Genetic Animal Models of Cardiovascular Pathologies
Abstract
1. Introduction
2. Genetic Strains Selected to Maintain Phenotypic Characteristics Resulting from Spontaneous Genetic Mutations and Naturally Occurring Pathology
3. Transgenic and Knockout Animal Models
4. Genetically Encoded Tools in Cardiovascular Disease Modeling
5. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CVDs | Cardiovascular diseases |
| AAV | Adeno-associated virus |
| CRISPR-Cas9 | Cas9, CRISPR-associated protein 9 |
| CAD | Coronary artery disease |
| SD | Sprague Dawley |
| SHR | Spontaneously hypertensive rat |
| DSS | Dahl salt-sensitive |
| FHH | Fawn-hooded hypertensive |
| BUF | Buffalo |
| GK | Goto-Kakizaki |
| MWF | Munich Wistar Frömter |
| NZGH | New Zealand genetically hypertensive |
| BP | Blood pressure |
| AH | Arterial hypertension |
| SBP | Systolic blood pressure |
| DBP | Diastolic blood pressure |
| SHR-SP | Spontaneously hypertensive stroke-prone rats |
| MNS | Milan normotensive strain |
| MHS | Milan hypertensive strain |
| QTL | Quantitative trait locus |
| SHP | Sabra hypertensive-prone |
| DCMP | Dilated cardiomyopathy |
| HCMP | Hypertrophic cardiomyopathy |
| RCMP | Restrictive cardiomyopathy |
| cTnT | Low-molecular cardiac troponin T |
| ACTC | Cardiac actin |
| TPM1 | α-tropomyosin |
| MYBPC | Myosin-binding protein |
| ARVC | Arrhythmogenic right ventricular dysplasia/cardiomyopathy |
| WHHL | Watanabe heritable hyperlipidaemic |
| LDL | Low-density lipoprotein |
| CETP | Cholesterol ester transporter protein |
| PDGFs | Platelet-derived growth factors |
| ESC | Embryonic stem cell |
| APD | Automated peritoneal dialysis |
| SR | Sarcoplasmic reticulum |
| CPVT | Catecholaminergic polymorphic ventricular tachycardia |
| AF | Atrial fibrillation |
| LQTS | Long QT syndrome |
| MyBP-C | Myosin-binding protein-C |
| CETP | Cholesteryl ester transfer protein |
| NFAT | Nuclear factor of activated T-cells |
| Akt (PKB) | Protein kinase B |
| MAPK | Mitogen-activated protein kinases |
| MYH7 | β-myosin heavy chain |
| MYBPC3 | Myosin-binding protein C3 |
| ELC | Essential light chain |
| PI3K | Phosphoinositide-3-kinase |
| PKM1 | Muscle isoenzyme pyruvate kinase 1 |
| AAVR | Adeno-associated virus receptor |
| VEGF | Vascular endothelial growth factor |
| HRC | Calcium-binding protein |
| HRC-KD | Calcium-binding protein gene knockdown |
| DAAO | D-amino acid oxidase |
| BNP | Brain natriuretic peptide |
| ANP | Atrial natriuretic peptide |
| Nrf2 | Nuclear factor |
| GSH | Reduced glutathione |
References
- Blackwell, D.J.; Schmeckpeper, J.; Knollmann, B.C. Animal models to study cardiac arrhythmias. Circ. Res. 2022, 130, 1926–1964. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.-P.; Liu, Y.; Fan, Y.-J.; Zhao, Y.-Y.; Feng, J.-Q.; Liu, Y. To develop a novel animal model of myocardial infarction: A research imperative. Anim. Models. Exp. Med. 2018, 1, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Li, Y.; Chan, T.K.; Zhao, H.; Xiang, Y.; Chang, X.; Zhou, H.; Xu, D.; Ong, S.B. Large animal models of cardiac ischemia-reperfusion injury: Where are we now? Zool. Res. 2023, 44, 591–603. [Google Scholar] [CrossRef]
- Getz, G.S.; Reardon, C.A. Animal models of atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 1104–1115. [Google Scholar] [CrossRef]
- Emini Veseli, B.; Perrotta, P.; De Meyer, G.R.A.; Roth, L.; Van der Donckt, C.; Martinet, W.; De Meyer, G.R.Y. Animal models of atherosclerosis. Eur. J. Pharmacol. 2017, 816, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Milani-Nejad, N.; Janssen, P.M.L. Small and large animal models in cardiac contraction research: Advantages and disadvantages. Pharmacol. Ther. 2014, 141, 235–249. [Google Scholar] [CrossRef]
- Saljic, A.; Jespersen, T.; Buhl, R. Anti-arrhythmic investigations in large animal models of atrial fibrillation. Br. J. Pharmacol. 2022, 179, 838–858. [Google Scholar] [CrossRef]
- Garcia-Gonzalez, I.; Mühleder, S.; Fernández-Chacón, M.; Benedito, R. Genetic tools to study cardiovascular biology. Front. Physiol. 2020, 11, 1084. [Google Scholar] [CrossRef]
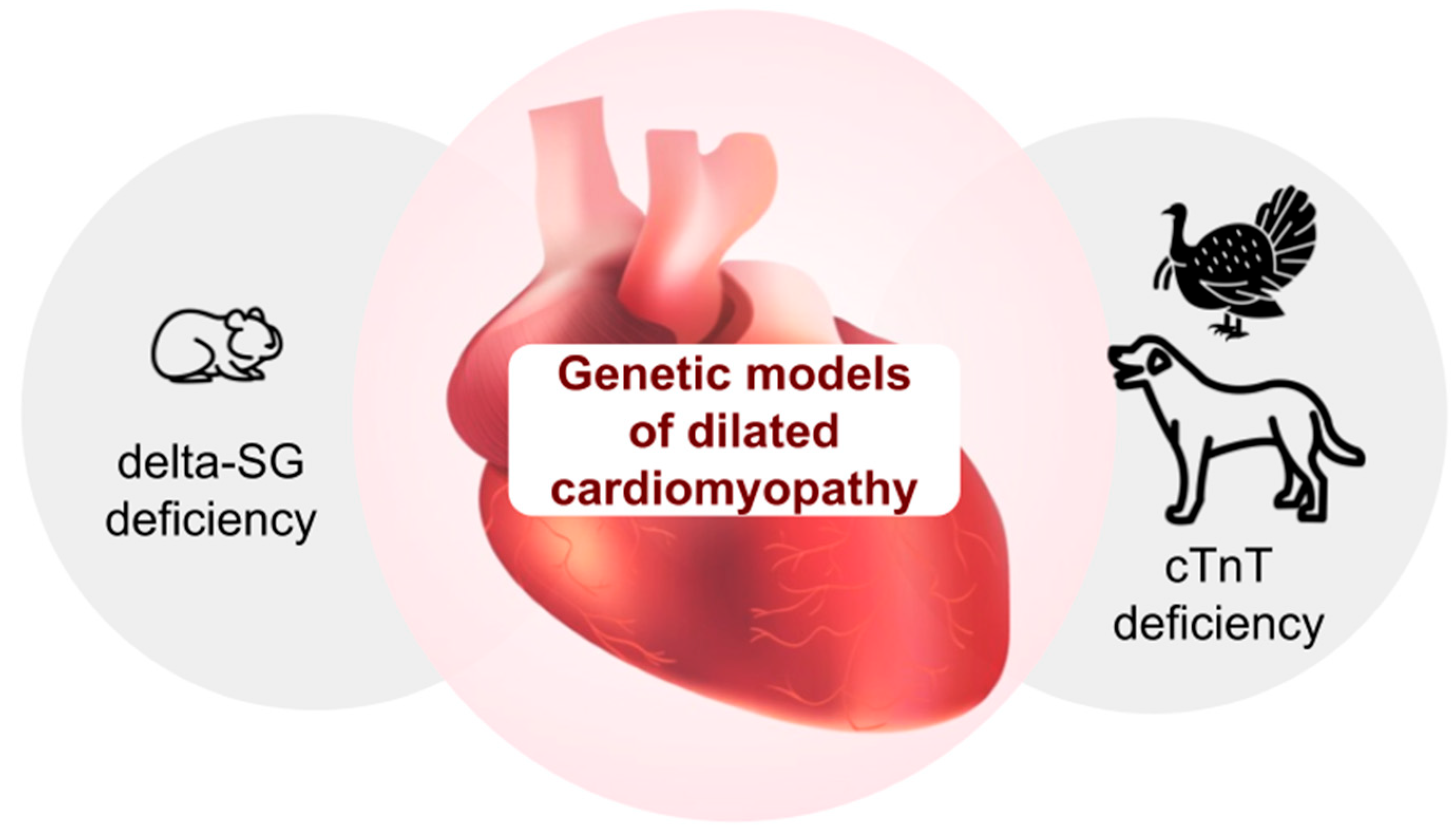
- Recchia, F.A.; Lionetti, V. Animal models of dilated cardiomyopathy for translational research. Vet. Res. Commun. 2007, 31 (Suppl. 1), 35–41. [Google Scholar] [CrossRef]
- Kaur, N.; Sharma, R.K.; Singh Kushwah, A.; Singh, N.; Thakur, S. A Comprehensive review of dilated cardiomyopathy in pre-clinical animal models in addition to herbal treatment options and multi-modality imaging strategies. Cardiovasc. Hematol. Disord. Drug Targets 2023, 22, 207–225. [Google Scholar]
- Ikeda, Y.; Ross, J.J. Models of dilated cardiomyopathy in the mouse and the hamster. Curr. Opin. Cardiol. 2000, 15, 197. [Google Scholar] [CrossRef] [PubMed]
- Gannon, M.P.; Link, M.S. Phenotypic variation and targeted therapy of hypertrophic cardiomyopathy using genetic animal models. Trends Cardiovasc. Med. 2021, 31, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Maass, A.; Leinwand, L.A. Animal models of hypertrophic cardiomyopathy. Curr. Opin. Cardiol. 2000, 15, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Yadav, S.; Sitbon, Y.H.; Kazmierczak, K.; Szczesna-Cordary, D. Hereditary heart disease: Pathophysiology, clinical presentation, and animal models of HCM, RCM and DCM associated with mutations in cardiac myosin light chains. Pflugers Arch. 2019, 471, 683–699. [Google Scholar] [CrossRef]
- Orgil, B.-O.; Purevjav, E. Molecular pathways and animal models of cardiomyopathies. Adv. Exp. Med. Biol. 2024, 1441, 991–1019. [Google Scholar]
- Gerull, B.; Brodehl, A. Genetic animal models for arrhythmogenic cardiomyopathy. Front. Physiol. 2020, 11, 624. [Google Scholar] [CrossRef]
- Niu, Y.; Sun, Y.; Liu, Y.; Du, K.; Xu, X.; Ding, Y. Using Zebrafish animal model to study the genetic underpinning and mechanism of arrhythmogenic cardiomyopathy. Int. J. Mol. Sci. 2023, 24, 4106. [Google Scholar] [CrossRef]
- Bacmeister, L.; Schwarzl, M.; Warnke, S.; Stoffers, B.; Blankenberg, S.; Westermann, D.; Lindner, D. Inflammation and fibrosis in murine models of heart failure. Basic Res. Cardiol. 2019, 114, 19. [Google Scholar] [CrossRef]
- Lerman, L.O.; Kurtz, T.W.; Touyz, R.M.; Ellison, D.H.; Chade, A.R.; Crowley, S.D.; Mattson, D.L.; Mullins, J.J.; Osborn, J.; Eirin, A.; et al. Animal models of hypertension: A scientific statement from the American heart association. Hypertension 2019, 73, e87–e120. [Google Scholar] [CrossRef]
- Tsui, B.M.W.; Kraitchman, D.L. Recent advances in small-animal cardiovascular imaging. J. Nucl. Med. 2009, 50, 667–670. [Google Scholar] [CrossRef][Green Version]
- Hickman, D.L.; Johnson, J.; Vemulapalli, T.H.; Crisler, J.R.; Shepherd, R. Chapter 7-Commonly used animal models. In Principles of Animal Research for Graduate and Undergraduate Students; Suckow, M.A., Stewart, K.L., Eds.; Academic Press: Boston, MA, USA, 2017; pp. 117–175. [Google Scholar]
- Raake, P.W.; Hinkel, R.; Müller, S.; Delker, S.; Kreuzpointner, R.; Kupatt, C.; Katus, H.A.; Kleinschmidt, J.A.; Boekstegers, P.; Müller, O.J. Cardio-specific long-term gene expression in a porcine model after selective pressure-regulated retroinfusion of adeno-associated viral (AAV) vectors. Gene Ther. 2008, 15, 12–17. [Google Scholar] [CrossRef]
- Katz, M.G.; Fargnoli, A.S.; Weber, T.; Hajjar, R.J.; Bridges, C.R. Use of adeno-associated virus vector for cardiac gene delivery in large-animal surgical models of heart failure. Hum. Gene Ther. Clin. Dev. 2017, 28, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Ni, L.; Scott, L., Jr.; Campbell, H.M.; Pan, X.; Alsina, K.M.; Reynolds, J.; Philippen, L.E.; Hulsurkar, M.; Lagor, W.R.; Li, N.; et al. Atrial-specific gene delivery using an adeno-associated viral vector. Circ. Res. 2019, 124, 256–262. [Google Scholar] [CrossRef]
- Ziegler, T.; Bozoglu, T.; Kupatt, C. AAV-mediated somatic gene editing for cardiac and skeletal muscle in a large animal model. Methods Mol. Biol. 2022, 2573, 63–74. [Google Scholar] [PubMed]
- Okamoto, K.; Aoki, K. Development of a strain of spontaneously hypertensive rats. Jpn. Circ. J. 1963, 27, 282–293. [Google Scholar] [CrossRef]
- Hallbäck, M.; Weiss, L. Mechanisms of spontaneous hypertension in rats. Med. Clin. N. Am. 1977, 61, 593–609. [Google Scholar] [CrossRef] [PubMed]
- Yamori, Y. Pathogenesis of Spontaneous Hypertension as a Model for Essential Hypertension: Symposium on pathogenesis of essential hypertension. Jpn. Circ. J. 1977, 41, 259–266. [Google Scholar] [CrossRef]
- Di Nicolantonio, R.; Lan, L.; Wilks, A. Nucleotide variations in intron 1 of the renin gene of the spontaneously hypertensive rat. Clin. Exp. Hypertens. 1998, 20, 27–40. [Google Scholar] [CrossRef]
- Yu, H.; Di Nicolantonio, R.; Lan, L.; Wilks, A. Mutations in the first intron of the SHR renin gene disrupt putative regulatory elements. Clin. Exp. Pharmacol. Physiol. 1995, 22, 450–451. [Google Scholar] [CrossRef]
- Blagonravov, M.L.; Bryk, A.A.; Goryachev, V.A.; Medvedeva, E.V.; Demurov, E.A.; Korshunova, A.Y. Bright light therapy increases blood pressure and changes the structure of circadian rhythm of melatonin secretion in spontaneously hypertensive rats. Bull. Exp. Biol. Med. 2019, 168, 214–218. [Google Scholar] [CrossRef]
- Bryk, A.A.; Blagonravov, M.L.; Goryachev, V.A.; Chibisov, S.M.; Azova, M.M.; Syatkin, S.P. Daytime exposure to blue light alters cardiovascular circadian rhythms, electrolyte excretion and melatonin production. Pathophysiology 2022, 29, 118–133. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, K.; Hazama, F.; Yamori, Y.; Haebara, H.; Nagaoka, A. Pathogenesis and prevention of stroke in spontaneously hypertensive rats. Clin. Sci. Mol. Med. 1975, 48 (Suppl. S2), 161s–163s. [Google Scholar] [CrossRef]
- Nabika, T.; Ohara, H.; Kato, N.; Isomura, M. The stroke-prone spontaneously hypertensive rat: Still a useful model for post-GWAS genetic studies? Hypertens. Res. 2012, 35, 477–484. [Google Scholar] [CrossRef]
- Bing, O.H.; Brooks, W.W.; Robinson, K.G.; Slawsky, M.T.; Hayes, J.A.; Litwin, S.E.; Sen, S.; Conrad, C.H. The spontaneously hypertensive rat as a model of the transition from compensated left ventricular hypertrophy to failure. J. Mol. Cell. Cardiol. 1995, 27, 383–396. [Google Scholar] [CrossRef]
- Bing, O.H.L.; Conrad, C.H.; Boluyt, M.O.; Robinson, K.G.; Brooks, W.W. Studies of prevention, treatment and mechanisms of heart failure in the aging spontaneously hypertensive rat. Heart Fail. Rev. 2002, 7, 71–88. [Google Scholar] [CrossRef]
- Bashyam, H. Lewis Dahl and the genetics of salt-induced hypertension. J. Exp. Med. 2007, 204, 1507. [Google Scholar] [CrossRef] [PubMed]
- Joe, B. Dr. Lewis Kitchener Dahl, the Dahl Rats and the ‘Inconvenient truth’ about the Genetics of Hypertension. Hypertension 2015, 65, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Dahl, L.K.; Heine, M.; Tassinari, L. Effects of chronia excess salt ingestion. Evidence that genetic factors play an important role in susceptibility to experimental hypertension. J. Exp. Med. 1962, 115, 1173–1190. [Google Scholar] [CrossRef]
- Garrett, M.R.; Rapp, J.P. Defining the blood pressure QTL on chromosome 7 in Dahl rats by a 177-kb congenic segment containing Cyp11b1. Mamm. Genome 2003, 14, 268–273. [Google Scholar] [CrossRef]
- Provoost, A.P.; De Keijzer, M.H. The Fawn-Hooded rat: A model for chronic renal failure. In Experimental and Genetic Rat Models of Chronic Renal Failure; Gretz, N., Strauch, M., Eds.; Karger Publishers: Basel, Switzerland, 1993. [Google Scholar]
- Kreisberg, J.I.; Karnovsky, M.J. Focal glomerular sclerosis in the fawn-hooded rat. Am. J. Pathol. 1978, 92, 637–652. [Google Scholar]
- Mattson, D.L.; Dwinell, M.R.; Greene, A.S.; Kwitek, A.E.; Roman, R.J.; Cowley, A.W.; Jacob, H.J. Chromosomal mapping of the genetic basis of hypertension and renal disease in FHH rats. Am. J. Physiol.-Ren. Physiol. 2007, 293, F1905–F1914. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Fernandez, E.; Fan, L.; Wang, S.; Liu, Y.; Gao, W.; Thomas, K.N.; Fan, F.; Roman, R.J. The adducin saga: Pleiotropic genomic targets for precision medicine in human hypertension—Vascular, renal, and cognitive diseases. Physiol. Genom. 2022, 54, 58–70. [Google Scholar] [CrossRef] [PubMed]
- Fan, F.; Geurts, A.M.; Pabbidi, M.R.; Ge, Y.; Zhang, C.; Wang, S.; Liu, Y.; Gao, W.; Guo, Y.; Li, L.; et al. A mutation in γ-adducin impairs autoregulation of renal blood flow and promotes the development of kidney disease. J. Am. Soc. Nephrol. 2020, 31, 687–700. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, G.; Fox, U.; Imbasciati, E. The development of a new strain of spontaneously hypertensive rats. Life Sci. 1974, 14, 339–347. [Google Scholar] [CrossRef]
- Gao, W.; Liu, Y.; Fan, L.; Zheng, B.; Jefferson, J.R.; Wang, S.; Zhang, H.; Fang, X.; Nguyen, B.V.; Zhu, T.; et al. Role of γ-adducin in actin cytoskeleton rearrangements in podocyte pathophysiology. Am. J. Physiol-Ren. Physiol. 2021, 320, F97–F113. [Google Scholar] [CrossRef]
- Dupont, J.; Dupont, J.C.; Froment, A.; Milon, H.; Vincent, M. Selection of three strains of rats with spontaneously different levels of blood pressure. Biomedicine 1973, 19, 36–41. [Google Scholar]
- Vincent, M.; Sassard, J. The Lyonnese strains of genetically hypertensive, normotensive, and hypotensive rats. Paroi Arterielle 1980, 6, 139–142. [Google Scholar]
- Vincent, M.; Boussaïri, E.H.; Cartier, R.; Lo, M.; Sassolas, A.; Cerutti, C.; Barrès, C.; Gustin, M.P.; Cuisinaud, G.; Samani, N.J.; et al. High blood pressure and metabolic disorders are associated in the Lyon hypertensive rat. J. Hypertens. 1993, 11, 1179–1185. [Google Scholar] [CrossRef]
- Florin, M.; Lo, M.; Liu, K.L.; Sassard, J. Salt sensitivity in genetically hypertensive rats of the Lyon strain. Kidney Int. 2001, 59, 1865–1872. [Google Scholar] [CrossRef]
- Vincent, M.; Cartier, R.; Privat, P.; Benzoni, D.; Samani, N.J.; Sassard, J. Major cardiovascular risk factors in Lyon hypertensive rats. A correlation analysis in a segregating population. J. Hypertens. 1996, 14, 469–474. [Google Scholar] [CrossRef]
- Bilusic, M.; Bataillard, A.; Tschannen, M.R.; Gao, L.; Barreto, N.E.; Vincent, M.; Wang, T.; Jacob, H.J.; Sassard, J.; Kwitek, A.E. Mapping the genetic determinants of hypertension, metabolic diseases, and related phenotypes in the Lyon hypertensive rat. Hypertension 2004, 44, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Clark, K.C.; Wagner, V.A.; Holl, K.L.; Reho, J.J.; Tutaj, M.; Smith, J.R.; Dwinell, M.R.; Grobe, J.L.; Kwitek, A.E. Body composition and metabolic changes in a Lyon hypertensive congenic rat and identification of Ercc6l2 as a positional candidate gene. Front. Genet. 2022, 13, 903971. [Google Scholar] [CrossRef]
- Ben-Ishay, D.; Saliternik, R.; Welner, A. Separation of two strains of rats with inbred dissimilar sensitivity to Doca-salt hypertension. Experientia 1972, 28, 1321–1322. [Google Scholar] [CrossRef]
- Köhler, R.; Kreutz, R.; Grundig, A.; Rothermund, L.; Yagil, C.; Yagil, Y.; Pries, A.R.; Hoyer, J. Impaired function of endothelial pressure-activated cation channel in salt-sensitive genetic hypertension. J. Am. Soc. Nephrol. 2001, 12, 1624–1629. [Google Scholar] [PubMed]
- Yagil, Y.; Yagil, C. Genetic basis of salt-susceptibility in the Sabra rat model of hypertension. Kidney Int. 1998, 53, 1493–1500. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rapp, J.P. Genetic Analysis of inherited hypertension in the rat. Physiol. Rev. 2000, 80, 135–172. [Google Scholar] [CrossRef]
- Yagil, C.; Sapojnikov, M.; Kreutz, R.; Katni, G.; Lindpaintner, K.; Ganten, D.; Yagil, Y. Salt susceptibility maps to chromosomes 1 and 17 with sex specificity in the Sabra rat model of hypertension. Hypertension 1998, 31, 119–124. [Google Scholar] [CrossRef]
- Yagil, C.; Sapojnikov, M.; Katni, G.; Ilan, Z.; Zangen, S.W.; Rosenmann, E.; Yagil, Y. Proteinuria and glomerulosclerosis in the Sabra genetic rat model of salt susceptibility. Physiol. Genom. 2002, 9, 167–178. [Google Scholar] [CrossRef][Green Version]
- Simpson, F.O.; Phelan, E.L.; Clark, D.W.J.; Jones, D.R.; Gresson, C.R.; Lee, D.R.; Bird, D.L. Studies on the New Zealand strain of genetically hypertensive rats. Clin. Sci. Mol. Med. 1973, 45, 15s–21s. [Google Scholar] [CrossRef]
- Hackbarth, H.; Gwinner, W.; Alt, J.M.; Hagemann, I.; Thiemann, A.; Finke, B. The Munich Wistar Frömter rat: Proteinuria and blood pressure in correlation to the number of superficial glomeruli. Ren. Physiol. Biochem. 1991, 14, 246–252. [Google Scholar] [CrossRef]
- van Es, N.; Schulz, A.; Ijpelaar, D.; van der Wal, A.; Kuhn, K.; Schütten, S.; Kossmehl, P.; Nyengaard, J.R.; de Heer, E.; Kreutz, R. Elimination of severe albuminuria in aging hypertensive rats by exchange of 2 chromosomes in double-consomic rats. Hypertension 2011, 58, 219–224. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schlager, G. Spontaneous hypertension in laboratory animals: A review of the genetic implications. J. Hered. 1972, 63, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Alexander, N.; Hinshaw, L.B.; Drury, D.R. Development of a strain of spontaneously hypertensive rabbits. Proc. Soc. Exp. Biol. Med. Soc. Exp. Biol. Med. 1954, 86, 855–858. [Google Scholar] [CrossRef]
- Li, D.; Wang, Q.; Zhang, Y.; Li, D.; Yang, D.; Wei, S.; Su, L.; Ye, T.; Zheng, X.; Peng, K.; et al. A novel swine model of spontaneous hypertension with sympathetic hyperactivity responds well to renal denervation. Am. J. Hypertens. 2016, 29, 63–72. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tippett, F.E.; Padgett, G.A.; Eyster, G.; Blanchard, G.; Bell, T. Primary hypertension in a colony of dogs. Hypertension 1987, 9, 49–58. [Google Scholar] [CrossRef]
- Littman, M.P.; Robertson, J.L.; Bovée, K.C. Spontaneous systemic hypertension in dogs: Five cases (1981–1983). J. Am. Vet. Med. Assoc. 1988, 193, 486–494. [Google Scholar] [CrossRef]
- Sakamoto, A. Electrical and ionic abnormalities in the heart of cardiomyopathic hamsters: In quest of a new paradigm for cardiac failure and lethal arrhythmia. Mol. Cell. Biochem. 2004, 259, 183–187. [Google Scholar] [CrossRef]
- Mancinelli, R.; Vargiu, R.; Cappai, A.; Floris, G.; Fraschini, M.; Faa, G. A metabolic approach to the treatment of dilated cardiomyopathy in BIO T0-2 cardiomyopathic Syrian hamsters. BioFactors Oxf. Engl. 2005, 25, 127–135. [Google Scholar] [CrossRef]
- Sakamoto, A.; Ono, K.; Abe, M.; Jasmin, G.; Eki, T.; Murakami, Y.; Masaki, T.; Toyo-oka, T.; Hanaoka, F. Both hypertrophic and dilated cardiomyopathies are caused by mutation of the same gene, delta-sarcoglycan, in hamster: An animal model of disrupted dystrophin-associated glycoprotein complex. Proc. Natl. Acad. Sci. USA 1997, 94, 13873–13878. [Google Scholar] [CrossRef]
- Sakamoto, A. Molecular pathogenesis of severe cardiomyopathy in the TO-2 hamster. Exp. Clin. Cardiol. 2003, 8, 143–146. [Google Scholar]
- Panchal, B.C.; Trippodo, N.C. Systemic and regional haemodynamics in conscious BIO T0-2 cardiomyopathic hamsters. Cardiovasc. Res. 1993, 27, 2264–2269. [Google Scholar] [CrossRef] [PubMed]
- England, J.; Loughna, S.; Rutland, C.S. Multiple species comparison of cardiac troponin T and dystrophin: Unravelling the DNA behind dilated cardiomyopathy. J. Cardiovasc. Dev. Dis. 2017, 4, 8. [Google Scholar] [CrossRef]
- Biesiadecki, B.J.; Elder, B.D.; Yu, Z.-B.; Jin, J.-P. Cardiac troponin T variants produced by aberrant splicing of multiple exons in animals with high instances of dilated cardiomyopathy. J. Biol. Chem. 2002, 277, 50275–50285. [Google Scholar] [CrossRef]
- Biesiadecki, B.J.; Jin, J.-P. Exon skipping in cardiac troponin T of turkeys with inherited dilated cardiomyopathy. J. Biol. Chem. 2002, 277, 18459–18468. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.N.; Parvatiyar, M.S.; Potter, J.D. Troponin and cardiomyopathy. Biochem. Biophys. Res. Commun. 2008, 369, 74–81. [Google Scholar] [CrossRef]
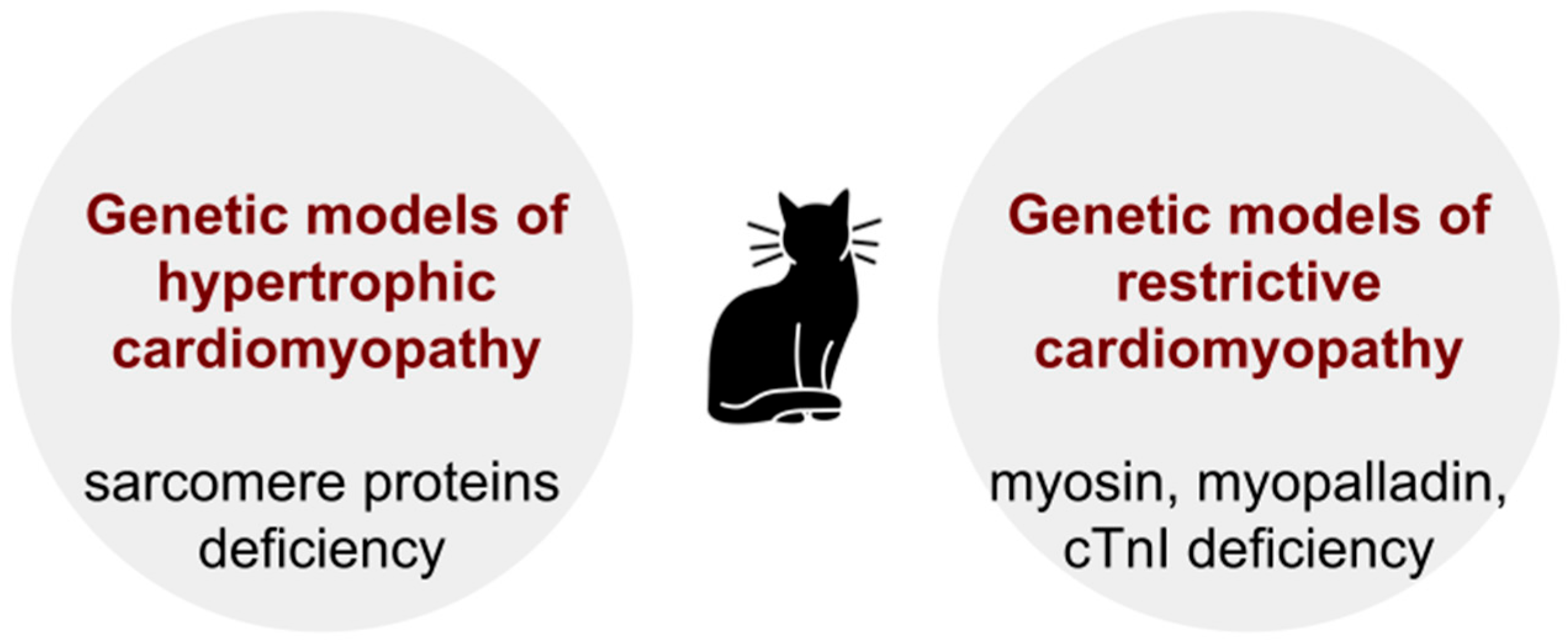
- Marsiglia, J.D.C.; Pereira, A.C. Hypertrophic Cardiomyopathy: How do mutations lead to disease? Arq. Bras. Cardiol. 2014, 102, 295–304. [Google Scholar] [CrossRef]
- Sweet, M.; Taylor, M.R.G.; Mestroni, L. Diagnosis, prevalence, and screening of familial dilated cardiomyopathy. Expert. Opin. Orphan. Drugs 2015, 3, 869–876. [Google Scholar] [CrossRef] [PubMed]
- Grünig, E.; Tasman, J.A.; Kücherer, H.; Franz, W.; Kübler, W.; Katus, H.A. Frequency and phenotypes of familial dilated cardiomyopathy. J. Am. Coll. Cardiol. 1998, 31, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, S.K.; Arnett, D.K.; Assimes, T.L.; Basson, C.T.; Chakravarti, A.; Ellinor, P.T.; Engler, M.B.; Goldmuntz, E.; Herrington, D.M.; Hershberger, R.E.; et al. Genetics and genomics for the prevention and treatment of cardiovascular disease: Update: A scientific statement from the American Heart Association. Circulation 2013, 128, 2813–2851. [Google Scholar] [CrossRef]
- Lopes, L.R.; Ho, C.Y.; Elliott, P.M. Genetics of hypertrophic cardiomyopathy: Established and emerging implications for clinical practice. Eur. Heart J. 2024, 45, 2727–2734. [Google Scholar] [CrossRef]
- Teekakirikul, P.; Zhu, W.; Huang, H.C.; Fung, E. Hypertrophic cardiomyopathy: An overview of genetics and management. Biomolecules 2019, 9, 878. [Google Scholar] [CrossRef] [PubMed]
- Topriceanu, C.-C.; Pereira, A.C.; Moon, J.C.; Captur, G.; Ho, C.Y. Meta-analysis of penetrance and systematic review on transition to disease in genetic hypertrophic cardiomyopathy. Circulation 2024, 149, 107–123. [Google Scholar] [CrossRef] [PubMed]
- Bos, J.M.; Towbin, J.A.; Ackerman, M.J. Diagnostic, prognostic, and therapeutic implications of genetic testing for hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2009, 54, 201–211. [Google Scholar] [CrossRef]
- Authors/Task Force members; Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; Hagege, A.A.; Lafont, A.; Limongelli, G.; et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The task force for the diagnosis and management of hypertrophic cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2733–2779. [Google Scholar]
- Freeman, L.M.; Rush, J.E.; Stern, J.A.; Huggins, G.S.; Maron, M.S. Feline hypertrophic cardiomyopathy: A spontaneous large animal model of human HCM. Cardiol. Res. 2017, 8, 139. [Google Scholar] [CrossRef] [PubMed]
- Payne, J.R.; Brodbelt, D.C.; Luis Fuentes, V. Cardiomyopathy prevalence in 780 apparently healthy cats in rehoming centres (the CatScan study). J. Vet. Cardiol. 2015, 17, S244–S257. [Google Scholar] [CrossRef]
- Kittleson, M.D.; Meurs, K.M.; Munro, M.J.; Kittleson, J.A.; Liu, S.K.; Pion, P.D.; Towbin, J.A. Familial hypertrophic cardiomyopathy in maine coon cats: An animal model of human disease. Circulation 1999, 99, 3172–3180. [Google Scholar] [CrossRef]
- Fox, P.R. Hypertrophic cardiomyopathy. Clinical and pathologic correlates. J. Vet. Cardiol. 2003, 5, 39–45. [Google Scholar] [CrossRef]
- Kittleson, M.D.; Meurs, K.M.; Harris, S.P. The genetic basis of hypertrophic cardiomyopathy in cats and humans. J. Vet. Cardiol. 2015, 17, S53–S73. [Google Scholar] [CrossRef]
- Ripoll Vera, T.; Monserrat Iglesias, L.; Hermida Prieto, M.; Ortiz, M.; Rodriguez Garcia, I.; Govea Callizo, N.; Gómez Navarro, C.; Rosell Andreo, J.; Gámez Martínez, J.M.; Pons Lladó, G.; et al. The R820W mutation in the MYBPC3 gene, associated with hypertrophic cardiomyopathy in cats, causes hypertrophic cardiomyopathy and left ventricular non-compaction in humans. Int. J. Cardiol. 2010, 145, 405–407. [Google Scholar] [CrossRef]
- Chintanaphol, M.; Orgil, B.-O.; Alberson, N.R.; Towbin, J.A.; Purevjav, E. Restrictive cardiomyopathy: From genetics and clinical overview to animal modeling. Rev. Cardiovasc. Med. 2022, 23, 108. [Google Scholar] [CrossRef] [PubMed]
- Towbin, J.A. Inherited cardiomyopathies. Circ. J. 2014, 78, 2347–2356. [Google Scholar] [CrossRef]
- Parvatiyar, M.S.; Pinto, J.R.; Dweck, D.; Potter, J.D. Cardiac troponin mutations and restrictive cardiomyopathy. J. Biomed. Biotechnol. 2010, 2010, 350706. [Google Scholar] [CrossRef]
- Fox, P.R.; Basso, C.; Thiene, G.; Maron, B.J. Spontaneously occurring restrictive nonhypertrophied cardiomyopathy in domestic cats: A new animal model of human disease. Cardiovasc. Pathol. 2014, 23, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Karakama, S.; Hirakawa, A.; Tsuchiaka, S.; Kobayashi, M.; Machida, N. Pathological features and pathogenesis of the endomyocardial form of restrictive cardiomyopathy in cats. J. Comp. Pathol. 2016, 155, 190–198. [Google Scholar] [CrossRef] [PubMed]
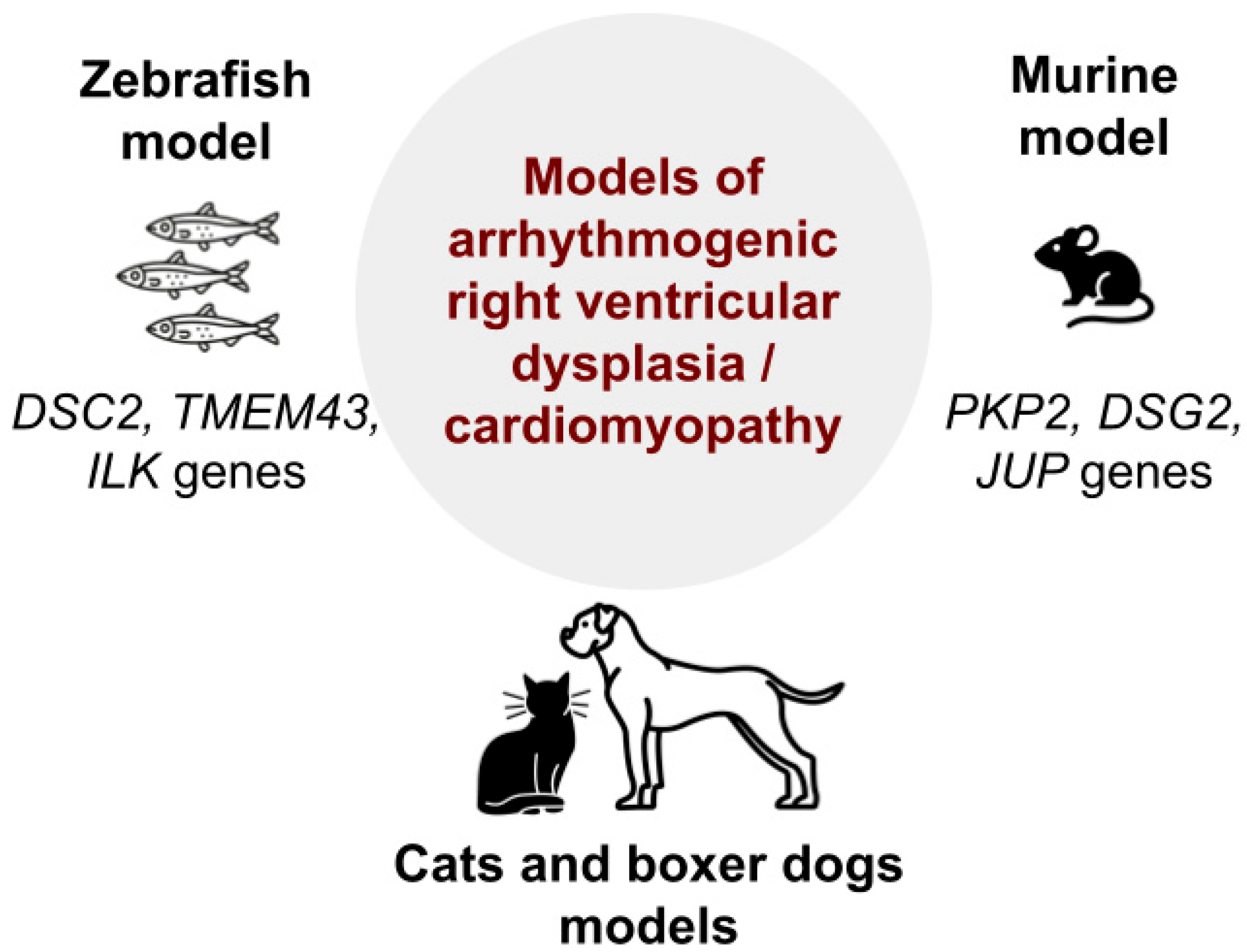
- Padrón-Barthe, L.; Domínguez, F.; Garcia-Pavia, P.; Lara-Pezzi, E. Animal models of arrhythmogenic right ventricular cardiomyopathy: What have we learned and where do we go? Insight for therapeutics. Basic Res. Cardiol. 2017, 112, 50. [Google Scholar] [CrossRef]
- Gallicano, G.I.; Kouklis, P.; Bauer, C.; Yin, M.; Vasioukhin, V.; Degenstein, L.; Fuchs, E. Desmoplakin is required early in development for assembly of desmosomes and cytoskeletal linkage. J. Cell Biol. 1998, 143, 2009–2022. [Google Scholar] [CrossRef]
- Garrod, D.; Chidgey, M. Desmosome structure, composition and function. Biochim. Biophys. Acta 2008, 1778, 572–587. [Google Scholar] [CrossRef]
- Eshkind, L.; Tian, Q.; Schmidt, A.; Franke, W.W.; Windoffer, R.; Leube, R.E. Loss of desmoglein 2 suggests essential functions for early embryonic development and proliferation of embryonal stem cells. Eur. J. Cell Biol. 2002, 81, 592–598. [Google Scholar] [CrossRef]
- Bierkamp, C.; Mclaughlin, K.J.; Schwarz, H.; Huber, O.; Kemler, R. Embryonic heart and skin defects in mice lacking plakoglobin. Dev. Biol. 1996, 180, 780–785. [Google Scholar] [CrossRef]
- Li, J.; Swope, D.; Raess, N.; Cheng, L.; Muller, E.J.; Radice, G.L. Cardiac tissue-restricted deletion of plakoglobin results in progressive cardiomyopathy and activation of {beta}-catenin signaling. Mol. Cell Biol. 2011, 31, 1134–1144. [Google Scholar] [CrossRef]
- Merner, N.D.; Hodgkinson, K.A.; Haywood, A.F.; Connors, S.; French, V.M.; Drenckhahn, J.D.; Kupprion, C.; Ramadanova, K.; Thierfelder, L.; McKenna, W.; et al. Arrhythmogenic right ventricular cardiomyopathy type 5 is a fully penetrant, lethal arrhythmic disorder caused by a missense mutation in the TMEM43 gene. Am. J. Hum. Genet. 2008, 82, 809–821. [Google Scholar] [CrossRef] [PubMed]
- Brodehl, A.; Rezazadeh, S.; Williams, T.; Munsie, N.M.; Liedtke, D.; Oh, T.; Ferrier, R.; Shen, Y.; Jones, S.J.M.; Stiegler, A.L.; et al. Mutations in ILK, encoding integrin-linked kinase, are associated with arrhythmogenic cardiomyopathy. Transl. Res. 2019, 208, 15–29. [Google Scholar] [CrossRef]
- van Tintelen, J.P.; Entius, M.M.; Bhuiyan, Z.A.; Jongbloed, R.; Wiesfeld, A.C.; Wilde, A.A.; van der Smagt, J.; Boven, L.G.; Mannens, M.M.; van Langen, I.M.; et al. Plakophilin-2 mutations are the major determinant of familial arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circulation 2006, 113, 1650–1658. [Google Scholar] [CrossRef]
- Grossmann, K.S.; Grund, C.; Huelsken, J.; Behrend, M.; Erdmann, B.; Franke, W.W.; Birchmeier, W. Requirement of plakophilin 2 for heart morphogenesis and cardiac junction formation. J. Cell Biol. 2004, 167, 149–160. [Google Scholar] [CrossRef]
- Pilichou, K.; Remme, C.A.; Basso, C.; Campian, M.E.; Rizzo, S.; Barnett, P.; Scicluna, B.P.; Bauce, B.; van den Hoff, M.J.; de Bakker, J.M.; et al. Myocyte necrosis underlies progressive myocardial dystrophy in mouse dsg2-related arrhythmogenic right ventricular cardiomyopathy. J. Exp. Med. 2009, 206, 1787–1802. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.N.; Gurha, P.; Lombardi, R.; Ruggiero, A.; Willerson, J.T.; Marian, A.J. The hippo pathway is activated and is a causal mechanism for adipogenesis in arrhythmogenic cardiomyopathy. Circ. Res. 2014, 114, 454–468. [Google Scholar] [CrossRef]
- Heuser, A.; Plovie, E.R.; Ellinor, P.T.; Grossmann, K.S.; Shin, J.T.; Wichter, T.; Basson, C.T.; Lerman, B.B.; Sasse-Klaassen, S.; Thierfelder, L.; et al. Mutant desmocollin-2 causes arrhythmogenic right ventricular cardiomyopathy. Am. J. Hum. Genet. 2006, 79, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Zink, M.; Seewald, A.; Rohrbach, M.; Brodehl, A.; Liedtke, D.; Williams, T.; Childs, S.J.; Gerull, B. Altered expression of TMEM43 causes abnormal cardiac structure and function in Zebrafish. Int. J. Mol. Sci. 2022, 23, 9530. [Google Scholar] [CrossRef]
- Basso, C.; Fox, P.R.; Meurs, K.M.; Towbin, J.A.; Spier, A.W.; Calabrese, F.; Maron, B.J.; Thiene, G. Arrhythmogenic right ventricular cardiomyopathy causing sudden cardiac death in boxer dogs: A new animal model of human disease. Circulation 2004, 109, 1180–1185. [Google Scholar] [CrossRef]
- Fox, P.R.; Maron, B.J.; Basso, C.; Liu, S.K.; Thiene, G. Spontaneously occurring arrhythmogenic right ventricular cardiomyopathy in the domestic cat: A new animal model similar to the human disease. Circulation 2000, 102, 1863–1870. [Google Scholar] [CrossRef]
- Buja, L.M.; Kita, T.; Goldstein, J.L.; Watanabe, Y.; Brown, M.S. Cellular pathology of progressive atherosclerosis in the WHHL rabbit. An animal model of familial hypercholesterolemia. Arteriosclerosis 1983, 3, 87–101. [Google Scholar] [CrossRef]
- Buja, L.M.; Clubb, F.J.; Bilheimer, D.W.; Willerson, J.T. Pathobiology of human familial hypercholesterolaemia and a related animal model, the Watanabe heritable hyperlipidaemic rabbit. Eur. Heart J. 1990, 11 (Suppl. E), 41–52. [Google Scholar] [CrossRef] [PubMed]
- Aliev, G.; Burnstock, G. Watanabe rabbits with heritable hypercholesterolaemia: A model of atherosclerosis. Histol. Histopathol. 1998, 13, 797–817. [Google Scholar]
- Nolte, C.J.; Tercyak, A.M.; Wu, H.M.; Small, D.M. Chemical and physiochemical comparison of advanced atherosclerotic lesions of similar size and cholesterol content in cholesterol-fed New Zealand white and Watanabe heritable hyperlipidemic rabbits. Lab. Investig. J. Tech. Methods Pathol. 1990, 62, 213–222. [Google Scholar]
- Shiomi, M.; Ito, T.; Yamada, S.; Kawashima, S.; Fan, J. Development of an animal model for spontaneous myocardial infarction (WHHLMI rabbit). Arterioscler. Thromb. Vasc. Biol. 2003, 23, 1239–1244. [Google Scholar] [CrossRef]
- Shiomi, M.; Fan, J. Unstable coronary plaques and cardiac events in myocardial infarction-prone Watanabe heritable hyperlipidemic rabbits: Questions and quandaries. Curr. Opin. Lipidol. 2008, 19, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Shiomi, M.; Yamada, S.; Ito, T. Atheroma stabilizing effects of simvastatin due to depression of macrophages or lipid accumulation in the atheromatous plaques of coronary plaque-prone WHHL rabbits. Atherosclerosis 2005, 178, 287–294. [Google Scholar] [CrossRef]
- Suzuki, H.; Kobayashi, H.; Sato, F.; Yonemitsu, Y.; Nakashima, Y.; Sueishi, K. Plaque-stabilizing effect of pitavastatin in Watanabe heritable hyperlipidemic (WHHL) rabbits. J. Atheroscler. Thromb. 2003, 10, 109–116. [Google Scholar] [CrossRef][Green Version]
- Li, S.; Liang, J.; Niimi, M.; Bilal Waqar, A.; Kang, D.; Koike, T.; Wang, Y.; Shiomi, M.; Fan, J. Probucol suppresses macrophage infiltration and MMP expression in atherosclerotic plaques of WHHL rabbits. J. Atheroscler. Thromb. 2014, 21, 648–658. [Google Scholar] [CrossRef]
- Kurokawa, J.; Hayashi, K.; Toyota, Y.; Shingu, T.; Shiomi, M.; Kajiyama, G. High dose of fluvastatin sodium (XU62-320), a new inhibitor of 3-hydroxy-3-methylglutaryl coenzyme A reductase, lowers plasma cholesterol levels in homozygous Watanabe-heritable hyperlipidemic rabbits. Biochim. Biophys. Acta 1995, 1259, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Shiomi, M.; Yamada, S.; Amano, Y.; Nishimoto, T.; Ito, T. Lapaquistat acetate, a squalene synthase inhibitor, changes macrophage/lipid-rich coronary plaques of hypercholesterolaemic rabbits into fibrous lesions. Br. J. Pharmacol. 2008, 154, 949–957. [Google Scholar] [CrossRef] [PubMed]
- Imanishi, T.; Kuroi, A.; Ikejima, H.; Kobayashi, K.; Muragaki, Y.; Mochizuki, S.; Goto, M.; Yoshida, K.; Akasaka, T. Effects of angiotensin converting enzyme inhibitor and angiotensin II receptor antagonist combination on nitric oxide bioavailability and atherosclerotic change in Watanabe heritable hyperlipidemic rabbits. Hypertens. Res. 2008, 31, 575–584. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shiomi, M. The history of the WHHL rabbit, an animal model of familial hypercholesterolemia (II). J. Atheroscler. Thromb. 2020, 27, 119–131. [Google Scholar] [CrossRef]
- Chowdhury, J.R.; Grossman, M.; Gupta, S.; Chowdhury, N.R.; Baker, J.R.; Wilson, J.M. Long-term improvement of hypercholesterolemia after ex vivo gene therapy in LDLR-deficient rabbits. Science 1991, 254, 1802–1805. [Google Scholar] [CrossRef]
- Fan, J.; Chen, Y.; Yan, H.; Liu, B.; Wang, Y.; Zhang, J.; Chen, Y.E.; Liu, E.; Liang, J. Genomic and transcriptomic analysis of hypercholesterolemic rabbits: Progress and perspectives. Int. J. Mol. Sci. 2018, 19, 3512. [Google Scholar] [CrossRef]
- Zhang, J.; Niimi, M.; Yang, D.; Liang, J.; Xu, J.; Kimura, T.; Mathew, A.V.; Guo, Y.; Fan, Y.; Zhu, T.; et al. Deficiency of cholesteryl ester transfer protein protects against atherosclerosis in rabbits. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 1068–1075. [Google Scholar] [CrossRef]
- Bruter, A.V.; Varlamova, E.A.; Okulova, Y.D.; Tatarskiy, V.V.; Silaeva, Y.Y.; Filatov, M.A. Genetically modified mice as a tool for the study of human diseases. Mol. Biol. Rep. 2014, 51, 135. [Google Scholar] [CrossRef]
- Guy, L.-G.; Kothary, R.; Wall, L. Position effects in mice carrying a lacZ transgene in cis with the β-globin LCR can be explained by a graded model. Nucleic. Acids Res. 1997, 25, 4400–4407. [Google Scholar] [CrossRef]
- Grigliatti, T.; Mottus, R.C. Position effects. In Brenner’s Encyclopedia of Genetics, 2nd ed.; Maloy, S., Hughes, K., Eds.; Academic Press: San Diego, CA, USA, 2013; pp. 418–420. [Google Scholar]
- Jänsch, M.; Lubomirov, L.T.; Trum, M.; Williams, T.; Schmitt, J.; Schuh, K.; Qadri, F.; Maier, L.S.; Bader, M.; Ritter, O. Inducible over-expression of cardiac Nos1ap causes short QT syndrome in transgenic mice. FEBS Open Bio 2023, 13, 118–132. [Google Scholar] [CrossRef]
- Gallini, R.; Lindblom, P.; Bondjers, C.; Betsholtz, C.; Andrae, J. PDGF-A and PDGF-B induces cardiac fibrosis in transgenic mice. Exp. Cell Res. 2016, 349, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Brodehl, A.; Belke, D.D.; Garnett, L.; Martens, K.; Abdelfatah, N.; Rodriguez, M.; Diao, C.; Chen, Y.X.; Gordon, P.M.; Nygren, A.; et al. Transgenic mice overexpressing desmocollin-2 (DSC2) develop cardiomyopathy associated with myocardial inflammation and fibrotic remodeling. PLoS ONE 2017, 12, e0174019. [Google Scholar] [CrossRef]
- Carroll, K.J.; Makarewich, C.A.; McAnally, J.; Anderson, D.M.; Zentilin, L.; Liu, N.; Giacca, M.; Bassel-Duby, R.; Olson, E.N. A mouse model for adult cardiac-specific gene deletion with CRISPR/Cas9. Proc. Natl. Acad. Sci. USA 2016, 113, 338–343. [Google Scholar] [CrossRef]
- Singh Angom, R.; Wang, Y.; Wang, E.; Dutta, S.K.; Mukhopadhyay, D. Conditional, tissue-specific CRISPR/Cas9 vector system in Zebrafish reveals the role of Nrp1b in heart regeneration. Arterioscler. Thromb. Vasc. Biol. 2023, 43, 1921–1934. [Google Scholar] [CrossRef]
- Hoofnagle, M.H.; Neppl, R.L.; Berzin, E.L.; Teg Pipes, G.C.; Olson, E.N.; Wamhoff, B.W.; Somlyo, A.V.; Owens, G.K. Myocardin is differentially required for the development of smooth muscle cells and cardiomyocytes. Am. J. Physiol. Heart Circ. Physiol. 2011, 300, H1707–H1721. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Adastra, K.L.; Frolova, A.I.; Chi, M.M.; Cusumano, D.; Bade, M.; Carayannopoulos, M.O.; Moley, K.H. Slc2a8 deficiency in mice results in reproductive and growth impairments. Biol. Reprod. 2012, 87, 49. [Google Scholar] [CrossRef] [PubMed]
- Crotti, L.; Johnson, C.N.; Graf, E.; De Ferrari, G.M.; Cuneo, B.F.; Ovadia, M.; Papagiannis, J.; Feldkamp, M.D.; Rathi, S.G.; Kunic, J.D.; et al. Calmodulin mutations associated with recurrent cardiac arrest in infants. Circulation 2013, 127, 1009–1017. [Google Scholar] [CrossRef]
- Verdonschot, J.A.J.; Vanhoutte, E.K.; Claes, G.R.F.; Helderman-van den Enden, A.T.J.M.; Hoeijmakers, J.G.J.; Hellebrekers, D.M.E.I.; de Haan, A.; Christiaans, I.; Lekanne Deprez, R.H.; Boen, H.M.; et al. A mutation update for the FLNC gene in myopathies and cardiomyopathies. Hum. Mutat. 2020, 41, 1091–1111. [Google Scholar] [CrossRef]
- Badura, K.; Buławska, D.; Dąbek, B.; Witkowska, A.; Lisińska, W.; Radzioch, E.; Skwira, S.; Młynarska, E.; Rysz, J.; Franczyk, B. Primary electrical heart disease—Principles of pathophysiology and genetics. Int. J. Mol. Sci. 2024, 25, 1826. [Google Scholar] [CrossRef]
- Rivolta, I.; Binda, A.; Masi, A.; DiFrancesco, J.C. Cardiac and neuronal HCN channelopathies. Pflugers Arch. 2020, 472, 931–951. [Google Scholar] [CrossRef]
- Crotti, L.; Brugada, P.; Calkins, H.; Chevalier, P.; Conte, G.; Finocchiaro, G.; Postema, P.G.; Probst, V.; Schwartz, P.J.; Behr, E.R. From gene-discovery to gene-tailored clinical management: 25 years of research in channelopathies and cardiomyopathies. Europace 2023, 25, euad180. [Google Scholar] [CrossRef] [PubMed]
- Charpentier, F.; Bourgé, A.; Mérot, J. Mouse models of SCN5A-related cardiac arrhythmias. Prog. Biophys. Mol. Biol. 2008, 98, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Marchal, G.A.; Rivaud, M.R.; Wolswinkel, R.; Basso, C.; van Veen, T.A.B.; Bezzina, C.R.; Remme, C.A. Genetic background determines the severity of age-dependent cardiac structural abnormalities and arrhythmia susceptibility in Scn5a-1798insD mice. Europace 2024, 26, euae153. [Google Scholar] [CrossRef]
- Higashikuni, Y.; Liu, W.; Numata, G.; Tanaka, K.; Fukuda, D.; Tanaka, Y.; Hirata, Y.; Imamura, T.; Takimoto, E.; Komuro, I.; et al. NLRP3 inflammasome activation through heart-brain interaction initiates cardiac inflammation and hypertrophy during pressure overload. Circulation 2023, 147, 338–355. [Google Scholar] [CrossRef] [PubMed]
- Lebek, S.; Caravia, X.M.; Straub, L.G.; Alzhanov, D.; Tan, W.; Li, H.; McAnally, J.R.; Chen, K.; Xu, L.; Scherer, P.E.; et al. CRISPR-Cas9 base editing of pathogenic CaMKIIδ improves cardiac function in a humanized mouse model. J. Clin. Investig. 2024, 134, e175164. [Google Scholar] [CrossRef]
- Ma, Z.G.; Yuan, Y.P.; Fan, D.; Zhang, X.; Teng, T.; Song, P.; Kong, C.Y.; Hu, C.; Wei, W.Y.; Tang, Q.Z. IRX2 regulates angiotensin II-induced cardiac fibrosis by transcriptionally activating EGR1 in male mice. Nat. Commun. 2023, 14, 4967. [Google Scholar] [CrossRef]
- Choy, L.; Yeo, J.M.; Tse, V.; Chan, S.P.; Tse, G. Cardiac disease and arrhythmogenesis: Mechanistic insights from mouse models. Int. J. Cardiol. Heart Vasc. 2016, 12, 1–10. [Google Scholar] [CrossRef]
- Tamargo, J.; Caballero, R.; Núñez, L.; Gómez, R.; Vaquero, M.; Delpón, E. Genetically engineered mice as a model for studying cardiac arrhythmias. Front. Biosci. J. Virtual. Libr. 2007, 12, 22–38. [Google Scholar] [CrossRef][Green Version]
- Dobrev, D.; Wehrens, X.H.T. Mouse models of cardiac arrhythmias. Circ. Res. 2018, 123, 332–334. [Google Scholar] [CrossRef]
- Sharma, A.K.; Singh, S.; Bhat, M.; Gill, K.; Zaid, M.; Kumar, S.; Shakya, A.; Tantray, J.; Jose, D.; Gupta, R.; et al. New drug discovery of cardiac anti-arrhythmic drugs: Insights in animal models. Sci. Rep. 2023, 13, 16420. [Google Scholar] [CrossRef]
- Sun, W.; Liu, X.; Song, L.; Tao, L.; Lai, K.; Jiang, H.; Xiao, H. The TTN p. Tyr4418Ter mutation causes cardiomyopathy in human and mice. PLoS ONE 2024, 19, e0296802. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Liu, Z.; Sun, J.; Chen, Z.; Gao, F.; Guo, Y. Adenine base editor-based correction of the cardiac pathogenic Lmna c.1621C > T mutation in murine hearts. J. Cell Mol. Med. 2024, 28, e18145. [Google Scholar] [CrossRef]
- Huang, J.Y.; Kan, S.H.; Sandfeld, E.K.; Dalton, N.D.; Rangel, A.D.; Chan, Y.; Davis-Turak, J.; Neumann, J.; Wang, R.Y. CRISPR-Cas9 generated pompe knock-in murine model exhibits early-onset hypertrophic cardiomyopathy and skeletal muscle weakness. Sci. Rep. 2020, 10, 10321. [Google Scholar] [CrossRef]
- Xia, Y.; Hu, J.; Li, X.; Zheng, S.; Wang, G.; Tan, S.; Zou, Z.; Ling, Q.; Yang, F.; Fan, X. Investigating the pathogenesis of MYH7 mutation Gly823Glu in familial hypertrophic cardiomyopathy using a mouse model. J. Vis. Exp. 2022, 186. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Han, M.; Liang, L.; Song, Q.; Li, X.; Du, Y.; Hu, D.; Cheng, Y.; Wang, Q.K.; Ke, T. Mog1 deficiency promotes cardiac contractile dysfunction and isoproterenol-induced arrhythmias associated with cardiac fibrosis and Cx43 remodeling. Biochim. Biophys. Acta Mol. Basis Dis. 2022, 1868, 166429. [Google Scholar] [CrossRef]
- Hu, Z.; Crump, S.M.; Anand, M.; Kant, R.; Levi, R.; Abbott, G.W. Kcne3 deletion initiates extracardiac arrhythmogenesis in mice. FASEB J. 2014, 28, 935–945. [Google Scholar] [CrossRef]
- Frasier, C.R.; Wagnon, J.L.; Bao, Y.O.; McVeigh, L.G.; Lopez-Santiago, L.F.; Meisler, M.H.; Isom, L.L. Cardiac arrhythmia in a mouse model of sodium channel SCN8A epileptic encephalopathy. Proc. Natl. Acad. Sci. USA 2016, 113, 12838–12843. [Google Scholar] [CrossRef] [PubMed]
- Padua, M.B.; Helm, B.M.; Wells, J.R.; Smith, A.M.; Bellchambers, H.M.; Sridhar, A.; Ware, S.M. Congenital heart defects caused by FOXJ1. Hum. Mol. Genet. 2023, 32, 2335–2346. [Google Scholar] [CrossRef] [PubMed]
- Marguerie, A.; Bajolle, F.; Zaffran, S.; Brown, N.A.; Dickson, C.; Buckingham, M.E.; Kelly, R.G. Congenital heart defects in Fgfr2-IIIb and Fgf10 mutant mice. Cardiovasc. Res. 2006, 71, 50–60. [Google Scholar] [CrossRef]
- Yu, Z.; Tang, P.L.; Wang, J.; Bao, S.; Shieh, J.T.; Leung, A.W.; Zhang, Z.; Gao, F.; Wong, S.Y.; Hui, A.L.; et al. Mutations in Hnrnpa1 cause congenital heart defects. JCI Insight 2018, 3, e98555. [Google Scholar] [CrossRef]
- Ilchuk, L.A.; Kochegarova, K.K.; Baikova, I.P.; Safonova, P.D.; Bruter, A.V.; Kubekina, M.V.; Okulova, Y.D.; Minkovskaya, T.E.; Kuznetsova, N.A.; Dolmatova, D.M.; et al. Mutations in filamin C associated with both alleles do not affect the functioning of mice cardiac muscles. Int. J. Mol. Sci. 2025, 26, 1409. [Google Scholar] [CrossRef] [PubMed]
- Filatov, M.A.; Ilchuk, L.A.; Baikova, I.P. E12.5 whole mouse embryo culture. Reprod. Biol. 2025, 25, 100995. [Google Scholar] [CrossRef] [PubMed]
- Yue, Y.; Zong, W.; Li, X.; Li, J.; Zhang, Y.; Wu, R.; Liu, Y.; Cui, J.; Wang, Q.; Bian, Y.; et al. Long-term, in toto live imaging of cardiomyocyte behaviour during mouse ventricle chamber formation at single-cell resolution. Nat. Cell Biol. 2020, 22, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Angom, R.S.; Nakka, N.M.R. Zebrafish as a model for cardiovascular and metabolic disease: The future of precision medicine. Biomedicines 2024, 12, 693. [Google Scholar] [CrossRef]
- Verkerk, L.; Verkerk, A.O.; Wilders, R. Zebrafish as a model system for Brugada syndrome. Rev. Cardiovasc. Med. 2024, 25, 313. [Google Scholar] [CrossRef]
- Ding, Y.; Dvornikov, A.V.; Ma, X.; Zhang, H.; Wang, Y.; Lowerison, M.; Packard, R.R.; Wang, L.; Chen, J.; Zhang, Y.; et al. Haploinsufficiency of mechanistic target of rapamycin ameliorates bag3 cardiomyopathy in adult zebrafish. Dis. Model. Mech. 2019, 12, dmm040154. [Google Scholar] [CrossRef]
- Chen, D.; Zhang, Z.; Chen, C.; Yao, S.; Yang, Q.; Li, F.; He, X.; Ai, C.; Wang, M.; Guan, M.X. Deletion of Gtpbp3 in zebrafish revealed the hypertrophic cardiomyopathy manifested by aberrant mitochondrial tRNA metabolism. Nucleic. Acids Res. 2019, 47, 5341–5355. [Google Scholar] [CrossRef]
- Orr, N.; Arnaout, R.; Gula, L.J.; Spears, D.A.; Leong-Sit, P.; Li, Q.; Tarhuni, W.; Reischauer, S.; Chauhan, V.S.; Borkovich, M.; et al. A mutation in the atrial-specific myosin light chain gene (MYL4) causes familial atrial fibrillation. Nat. Commun. 2016, 7, 11303. [Google Scholar] [CrossRef]
- Shih, Y.-H.; Zhang, Y.; Ding, Y.; Ross, C.A.; Li, H.; Olson, T.M.; Xu, X. Cardiac transcriptome and dilated cardiomyopathy genes in zebrafish. Circ. Cardiovasc. Genet. 2015, 8, 261–269. [Google Scholar] [CrossRef]
- Kimmel, C.B.; Ballard, W.W.; Kimmel, S.R.; Ullmann, B.; Schilling, T.F. Stages of embryonic development of the zebrafish. Dev. Dyn. 1995, 203, 253–310. [Google Scholar] [CrossRef]
- Varshney, G.K.; Sood, R.; Burgess, S.M. Understanding and editing the Zebrafish genome. Adv. Genet. 2015, 92, 1–52. [Google Scholar]
- Xu, J.; Zhang, J.; Yang, D.; Song, J.; Pallas, B.; Zhang, C.; Hu, J.; Peng, X.; Christensen, N.D.; Han, R.; et al. Gene editing in rabbits: Unique opportunities for translational biomedical research. Front. Genet. 2021, 12, 642444. [Google Scholar] [CrossRef] [PubMed]
- Silaeva, Y.Y.; Safonova, P.D.; Popov, D.V.; Filatov, M.A.; Okulova, Y.D.; Shafei, R.A.; Skobel, O.I.; Vysotskii, D.E.; Gubarev, Y.D.; Glazko, V.I.; et al. Generation of LEPR knockout rabbits with CRISPR/CAS9 system. Dokl. Biol. Sci. 2024, 518, 248–255. [Google Scholar] [CrossRef]
- Fan, J.; Niimi, M.; Chen, Y.; Suzuki, R.; Liu, E. Use of rabbit models to study atherosclerosis. Methods Mol. Biol. 2022, 2419, 413–431. [Google Scholar] [PubMed]
- Fan, J.; Kitajima, S.; Watanabe, T.; Xu, J.; Zhang, J.; Liu, E.; Chen, Y.E. Rabbit models for the study of human atherosclerosis: From pathophysiological mechanisms to translational medicine. Pharmacol. Ther. 2015, 146, 104–119. [Google Scholar] [CrossRef]
- Yan, Q.; Zhang, Q.; Yang, H.; Zou, Q.; Tang, C.; Fan, N.; Lai, L. Generation of multi-gene knockout rabbits using the Cas9/gRNA system. Cell Regen. 2014, 3, 12. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lv, Q.; Yuan, L.; Deng, J.; Chen, M.; Wang, Y.; Zeng, J.; Li, Z.; Lai, L. Efficient generation of myostatin gene mutated rabbit by CRISPR/Cas9. Sci. Rep. 2016, 6, 25029. [Google Scholar] [CrossRef]
- Hashikawa, Y.; Hayashi, R.; Tajima, M.; Okubo, T.; Azuma, S.; Kuwamura, M.; Takai, N.; Osada, Y.; Kunihiro, Y.; Mashimo, T.; et al. Generation of knockout rabbits with X-linked severe combined immunodeficiency (X-SCID) using CRISPR/Cas9. Sci. Rep. 2020, 10, 9957. [Google Scholar] [CrossRef]
- Lang, C.N.; Koren, G.; Odening, K.E. Transgenic rabbit models to investigate the cardiac ion channel disease long QT syndrome. Prog. Biophys. Mol. Biol. 2016, 121, 142–156. [Google Scholar] [CrossRef]
- Lombardi, R.; Rodriguez, G.; Chen, S.N.; Ripplinger, C.M.; Li, W.; Chen, J.; Willerson, J.T.; Betocchi, S.; Wickline, S.A.; Efimov, I.R.; et al. Resolution of established cardiac hypertrophy and fibrosis and prevention of systolic dysfunction in a transgenic rabbit model of human cardiomyopathy through thiol-sensitive mechanisms. Circulation 2009, 119, 1398–1407. [Google Scholar] [CrossRef]
- Biermann, J.; Wu, K.; Odening, K.E.; Asbach, S.; Koren, G.; Peng, X.; Zehender, M.; Bode, C.; Brunner, M. Nicorandil normalizes prolonged repolarisation in the first transgenic rabbit model with long-QT syndrome 1 both in vitro and in vivo. Eur. J. Pharmacol. 2011, 650, 309–316. [Google Scholar] [CrossRef]
- Shan, J.; Xie, W.; Betzenhauser, M.; Reiken, S.; Chen, B.-X.; Wronska, A.; Marks, A.R. Calcium leak through ryanodine receptors leads to atrial fibrillation in three mouse models of catecholaminergic polymorphic ventricular tachycardia. Circ. Res. 2012, 111, 708–717. [Google Scholar] [CrossRef] [PubMed]
- Blackwell, D.J.; Faggioni, M.; Wleklinski, M.J.; Gomez-Hurtado, N.; Venkataraman, R.; Gibbs, C.E.; Baudenbacher, F.J.; Gong, S.; Fishman, G.I.; Boyle, P.M.; et al. The Purkinje–myocardial junction is the anatomic origin of ventricular arrhythmia in CPVT. JCI Insight 2022, 7, e151893. [Google Scholar] [CrossRef] [PubMed]
- Shimizum, W.; Horie, M. Phenotypic manifestations of mutations in genes encoding subunits of cardiac potassium channels. Circ. Res. 2011, 109, 97–109. [Google Scholar] [CrossRef]
- Casimiro, M.C.; Knollmann, B.C.; Ebert, S.N.; Vary, J.C., Jr.; Greene, A.E.; Franz, M.R.; Grinberg, A.; Huang, S.P.; Pfeifer, K. T Targeted disruption of the Kcnq1 gene produces a mouse model of Jervell and Lange–Nielsen Syndrome. Proc. Natl. Acad. Sci. USA 2001, 98, 2526–2531. [Google Scholar] [CrossRef]
- Wan, E.; Abrams, J.; Weinberg, R.L.; Katchman, A.N.; Bayne, J.; Zakharov, S.I.; Yang, L.; Morrow, J.P.; Garan, H.; Marx, S.O. Aberrant sodium influx causes cardiomyopathy and atrial fibrillation in mice. J. Clin. Investig. 2016, 126, 112–122. [Google Scholar] [CrossRef]
- Temple, J.; Frias, P.; Rottman, J.; Yang, T.; Wu, Y.; Verheijck, E.E.; Zhang, W.; Siprachanh, C.; Kanki, H.; Atkinson, J.B.; et al. Atrial fibrillation in KCNE1-null mice. Circ. Res. 2005, 97, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Leoni, A.L.; Gavillet, B.; Rougier, J.S.; Marionneau, C.; Probst, V.; Le Scouarnec, S.; Schott, J.J.; Demolombe, S.; Bruneval, P.; Huang, C.L.; et al. Variable Nav1.5 protein expression from the wild-type allele correlates with the penetrance of cardiac conduction disease in the Scn5a +/− mouse model. PLoS ONE 2010, 5, e9298. [Google Scholar] [CrossRef]
- Sugihara, H.; Kimura, K.; Yamanouchi, K.; Teramoto, N.; Okano, T.; Daimon, M.; Morita, H.; Takenaka, K.; Shiga, T.; Tanihata, J.; et al. Age-dependent echocardiographic and pathologic findings in a rat model with Duchenne muscular dystrophy generated by CRISPR/Cas9 genome editing. Int. Heart J. 2020, 61, 1279–1284. [Google Scholar] [CrossRef]
- Ponzoni, M.; Coles, J.G.; Maynes, J.T. Rodent models of dilated cardiomyopathy and heart failure for translational investigations and therapeutic discovery. Int. J. Mol. Sci. 2023, 24, 3162. [Google Scholar] [CrossRef]
- Ruppert, T.; Heckmann, M.B.; Rapti, K.; Schultheis, D.; Jungmann, A.; Katus, H.A.; Winter, L.; Frey, N.; Clemen, C.S.; Schröder, R.; et al. AAV-mediated cardiac gene transfer of wild-type desmin in mouse models for recessive desminopathies. Gene Ther. 2019, 27, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Caravia, X.M.; Ramirez-Martinez, A.; Gan, P.; Wang, F.; McAnally, J.R.; Xu, L.; Bassel-Duby, R.; Liu, N.; Olson, E.N. Loss of function of the nuclear envelope protein LEMD2 causes DNA damage-dependent cardiomyopathy. J. Clin. Investig. 2022, 132, e158897. [Google Scholar] [CrossRef]
- Santini, L.; Palandri, C.; Nediani, C.; Cerbai, E.; Coppini, R. Modelling genetic diseases for drug development: Hypertrophic cardiomyopathy. Pharmacol. Res. 2020, 160, 105176. [Google Scholar] [CrossRef] [PubMed]
- Geisterfer-Lowrance, A.A.; Christe, M.; Conner, D.A.; Ingwall, J.S.; Schoen, F.J.; Seidman, C.E.; Seidman, J.G. A mouse model of familial hypertrophic cardiomyopathy. Science 1996, 272, 731–734. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Sanbe, A.; Osinska, H.; Hewett, T.E.; Klevitsky, R.; Robbins, J. A mouse model of myosin binding protein C human familial hypertrophic cardiomyopathy. J. Clin. Investig. 1998, 102, 1292–1300. [Google Scholar] [CrossRef]
- Yang, Q.; Sanbe, A.; Osinska, H.; Hewett, T.E.; Klevitsky, R.; Robbins, J. In vivo modeling of myosin binding protein C familial hypertrophic cardiomyopathy. Circ Res. 1999, 85, 841–847. [Google Scholar] [CrossRef]
- Mogensen, J.; Kubo, T.; Duque, M.; Uribe, W.; Shaw, A.; Murphy, R.; Gimeno, J.R.; Elliott, P.; McKenna, W.J. Idiopathic restrictive cardiomyopathy is part of the clinical expression of cardiac troponin I mutations. J. Clin. Investig. 2003, 111, 209–216. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, L.; Pacciulli, D.; Zhao, J.; Nan, C.; Shen, W.; Quan, J.; Tian, J.; Huang, X. Restrictive cardiomyopathy caused by troponin mutations: Application of disease animal models in translational studies. Front. Physiol. 2016, 7, 629. [Google Scholar] [CrossRef]
- Yumoto, F.; Lu, Q.W.; Morimoto, S.; Tanaka, H.; Kono, N.; Nagata, K.; Ojima, T.; Takahashi-Yanaga, F.; Miwa, Y.; Sasaguri, T.; et al. Drastic Ca2+ sensitization of myofilament associated with a small structural change in troponin I in inherited restrictive cardiomyopathy. Biochem. Biophys. Res. Commun. 2005, 338, 1519–1526. [Google Scholar] [CrossRef]
- von Scheidt, M.; Zhao, Y.; Kurt, Z.; Pan, C.; Zeng, L.; Yang, X.; Schunkert, H.; Lusis, A.J. Applications and limitations of mouse models for understanding human atherosclerosis. Cell Metab. 2017, 25, 248–261. [Google Scholar] [CrossRef]
- Plump, A.S.; Smith, J.D.; Hayek, T.; Aalto-Setälä, K.; Walsh, A.; Verstuyft, J.G.; Rubin, E.M.; Breslow, J.L. Severe hypercholesterolemia and atherosclerosis in apolipoprotein E-deficient mice created by homologous recombination in ES cells. Cell 1992, 71, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.H.; Reddick, R.L.; Piedrahita, J.A.; Maeda, N. Spontaneous hypercholesterolemia and arterial lesions in mice lacking apolipoprotein E. Science 1992, 258, 468–471. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, S.; Goldstein, J.L.; Brown, M.S.; Herz, J.; Burns, D.K. Massive xanthomatosis and atherosclerosis in cholesterol-fed low density lipoprotein receptor-negative mice. J. Clin. Investig. 1994, 93, 1885–1893. [Google Scholar] [CrossRef] [PubMed]
- Westerterp, M.; van der Hoogt, C.C.; de Haan, W.; Offerman, E.H.; Dallinga-Thie, G.M.; Jukema, J.W.; Havekes, L.M.; Rensen, P.C. Cholesteryl ester transfer protein decreases high-density lipoprotein and severely aggravates atherosclerosis in APOE*3-Leiden mice. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 2552–2559. [Google Scholar] [CrossRef]
- Goettsch, C.; Hutcheson, J.D.; Hagita, S.; Rogers, M.A.; Creager, M.D.; Pham, T.; Choi, J.; Mlynarchik, A.K.; Pieper, B.; Kjolby, M.; et al. A single injection of gain-of-function mutant PCSK9 adeno-associated virus vector induces cardiovascular calcification in mice with no genetic modification. Atherosclerosis 2016, 251, 109–118. [Google Scholar] [CrossRef]
- Zhang, S.; Picard, M.H.; Vasile, E.; Zhu, Y.; Raffai, R.L.; Weisgraber, K.H.; Krieger, M. Diet-induced occlusive coronary atherosclerosis, myocardial infarction, cardiac dysfunction, and premature death in scavenger receptor class B type I-deficient, hypomorphic apolipoprotein ER61 mice. Circulation 2005, 111, 3457–3464. [Google Scholar] [CrossRef]
- Fan, J.; Chen, Y.; Yan, H.; Niimi, M.; Wang, Y.; Liang, J. Principles and applications of rabbit models for atherosclerosis research. J. Atheroscler. Thromb. 2018, 25, 213–220. [Google Scholar] [CrossRef]
- Zhao, Y.; Qu, H.; Wang, Y.; Xiao, W.; Zhang, Y.; Shi, D. Small rodent models of atherosclerosis. Biomed. Pharmacother. 2020, 129, 110426. [Google Scholar] [CrossRef]
- Wu, Y.; Xu, M.J.; Cao, Z.; Yang, C.; Wang, J.; Wang, B.; Liu, J.; Wang, Y.; Xian, X.; Zhang, F.; et al. Heterozygous Ldlr-deficient hamster as a model to evaluate the efficacy of PCSK9 antibody in hyperlipidemia and atherosclerosis. Int. J. Mol. Sci. 2019, 20, 5936. [Google Scholar] [CrossRef]
- Guyard-Dangremont, V.; Desrumaux, C.; Gambert, P.; Lallemant, C.; Lagrost, L. Phospholipid and cholesteryl ester transfer activities in plasma from 14 vertebrate species. Relation to atherogenesis susceptibility. Comp. Biochem. Physiol. B Biochem. Mol. Biol. 1998, 120, 517–525. [Google Scholar] [CrossRef]
- Xiangdong, L.; Yuanwu, L.; Hua, Z.; Liming, R.; Qiuyan, L.; Ning, L. Animal models for the atherosclerosis research: A review. Protein Cell 2011, 2, 189–201. [Google Scholar] [CrossRef]
- Wilkins, B.J.; Dai, Y.S.; Bueno, O.F.; Parsons, S.A.; Xu, J.; Plank, D.M.; Jones, F.; Kimball, T.R.; Molkentin, J.D. Calcineurin/NFAT coupling participates in pathological, but not physiological, cardiac hypertrophy. Circ. Res. 2004, 94, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Condorelli, G.; Drusco, A.; Stassi, G.; Bellacosa, A.; Roncarati, R.; Iaccarino, G.; Russo, M.A.; Gu, Y.; Dalton, N.; Chung, C.; et al. Akt induces enhanced myocardial contractility and cell size in vivo in transgenic mice. Proc. Natl. Acad. Sci. USA 2002, 99, 12333–12338. [Google Scholar] [CrossRef]
- Toepfer, C.N.; Wakimoto, H.; Garfinkel, A.C.; McDonough, B.; Liao, D.; Jiang, J.; Tai, A.C.; Gorham, J.M.; Lunde, I.G.; Lun, M.; et al. Hypertrophic cardiomyopathy mutations in MYBPC3 dysregulate myosin. Sci. Transl. Med. 2019, 11, eaat1199. [Google Scholar] [CrossRef]
- Kazmierczak, K.; Yuan, C.-C.; Liang, J.; Huang, W.; Rojas, A.I.; Szczesna-Cordary, D. Remodeling of the heart in hypertrophy in animal models with myosin essential light chain mutations. Front. Physiol. 2014, 5, 353. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Yan, X.; Feng, X.; Manning, W.J.; Dillmann, W.H.; Lorell, B.H. Transgenic expression of sarcoplasmic reticulum Ca(2+) atpase modifies the transition from hypertrophy to early heart failure. Circ. Res. 2001, 89, 422–429. [Google Scholar] [CrossRef]
- van der Velden, J.; Asselbergs, F.W.; Bakkers, J.; Batkai, S.; Bertrand, L.; Bezzina, C.R.; Bot, I.; Brundel, B.J.J.M.; Carrier, L.; Chamuleau, S.; et al. Animal models and animal-free innovations for cardiovascular research: Current status and routes to be explored. Consensus document of the ESC working group on myocardial function and the ESC working group on cellular biology of the heart. Cardiovasc. Res. 2002, 118, 3016–3051. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Landstrom, A.P.; Shah, S.H.; Wu, J.C.; Seidman, C.E.; American Heart Association. Gene therapy in cardiovascular disease: Recent advances and future directions in science: A science advisory from the American Heart Association. Circulation 2024, 150, e471–e480. [Google Scholar] [CrossRef]
- Oláh, A.; Ruppert, M.; Orbán, T.I.; Apáti, Á.; Sarkadi, B.; Merkely, B.; Radovits, T. Hemodynamic characterization of a transgenic rat strain stably expressing the calcium sensor protein GCaMP2. Am. J. Physiol.-Heart Circ. Physiol. 2019, 316, H1224–H1228. [Google Scholar] [CrossRef]
- Santin, Y.; Sicard, P.; Vigneron, F.; Guilbeau-Frugier, C.; Dutaur, M.; Lairez, O.; Couderc, B.; Manni, D.; Korolchuk, V.I.; Lezoualc’h, F.; et al. Oxidative stress by monoamine oxidase-A impairs transcription factor EB activation and autophagosome clearance, leading to cardiomyocyte necrosis and heart failure. Antioxid. Redox Signal. 2016, 25, 10–27. [Google Scholar] [CrossRef]
- Szebényi, K.; Füredi, A.; Kolacsek, O.; Pergel, E.; Bősze, Z.; Bender, B.; Vajdovich, P.; Tóvári, J.; Homolya, L.; Szakács, G.; et al. Generation of a homozygous transgenic rat strain stably expressing a calcium sensor protein for direct examination of calcium signaling. Sci. Rep. 2015, 5, 12645. [Google Scholar] [CrossRef]
- Bass-Stringer, S.; Tai, C.M.K.; McMullen, J.R. IGF1–PI3K-induced physiological cardiac hypertrophy: Implications for new heart failure therapies, biomarkers, and predicting cardiotoxicity. J. Sport Health Sci. 2021, 10, 637–647. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Li, C.; Elnwasany, A.; Sharma, G.; An, Y.A.; Zhang, G.; Elhelaly, W.M.; Lin, J.; Gong, Y.; Chen, G.; et al. PKM1 exerts critical roles in cardiac remodeling under pressure overload in the heart. Circulation 2021, 144, 712–727. [Google Scholar] [CrossRef]
- Sukumaran, A.; Sadayappan, S. Optimization of tamoxifen-induced gene regulation in cardiovascular research. J. Cardiovasc. Aging 2022, 2, 21. [Google Scholar] [CrossRef] [PubMed]
- Rouhi, L.; Fan, S.; Cheedipudi, S.M.; Olcum, M.; Jeong, H.H.; Zhao, Z.; Gurha, P.; Marian, A.J. Effects of tamoxifen inducible MerCreMer on gene expression in cardiac myocytes in mice. J. Cardiovasc. Aging 2022, 2, 8. [Google Scholar] [CrossRef]
- Rashbrook, V.S.; Brash, J.T.; Ruhrberg, C. Cre toxicity in mouse models of cardiovascular physiology and disease. Nat. Cardiovasc. Res. 2022, 1, 806–816. [Google Scholar] [CrossRef] [PubMed]
- Iwatate, M.; Gu, Y.; Dieterle, T.; Iwanaga, Y.; Peterson, K.L.; Hoshijima, M.; Chien, K.R.; Ross, J. In vivo high-efficiency transcoronary gene delivery and Cre–LoxP gene switching in the adult mouse heart. Gene Ther. 2003, 10, 1814–1820. [Google Scholar] [CrossRef][Green Version]
- Zengel, J.; Wang, Y.X.; Seo, J.W.; Ning, K.; Hamilton, J.N.; Wu, B.; Raie, M.; Holbrook, C.; Su, S.; Clements, D.R.; et al. Hardwiring tissue-specific AAV transduction in mice through engineered receptor expression. Nat. Methods 2023, 20, 1070–1081. [Google Scholar] [CrossRef]
- Park, C.S.; Cha, H.; Kwon, E.J.; Jeong, D.; Hajjar, R.J.; Kranias, E.G.; Cho, C.; Park, W.J.; Kim, D.H. AAV-Mediated knock-down of HRC exacerbates transverse aorta constriction-induced heart failure. PLoS ONE 2012, 7, e43282. [Google Scholar] [CrossRef]
- Doisne, N.; Grauso, M.; Mougenot, N.; Clergue, M.; Souil, C.; Coulombe, A.; Guicheney, P.; Neyroud, N. In vivo dominant-negative effect of an SCN5A Brugada syndrome variant. Front Physiol. 2021, 12, 661413. [Google Scholar] [CrossRef]
- Pak, V.V.; Ezeriņa, D.; Lyublinskaya, O.G.; Pedre, B.; Tyurin-Kuzmin, P.A.; Mishina, N.M.; Thauvin, M.; Young, D.; Wahni, K.; Martínez Gache, S.A.; et al. Ultrasensitive genetically encoded indicator for hydrogen peroxide identifies roles for the oxidant in cell migration and mitochondrial function. Cell Metab. 2020, 31, 642–653.e6. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Spyropoulos, F.; Michel, T. FRBM Mini REVIEW: Chemogenetic approaches to probe redox dysregulation in heart failure. Free Radic. Biol. Med. 2024, 217, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Steinhorn, B.; Sorrentino, A.; Badole, S.; Bogdanova, Y.; Belousov, V.; Michel, T. Chemogenetic generation of hydrogen peroxide in the heart induces severe cardiac dysfunction. Nat. Commun. 2018, 9, 4044. [Google Scholar] [CrossRef]
- Sorrentino, A.; Steinhorn, B.; Troncone, L.; Saravi, S.S.S.; Badole, S.; Eroglu, E.; Kijewski, M.F.; Divakaran, S.; Di Carli, M.; Michel, T. Reversal of heart failure in a chemogenetic model of persistent cardiac redox stress. Am. J. Physiol. Heart Circ. Physiol. 2019, 317, H617–H626. [Google Scholar] [CrossRef]
- Jaski, B.E.; Jessup, M.L.; Mancini, D.M.; Cappola, T.P.; Pauly, D.F.; Greenberg, B.; Borow, K.; Dittrich, H.; Zsebo, K.M.; Hajjar, R.J. Calcium upregulation by percutaneous administration of gene therapy in cardiac disease (CUPID Trial), a first-in-human phase 1/2 clinical trial. J. Card. Fail. 2009, 15, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Ambrosi, C.M.; Sadananda, G.; Han, J.L.; Entcheva, E. Adeno-associated virus mediated gene delivery: Implications for scalable in vitro and in vivo cardiac optogenetic models. Front. Physiol. 2019, 10, 168. [Google Scholar] [CrossRef]
- Fang, H.; Lai, N.C.; Gao, M.H.; Miyanohara, A.; Roth, D.M.; Tang, T.; Hammond, H.K. Comparison of adeno-associated virus serotypes and delivery methods for cardiac gene transfer. Hum. Gene Ther. Methods 2012, 23, 234–241. [Google Scholar] [CrossRef]
- Schröder, L.C.; Frank, D.; Müller, O.J. Transcriptional targeting approaches in cardiac gene transfer using AAV vectors. Pathogens 2023, 12, 1301. [Google Scholar] [CrossRef]
- Prasad, K.-M.R.; Xu, Y.; Yang, Z.; Acton, S.T.; French, B.A. Robust cardiomyocyte-specific gene expression following systemic injection of AAV: In vivo gene delivery follows a poisson distribution. Gene Ther. 2011, 18, 43–52. [Google Scholar] [CrossRef]
- Zincarelli, C.; Soltys, S.; Rengo, G.; Rabinowitz, J.E. Analysis of AAV serotypes 1-9 mediated gene expression and tropism in mice after systemic injection. Mol. Ther. 2008, 16, 1073–1080. [Google Scholar] [CrossRef]
- Rode, L.; Bär, C.; Groß, S.; Rossi, A.; Meumann, N.; Viereck, J.; Abbas, N.; Xiao, K.; Riedel, I.; Gietz, A.; et al. AAV capsid engineering identified two novel variants with improved in vivo tropism for cardiomyocytes. Mol. Ther. 2022, 30, 3601–3618. [Google Scholar] [CrossRef] [PubMed]


| Model | Genetic Basis/Modification | Main Cardiovascular Phenotype | Key Applications | Major Advantages | Main Limitations | Physiological Relevance | Genetic Manipulability | Reproducibility | Translational Relevance |
|---|---|---|---|---|---|---|---|---|---|
| SHR Rat | Polygenic (overexpression of the renin gene) | Essential hypertension, stroke-prone | Essential hypertension, cerebral circulatory disorders | Closely mimics human essential hypertension | Limited to neurogenic hypertension | High | Moderate | High | Moderate-High |
| SHR-SP Rat | Polygenic (derived from SHR) | Severe hypertension, stroke susceptibility | Stroke research | Reproducible stroke phenotype | Limited lifespan | High | Moderate | High | High |
| DSS Rat | Polygenic (CYP11B1) | Salt-sensitive hypertension | Sodium-related hypertension | Gene-environment interaction modeling | No human-like nephropathy | Moderate | Low | High | Moderate |
| FHH Rat | Polygenic (Add3, Rbm20, Shoc2) | Hypertensive nephropathy | Renal hypertension | Renal-cardiovascular crosstalk | Unclear primary pathology | Moderate | Low | Moderate | Moderate |
| MHS Rat | ADD1 mutation (α-adducin defect) | Primary hypertension with renal dysfunction | Hypertension with kidney involvement | Links hypertension to kidney pathology | Limited non-renal applications | Moderate | Low | High | Moderate |
| Milan Hypertensive Rat | Polygenic (α-adducin mutations) | Essential hypertension | Membrane transport studies | Well-characterized genetic basis | Limited availability | Moderate | Low | High | Moderate |
| Lyon Hypertensive Rat | Polygenic (Ercc6l2) | Metabolic syndrome, salt-sensitive hypertension | Insulin resistance studies | Human metabolic syndrome mimic | Complex genetic architecture | Moderate | Low | Moderate | Low |
| NZGH Rat | Polygenic selection | Spontaneous hypertension | Hypertension mechanisms | Stable phenotype | Low genetic tractability | Moderate | Low | High | Moderate |
| MWF Rat | Spontaneous renal dysfunction | Hypertension with proteinuria | Renal hypertension | Kidney-heart axis modeling | Slow progression | Moderate | Low | Moderate | Low |
| Sabra Hypertensive Rat | α2-Adrenoceptor variants | Salt-sensitive hypertension | Environmental hypertension | Human salt sensitivity reproduction | Limited genetic tools | Moderate | Low | High | Moderate |
| Buffalo Rat | Polygenic | Hypertension with insulin resistance | Metabolic hypertension | Metabolic-cardiovascular interactions | Complex phenotype | Moderate | Low | Moderate | Moderate |
| Goto-Kakizaki Rat | Polygenic | Diabetic cardiomyopathy | Diabetes-related CVD | Non-obese diabetes model | Mild cardiac phenotype | Moderate | Low | High | Moderate |
| WHHL Rabbit | LDLR mutation | Familial hypercholesterolemia | Atherosclerosis studies | Spontaneous human-like plaques | High cost, limited tools | High | Moderate | High | High |
| Ldlr−/− Mouse | LDLR knockout | Hypercholesterolemia | Plaque biology research | Rapid disease progression | Species-specific plaque differences | Moderate | High | High | Moderate |
| ApoE−/− Mouse | ApoE knockout | Severe atherosclerosis | Plaque development studies | Widely used model | Plaque composition differences | Moderate | High | High | Moderate |
| cMyBP-C KO Mouse | MYBPC3 deletion | Hypertrophic cardiomyopathy | Sarcomere dysfunction | Human mutation similarity | Mouse-specific physiology | Moderate | High | High | Moderate |
| Feline HCM Model | MYBPC3 mutation (natural) | Hypertrophic cardiomyopathy | Spontaneous HCM studies | Naturally occurring HCM | Limited genetic manipulation | High | Low | Moderate | High |
| Canine ARVC Model | PKP2 mutation (boxers) | Arrhythmogenic right ventricular cardiomyopathy | ARVC mechanisms, sudden cardiac death | Naturally mimics human ARVC | Ethical and cost challenges | High | Low | Moderate | High |
| Zebrafish (Tnnt2 KO) | Tnnt2 knockout | Cardiomyopathy | Cardiac development | High-throughput screening | Simplified cardiac structure | Low-Moderate | High | High | Low |
| CPVT Mouse | RYR2 mutation | Polymorphic VT | Arrhythmia mechanisms | Human CPVT recapitulation | Stress-dependent phenotype | Moderate | High | High | Moderate |
| LQTS Mouse | KCNQ1/KCNH2 KO | Long QT syndrome | Ion channel studies | Direct human mutation link | ECG differences | Moderate | High | High | Moderate |
| AAV9-MYH7 Mouse | AAV9-mediated MYH7 mutation | Hypertrophic cardiomyopathy | Gene therapy testing | Tissue-specific targeting | Transient expression | Moderate | High | Moderate | High |
| DREADD Rat | Chemogenetic hM3Dq receptor expression | Heart failure modulation | Neural regulation of cardiac function | Precise control of signaling pathways | Requires ligand administration | Moderate | High | High | Moderate |
| Animal Model | Advantages | Drawbacks |
|---|---|---|
| Danio rerio (zebrafish) | Short developmental period, low-cost maintenance | Two-chamber heart, which do not reproduce all processes typical for humans |
| Mus musculus (house mouse) | Short developmental period, low-cost maintenance | Small-size heart, high heartbeat rate |
| Rabbit | Short developmental period, high efficacy of gene modifications | Moderate maintenance costs |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blagonravov, M.; Ryabinina, A.; Karpov, R.; Ovechkina, V.; Filatov, M.; Silaeva, Y.; Syatkin, S.; Agostinelli, E.; Belousov, V.; Mozhaev, A. Genetic Animal Models of Cardiovascular Pathologies. Biomedicines 2025, 13, 1518. https://doi.org/10.3390/biomedicines13071518
Blagonravov M, Ryabinina A, Karpov R, Ovechkina V, Filatov M, Silaeva Y, Syatkin S, Agostinelli E, Belousov V, Mozhaev A. Genetic Animal Models of Cardiovascular Pathologies. Biomedicines. 2025; 13(7):1518. https://doi.org/10.3390/biomedicines13071518
Chicago/Turabian StyleBlagonravov, Mikhail, Anna Ryabinina, Ruslan Karpov, Vera Ovechkina, Maxim Filatov, Yulia Silaeva, Sergei Syatkin, Enzo Agostinelli, Vsevolod Belousov, and Andrey Mozhaev. 2025. "Genetic Animal Models of Cardiovascular Pathologies" Biomedicines 13, no. 7: 1518. https://doi.org/10.3390/biomedicines13071518
APA StyleBlagonravov, M., Ryabinina, A., Karpov, R., Ovechkina, V., Filatov, M., Silaeva, Y., Syatkin, S., Agostinelli, E., Belousov, V., & Mozhaev, A. (2025). Genetic Animal Models of Cardiovascular Pathologies. Biomedicines, 13(7), 1518. https://doi.org/10.3390/biomedicines13071518








