1. Introduction
Alzheimer’s disease (AD) is the most common cause of dementia, currently affecting over 55 million individuals worldwide, a figure expected to triple by 2050 as global populations age [
1]. Despite recent advances in diagnostic imaging and targeted therapies, there is still no curative treatment, and symptomatic management continues to be the standard of care. As such, there is a crucial public health need to focus on the identification and modification of risk factors that may delay or even prevent the onset of Alzheimer’s disease.
Approximately 40% of dementia cases have the potential to be prevented through better control of risk factors including hypertension (HTN), obesity, diabetes, depression, smoking, and low educational attainment [
2]. Among these, obesity and hypertension are of particular interest due to their role in promoting vascular dysfunction, systemic inflammation, and metabolic impairment, which have been increasingly recognized as a major contributor to cognitive deterioration [
3,
4]. As such, identifying controllable risk factors, such as HTN and obesity, has become a public health priority for delaying or preventing disease onset [
2]. Previous studies have demonstrated that HTN is significantly associated with an increased risk of AD [
5,
6]. Mechanistically, elevated blood pressure may cause damage to the blood–brain barrier, promote cerebral microinfarcts, and induce white matter lesions which can collectively accelerate neurodegeneration [
3,
7]. Moreover, HTN may further compound cognitive risk due to its often co-occurrence with other metabolic comorbidities [
3,
5].
Obesity has emerged as a risk factor for dementia and cognitive impairment. In large population studies, obesity has been associated with an increased risk of late-life AD [
8,
9,
10], mediated through mechanisms including chronic low-grade inflammation, insulin resistance, altered lipid metabolism, and adipokine dysregulation, all of which may promote the accumulation of amyloid plaques and accelerate neurodegenerative processes [
11,
12]. More importantly, HTN and obesity often coexist, creating complex metabolic syndromes. Specifically, studies have suggested that HTN, when combined with obesity may amplify the risk of cognitive dysfunction to a greater extent than either condition independently [
13,
14]. However, few studies have specifically focused on assessing whether comorbid obesity confers additional risk for AD development in hypertensive populations.
Socioeconomic factors, like the deprivation index, have been increasingly recognized as social determinants that influence cognitive health outcomes. The Area Deprivation Index (ADI) has shown the potential link between disadvantaged neighborhoods and poorer cognitive function, which aligns with previous smaller studies [
15]. Furthermore, higher ADI scores, indicating greater deprivation levels, have been found to be associated with increased AD neuropathology and cognitive decline [
16].
In this study, we leveraged the All of Us (AoU) Research Program, a large, nationally representative database, to extract a large electronic health record (EHR)-derived cohort of individuals with hypertension in order to evaluate the association between obesity and AD incidence within a hypertensive population. Using this resource, we identified relevant clinical variables. Refinements in dementia risk predictions have been made possible by advancements in genomic profiling. Genome-wide association studies (GWASs) created new opportunities to identify multiple loci implicated in AD. We integrated clinical predictors to assess their contribution to AD risk and compared AD-associated SNVs in the HTN cohort to those reported in the existing literature on the general population. By focusing our study on the hypertensive population, our study contributes new insights into aspects of AD pathogenesis that are not well understood and underscores the connection between metabolic health and AD development.
2. Materials and Methods
2.1. Data Extraction
Patient electronic health records (EHRs) were obtained from the All of Us (AoU) Controlled Tier Dataset v8. The data was filtered and compiled within the AoU dataset workspace. Dataframes containing patient information were downloaded using Python (v3.10.16) in the AoU workbench.
2.2. Data Preparation
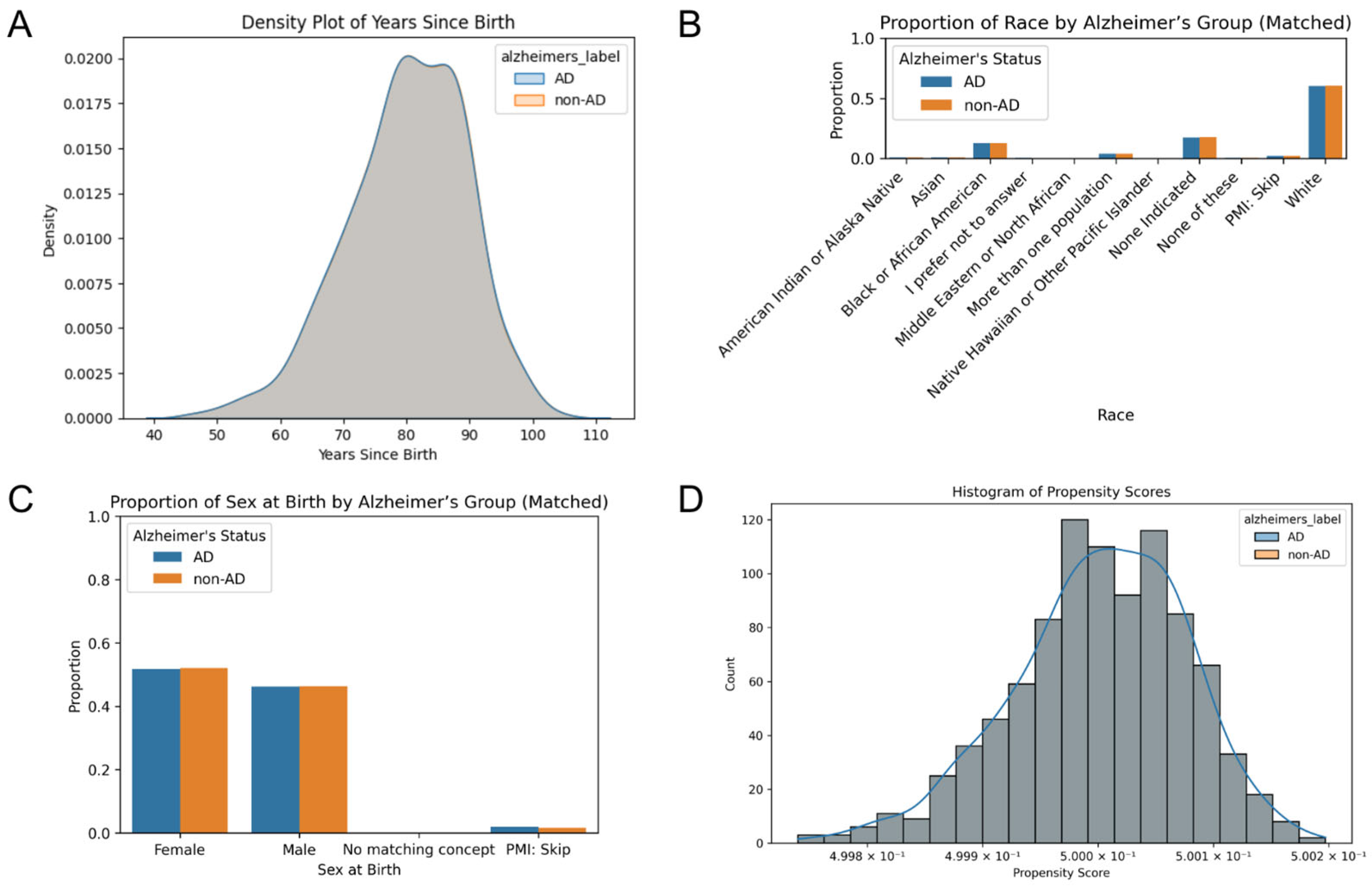
Patient dataframes were merged and filtered to include only patients older than 40 years who were diagnosed with HTN and prescribed anti-HTN drugs utilizing Python. Individuals diagnosed with AD before the age of 40 were excluded. Patients with AD were matched to a non-AD patient based on age, race, and sex at birth. This study includes 931 AD patients and 931 non-AD patients. Covariate balance between the matched cohorts was assessed using density plots, histograms, and grouped bar plots to evaluate the effectiveness of matching.
Blood pressure control was defined as an SBP of less than 120 mmHg; an SBP equal to or greater than 120 mmHg was considered uncontrolled. Due to the multiple measurements of SBP for each patient, the average of the measurements taken within a year of taking HTN drugs was utilized as the SBP of an individual. Obesity levels were categorized into four classes based on BMI: Not Obese (<30), Class 1 Obesity (30–34.9), Class 2 Obesity (35–39.9), and Class 3 Obesity (≥40). To maintain consistency, due to multiple BMI measurements, the average of the measurements within a year of taking HTN drugs was used as the BMI of a patient. Implausible BMI measurements were excluded by retaining only those between 10.0 and 60.0.
A dataframe was created for only patients older than 40 years who were not diagnosed with HTN. Patients were matched based on age, race, and sex at birth. The non-HTN cohort includes 222 AD patients and 222 non-AD patients. SBP and BMI were calculated as the average measurement since the age of 40. The remaining risk factors were calculated using the same method for the HTN cohort.
2.3. Statistical Analysis
All analyses were conducted in Python using Pandas (v2.2.3), scikit-learn (v1.3.0), lifelines (v0.30.0), scipy (v1.11.2), matplotlib (v3.7.2), and seaborn (v0.12.2). A Choropleth map was created by utilizing the GeoPandas (v1.0.1) and GeoPlot (v0.5.1) Python libraries to plot the incidence per state in the U.S. The first three digits of patients’ zip codes were utilized to determine the state of AD incidence.
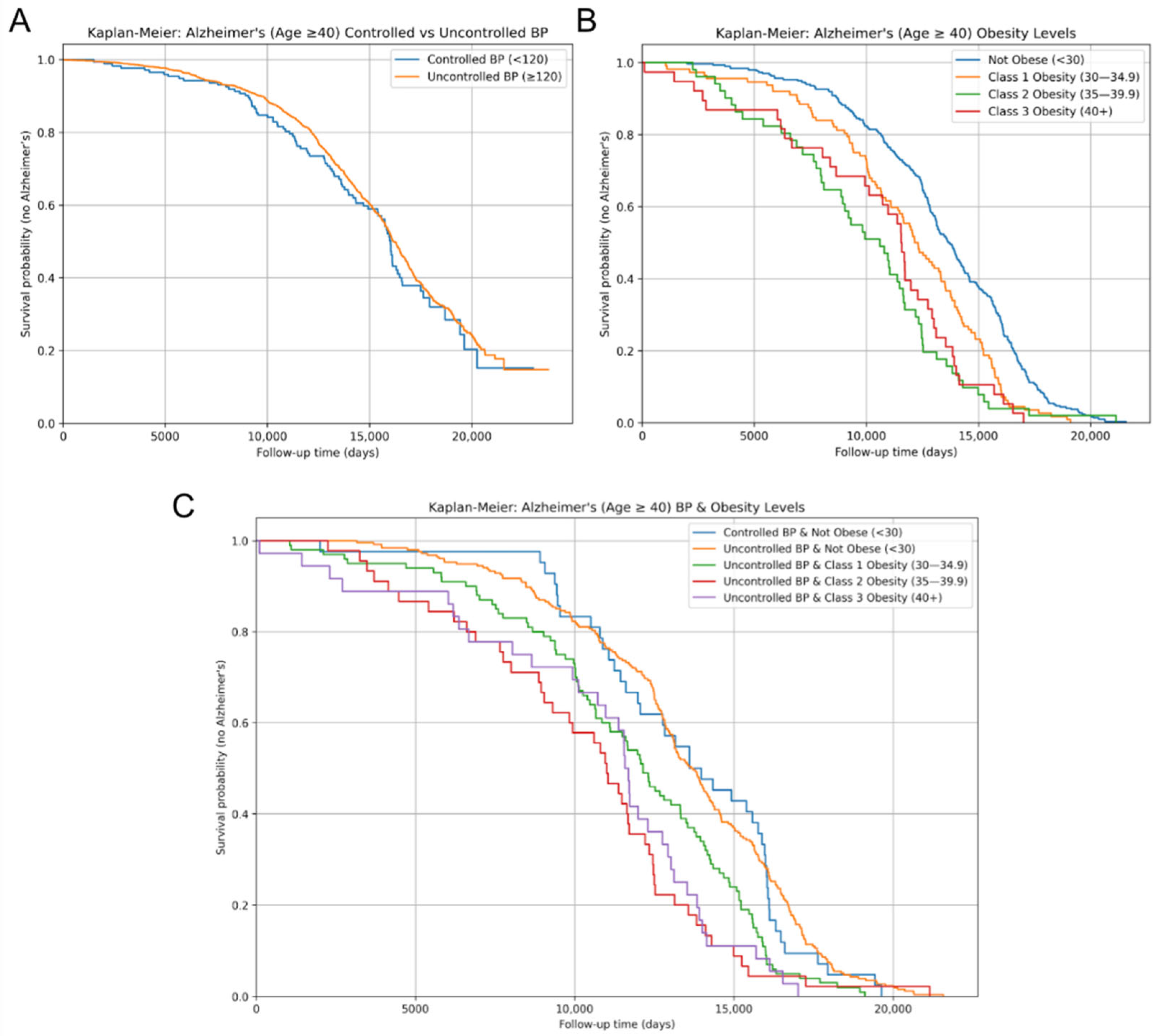
Kaplan–Meier survival curves for AD incidence were determined separately for each of the three cohorts: SBP control, obesity levels, and the combination of SBP control and obesity levels. Comparisons between groups were evaluated using the log-rank test. Patients missing follow-up time or AD status were excluded from all analyses. The follow-up time, measured in days, was the time after the age of 40 to either AD diagnosis or the current date for non-AD patients.
The multivariate Cox proportional hazards regression model was then employed to investigate the effects of several variables on the time to AD diagnosis. Blood pressure control and sex at birth were treated as binary categorical variables; race was one-hot encoded into multiple binary categorical variables, and BMI was categorized as an ordinal variable to track its progression. Hazard ratios (HRs) and the corresponding 95% confidence intervals (CIs) were computed to assess the association between covariates and time to AD diagnosis.
Pairwise comparisons between cohorts were performed. To visualize the significant associations (p < 0.05), forest plots were generated to display the HRs and CIs, with one group designated as the reference. Only cohort comparisons in which both groups had at least 30 individuals were included to reduce the risk of unreliable estimates due to small sample sizes.
Covariate distributions of years since birth, race, and sex at birth were examined across cohorts using density plots and bar plots to assess population differences.
2.4. Genome-Wide Association Study
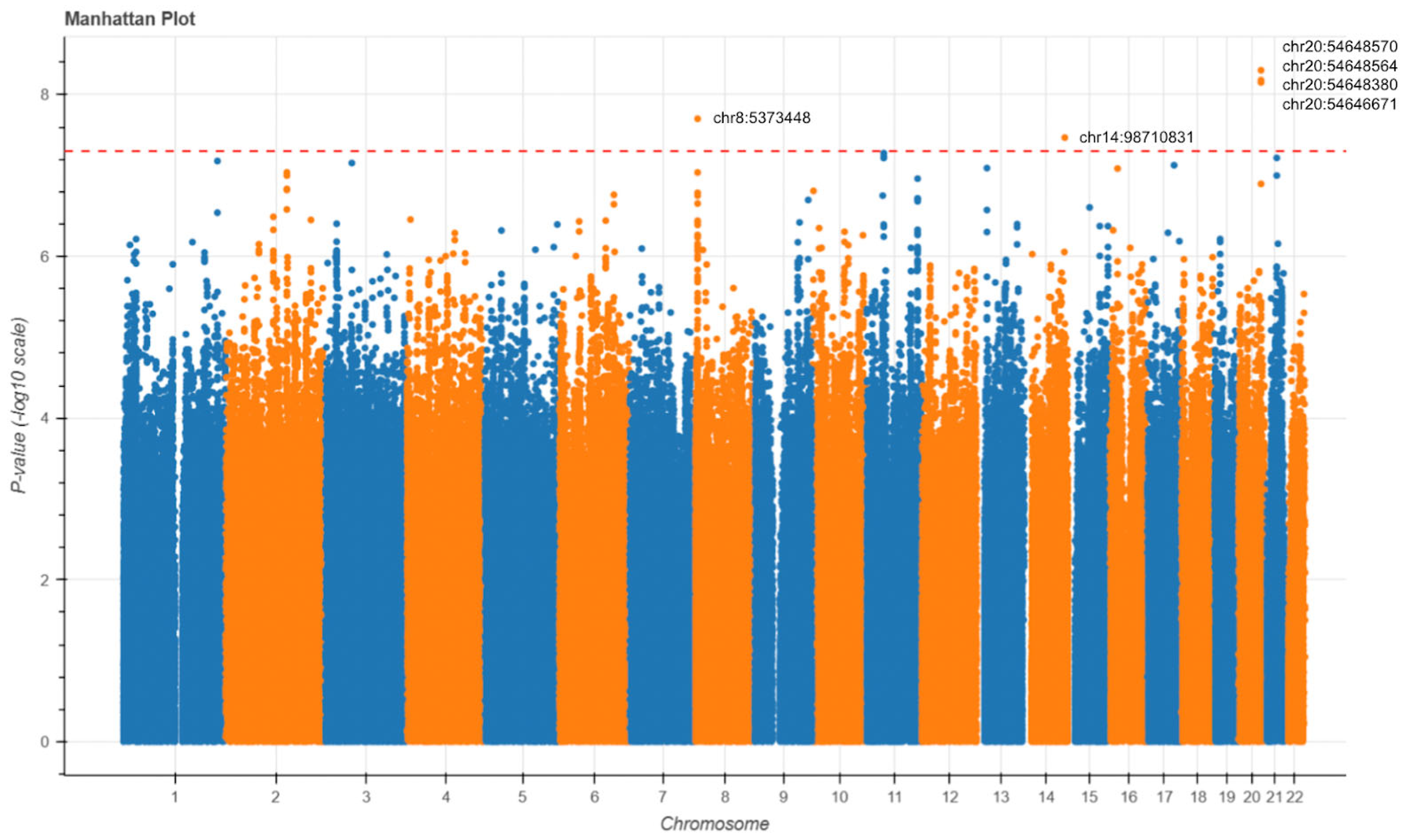
Due to constraints within the All of Us data platform, we were unable to perform matched case–control selection. Therefore, we limited our analysis to individuals with Alzheimer’s disease, comparing those with hypertension to those without. This approach allowed us to leverage available data while controlling for AD status across all individuals. A total of 1030 variant call format (VCF) files of the short-read whole-genome sequencing (WGS) data were downloaded and extracted through the AoU Controlled Tier Dataset v8. These files consisted of 846 AD individuals diagnosed with HTN and 184 HTN-free AD individuals. Genotype data were obtained from the NIH Genomic Data Commons and accessed through the Terra platform. VCF files were processed utilizing Hail (v0.2) on a Google Cloud Dataproc cluster. Only individuals with a diagnosis of Alzheimer’s disease were included. Quality control was performed by removing samples with genotype call rates below 90% or mean genotype quality below 10. Only biallelic SNVs on autosomal chromosomes with call rates above 98%, minor allele frequency (MAF) greater than 1%, and Hardy–Weinberg equilibrium (HWE) p-values above 1 × 10−6 were retained. Genome-wide association testing was performed using logistic regression under an additive genetic model. The binary outcome was hypertension status, and the predictor was the number of alternate alleles at each SNV. Covariates were not included. Genome-wide significance was defined as p < 5 × 10−8.
4. Discussion
In the context of global population aging, addressing the rising incidence of age-related diseases such as Alzheimer’s disease (AD) has become increasingly important. However, AD remains underexplored in hypertensive (HTN) populations, despite both conditions sharing common age-related risk factors and exhibiting similar trends in prevalence [
17]. In addressing this gap of understanding AD, our study provides evidence that obesity and the Area Deprivation Index (ADI) are key predictors of AD risk among individuals within the HTN population. While prior studies have linked HTN, obesity, and the Area Deprivation Index individually to AD risk [
4,
5,
6,
8,
9], our findings underscore the heightened vulnerability conferred by comorbid obesity and differential socioeconomic status within an already hypertensive population. Specifically, greater obesity and higher Area Deprivation Index values (higher levels of socioeconomic disadvantage) consistently displayed strong associations with earlier and more frequent AD diagnoses.
The relationship observed between increasing obesity class and AD incidence aligns with previous population-level studies linking obesity to late-life neurocognitive degeneration [
8,
9,
10]. Our results extend these findings by demonstrating that obesity’s effect remains robust even within a hypertensive population. The interaction between obesity and SBP appears to biologically influence AD onset through a convergence of metabolic and vascular pathways. Central adiposity is associated with structural brain changes including atrophy and white matter degradation, as well as the disruption of blood–brain barrier (BBB) integrity, which is implicated in cognitive decline and increased AD risk. Adipose tissue is now recognized as an active endocrine organ that secretes adipokines, mediating inflammation, insulin resistance, and neurodegenerative processes. These adipokines may directly affect brain function by modulating microglial activation, neuroinflammation, and neuronal insulin signaling. Additionally, chronic obesity often leads to peripheral insulin resistance, which has been closely linked to central (brain) insulin resistance, a hallmark of early AD pathology. Proinflammatory cytokines released in response to amyloid-β accumulation phosphorylate IRS-1 at inhibitory serine residues, impairing insulin signaling and cognitive function. Elevated SBP exacerbates these effects by further compromising cerebrovascular integrity, reducing cerebral perfusion, and accelerating small vessel disease—all of which amplify amyloid deposition and tau pathology. These mechanisms support the observation that individuals with both obesity and hypertension experience a more pronounced relationship between beta-amyloid burden and cognitive decline, as shown in longitudinal neuropsychological studies [
14]. Interestingly, this study reveals no significant association between SBP control alone and AD incidence. This may be due to the complexity of SBP’s temporal impact. Mid-life, rather than late-life SBP is more predictive of AD, or the variability in medication and treatment was not fully captured in our dataset. Individuals taking antihypertensive medications with previous damage due to longstanding hypertension prior to achieving SBP control are another limitation to control the ability of status to accurately reflect cumulative vascular burden. Additionally, this may be due to SBP thresholds that may not capture the full complexity of the range of vascular contributions to AD, especially when considering the variability of blood pressure readings. Furthermore, it is possible that metabolic disturbances associated with obesity exert a more direct or synergistic influence on neurodegeneration than SBP alone.
Furthermore, our findings align with a growing body of the literature suggesting that elevated neighborhood-level deprivation, measured by the Area Deprivation Index, contributes to heightened AD risk through multiple, interconnected pathways. AoU defines ADI as a composite metric based on education, health insurance, housing, income, and poverty. Individuals residing in disadvantaged neighborhoods are disproportionately exposed to adverse social determinants of health, including limited access to quality education, healthcare, nutritious food, and safe housing—all of which are associated with poor cognitive outcomes across the life course [
15]. Notably, Powell et al. demonstrated that living in the most disadvantaged decile was associated with more than twice the odds of AD neuropathology at autopsy after adjusting for age, sex, and year of death [
16]. Overall, these findings underscore the potential of ADI as a policy-relevant, currently overlooked AD risk factor and highlight the importance of incorporating socioeconomic status into disease management for AD.
Our genomic findings further enhance the interpretation of these results. The GWAS identified SNVs near genes such as DOK5, LINC02914, and PXMP2. DOK5 has previously been associated with reduced BMI and protection against obesity in a North Indian population, where specific variants were linked to a lower risk of obesity [
18]. Given the observed association between obesity status and increased risk of AD in our study, these findings suggest that DOK5 may influence AD risk through metabolic pathways. PXMP2, peroxisomal membrane protein 2, was recently found to play a role in peroxisomal lipid metabolism [
19]. LINC02914 has been less studied in the context of lipid metabolism, hypertension, or Alzheimer’s disease pathology, highlighting the need for additional functional studies to map its precise role in human diseases. We observed limited overlap between our GWAS signals and loci previously associated with blood pressure regulation, suggesting that the genetic architecture distinguishing hypertensive from non-hypertensive individuals within the AD population may be minimal. This raises the possibility that the shared pathways linking hypertension and AD are shaped more by environmental, lifestyle, or epigenetic factors than by distinct germline variations—consistent with our finding that the Area Deprivation Index is a significant risk factor for AD [
20].
Contrary to previous studies, we found no statistically significant difference in hazard ratios between males and females after adjusting for age. These findings suggest that previously observed sex differences in AD incidence may be due to differences in life expectancy, with women living longer on average and thus having greater incidences of late-onset AD [
21]. This is consistent with prior research showing that women tend to outlive men in nearly all populations worldwide, which leads to a widening sex gap in the oldest age groups, corresponding to a cohort where the risk of AD increases exponentially. Furthermore, by calculating the hazard ratio, which is time censored, instead of the odds ratio, which is calculated for an arbitrary time period, we obtained the instantaneous risk of developing AD instead of the cumulative risk over time. Given that AD diagnoses approximately double every five years beyond the age of 65, the overrepresentation of women in these oldest age brackets likely inflates female AD incidence statistics. Our results correct the widely held, oversimplified assumption that the female sex is intrinsically associated with greater AD susceptibility. Instead, our data support the interpretation that longevity, rather than sex-specific biology, is the cause of sex disparities in AD risk [
22].