance human radioresistance for deep space exploration and colonization. Oncotarget 2018, 9, 14692–14722. [Google Scholar] [CrossRef]
- Klabukov, I.; Smirnova, A.; Yakimova, A.; Kabakov, A.E.; Atiakshin, D.; Petrenko, D.; Shestakova, V.A.; Sulina, Y.; Yatsenko, E.; Stepanenko, V.N.; et al. Oncomatrix: Molecular Composition and Biomechanical Properties of the Extracellular Matrix in Human Tumors. J. Mol. Pathol. 2024, 5, 437–453. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baranovskii, D.; Smirnova, A.; Yakimova, A.; Kisel, A.; Koryakin, S.; Atiakshin, D.; Ignatyuk, M.; Potievskiy, M.; Saburov, V.; Budnik, S.; et al. Tissue-Cultured Chondrocytes Survive After Irradiation in 1300 Gy Dose. Biomedicines 2025, 13, 2153. https://doi.org/10.3390/biomedicines13092153
Baranovskii D, Smirnova A, Yakimova A, Kisel A, Koryakin S, Atiakshin D, Ignatyuk M, Potievskiy M, Saburov V, Budnik S, et al. Tissue-Cultured Chondrocytes Survive After Irradiation in 1300 Gy Dose. Biomedicines. 2025; 13(9):2153. https://doi.org/10.3390/biomedicines13092153
Chicago/Turabian StyleBaranovskii, Denis, Anna Smirnova, Anna Yakimova, Anastas Kisel, Sergey Koryakin, Dmitrii Atiakshin, Michael Ignatyuk, Mikhail Potievskiy, Vyacheslav Saburov, Sergey Budnik, and et al. 2025. "Tissue-Cultured Chondrocytes Survive After Irradiation in 1300 Gy Dose" Biomedicines 13, no. 9: 2153. https://doi.org/10.3390/biomedicines13092153
APA StyleBaranovskii, D., Smirnova, A., Yakimova, A., Kisel, A., Koryakin, S., Atiakshin, D., Ignatyuk, M., Potievskiy, M., Saburov, V., Budnik, S., Sulina, Y., Stepanenko, V. N., Churyukin, R., Akhmedov, B., Shegay, P., Kaprin, A. D., & Klabukov, I. (2025). Tissue-Cultured Chondrocytes Survive After Irradiation in 1300 Gy Dose. Biomedicines, 13(9), 2153. https://doi.org/10.3390/biomedicines13092153







