The Application of S-Substituted Pteridine for CCl4-Induced Acute Hepatitis Treatment in Rats
Abstract
1. Introduction
2. Materials and Methods
3. Results
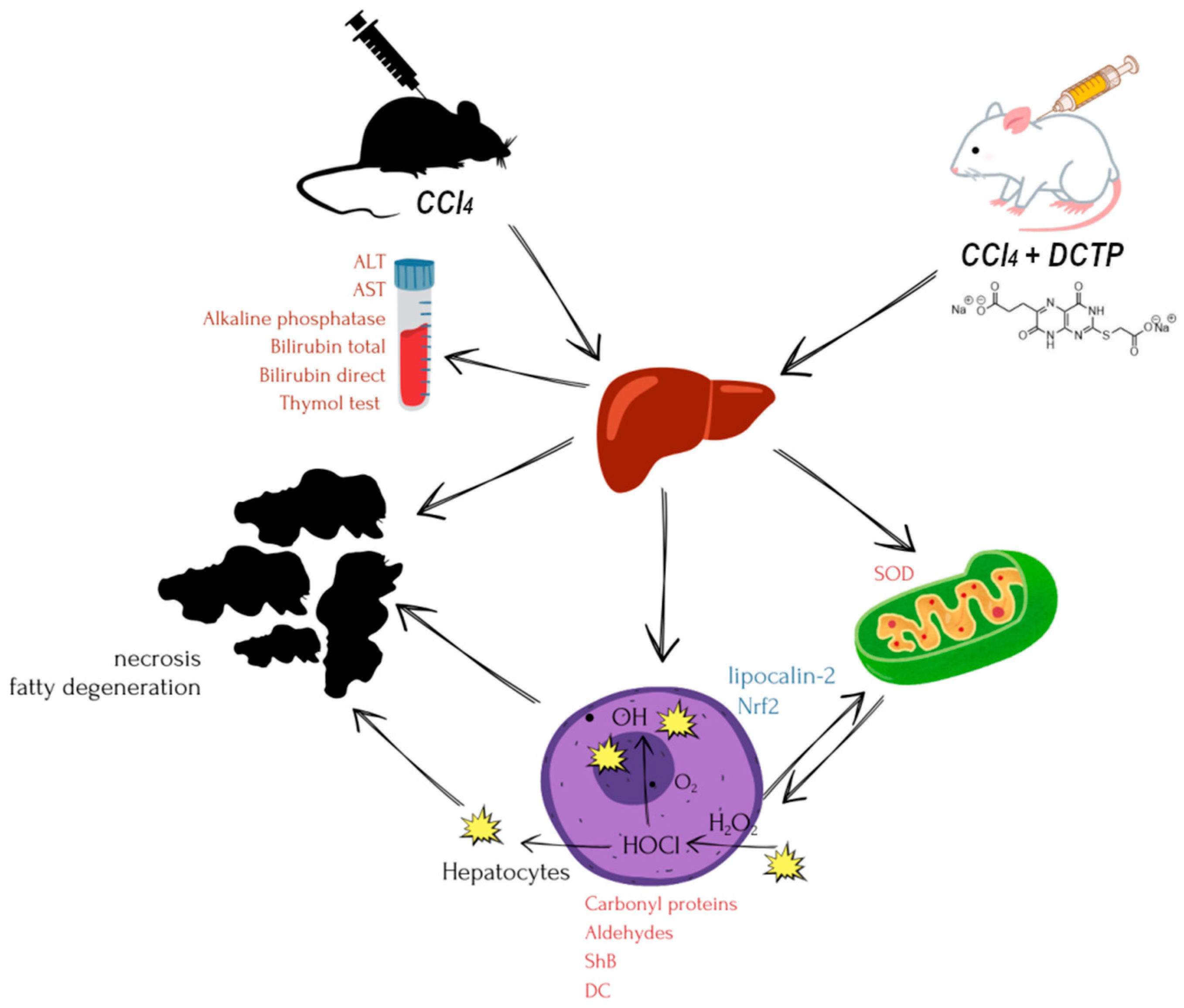
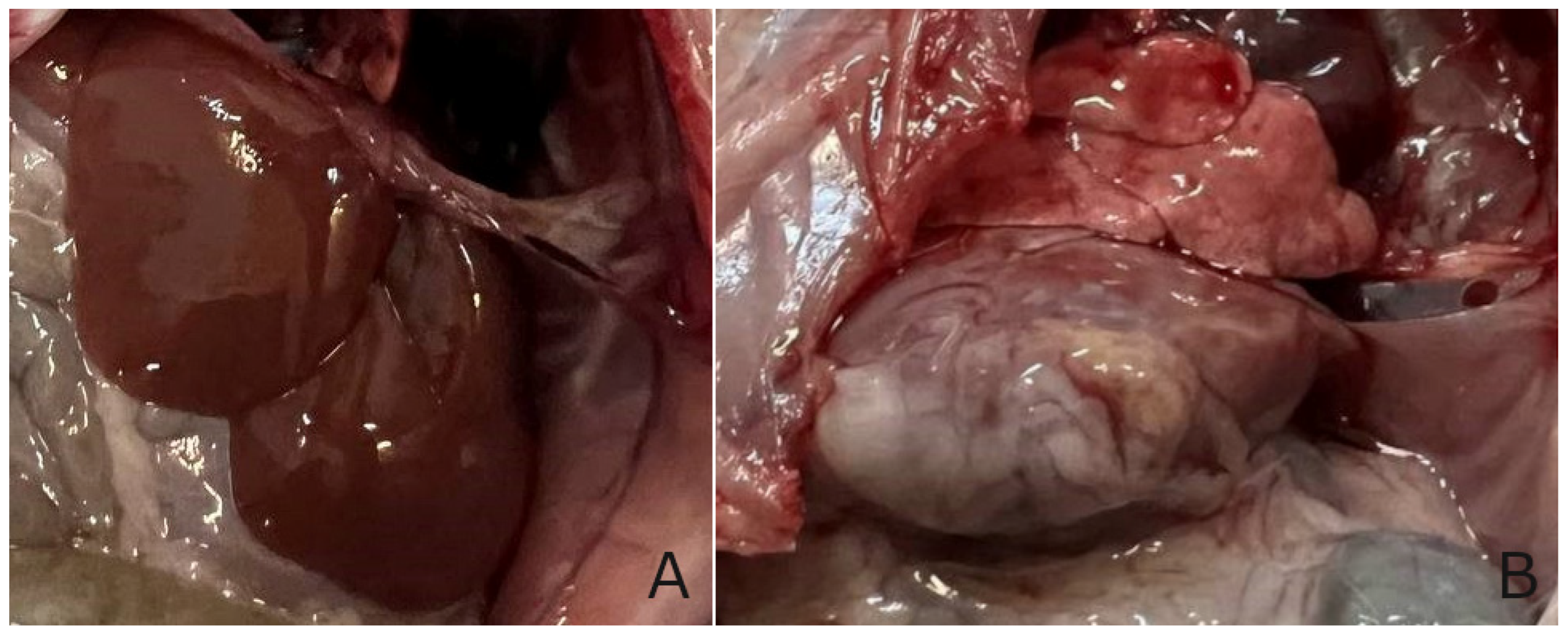
3.1. The Hepatoprotective Effect of DCTP on the Model of Toxic Liver Damage Induced by Carbon Tetrachloride
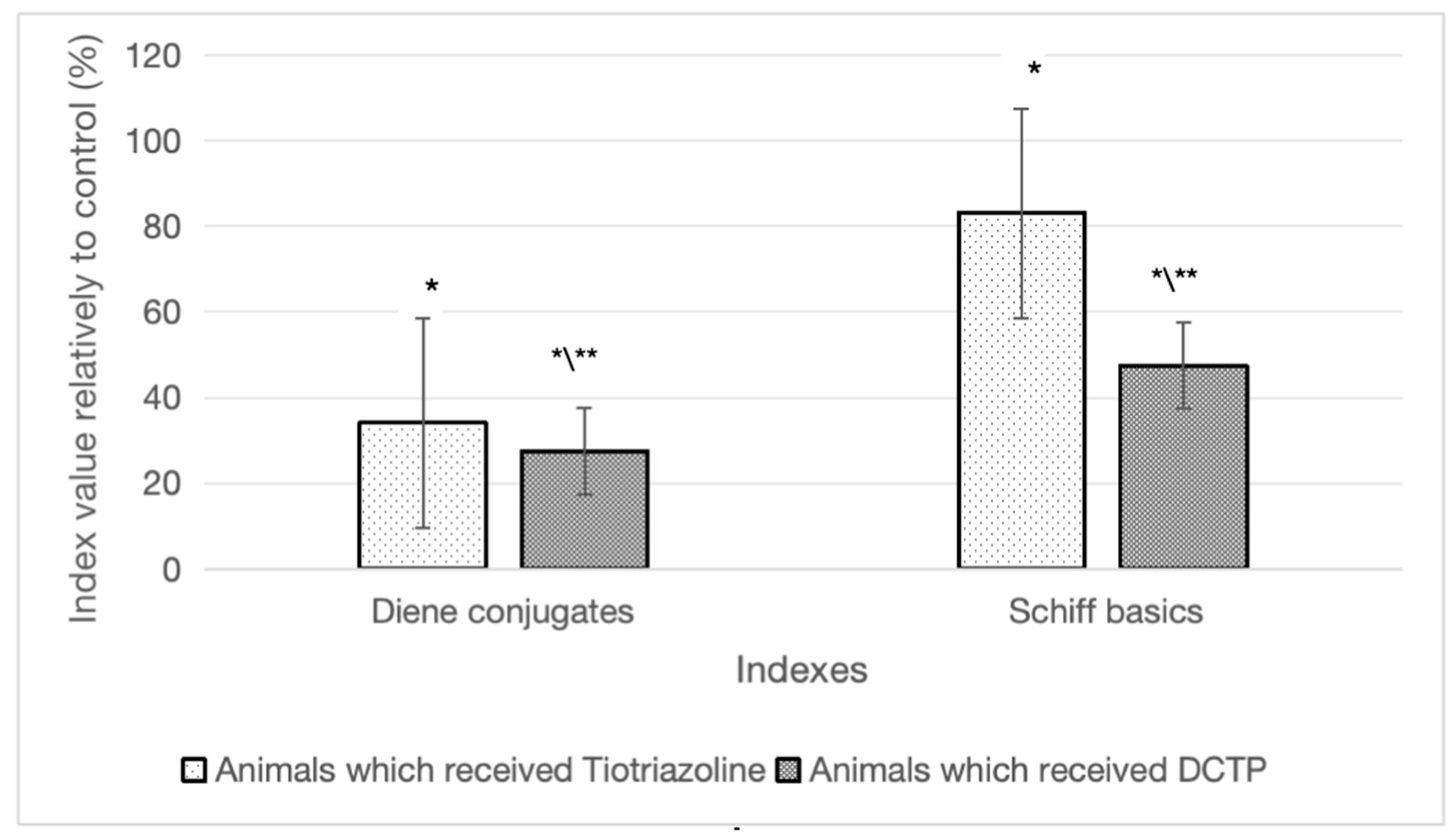
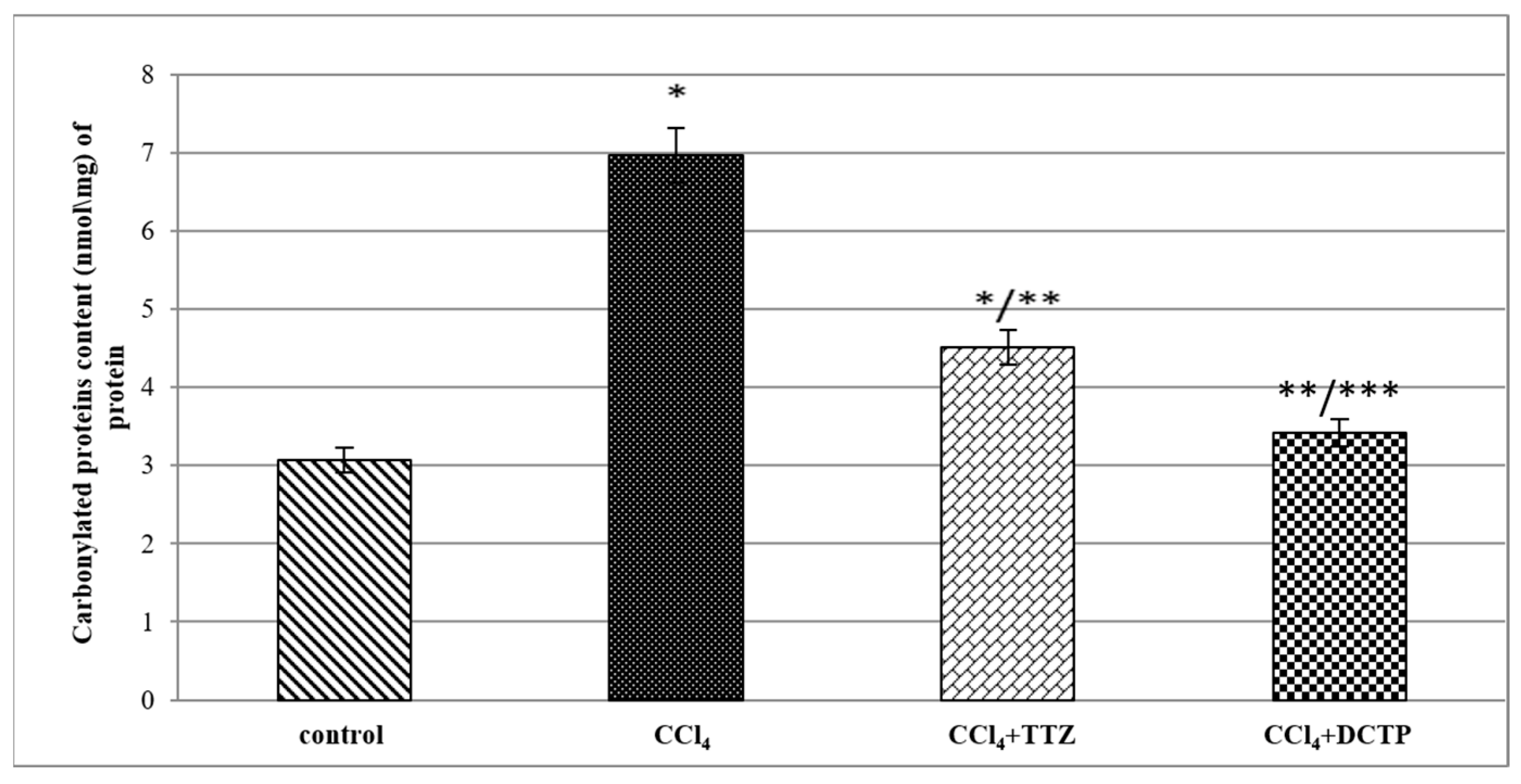
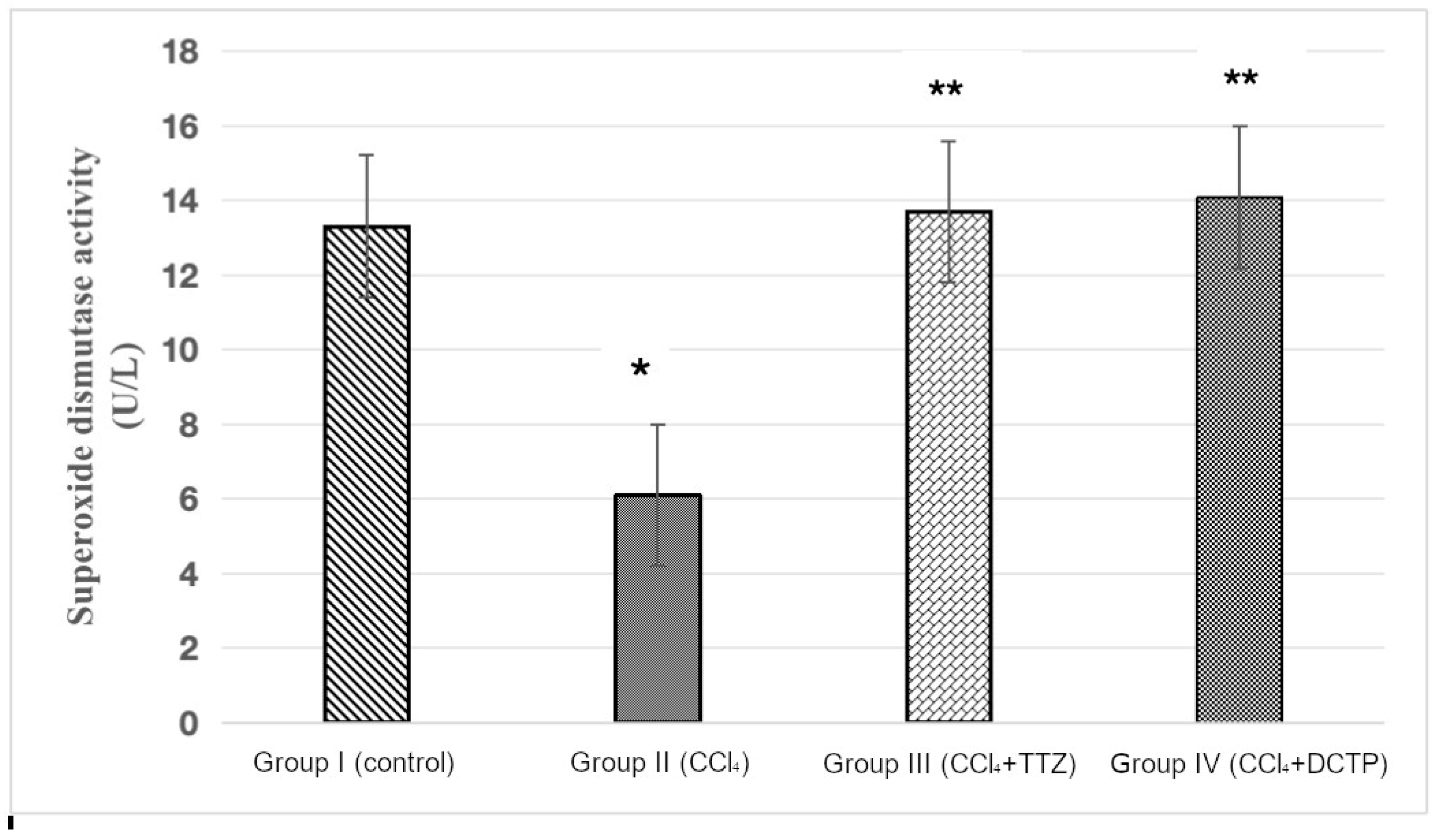
3.2. Some Indicators of the Prooxidant–Antioxidant System in the Studied Groups of Animals
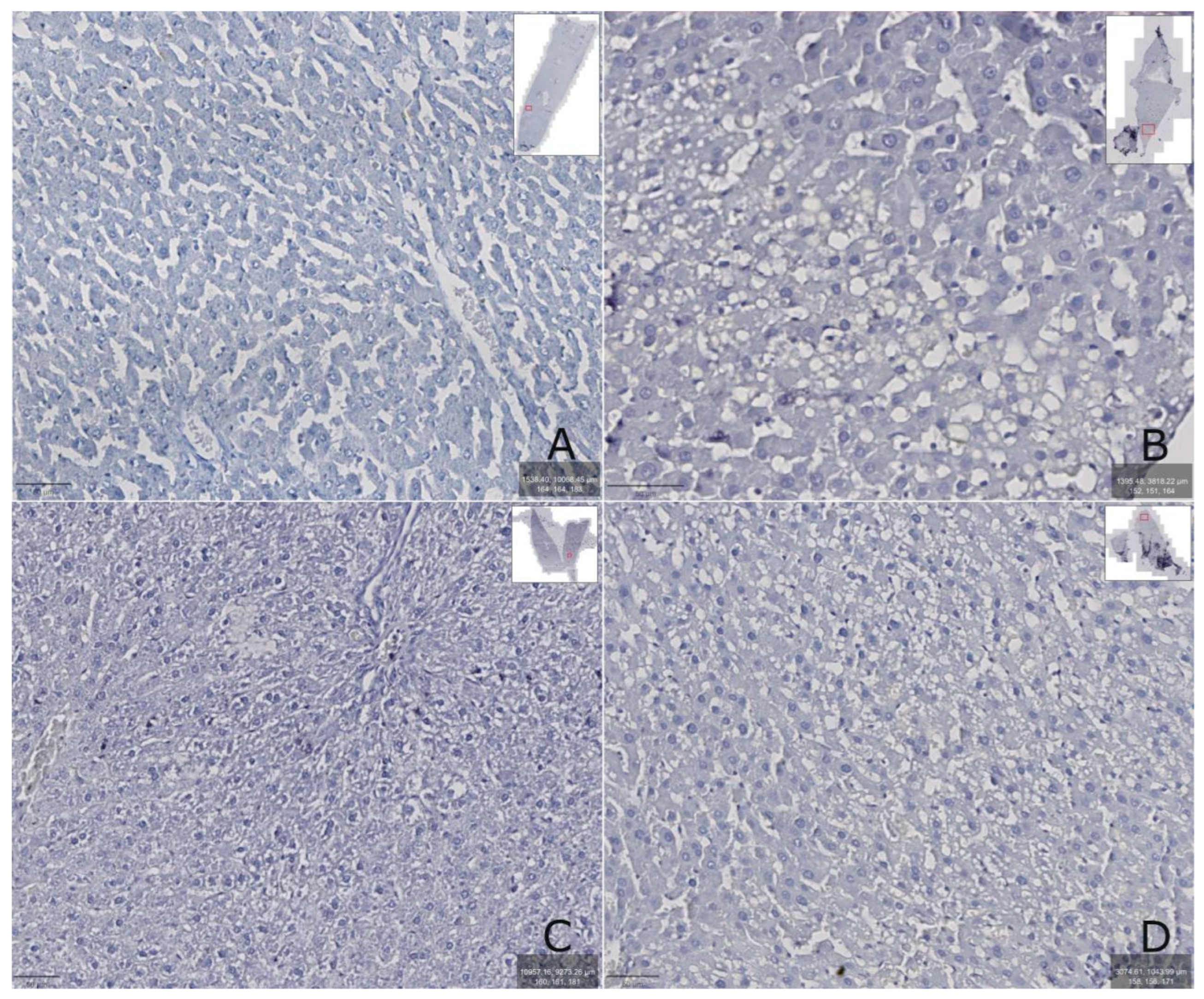
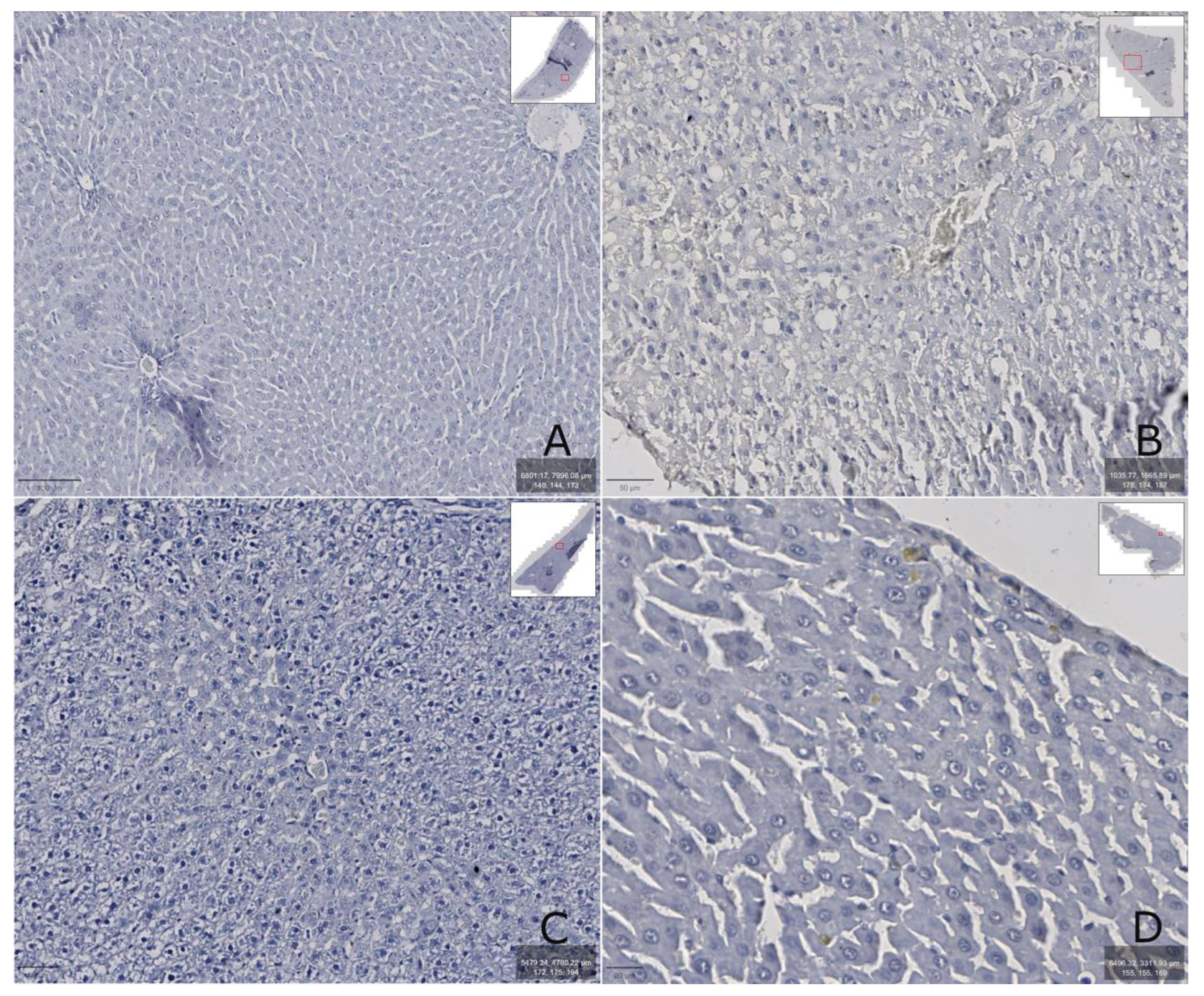
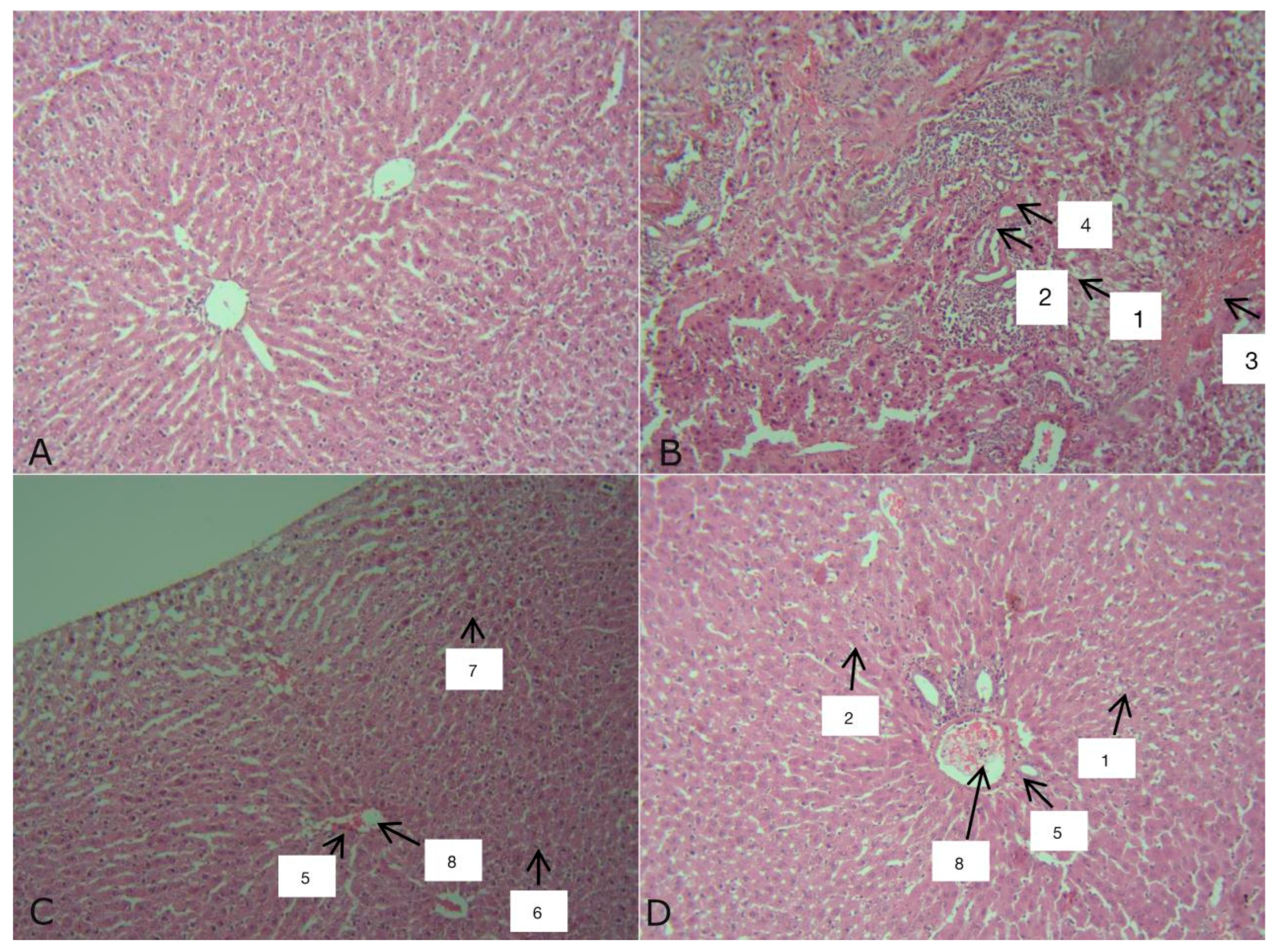
3.3. Immunohistological and Cytological Indices in the Studied Groups of Animals
3.4. Some Physiological Indicators in the Studied Groups of Animals
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Asrani, S.K.; Devarbhavi, H.; Eaton, J.; Kamath, P.S. Burden of Liver Diseases in the World. J. Hepatol. 2019, 70, 151–171. [Google Scholar] [CrossRef] [PubMed]
- Conway, R.; Carey, J.J. Risk of Liver Disease in Methotrexate Treated Patients. World J. Hepatol. 2017, 9, 1092. [Google Scholar] [CrossRef] [PubMed]
- O’Shea, R.S.; Dasarathy, S.; McCullough, A.J. Alcoholic Liver Disease. Hepatology 2009, 51, 307–328. [Google Scholar] [CrossRef]
- Saeter, G.; Lee, C.-Z.; Schwarze, P.K.; Ous, S.; Chen, D.-S.; Sung, J.-L.; Seglen, P.O. Changes in Ploidy Distributions in Human Liver Carcinogenesis. J. Natl. Cancer Inst. 1988, 80, 1480–1484. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Gordillo, K.; Shah, R.; Muriel, P. Oxidative Stress and Inflammation in Hepatic Diseases: Current and Future Therapy. Oxid. Med. Cell. Longev. 2017, 2017, 3140673. [Google Scholar] [CrossRef]
- Nolan, J.P. The Role of Intestinal Endotoxin in Liver Injury: A Long and Evolving History. Hepatology 2010, 52, 1829–1835. [Google Scholar] [CrossRef]
- Hoffman, D.R.; Marion, D.W.; Cornatzer, W.E.; Duerre, J.A. S-Adenosylmethionine and S-Adenosylhomocysteine Metabolism in Isolated Rat Liver. J. Biol. Chem. 1980, 255, 10822–10827. [Google Scholar] [CrossRef]
- Lan, X.; Field, M.S.; Stover, P.J. Cell Cycle Regulation of Folate-Mediated One-Carbon Metabolism. Wiley Interdiscip. Rev. Syst. Biol. Med. 2018, 10, e1426. [Google Scholar] [CrossRef]
- Hine, C.; Harputlugil, E.; Zhang, Y.; Ruckenstuhl, C.; Lee, B.C.; Brace, L.; Longchamp, A.; Treviño-Villarreal, J.H.; Mejia, P.; Ozaki, C.K.; et al. Endogenous Hydrogen Sulfide Production is Essential for Dietary Restriction Benefits. Cell 2015, 160, 132–144. [Google Scholar] [CrossRef]
- Sanderson, S.M.; Gao, X.; Dai, Z.; Locasale, J.W. Methionine Metabolism in Health and Cancer: A Nexus of Diet and Precision Medicine. Nat. Rev. Cancer 2019, 19, 625–637. [Google Scholar] [CrossRef]
- DrugBank. DB12687. Available online: https://go.drugbank.com/drugs/DB12687 (accessed on 12 December 2024).
- Kazunin, M.S.; Groma, N.V.; Nosulenko, I.S.; Kinichenko, A.O.; Antypenko, O.M.; Shvets, V.M.; Voskoboinik, O.Y.; Kovalenko, S.I. Thio-Containing Pteridines: Synthesis, Modification, and Biological Activity. Arch. Pharm. 2022, 355, 2200252. [Google Scholar] [CrossRef] [PubMed]
- Lohvinenko, N.; Shvets, V.; Berest, G.; Nosulenko, I.; Voskoboinik, O.; Severina, H.; Okovytyy, S.; Kovalenko, S. Prospects for the Use of Sulfur-Containing Pteridines in Toxic Liver Damage. Regul. Mech. Biosyst. 2024, 15, 374–381. [Google Scholar] [CrossRef]
- Milstien, S.; Kapatos, G.; Levine, R.A.; Shane, B. Chemistry and Biology of Pteridines and Folates; Springer: Boston, MA, USA, 2002. [Google Scholar] [CrossRef]
- Groma, N.; Berest, G.; Antypenko, O.; Voskoboinik, O.; Kopiika, V.; Kovalenko, S.; Shvets, V. Evaluation of the Toxicity and Hepatoprotective Properties of New S-Substituted Pteridins. Curr. Issues Pharm. Med. Sci. 2023, 36, 21–26. [Google Scholar] [CrossRef]
- Kozhem’yakin, Y.M.; Khromov, O.S.; Filonenko, M.A. Scientific and Practical Recommendations for the Development of Laboratory Creatures and Robots; Avitsena: Kyiv, Ukraine, 2002; p. 156. [Google Scholar]
- European Convention for the Protection of Vertebrate Animals Used for Experimental and Other Scientific Purposes; European Treaty Series—No. 123; Council of Europe: Strasbourg, France, 1986.
- Stefanov, O.V. Preclinical Study of Drugs (Methodical Recommendation); Avitsena: Kyiv, Ukraine, 2001; p. 527. [Google Scholar]
- Bhakuni, G.S.; Bedi, O.; Bariwal, J.; Deshmukh, R.; Kumar, P. Animal Models of Hepatotoxicity. Inflamm. Res. 2015, 65, 13–24. [Google Scholar] [CrossRef]
- Mazur, I.A.; Voloshin, N.A.; Chekman, I.S. Thiotriazolin: Pharmacological Aspects and Clinical Application; Zaporizhye: Lvov, Ukraine, 2005; p. 160. [Google Scholar]
- Recknagel, R.O.; Ghoshal, A.K. Quantitative Estimation of Peroxidative Degeneration of Rat Liver Microsomal and Mitochondrial Lipids After Carbon Tetrachloride Poisoning. Exp. Mol. Pathol. 1966, 5, 413–426. [Google Scholar] [CrossRef]
- Symons, M.C.R.; Diplock, A.T.; Rice-Evans, C.A. Techniques in Free Radical Research; Elsevier Science & Technology Books: Amsterdam, The Netherlands, 1991; ISBN 9780080858913. [Google Scholar]
- Kostyuk, V.A. A Simple and Sensitive Method for Determining Superoxide Dismutase Activity Based on the Oxidation Reaction of Quercetin. Questions Med. Chem. 1990, 36, 88–91. [Google Scholar]
- Levine, R.L.; Stadtman, E.R. Oxidative Modification of Proteins During Aging. Exp. Gerontol. 2001, 36, 1495–1502. [Google Scholar] [CrossRef]
- Vlizlo, V.V.; Fedoruk, R.S.; Ratych, I.B.; Vishurt, O.I.; Sharan, M.M.; Vudmaska, I.V.; Fedorovych, E.I. Laboratory Research Methods in Biology, Animal Husbandry and Veterinary Medicine: A Guide; Spolom: Lviv, Ukraine, 2012; 764p. [Google Scholar]
- Schumann, G.; Klauke, R.; Canalias, F.; Bossert-Reuther, S.; Franck, P.F.; Gella, F.-J.; Jørgensen, P.J.; Kang, D.; Lessinger, J.-M.; Panteghini, M.; et al. IFCC Primary Reference Procedures for the Measurement of Catalytic Activity Concentrations of Enzymes at 37 °C. Part 9: Reference Procedure for the Measurement of Catalytic Concentration of Alkaline Phosphatase. Clin. Chem. Lab. Med. 2011, 49, 9. [Google Scholar] [CrossRef]
- Davydov, V.V.; Shvets, V.N. Guide to Practical Classes in Biological Chemistry (for Students of Medical Schools III-IV Level of Accreditation); KhNU Named after V.N. Karazin: Kharkiv, Ukraine, 2011; 316p, ISBN 978-966-623-774-6. [Google Scholar]
- Jendrassik, L.; Grof, P. Colorimetric Method of Determination of Bilirubin. Biochem. Z. 1938, 297, 81–82. [Google Scholar]
- Menshikov, V.V. Laboratory Research Methods in Clinic. Meditsina 1987, 174–177. [Google Scholar]
- Borkham-Kamphorst, E.; Kovalenko, E.; Van Roeyen, C.R.; Gassler, N.; Bomble, M.; Ostendorf, T.; Floege, J.; Gressner, A.M.; Weiskirchen, R. Platelet-Derived Growth Factor Isoform Expression in Carbon Tetrachloride-Induced Chronic Liver Injury. Lab. Investig. 2008, 88, 1090–1100. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.-Y.; Yuan, W.-G.; He, P.; Lei, J.-H.; Wang, C.-X. Liver Fibrosis and Hepatic Stellate Cells: Etiology, Pathological Hallmarks and Therapeutic Targets. World J. Gastroenterol. 2016, 22, 10512. [Google Scholar] [CrossRef]
- Ighodaro, O.M.; Asejeje, A.O.; Adeosun, A.M.; Ujomu, T.S.; Olisedeme, C.J. Dose and Time Dependent Effects of Intraperitoneal Administration of Carbon Tetrachloride (CCl4) on Blood Lipid Profile in Wistar Rats. EC Pharmacol. Toxicol. 2020, 8, 21–25. [Google Scholar]
- Manhar, N.; Singh, S.K.; Yadav, P.; Bishnolia, M.; Khurana, A.; Bhatti, J.S.; Navik, U. Methyl Donor Ameliorates CCl4-Induced Nephrotoxicity by Inhibiting Oxidative Stress, Inflammation, and Fibrosis Through the Attenuation of Kidney Injury Molecule 1 and Neutrophil Gelatinase-Associated Lipocalin Expression. J. Biochem. Mol. Toxicol. 2025, 39, 3. [Google Scholar] [CrossRef]
- Stefan, N.; Kantartzis, K.; Häring, H.-U. Causes and Metabolic Consequences of Fatty Liver. Endocr. Rev. 2008, 29, 939–960. [Google Scholar] [CrossRef]
- Akagawa, M. Protein Carbonylation: Molecular Mechanisms, Biological Implications, and Analytical Approaches. Free Radic. Res. 2021, 55, 307–320. [Google Scholar] [CrossRef]
- Friguet, B.; Bulteau, A.-L.; Chondrogianni, N.; Conconi, M.; Petropoulos, I.-B. Protein Degradation by the Proteasome and Its Implications in Aging. Ann. N. Y. Acad. Sci. 2006, 908, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Davydov, V.V.; Bozhkov, A.I.; Kulchitsky, O.K. Physiological and Pathophysiological Role of Endogenous Aldehydes; Palmarium Academic Publishing: Saarbrucken, Germany, 2012; 240p. [Google Scholar]
- Carbone, D.L.; Doorn, J.A.; Kiebler, Z.; Ickes, B.R.; Petersen, D.R. Modification of Heat Shock Protein 90 by 4-Hydroxynonenal in a Rat Model of Chronic Alcoholic Liver Disease. J. Pharmacol. Exp. Ther. 2005, 315, 8–15. [Google Scholar] [CrossRef]
- Carbone, D.L.; Doorn, J.A.; Kiebler, Z.; Petersen, D.R. Cysteine Modification by Lipid Peroxidation Products Inhibits Protein Disulfide Isomerase. Chem. Res. Toxicol. 2005, 18, 1324–1331. [Google Scholar] [CrossRef]
- Walters, D.M.; Cho, H.-Y.; Kleeberger, S.R. Oxidative Stress and Antioxidants in the Pathogenesis of Pulmonary Fibrosis: A Potential Role for Nrf2. Antioxid. Redox Signal. 2008, 10, 321–332. [Google Scholar] [CrossRef]
- Wong, C.M.; Cheema, A.K.; Zhang, L.; Suzuki, Y.J. Protein Carbonylation as a Novel Mechanism in Redox Signaling. Circ. Res. 2008, 102, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Knockaert, L.; Berson, A.; Ribault, C.; Prost, P.-E.; Fautrel, A.; Pajaud, J.; Lepage, S.; Lucas-Clerc, C.; Bégué, J.-M.; Fromenty, B.; et al. Carbon Tetrachloride-Mediated Lipid Peroxidation Induces Early Mitochondrial Alterations in Mouse Liver. Lab. Investig. 2011, 92, 396–410. [Google Scholar] [CrossRef]
- VI International Scientific and Theoretical Conference «Sectoral Research XXI: Characteristics and Features»; Primedia eLaunch LLC: Dallas, TX, USA, 2023; ISBN 9798889557678. [CrossRef]
- Borkham-Kamphorst, E.; Drews, F.; Weiskirchen, R. Induction of Lipocalin-2 Expression in Acute and Chronic Experimental Liver Injury Moderated by Pro-Inflammatory Cytokines Interleukin-1β Through Nuclear Factor-κB Activation. Liver Int. 2011, 31, 656–665. [Google Scholar] [CrossRef]
- Dahl, S.L.; Woodworth, J.S.; Lerche, C.J.; Cramer, E.P.; Nielsen, P.R.; Moser, C.; Thomsen, A.R.; Borregaard, N.; Cowland, J.B. Lipocalin-2 Functions as Inhibitor of Innate Resistance to Mycobacterium tuberculosis. Front. Immunol. 2018, 9, 2717. [Google Scholar] [CrossRef]
- DeCicco, L.A.; Rikans, L.E.; Tutor, C.G.; Hornbrook, K.R. Serum and Liver Concentrations of Tumor Necrosis Factor α and Interleukin-1β Following Administration of Carbon Tetrachloride to Male Rats. Toxicol. Lett. 1998, 98, 115–121. [Google Scholar] [CrossRef]
- Teschke, R.; Vierke, W.; Goldermann, L. Carbon Tetrachloride (CCl4) Levels and Serum Activities of Liver Enzymes Following Acute CCl4 Intoxication. Toxicol. Lett. 1983, 17, 175–180. [Google Scholar] [CrossRef]
- Teschke, R. Liver Injury by Carbon Tetrachloride Intoxication in 16 Patients Treated with Forced Ventilation to Accelerate Toxin Removal via the Lungs: A Clinical Report. Toxics 2018, 6, 25. [Google Scholar] [CrossRef]
- Stepanov, Y.M.; Kosynskaya, S.I. The Use of Thiotriazoline in Patients with Chronic Liver Diseases. Zaporizhzhya Med. J. 2010, 5, 69–70. [Google Scholar]
- Bernabeu-Wittel, M.; Gómez-Díaz, R.; González-Molina, Á.; Vidal-Serrano, S.; Díez-Manglano, J.; Salgado, F.; Soto-Martín, M.; Ollero-Baturone, M.; Researchers, O.B.O.T.P. Oxidative Stress, Telomere Shortening, and Apoptosis Associated to Sarcopenia and Frailty in Patients with Multimorbidity. J. Clin. Med. 2020, 9, 2669. [Google Scholar] [CrossRef]
- Zhou, J.; Zheng, Q.; Chen, Z. The Nrf2 Pathway in Liver Diseases. Front. Cell Dev. Biol. 2022, 10, 826204. [Google Scholar] [CrossRef]
- Yamashita, Y.; Ueyama, T.; Nishi, T.; Yamamoto, Y.; Kawakoshi, A.; Sunami, S.; Iguchi, M.; Tamai, H.; Ueda, K.; Ito, T.; et al. Nrf2-Inducing Anti-Oxidation Stress Response in the Rat Liver—New Beneficial Effect of Lansoprazole. PLoS ONE 2014, 9, e97419. [Google Scholar] [CrossRef]
- Asimakopoulou, A.; Weiskirchen, S.; Weiskirchen, R. Lipocalin 2 (LCN2) Expression in Hepatic Malfunction and Therapy. Front. Physiol. 2016, 7, 430. [Google Scholar] [CrossRef] [PubMed]
- Llewellyn, J.; Fede, C.; Loneker, A.E.; Friday, C.S.; Hast, M.W.; Theise, N.D.; Furth, E.E.; Guido, M.; Stecco, C.; Wells, R.G. Glisson’s Capsule Matrix Structure and Function Is Altered in Patients with Cirrhosis Irrespective of Etiology. JHEP Rep. 2023, 5, 100760. [Google Scholar] [CrossRef] [PubMed]
- Stecco, C.; Sfriso, M.M.; Porzionato, A.; Rambaldo, A.; Albertin, G.; Macchi, V.; De Caro, R. Microscopic Anatomy of the Visceral Fasciae. J. Anat. 2017, 231, 121–128. [Google Scholar] [CrossRef]
- Allen, W.E. Terminologia Anatomica: International Anatomical Terminology and Terminologia Histologica: International Terms for Human Cytology and Histology. J. Anat. 2009, 215, 221. [Google Scholar] [CrossRef]
- Benias, P.C.; Wells, R.G.; Sackey-Aboagye, B.; Klavan, H.; Reidy, J.; Buonocore, D.; Miranda, M.; Kornacki, S.; Wayne, M.; Carr-Locke, D.L.; et al. Structure and Distribution of an Unrecognized Interstitium in Human Tissues. Sci. Rep. 2018, 8, 23062. [Google Scholar] [CrossRef]
- Hayashi, S.; Murakami, G.; Ohtsuka, A.; Itoh, M.; Nakano, T.; Fukuzawa, Y. Connective Tissue Configuration in the Human Liver Hilar Region with Special Reference to the Liver Capsule and Vascular Sheath. J. Hepatobiliary-Pancreat. Surg. 2008, 15, 640–647. [Google Scholar] [CrossRef]
- Wang, J.; Kubes, P. A Reservoir of Mature Cavity Macrophages That Can Rapidly Invade Visceral Organs to Affect Tissue Repair. Cell 2016, 165, 668–678. [Google Scholar] [CrossRef]
- Wagner, B.A.; Venkataraman, S.; Buettner, G.R. The Rate of Oxygen Utilization by Cells. Free Radic. Biol. Med. 2011, 51, 700–712. [Google Scholar] [CrossRef]
- Acharya, P.; Chouhan, K.; Weiskirchen, S.; Weiskirchen, R. Cellular Mechanisms of Liver Fibrosis. Front. Pharmacol. 2021, 12, 671640. [Google Scholar] [CrossRef]
- Guilliams, M.; Bonnardel, J.; Haest, B.; Vanderborght, B.; Wagner, C.; Remmerie, A.; Bujko, A.; Martens, L.; Thoné, T.; Browaeys, R.; et al. Spatial Proteogenomics Reveals Distinct and Evolutionarily Conserved Hepatic Macrophage Niches. Cell 2022, 185, 379–396.e38. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Kang, C.H.; Gou, X.; Peng, Q.; Yan, J.; Zhuo, S.; Cheng, C.L.; He, Y.; Kang, Y.; Xia, W.; et al. Quantification of Liver Fibrosis via Second Harmonic Imaging of the Glisson’s Capsule from Liver Surface. J. Biophotonics 2015, 9, 351–363. [Google Scholar] [CrossRef]
- Balog, S.; Li, Y.; Ogawa, T.; Miki, T.; Saito, T.; French, S.W.; Asahina, K. Development of Capsular Fibrosis Beneath the Liver Surface in Humans and Mice. Hepatology 2019, 71, 291–305. [Google Scholar] [CrossRef]
- Li, Y.; Wang, J.; Asahina, K. Mesothelial Cells Give Rise to Hepatic Stellate Cells and Myofibroblasts via Mesothelial-Mesenchymal Transition in Liver Injury. Proc. Natl. Acad. Sci. USA 2013, 110, 2324–2329. [Google Scholar] [CrossRef]
- Bozhkov, A.; Ionov, I.; Kurhuzova, N.; Novikova, A.; Katerynych, O.; Akzhyhitov, R. Vitamin A Intake Forms Resistance to Hypervitaminosis A and Affects the Functional Activity of the Liver. Clin. Nutr. Open Sci. 2022, 41, 82–97. [Google Scholar] [CrossRef]
- Salama, S.; Kue, C.S.; Mohamad, H.; Omer, F.; Ibrahim, M.Y.; Abdulla, M.; Ali, H.; Mariod, A.; Jayash, S.N. Hepatoprotective Potential of a Novel Quinazoline Derivative in Thioacetamide-Induced Liver Toxicity. Front. Pharmacol. 2022, 13, 943340. [Google Scholar] [CrossRef]
- He, Y.; Xia, Z.; Yu, D.; Wang, J.; Jin, L.; Huang, D.; Ye, X.; Li, X.; Zhang, B. Hepatoprotective Effects and Structure–Activity Relationship of Five Flavonoids against Lipopolysaccharide/D-Galactosamine-Induced Acute Liver Failure in Mice. Int. Immunopharmacol. 2019, 68, 171–178. [Google Scholar] [CrossRef]
- Chandel, N.S. Nucleotide Metabolism. Cold Spring Harb. Perspect. Biol. 2021, 13, a040592. [Google Scholar] [CrossRef]
- Halabitska, I.; Oksenych, V.; Kamyshnyi, O. Exploring the Efficacy of Alpha-Lipoic Acid in Comorbid Osteoarthritis and Type 2 Diabetes Mellitus. Nutrients 2024, 16, 3349. [Google Scholar] [CrossRef]
- Shan, D.; Dai, S.; Chen, Q.; Xie, Y.; Hu, Y. Hepatoprotective Agents in the Management of Intrahepatic Cholestasis of Pregnancy: Current Knowledge and Prospects. Front. Pharmacol. 2023, 14, 1218432. [Google Scholar] [CrossRef]
- Oliveira, C.; Cotrim, H.; Stefano, J.T.; Siqueira, A.; Salgado, A.; Parise, E. N-Acetylcysteine and/or Ursodeoxycholic Acid Associated with Metformin in Non-Alcoholic Steatohepatitis: An Open-Label Multicenter Randomized Controlled Trial. Arq. Gastroenterol. 2019, 56, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Petakh, P.; Kamyshna, I.; Oksenych, V.; Kainov, D.; Kamyshnyi, A. Metformin Therapy Changes Gut Microbiota Alpha-Diversity in COVID-19 Patients with Type 2 Diabetes: The Role of SARS-CoV-2 Variants and Antibiotic Treatment. Pharmaceuticals 2023, 16, 904. [Google Scholar] [CrossRef] [PubMed]
- Petakh, P.; Griga, V.; Mohammed, I.B.; Loshak, K.; Poliak, I.; Kamyshnyiy, A. Effects of Metformin, Insulin on Hematological Parameters of COVID-19 Patients with Type 2 Diabetes. Med. Arch. 2022, 76, 329–332. [Google Scholar] [CrossRef]
- Halabitska, I.; Petakh, P.; Lushchak, O.; Kamyshna, I.; Oksenych, V.; Kamyshnyi, O. Metformin in Antiviral Therapy: Evidence and Perspectives. Viruses 2024, 16, 1938. [Google Scholar] [CrossRef]
- Perazza, F.; Leoni, L.; Colosimo, S.; Musio, A.; Bocedi, G.; D’avino, M.; Agnelli, G.; Nicastri, A.; Rossetti, C.; Sacilotto, F.; et al. Metformin and the Liver: Unlocking the Full Therapeutic Potential. Metabolites 2024, 14, 186. [Google Scholar] [CrossRef]
- Buchynskyi, M.; Oksenych, V.; Kamyshna, I.; Vorobets, I.; Halabitska, I.; Kamyshnyi, O. Modulatory Roles of AHR, FFAR2, FXR, and TGR5 Gene Expression in Metabolic-Associated Fatty Liver Disease and COVID-19 Outcomes. Viruses 2024, 16, 985. [Google Scholar] [CrossRef]
- Buchynskyi, M.; Oksenych, V.; Kamyshna, I.; Budarna, O.; Halabitska, I.; Petakh, P.; Kamyshnyi, O. Genomic Insight into COVID-19 Severity in MAFLD Patients: A Single-Center Prospective Cohort Study. Front. Genet. 2024, 15, 1460318. [Google Scholar] [CrossRef]
- Bataller, R.; North, K.E.; Brenner, D.A. Genetic Polymorphisms and the Progression of Liver Fibrosis: A Critical Appraisal. Hepatology 2003, 37, 493–503. [Google Scholar] [CrossRef]
- Abdelmonem, B.H.; Abdelaal, N.M.; Anwer, E.K.E.; Rashwan, A.A.; Hussein, M.A.; Ahmed, Y.F.; Khashana, R.; Hanna, M.M.; Abdelnaser, A. Decoding the Role of CYP450 Enzymes in Metabolism and Disease: A Comprehensive Review. Biomedicines 2024, 12, 1467. [Google Scholar] [CrossRef]
- Belenichev, I.; Popazova, O.; Bukhtiyarova, N.; Savchenko, D.; Oksenych, V.; Kamyshnyi, O. Modulating Nitric Oxide: Implications for Cytotoxicity and Cytoprotection. Antioxidants 2024, 13, 504. [Google Scholar] [CrossRef]
- Gan, C.; Yuan, Y.; Shen, H.; Gao, J.; Kong, X.; Che, Z.; Guo, Y.; Wang, H.; Dong, E.; Xiao, J. Liver Diseases: Epidemiology, Causes, Trends and Predictions. Signal Transduct. Target. Ther. 2025, 10, 33. [Google Scholar] [CrossRef] [PubMed]
- Björnsson, H.K.; Björnsson, E.S. Drug-Induced Liver Injury: Pathogenesis, Epidemiology, Clinical Features, and Practical Management. Eur. J. Intern. Med. 2022, 97, 26–31. [Google Scholar] [CrossRef]
- Rehman, S.T.; Rehman, H.; Abid, S. Impact of Coronavirus Disease 2019 on Prevention and Elimination Strategies for Hepatitis B and Hepatitis C. World J. Hepatol. 2021, 13, 781–789. [Google Scholar] [CrossRef]
- Jiménez-Mendoza, J.; Rivera-López, F.; González-Lara, M.; Valdez-Echeverría, R.; Castro-Narro, G.; Tore, A.; Uscanga-Domínguez, L.; Moctezuma-Velázquez, C. Seroprevalence of Hepatitis B and C Viruses in Moderate and Severe COVID-19 Inpatients: A Cross-Sectional Study at a Referral Center in Mexico. Ann. Hepatol. 2022, 27, 100688. [Google Scholar] [CrossRef]
- He, Y.F.; Jiang, Z.G.; Wu, N.; Bian, N.; Ren, J.L. Correlation between COVID-19 and Hepatitis B: A Systematic Review. World J. Gastroenterol. 2022, 28, 6599–6618. [Google Scholar] [CrossRef]
- Elsharkawy, A.; Samir, R.; Abdallah, M.; Hassany, M.; El-Kassas, M. The implications of the COVID-19 pandemic on hepatitis B and C elimination programs in Egypt: Current situation and future perspective. Egypt. Liver J. 2023, 13, 50. [Google Scholar] [CrossRef]
- Petakh, P.; Isevych, V.; Kamyshnyi, A.; Oksenych, V. Weil’s Disease—Immunopathogenesis, Multiple Organ Failure, and Potential Role of Gut Microbiota. Biomolecules 2022, 12, 1830. [Google Scholar] [CrossRef]
- Weiskirchen, R. Hepatoprotective and Anti-fibrotic Agents: It’s Time to Take the Next Step. Front. Pharmacol. 2015, 6, 303. [Google Scholar] [CrossRef]
- Jadhav, P.A.; Thomas, A.B.; Pathan, M.K.; Chaudhari, S.Y.; Wavhale, R.D.; Chitlange, S.S. Unlocking the therapeutic potential of unexplored phytocompounds as hepatoprotective agents through integration of network pharmacology and in-silico analysis. Sci. Rep. 2025, 15, 8425. [Google Scholar] [CrossRef]
- Halabitska, I.; Babinets, L.; Oksenych, V.; Kamyshnyi, O. Diabetes and Osteoarthritis: Exploring the Interactions and Therapeutic Implications of Insulin, Metformin, and GLP-1-Based Interventions. Biomedicines 2024, 12, 1630. [Google Scholar] [CrossRef]
- Halabitska, I.; Petakh, P.; Kamyshna, I.; Oksenych, V.; Kainov, D.E.; Kamyshnyi, O. The interplay of gut microbiota, obesity, and depression: Insights and interventions. Cell. Mol. Life Sci. 2024, 81, 443. [Google Scholar] [CrossRef] [PubMed]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.-P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef] [PubMed]
- Leon, B.M.; Maddox, T.M. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J. Diabetes 2015, 6, 1246–1258. [Google Scholar] [CrossRef]
- Dzhuryak, V.; Sydorchuk, L.; Sydorchuk, A.; Kamyshnyi, O.; Kshanovska, A.; Levytska, S.; Knut, R.; Sheremet, M.; Ivashchuk, M.; Petrynych, O.; et al. The cytochrome 11B2 aldosterone synthase gene CYP11B2 (RS1799998) polymorphism associates with chronic kidney disease in hypertensive patients. Biointerface Res. Appl. Chem. 2020, 10, 5406–5411. [Google Scholar] [CrossRef]
- Bernhard, J.; Galli, L.; Speidl, W.S.; Krychtiuk, K.A. Cardiovascular Risk Reduction in Metabolic Dysfunction-Associated Steatotic Liver Disease and Metabolic Dysfunction-Associated Steatohepatitis. Curr. Cardiol. Rep. 2025, 27, 28. [Google Scholar] [CrossRef]
- Gutiérrez-Cuevas, J.; Santos, A.; Armendariz-Borunda, J. Pathophysiological Molecular Mechanisms of Obesity: A Link between MAFLD and NASH with Cardiovascular Diseases. Int. J. Mol. Sci. 2021, 22, 11629. [Google Scholar] [CrossRef]
- Țenea-Cojan, Ș.-T.; Dinescu, V.-C.; Gheorman, V.; Dragne, I.-G.; Gheorman, V.; Forțofoiu, M.-C.; Fortofoiu, M.; Dobrinescu, A.G. Exploring Multidisciplinary Approaches to Comorbid Psychiatric and Medical Disorders: A Scoping Review. Life 2025, 15, 251. [Google Scholar] [CrossRef]
- Rayman, G.; Akpan, A.; Cowie, M.; Evans, R.; Patel, M.; Posporelis, S.; Walsh, K. Managing patients with comorbidities: Future models of care. Future Healthc. J. 2022, 9, 101–105. [Google Scholar] [CrossRef]
- Kloock, S.; Ziegler, C.G.; Dischinger, U. Obesity and its comorbidities, current treatment options and future perspectives: Challenging bariatric surgery? Pharmacol. Ther. 2023, 251, 108549. [Google Scholar] [CrossRef]
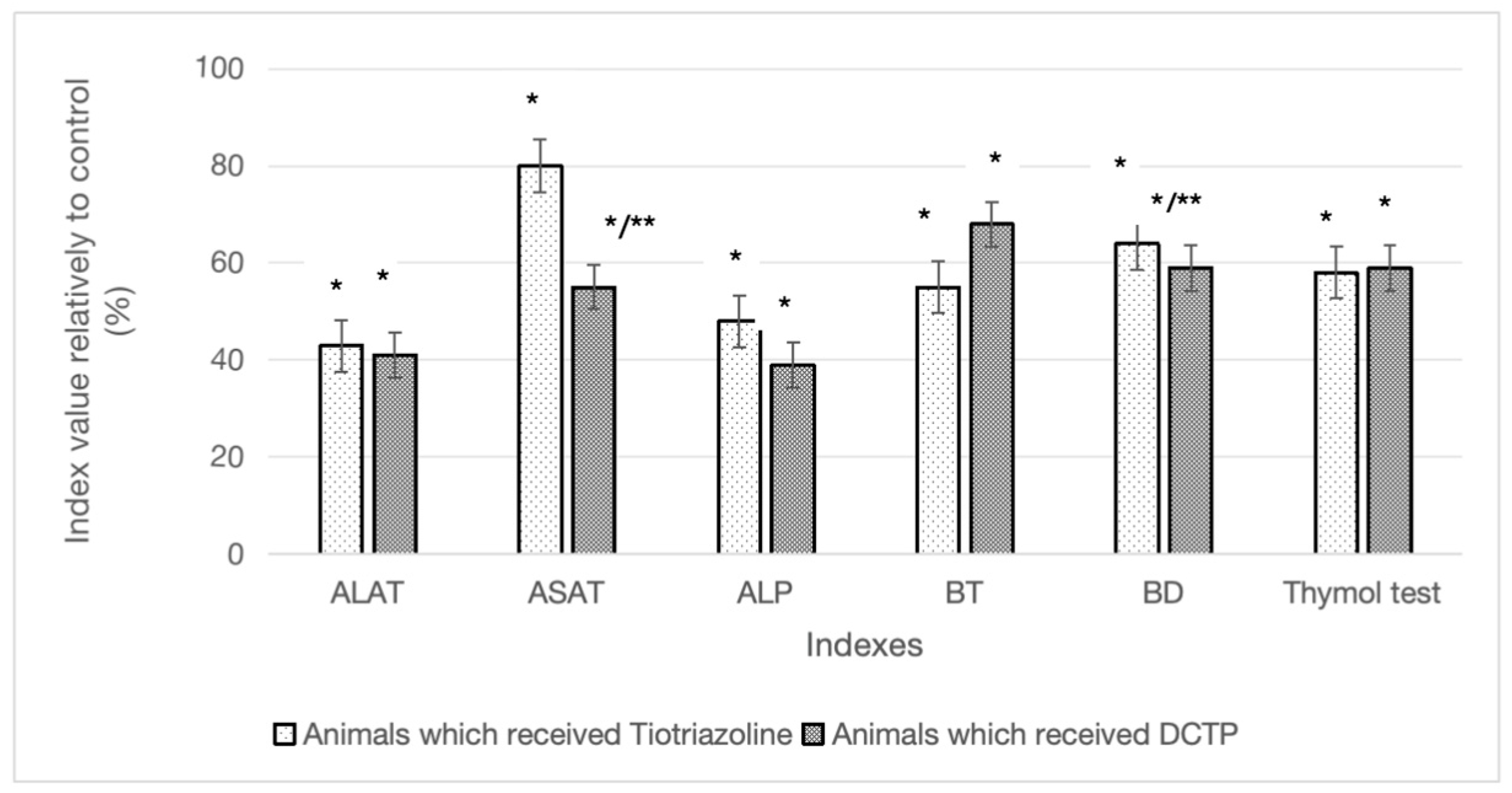

| Indicators | Experimental Groups | |||
|---|---|---|---|---|
| Group I (Control) | Group II (CCl4) | Group III (CCl4 + TTZ) | Group IV (CCl4 + DCTP) | |
| ALT (Units/L) | 42.60 ± 2.80 | 147.90 ± 9.49 * | 63.03 ± 10.50 */** | 60.50 ± 6.80 */** |
| AST (Units/L) | 78.10 ± 5.30 | 162.70 ± 12.80 * | 129.50 ± 11.49 */** | 92.70 ± 9.80 */**/*** |
| De Ritis coefficient | 1.80 ± 0.10 * | 1.10 ± 0.03 * | 2.12 ± 0.49 ** | 1.56 ± 0.29 */**/*** |
| Alkaline phosphatase (Units/L) | 90.50 ± 15.80 | 228.30 ± 44.70 * | 101.50 ± 5.45 ** | 89.40 ± 21.00 ** |
| Total bilirubin (mmol/L) | 9.60 ± 1.80 | 19.18 ± 1.80 * | 10.35 ± 1.05 ** | 12.90 ± 2.10 ** |
| Direct bilirubin (mmol/L) | 3.30 ± 0.10 | 5.58 ± 0.78 * | 3.56 ± 0.19 ** | 3.30 ± 0.40 ** |
| Thymol test (Sh) | 0.90 ± 0.05 | 4.62 ± 0.56 * | 1.93 ± 0.46 ** | 1.90 ± 0.20 ** |
| Animal Group | Diene Conjugates (nmol/g) | Schiff Bases (nmol/g) |
|---|---|---|
| Group I (control) | 25.19 ± 2.38 | 38.80 ± 17.69 |
| Group II (CCl4) | 48.34 ± 1.06 * | 116.00 ± 28.33 * |
| Group III (CCl4 + TTZ) | 34.22 ± 2.63 ** | 83.11 ± 14.94 ** |
| Group IV (CCl4 + DCTP) | 27.48 ± 1.34 **/*** | 47.56 ± 10.67 **/*** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lohvinenko, N.; Shvets, V.; Antypenko, O.; Voskoboinik, O.; Bozhkov, A.; Maslak, H.; Oksenych, V.; Kamyshnyi, O.; Okovytyy, S.; Kovalenko, S. The Application of S-Substituted Pteridine for CCl4-Induced Acute Hepatitis Treatment in Rats. Biomedicines 2025, 13, 1276. https://doi.org/10.3390/biomedicines13061276
Lohvinenko N, Shvets V, Antypenko O, Voskoboinik O, Bozhkov A, Maslak H, Oksenych V, Kamyshnyi O, Okovytyy S, Kovalenko S. The Application of S-Substituted Pteridine for CCl4-Induced Acute Hepatitis Treatment in Rats. Biomedicines. 2025; 13(6):1276. https://doi.org/10.3390/biomedicines13061276
Chicago/Turabian StyleLohvinenko, Natalia, Volodymyr Shvets, Oleksii Antypenko, Oleksii Voskoboinik, Andrii Bozhkov, Hanna Maslak, Valentyn Oksenych, Oleksandr Kamyshnyi, Sergiy Okovytyy, and Serhii Kovalenko. 2025. "The Application of S-Substituted Pteridine for CCl4-Induced Acute Hepatitis Treatment in Rats" Biomedicines 13, no. 6: 1276. https://doi.org/10.3390/biomedicines13061276
APA StyleLohvinenko, N., Shvets, V., Antypenko, O., Voskoboinik, O., Bozhkov, A., Maslak, H., Oksenych, V., Kamyshnyi, O., Okovytyy, S., & Kovalenko, S. (2025). The Application of S-Substituted Pteridine for CCl4-Induced Acute Hepatitis Treatment in Rats. Biomedicines, 13(6), 1276. https://doi.org/10.3390/biomedicines13061276











