Effects of Statins on All-Cause Mortality in Patients with Breast Cancer: A Population-Based Study
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Data Analysis
2.3. Statistical Analysis
3. Results
3.1. Clinical Characteristics of Patients Stratified by Statin Use
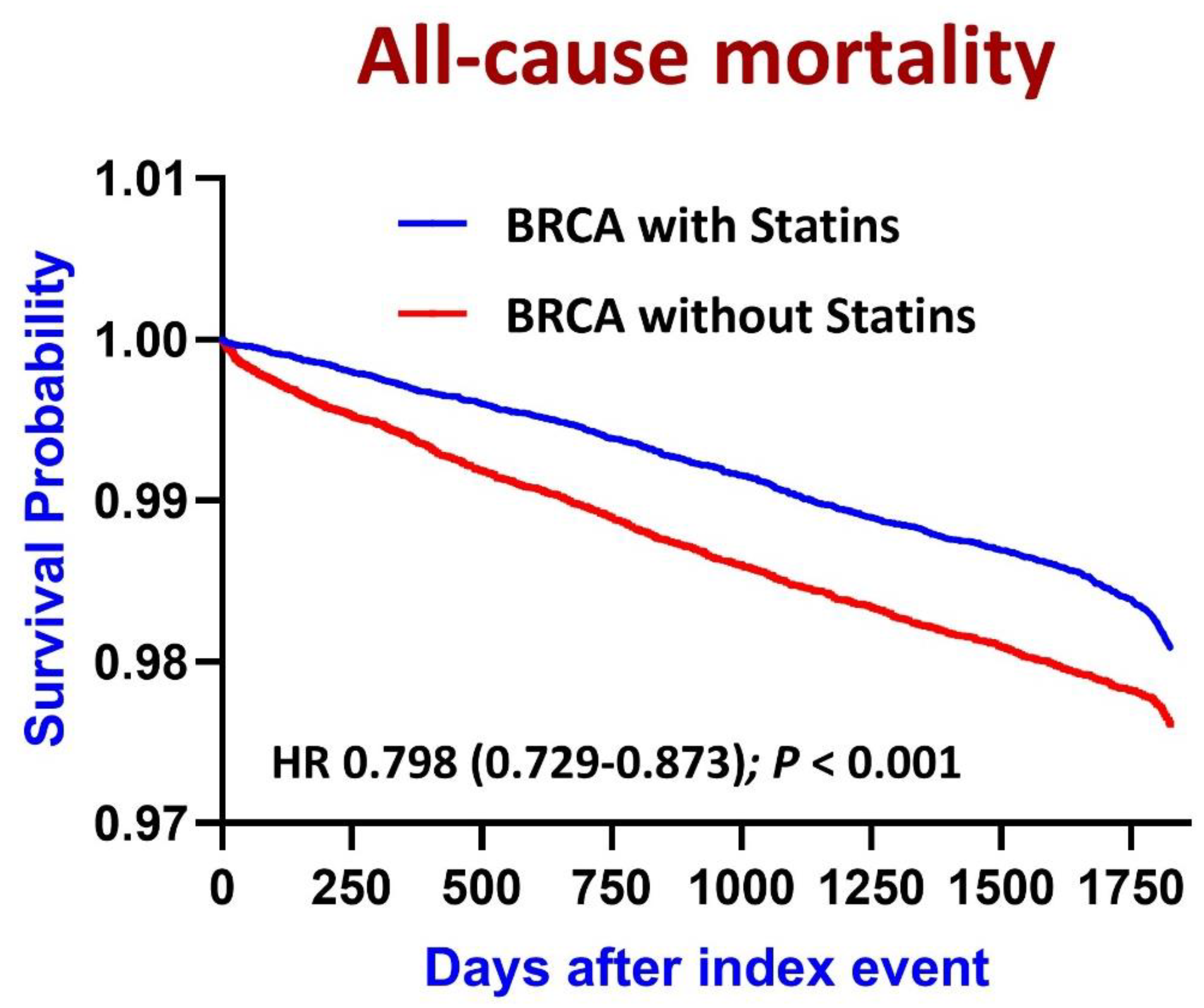
3.2. Effects of Statin Use on Survival
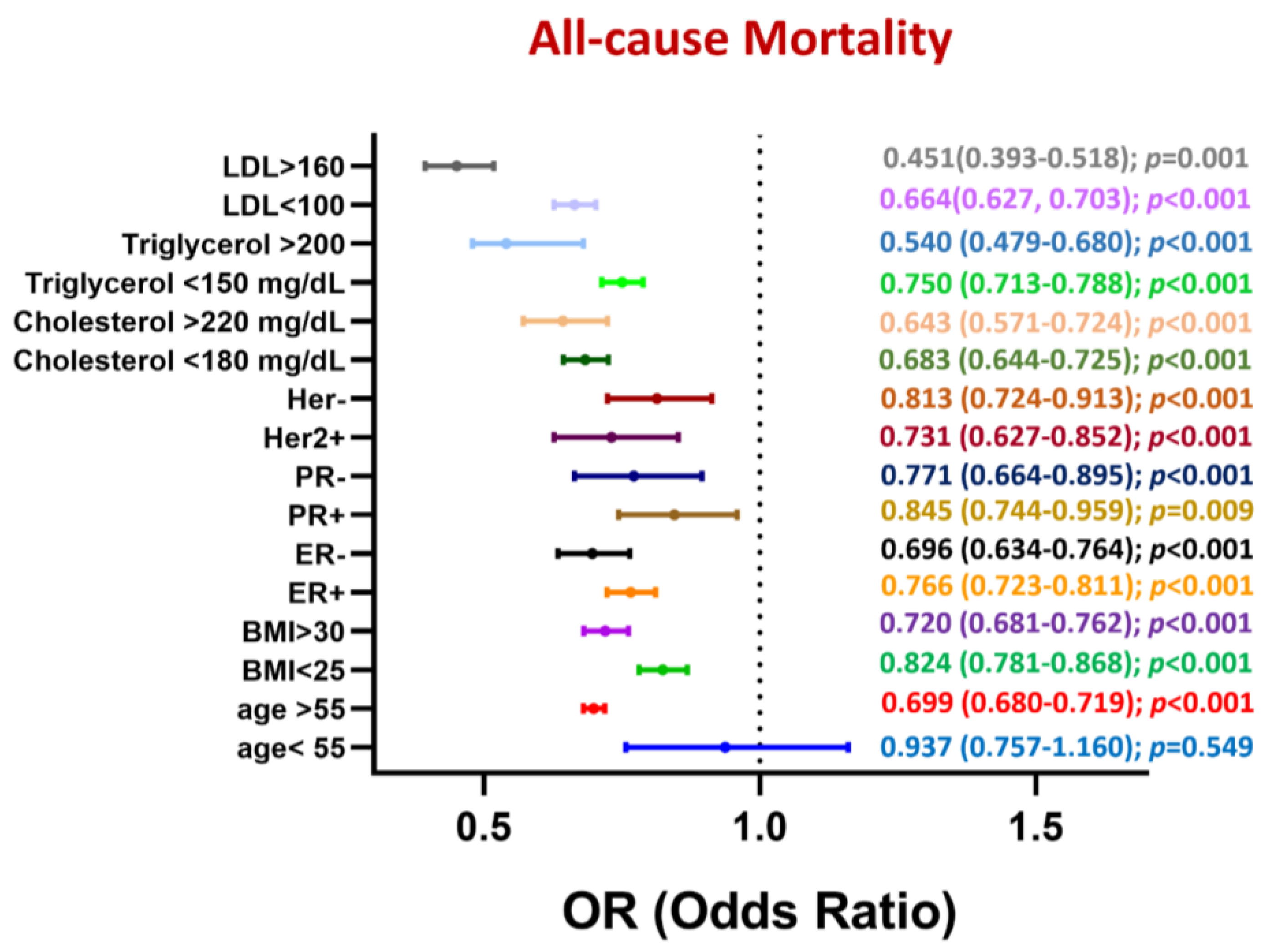
3.3. Subgroup Analysis of All-Cause Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karthikayan, A.; Sureshkumar, S.; Kadambari, D.; Vijayakumar, C. Low serum 25-hydroxy vitamin D levels are associated with aggressive breast cancer variants and poor prognostic factors in patients with breast carcinoma. Arch. Endocrinol. Metab. 2018, 62, 452–459. [Google Scholar] [CrossRef] [PubMed]
- Sotiriou, C.; Pusztai, L. Gene-expression signatures in breast cancer. N. Engl. J. Med. 2009, 360, 790–800. [Google Scholar] [CrossRef]
- Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature 2012, 490, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Perou, C.M.; Sorlie, T.; Eisen, M.B.; van de Rijn, M.; Jeffrey, S.S.; Rees, C.A.; Pollack, J.R.; Ross, D.T.; Johnsen, H.; Akslen, L.A.; et al. Molecular portraits of human breast tumours. Nature 2000, 406, 747–752. [Google Scholar] [CrossRef]
- Sorlie, T.; Perou, C.M.; Tibshirani, R.; Aas, T.; Geisler, S.; Johnsen, H.; Hastie, T.; Eisen, M.B.; van de Rijn, M.; Jeffrey, S.S.; et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc. Natl. Acad. Sci. USA 2001, 98, 10869–10874. [Google Scholar] [CrossRef]
- Foulkes, W.D.; Smith, I.E.; Reis-Filho, J.S. Triple-negative breast cancer. N. Engl. J. Med. 2010, 363, 1938–1948. [Google Scholar] [CrossRef]
- Murtola, T.J.; Visvanathan, K.; Artama, M.; Vainio, H.; Pukkala, E. Statin use and breast cancer survival: A nationwide cohort study from Finland. PLoS ONE 2014, 9, e110231. [Google Scholar] [CrossRef] [PubMed]
- Beckwitt, C.H.; Clark, A.M.; Ma, B.; Whaley, D.; Oltvai, Z.N.; Wells, A. Statins attenuate outgrowth of breast cancer metastases. Br. J. Cancer 2018, 119, 1094–1105. [Google Scholar] [CrossRef]
- Bjarnadottir, O.; Romero, Q.; Bendahl, P.O.; Jirstrom, K.; Ryden, L.; Loman, N.; Uhlen, M.; Johannesson, H.; Rose, C.; Grabau, D.; et al. Targeting HMG-CoA reductase with statins in a window-of-opportunity breast cancer trial. Breast Cancer Res. Treat. 2013, 138, 499–508. [Google Scholar] [CrossRef]
- Hosseini, F.S.; Ahmadi, A.; Kesharwani, P.; Hosseini, H.; Sahebkar, A. Regulatory effects of statins on Akt signaling for prevention of cancers. Cell Signal 2024, 120, 111213. [Google Scholar] [CrossRef]
- Campbell, M.J.; Esserman, L.J.; Zhou, Y.; Shoemaker, M.; Lobo, M.; Borman, E.; Baehner, F.; Kumar, A.S.; Adduci, K.; Marx, C.; et al. Breast cancer growth prevention by statins. Cancer Res. 2006, 66, 8707–8714. [Google Scholar] [CrossRef] [PubMed]
- Ghosh-Choudhury, N.; Mandal, C.C.; Ghosh-Choudhury, N.; Ghosh Choudhury, G. Simvastatin induces derepression of PTEN expression via NFkappaB to inhibit breast cancer cell growth. Cell Signal 2010, 22, 749–758. [Google Scholar] [CrossRef]
- Gopalan, A.; Yu, W.; Sanders, B.G.; Kline, K. Simvastatin inhibition of mevalonate pathway induces apoptosis in human breast cancer cells via activation of JNK/CHOP/DR5 signaling pathway. Cancer Lett. 2013, 329, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Denoyelle, C.; Vasse, M.; Korner, M.; Mishal, Z.; Ganne, F.; Vannier, J.P.; Soria, J.; Soria, C. Cerivastatin, an inhibitor of HMG-CoA reductase, inhibits the signaling pathways involved in the invasiveness and metastatic properties of highly invasive breast cancer cell lines: An in vitro study. Carcinogenesis 2001, 22, 1139–1148. [Google Scholar] [CrossRef]
- Schointuch, M.N.; Gilliam, T.P.; Stine, J.E.; Han, X.; Zhou, C.; Gehrig, P.A.; Kim, K.; Bae-Jump, V.L. Simvastatin, an HMG-CoA reductase inhibitor, exhibits anti-metastatic and anti-tumorigenic effects in endometrial cancer. Gynecol. Oncol. 2014, 134, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Hillis, A.L.; Martin, T.D.; Manchester, H.E.; Hogstrom, J.; Zhang, N.; Lecky, E.; Kozlova, N.; Lee, J.; Persky, N.S.; Root, D.E.; et al. Targeting Cholesterol Biosynthesis with Statins Synergizes with AKT Inhibitors in Triple-Negative Breast Cancer. Cancer Res. 2024, 84, 3250–3266. [Google Scholar] [CrossRef]
- El-Shafei, N.H.; Zaafan, M.A.; Kandil, E.A.; Sayed, R.H. Simvastatin ameliorates testosterone-induced prostatic hyperplasia in rats via modulating IGF-1/PI3K/AKT/FOXO signaling. Eur. J. Pharmacol. 2023, 950, 175762. [Google Scholar] [CrossRef]
- Hu, T.; Shen, H.; Huang, H.; Yang, Z.; Zhou, Y.; Zhao, G. Cholesterol-lowering drug pitavastatin targets lung cancer and angiogenesis via suppressing prenylation-dependent Ras/Raf/MEK and PI3K/Akt/mTOR signaling. Anti-Cancer Drugs 2020, 31, 377–384. [Google Scholar] [CrossRef]
- Afshordel, S.; Kern, B.; Clasohm, J.; Konig, H.; Priester, M.; Weissenberger, J.; Kogel, D.; Eckert, G.P. Lovastatin and perillyl alcohol inhibit glioma cell invasion, migration, and proliferation--impact of Ras-/Rho-prenylation. Pharmacol. Res. 2015, 91, 69–77. [Google Scholar] [CrossRef]
- Mao, W.; Cai, Y.; Chen, D.; Jiang, G.; Xu, Y.; Chen, R.; Wang, F.; Wang, X.; Zheng, M.; Zhao, X.; et al. Statin shapes inflamed tumor microenvironment and enhances immune checkpoint blockade in non-small cell lung cancer. JCI Insight 2022, 7, e161940. [Google Scholar] [CrossRef]
- Jiang, W.; Hu, J.W.; He, X.R.; Jin, W.L.; He, X.Y. Statins: A repurposed drug to fight cancer. J. Exp. Clin. Cancer Res. 2021, 40, 241. [Google Scholar] [CrossRef]
- Hyder, T.; Marti, J.L.G.; Nasrazadani, A.; Brufsky, A.M. Statins and endocrine resistance in breast cancer. Cancer Drug Resist. 2021, 4, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Centonze, G.; Natalini, D.; Piccolantonio, A.; Salemme, V.; Morellato, A.; Arina, P.; Riganti, C.; Defilippi, P. Cholesterol and Its Derivatives: Multifaceted Players in Breast Cancer Progression. Front. Oncol. 2022, 12, 906670. [Google Scholar] [CrossRef]
- Centonze, G.; Natalini, D.; Grasso, S.; Morellato, A.; Salemme, V.; Piccolantonio, A.; D’Attanasio, G.; Savino, A.; Bianciotto, O.T.; Fragomeni, M.; et al. p140Cap modulates the mevalonate pathway decreasing cell migration and enhancing drug sensitivity in breast cancer cells. Cell Death Dis. 2023, 14, 849. [Google Scholar] [CrossRef]
- Beckwitt, C.H.; Shiraha, K.; Wells, A. Lipophilic statins limit cancer cell growth and survival, via involvement of Akt signaling. PLoS ONE 2018, 13, e0197422. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Jung, H.H.; Ahn, J.S.; Im, Y.H. Statin induces inhibition of triple negative breast cancer (TNBC) cells via PI3K pathway. Biochem. Biophys. Res. Commun. 2013, 439, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Malone, K.E.; Heckbert, S.R.; Li, C.I. Statin use and risks of breast cancer recurrence and mortality. Cancer 2024, 130, 3106–3114. [Google Scholar] [CrossRef]
- Benjamin, D.J.; Haslam, A.; Prasad, V. Cardiovascular/anti-inflammatory drugs repurposed for treating or preventing cancer: A systematic review and meta-analysis of randomized trials. Cancer Med. 2024, 13, e7049. [Google Scholar] [CrossRef]
- Giorello, M.B.; Marks, M.P.; Osinalde, T.M.; Padin, M.D.R.; Wernicke, A.; Calvo, J.C.; Chasseing, N.A.; Vellon, L. Post-surgery statin use contributes to favorable outcomes in patients with early breast cancer. Cancer Epidemiol. 2024, 90, 102573. [Google Scholar] [CrossRef]
- McKechnie, T.; Brown, Z.; Lovrics, O.; Yang, S.; Kazi, T.; Eskicioglu, C.; Parvez, E. Concurrent Use of Statins in Patients Undergoing Curative Intent Treatment for Triple Negative Breast Cancer: A Systematic Review and Meta-Analysis. Clin. Breast Cancer 2024, 24, e103–e115. [Google Scholar] [CrossRef]
- Jia, X.; Lu, Y.; Xu, Z.; Mu, Q. Impact of statin use on breast cancer recurrence and mortality before and after diagnosis: A systematic review and meta-analysis. Front. Oncol. 2023, 13, 1256747. [Google Scholar] [CrossRef] [PubMed]
- Kamal, A.; Boerner, J.; Assad, H.; Chen, W.; Simon, M.S. The Effect of Statins on Markers of Breast Cancer Proliferation and Apoptosis in Women with In Situ or Early-Stage Invasive Breast Cancer. Int. J. Mol. Sci. 2024, 25, 9587. [Google Scholar] [CrossRef]
- Li, L.; Wang, H.; Zhang, S.; Gao, S.; Lu, X.; Pan, Y.; Tang, W.; Huang, R.; Qiao, K.; Ning, S. Statins inhibit paclitaxel-induced PD-L1 expression and increase CD8+ T cytotoxicity for better prognosis in breast cancer. Int. J. Surg. 2024, 110, 4716–4726. [Google Scholar] [CrossRef]
- Van Wyhe, R.D.; Rahal, O.M.; Woodward, W.A. Effect of statins on breast cancer recurrence and mortality: A review. Breast Cancer 2017, 9, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Atale, N.; Wells, A. Statins as Secondary Preventive Agent to Limit Breast Cancer Metastatic Outgrowth. Int. J. Mol. Sci. 2025, 26, 1300. [Google Scholar] [CrossRef]
- Marti, J.L.G.; Wells, J.Z.; Wells, A. Statins as a Secondary Preventive Agent for Metastatic Cancer. J. Thorac. Oncol. 2023, 18, e125–e126. [Google Scholar] [CrossRef]
- Murto, M.O.; Simolin, N.; Arponen, O.; Siltari, A.; Artama, M.; Visvanathan, K.; Jukkola, A.; Murtola, T.J. Statin Use, Cholesterol Level, and Mortality Among Females With Breast Cancer. JAMA Netw. Open 2023, 6, e2343861. [Google Scholar] [CrossRef] [PubMed]
- Scott, O.W.; TinTin, S.; Harborg, S.; Kuper-Hommel, M.J.J.; Lawrenson, R.; Elwood, J.M. Post-diagnostic statin use and breast cancer-specific mortality: A population-based cohort study. Breast Cancer Res. Treat. 2023, 199, 195–206. [Google Scholar] [CrossRef]
- Lee, K.; Noh, E.; Moon, S.J.; Joo, Y.Y.; Kang, E.J.; Seo, J.H.; Park, I.H. Statin use in patients with hormone receptor-positive metastatic breast cancer treated with everolimus and exemestane. Cancer Med. 2023, 12, 5461–5470. [Google Scholar] [CrossRef]
- Kato, C.; Iizuka-Ohashi, M.; Honda, M.; Konishi, E.; Yokota, I.; Boku, S.; Mizuta, N.; Morita, M.; Sakaguchi, K.; Taguchi, T.; et al. Additional statin treatment enhances the efficacy of HER2 blockade and improves prognosis in Rac1-high/HER2-positive breast cancer. Biochim. Biophys. Acta Mol. Basis Dis. 2024, 1870, 167458. [Google Scholar] [CrossRef]
- Jiralerspong, S.; Goodwin, P.J. Obesity and Breast Cancer Prognosis: Evidence, Challenges, and Opportunities. J. Clin. Oncol. 2016, 34, 4203–4216. [Google Scholar] [CrossRef] [PubMed]
- Manthravadi, S.; Shrestha, A.; Madhusudhana, S. Impact of statin use on cancer recurrence and mortality in breast cancer: A systematic review and meta-analysis. Int. J. Cancer 2016, 139, 1281–1288. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Yi, Z.; Guan, X.; Zeng, Y.X.; Ma, F. The relationship between statins and breast cancer prognosis varies by statin type and exposure time: A meta-analysis. Breast Cancer Res. Treat. 2017, 164, 1–11. [Google Scholar] [CrossRef]
- Koohestanimobarhan, S.; Salami, S.; Imeni, V.; Mohammadi, Z.; Bayat, O. Lipophilic statins antagonistically alter the major epithelial-to-mesenchymal transition signaling pathways in breast cancer stem-like cells via inhibition of the mevalonate pathway. J. Cell Biochem. 2019, 120, 2515–2531. [Google Scholar] [CrossRef] [PubMed]


| Characteristic Name | Before Propensity Score Matching | After Propensity Score Matching | ||||||
|---|---|---|---|---|---|---|---|---|
| Patients with Statins (n = 104,754) | Patients without Statins (n = 692,146) | p Value | Std diff | Patients with Statins (n = 93,435) | Patients without Statins (n = 93,435) | p Value | Std diff | |
| Basic demographics (%) | ||||||||
| Age at Index, mean (mean+/−SD) | 67.8 +/− 10.6 | 58.6 +/− 14.1 | <0.001 | 0.74 | 67.6 +/− 10.7 | 68.0 +/− 10.9 | <0.001 | 0.038 |
| White (%) | 70.80% | 53.60% | <0.001 | 0.36 | 71.20% | 71.60% | 0.045 | 0.009 |
| Black or African American (%) | 14.80% | 7.00% | <0.001 | 0.25 | 13.70% | 13.10% | <0.001 | 0.019 |
| Asian (%) | 3.90% | 5.00% | <0.001 | 0.05 | 3.90% | 3.90% | 0.559 | 0.003 |
| Laboratory, Mean ± SD | ||||||||
| Glucose [Mass/volume] in Serum, Plasma, or Blood | 118.1 +/− 47.1 | 105.4 +/− 34.3 | <0.001 | 0.31 | 116.0 +/− 45.3 | 113.3 +/− 43.4 | <0.001 | 0.06 |
| Alanine aminotransferase [Enzymatic activity/volume] in Serum, Plasma, or Blood | 23.8 +/− 27.2 | 26.8 +/− 57.4 | <0.001 | 0.07 | 23.9 +/− 26.7 | 27.3 +/− 63.1 | <0.001 | 0.071 |
| Aspartate aminotransferase [Enzymatic activity/volume] in Serum or Plasma | 25.3 +/− 32.3 | 31.6 +/− 94.5 | <0.001 | 0.09 | 25.3 +/− 30.8 | 33.3 +/− 95.8 | <0.001 | 0.112 |
| Alkaline phosphatase [Enzymatic activity/volume] in Serum, Plasma, or Blood | 84.3 +/− 47.7 | 94.2 +/− 97.8 | <0.001 | 0.13 | 84.1 +/− 48.1 | 97.5 +/− 92.6 | <0.001 | 0.182 |
| Lactate dehydrogenase [Enzymatic activity/volume] in Serum or Plasma | 248.1 +/− 243.6 | 270.7 +/− 360.5 | <0.001 | 0.074 | 247.6 +/− 247.8 | 292.2 +/− 380.9 | <0.001 | 0.139 |
| Bilirubin.Total [Mass/volume] in Serum, Plasma, or Blood | 0.5 +/− 0.7 | 0.6 +/− 1.1 | <0.001 | 0.084 | 0.5 +/− 0.6 | 0.6 +/− 1.2 | <0.001 | 0.096 |
| Albumin [Mass/volume] in Serum, Plasma, or Blood | 4.0 +/− 0.5 | 4.0 +/− 0.6 | <0.001 | 0.025 | 4.0 +/− 0.5 | 3.9 +/− 0.6 | <0.001 | 0.278 |
| Cholesterol [Mass/volume] in Serum or Plasma | 183.5 +/− 47.2 | 196.3 +/− 41.3 | <0.001 | 0.287 | 185.1 +/− 47.0 | 192.6 +/− 43.7 | <0.001 | 0.166 |
| Cholesterol in LDL [Mass/volume] in Serum or Plasma | 101.3 +/− 39.3 | 111.7 +/− 33.3 | <0.001 | 0.287 | 102.5 +/− 39.3 | 109.6 +/− 34.7 | <0.001 | 0.192 |
| Cholesterol in HDL [Mass/volume] in Serum or Plasma | 54.1 +/− 18.7 | 60.0 +/− 21.1 | <0.001 | 0.296 | 54.6 +/− 18.8 | 57.6 +/− 21.7 | <0.001 | 0.15 |
| Triglyceride [Mass/volume] in Serum, Plasma, or Blood | 138.4 +/− 83.0 | 114.6 +/− 70.5 | <0.001 | 0.308 | 137.8 +/− 83.1 | 122.9 +/− 74.3 | <0.001 | 0.189 |
| Hemoglobin A1c/Hemoglobin.total in Blood | 6.8 +/− 1.5 | 6.1 +/− 1.3 | <0.001 | 0.494 | 6.7 +/− 1.5 | 6.4 +/− 1.5 | <0.001 | 0.194 |
| BMI | 30.3 +/− 7.2 | 27.7 +/− 6.8 | <0.001 | 0.364 | 30.1 +/− 7.1 | 28.8 +/− 7.2 | <0.001 | 0.175 |
| Diagnosis (%) | ||||||||
| Diabetes Mellitus | 22.30% | 3.10% | <0.001 | 0.602 | 17.60% | 16.60% | <0.001 | 0.027 |
| Acute Kidney Failure and Chronic Kidney Disease | 7.30% | 1.50% | <0.001 | 0.288 | 6.40% | 6.30% | 0.276 | 0.005 |
| Hypertensive Diseases | 46.60% | 10.50% | <0.001 | 0.871 | 43.40% | 43.60% | 0.253 | 0.005 |
| Outcomes | Groups | Cases Followed | Incident Cases | Risk (%) | Risk Ratio | Odds Ratio | Risk Difference (p Value) |
|---|---|---|---|---|---|---|---|
| All-cause Mortality | with statins | 93,236 | 10,412 | 11.2 | 0.721 (0.705, 0.739) | 0.686 (0.668, 0.705) | <0.001 |
| without statins | 92,578 | 14,332 | 15.5 | ||||
| Myocardial Infarction | with statins | 90,661 | 4454 | 4.9 | 4.390 (4.105, 4.694) | 4.565 (4.264, 4.887) | <0.001 |
| without statins | 92,569 | 1036 | 1.1 | ||||
| Ischemic Stroke | with statins | 89,437 | 5653 | 6.3 | 4.250 (4.009, 4.505) | 4.469 (4.210, 4.744) | <0.001 |
| without statins | 92,048 | 1369 | 1.5 | ||||
| Atrial Fibrillation | with statins | 86,617 | 8473 | 9.8 | 2.272 (2.190, 2.358) | 2.410 (2.317, 2.507) | <0.001 |
| without statins | 88,226 | 3798 | 4.3 | ||||
| Ventricular Arrhythmias | with statins | 85,840 | 11,919 | 13.9 | 2.644 (2.560, 2.731) | 2.909 (2.808, 3.013) | <0.001 |
| without statins | 89,702 | 4711 | 5.3 | ||||
| Acute Heart Failure | with statins | 91,903 | 4999 | 5.4 | 3.502 (3.305, 3.711) | 3.646 (3.436, 3.869) | <0.001 |
| without statins | 92,775 | 1441 | 1.6 | ||||
| Pulmonary Embolism | with statins | 92,007 | 3043 | 3.3 | 1.864 (1.757, 1.978) | 1.894 (1.782, 2.013) | <0.001 |
| without statins | 92,281 | 1637 | 1.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, C.-F.; Li, C.-H.; Wang, J.; Lu, K.-C.; Tsai, K.-W. Effects of Statins on All-Cause Mortality in Patients with Breast Cancer: A Population-Based Study. Biomedicines 2025, 13, 1556. https://doi.org/10.3390/biomedicines13071556
Cheng C-F, Li C-H, Wang J, Lu K-C, Tsai K-W. Effects of Statins on All-Cause Mortality in Patients with Breast Cancer: A Population-Based Study. Biomedicines. 2025; 13(7):1556. https://doi.org/10.3390/biomedicines13071556
Chicago/Turabian StyleCheng, Ching-Feng, Chao-Hsu Li, Joshua Wang, Kuo-Cheng Lu, and Kuo-Wang Tsai. 2025. "Effects of Statins on All-Cause Mortality in Patients with Breast Cancer: A Population-Based Study" Biomedicines 13, no. 7: 1556. https://doi.org/10.3390/biomedicines13071556
APA StyleCheng, C.-F., Li, C.-H., Wang, J., Lu, K.-C., & Tsai, K.-W. (2025). Effects of Statins on All-Cause Mortality in Patients with Breast Cancer: A Population-Based Study. Biomedicines, 13(7), 1556. https://doi.org/10.3390/biomedicines13071556






