1. Introduction
In recent years, there has been considerable interest in Kv channels as potential therapeutic targets for the treatment of chronic pain [
1,
2]. Kv channels form a large family, with several different subtypes co-expressed within nociceptive neurons [
3,
4,
5]. These include Kv2.1 and Kv2.2, as well as modulatory or ‘silent’ KvS subunits, such as Kv9.1 and Kv6.4, which do not form functional channels alone but co-assemble with Kv2 subunits to form heteromeric channels [
6,
7,
8]. The dysregulation of Kv2 and KvS subunits has been shown to be associated with altered pain sensitivity [
5,
9,
10,
11,
12]. For example, in animal models of chronic neuropathic pain, the expression of Kv2.1, Kv2.2, and Kv9.1 channels is down-regulated, and, for Kv9.1, the time course mirrors the development of pain [
5,
10,
11]. Further evidence to support a role for Kv9.1 in modulating pain has come from its selective knockdown in mouse sensory neurons, which caused exaggerated pain responses in models of neuropathy. There have also been single-nucleotide polymorphisms (SNPs) identified in both human Kv9.1 and Kv6.4, which are associated with altered pain sensitivity [
13,
14]. For example, a rare mutation within the pore region of Kv6.4, Val419Met, which disrupts its ability to form heteromeric channels with Kv2 subunits, produces an increase in the pain threshold and is associated with reduced human labour pain [
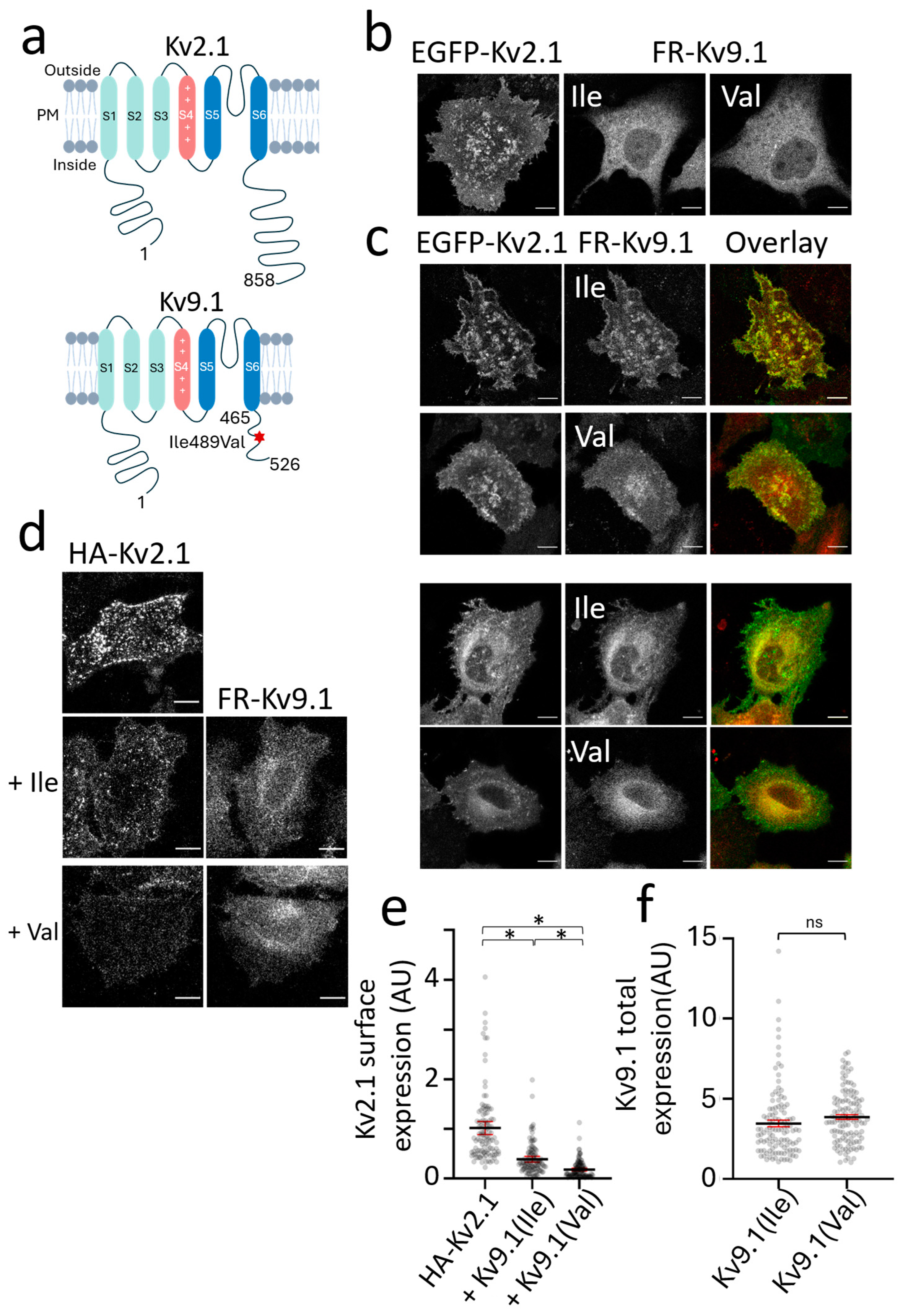
13]. For Kv9.1, a common SNP that produces a Val substitution for Ile489 was shown to be associated with higher pain scores in five out of six independent patient cohorts and across a number of human chronic pain conditions, including sciatic and phantom limb pain [
14]. Additionally, the risk profile was additive, with two copies conferring greater risk than one. The mechanism by which Kv9.1 regulates pain sensitivity remains unknown, but we hypothesise that this occurs via its association with and regulation of Kv2 channels.
KvS comprises a group of 10 subunits that have been identified to date [
6]. They share the same architecture as other Kv subunits, where all four subunits of KvS-Kv2 heterotetrameric assemblies contribute to the central conduction pore [
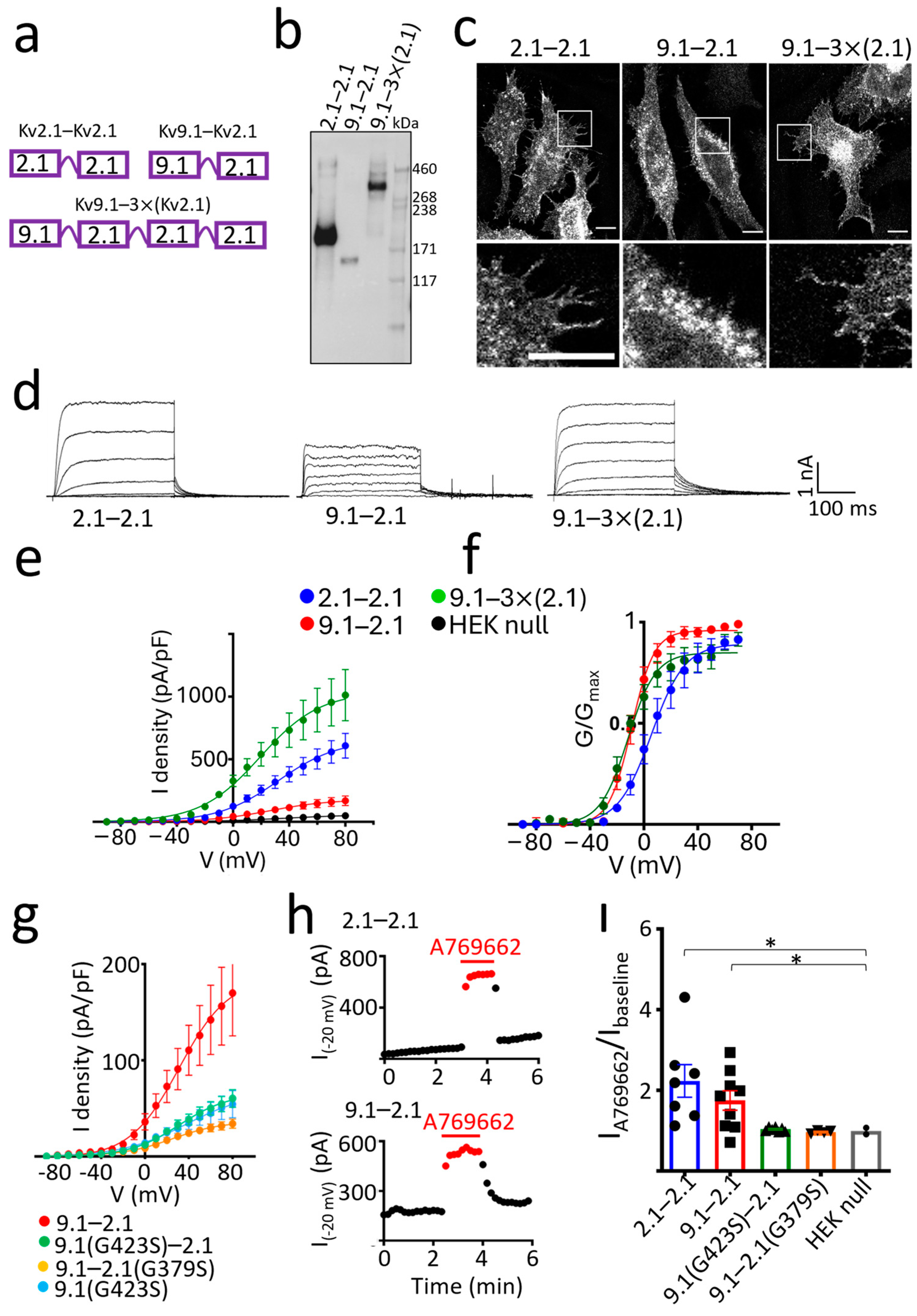
7]. The preferred stoichiometry of these assemblies remains controversial. The use of FRET to investigate the channels formed between rat Kv9.3 and Kv2.1 indicated a fixed stoichiometry of one Kv9.3 to three Kv2.1 subunits [
15]. A similar structure was proposed for Kv6.4-Kv2.1 heteromeric assemblies based upon both an analysis of the movement of voltage sensors within the channel complex and the counting of subunits within plasma membrane (PM) channels by the bleaching of GFP tags on either Kv6.4 or Kv2.1 [
16]. Recent evidence has suggested, however, that the preferred ratio is 2:2, with Kv6.4 and Kv2.1 subunits alternating around the pore [
17]. This evidence includes an analysis of the properties of different tetrameric concatamers of Kv2.1 and Kv6.4, and it suggests that more than one stoichiometric arrangement might be permitted, dependent on the KvS subunit involved.
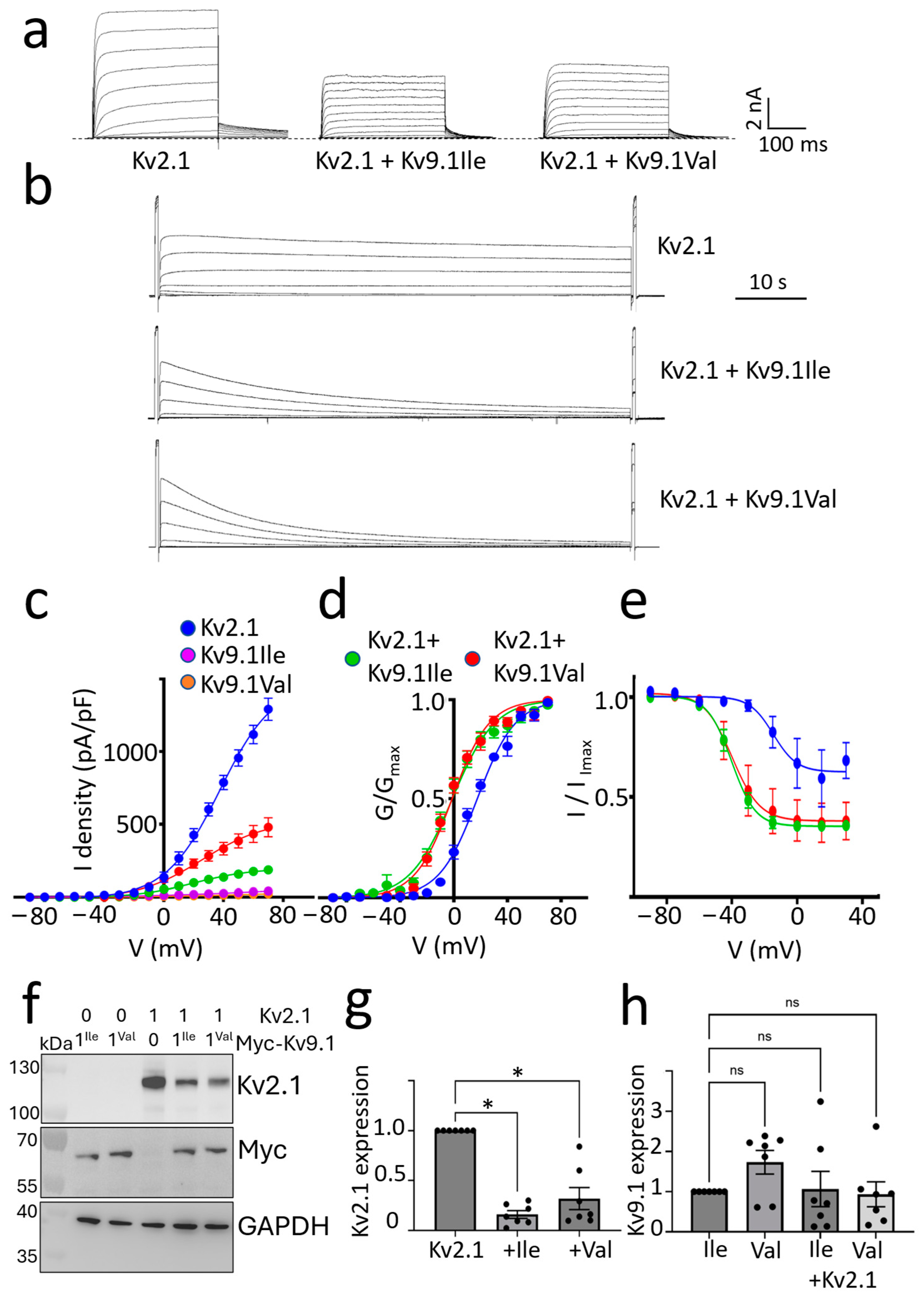
Measurements of KvS-Kv2 channel currents following the expression in heterologous systems indicate that different KvS subunits modulate the conductance properties of Kv2 channels in different ways. Neuronal Kv2 channels are delayed rectifier channels, which play a role in the repolarisation of the membrane potential during action potential firing and regulate the width of the action potentials, the after-hyperpolarisation, and the frequency of firing [
18]. The co-expression of Kv6.4 with Kv2.1 produces a small (5 mV) hyperpolarising shift in the voltage dependence of channel activation and a more profound (30 mV) hyperpolarising shift in steady-state inactivation [
6,
13]. The shift in inactivation and the resultant decrease in the amplitude of Kv currents reduce the threshold current needed to evoke an action potential and hence increase neuronal excitability. Neuronal excitability is predicted to be reduced for the ‘assembly deficient’ Kv6.4 pore mutant, which would explain the elevated pain threshold in individuals expressing this variant. An early study examining the effect of rat Kv9.1 on Kv2.1 currents in Xenopus oocytes also showed a hyperpolarising shift in the voltage dependence of both channel activation and inactivation compared with Kv2.1 alone, as well as a suppression of Kv2.1 current amplitudes [
8]. A comparison of how the two human variants of Kv9.1 (Ile 489 and Val489) affect Kv2.1-mediated currents remains to be conducted [
14].
In addition to a consideration of the effects of Kv9.1 on the conducting properties of Kv2.1 channels, these channels also have an important non-conducting role, which is to stabilise junctions between the endoplasmic reticulum (ER) and the PM [
19,
20]. Both Kv2.1 and Kv2.2 form micrometre-sized clusters at the PM, which are thought to comprise hundreds of channels [
21,
22,
23,
24,
25,
26,
27]. A clustered distribution for Kv2.1 and Kv2.2 was also recently shown in DRG neurons [
28]. Channels within these clusters interact with ER resident VAMP-associated proteins (VAPs), and this is involved in the stabilisation and remodelling of ER-PM junctions [
29,
30]. This function is independent of the conduction of K
+ [
19] and the channels within clusters are thought to be non-conducting [
21,
31]. ER-PM junctions are sites of lipid and protein transport [
32] and important for Ca
2+ homeostasis [
33,
34,
35]. In a variety of cells, including pancreatic beta cells and peripheral and central neurons, Kv2.1 clusters have been shown to coincide with insertion platforms for the delivery of Kv2.1 and other ion channels to the plasma membrane, a process dependent upon an interaction between Kv2.1 and syntaxin [
32]. Recent studies have also provided evidence for conductance-independent roles for Kv2.1 in regulating Ca
2+ uptake into the ER and in regulating the release of both dense core vesicles and synaptic vesicles [
33,
36,
37]. How modulatory KvS subunits affect Kv2 channel clusters and the dynamics of ER-PM junctions is unknown. A change in these non-conducting properties of Kv2 would be expected to have an important effect on neuronal transmission.
In this study, we set out to test the hypothesis that the two Kv9.1 variants differ in their regulation of Kv2.1 by examining both the conducting and non-conducting of Kv2.1 in the absence of and then in the presence of either Kv9.1Ile or Kv9.1Val. Although retained within the ER when expressed alone, both variants trafficked with Kv2.1 and Kv2.2 to the PM and co-localised within surface clusters. They produced similar hyperpolarising shifts in the voltage-dependence of Kv2.1 channel activation and inactivation. They decreased Kv2.1 PM expression, and this effect was more pronounced for Kv9.1Val compared to Kv9.1Ile in both HeLa cells and neurons. These results suggest that the link between Kv9.1Val and pain is the inhibition of Kv2.1 PM expression, which is consistent with the downregulation of Kv2 in pain models [
5].
2. Materials and Methods
2.1. Ethics
C57Bl/6J mice were maintained under conventional housing conditions and a 12–12 light–dark cycle. The neonatal mice (postnatal age 0–2 days) used for the experiments were culled by an appropriate Schedule 1 procedure (cervical dislocation) in accordance with the Animals Scientific Procedures Act 1986 amendment regulations 2012. Schedule 1 training of the experimenters was overseen and approved by the local Named Training and Competency Officer (NTCO). Experiments were reviewed a priori by the Animal Welfare Ethical Review Body at the University of Sussex.
2.2. HeLa Cell Culture and Transfection
Human cervical carcinoma HeLa cells (obtained from Merck, Dorset, UK, 3021013) were cultured and maintained in Dulbecco’s Modified Eagle Medium (DMEM)/F12 (1:1) (Gibco, Paisley, Scotland, 21331-020) supplemented with 1% GlutaMax (Gibco, Paisley, Scotland, 35050-038), 10% fetal bovine serum (FBS) (Merck, Dorset, UK, 9665), and 1% penicillin/streptomycin (P/S) (Gibco, Paisley, Scotland, 15140122) in 5% CO2 at 37 °C. Cells were seeded on coverslips precoated with collagen (Merck, Dorset, UK, 125-50) and grown to a confluency of 40–60%. Cells were transiently transfected 24 h post plating with 1–3 µg plasmids using TransIT-LT1 (Mirus bio, Madison, WI, USA, MIR 2304). Experiments were conducted 48 h post transfection.
2.3. Culture and Transfection of Mouse Hippocampal Neurons
To culture hippocampal neurons, 3 to 4 pups of mouse C57BL/6 of either sex on postnatal days 1 to 2 were used to plate 6 wells of a 12-well plate. Briefly, CA1 to CA3 regions with the dentate gyri were dissected in 1×Hank’s Balanced Salt Solution (HBSS) (Gibco, Paisley, Scotland, 14155048) containing 1% P/S and mechanically dissociated by gently pipetting up and down in a plating medium until a homogenous mixture was obtained. The plating media consisted of Minimum Essential Media (MEM) (Gibco, Paisley, Scotland, 51200087) supplemented with 20 mM D-(+)-Glucose (Merck, Dorset, UK, 24895335), 1% P/S, 1% sodium pyruvate, HEPES (Merck, Dorset, UK, H0887), 1×N2 (Gibco, Paisley, Scotland, 17502048), and 10% heat-inactivated horse serum (Gibco, Paisley, Scotland, 26050-088). The mixture was further diluted with the plating media before dispensing 0.5 mL onto 16 mm coverslips pre-coated with poly-D-lysine (50 µg/mL) (Gibco, Paisley, Scotland, A38904-01) and laminin (20 µg/mL) (Merck, Dorset, UK, L2020). Cells were incubated for 2 to 3 h in 5% CO
2 at 37 °C before adding 2 mL of neurobasal A (Gibco, Paisley, Scotland, 1249015) supplemented with 1×B27 (Gibco, Paisley, Scotland, 11530536), 1% P/S, and 0.5 mM GlutaMAX. Cultures were treated with 3.25 µM of AraC at 4 to 5 days in vitro (DIV). DNA transfection using Ca
2+ phosphate (Promega, Southampton, UK, E1200) was performed on cultures aged 6 to 7 DIV following a modified protocol described previously (Jiang, M. and Chen, G. 2006 [
38]). In our approach, 50 µL of 2×HBS (HEPES buffered saline) and a combined 50 µL solution containing 5 µL of 2 M CaCl
2, DNA, and H
2O were employed. Transfected neurons were imaged 48–72 h post-transfection. A minimum of three independent cultures were used to repeat experiments to ensure reproducibility.
2.4. HEK293 Cell Culture and Transfection for Electrophysiology and Western Blot
Human kidney embryonic cells (HEK293; a gift from Dr Mark O’Driscoll’s research laboratory at the University of Sussex) were cultured in high-glucose DMEM (ThermoFisher Scientific, Cambridge, UK, 41966-029), supplemented with 1% P/S (Merck, Dorset, UK, P4333), and 10% tet-free FBS (Biosera, Cholet, France, FB1001T). Cells were passaged twice a week and maintained in 5% CO2 at 37 °C.
For patch clamp experiments, HEK293 cells were transiently transfected with wild type or mutant human Kv2.1 and human Kv9.1 inserted into the pCDNA5 vector and with EGFP (pMax-EGFP) (Lonza, Slough, UK, VPA-1002) as a transfection marker using the GeneJammer transfection reagent (Agilent Technology, Cambridge, UK, 204130) according to the manufacturer’s instructions. Then, 24 h post transfection (Day 1), HEK293 cells were trypsinised (Gibco, Paisley, Scotland, 253300) and reseeded on poly-D-lysine-coated coverslips (0.1 mg/mL) (Merck, Dorset, UK, 253300) (ThermoFisher Scientific, Cambridge, UK, 11708701) and used for the electrophysiological experiments 48–72 h post-transfection. Only eGFP-positive cells were recorded during electrophysiology studies.
For the Western blot experiments, HEK293 cells were cultured in the normal way, plated in a 6-well plate and transfected 24 h post plating with 2 µg DNA using 2 μL of Lipofectamine 2000 (ThermoFisher Scientific, Cambridge, UK, 11668027) per well.
2.5. Preparation of Plasmid Constructs
Human Kv2.1 (GeneCards;
KCNB1 (858aa); NCBI Gene: 3745, OMIM
®®: 600397, UniProtKB/Swiss-Prot: Q14721); Human Kv9.1 (GeneCards;
KCNS1 (526aa); NCBI Gene (3787), OMIM
®®: 602905, UniProtKB/Swiss-Prot: Q96KK3); and Human Kv2.2 (GeneCards;
KCNB2 (911aa); NCBI Gene: 3745, OMIM
®®: 600397, UniProtKB/Swiss-Prot: Q14721) were cloned in the mammalian expression vector pcDNA5, obtained as a gift from our colleague Dr Owen S. Wells, of the Sussex Genome Centre (pcDNA™5/FRT Mammalian Expression Vector) (ThermoFisher Scientific, Cambridge, UK, V601020). EGFP-tagged human Kv2.1 in pEGFP-C1 was obtained from Addgene (Watertown, MA, USA, 111538) and underwent several modifications. A glycine-rich flexible linker (GGGGSx2) was introduced between EGFP and Kv2.1 through polymerase chain reaction (PCR) amplification. The resulting PCR product was then blunt-end ligated using KLD mix (New England Biolabs, Herts, UK, M0554S). A stop codon was added at the end of the Kv2.1 sequence, and a point mutation, Pro129Leu, was introduced to match the sequence of Uniprot (Q14721). The following clones, including FusionRed-Kv2.1, EGFP-Kv2.2, mCherry-Kv9.1(Ile), FusionRed-Kv9.1(Ile), and concatemers, were constructed by Gibson assembly cloning using NEBuilder HiFi DNA Assembly Master Mix (New England Biolabs, Herts, UK, MSS20A) according to the manufacturer’s instructions. All PCRs were performed using the Q5 High-Fidelity Polymerase (New England Biolabs, Herts, UK, M0491S). In brief, FusionRed-Kv2.1 was constructed by replacing the EGFP of the EGFP-Kv2.1 plasmid with FusionRed. EGFP-Kv2.2 was generated by inserting EGFP with the linker sequence at the N terminus of Kv2.2 in pcDNA5. FusionRed-Kv9.1(Ile) and mCherry-Kv9.1(Ile) were made by subcloning both FusionRed and mCherry at the N terminus of Kv9.1 in pcDNA5, respectively. Concatemers were generated by the sequential insertion of individual subunits into Kv2.1 in pEGFP-C1 after removing EGFP. Briefly, EGFP was replaced by Kv9.1 and Kv2.1 in order to make the concatemers Kv9.1-Kv2.1 and Kv2.1-Kv2.1, respectively. The concatemer Kv9.1-Kv2.1-Kv2.1-Kv2.1 was created by subcloning Kv2.1-Kv2.1 downstream of Kv9.1-Kv2.1. The stop codons in between subunits were removed, and the adjacent subunits were segregated by the linker GGGGS×2. The Myc-Kv9.1 clone was created by inserting the Myc tag and linker GGGGS×2 upstream of Kv9.1 in pcDNA5. To generate HA-Kv2.1 and HA-Kv9.1, a single copy of the hemagglutinin (HA) epitope sequence YPYDVPDYA was inserted within the first extracellular domain after glycine 221 and 260, respectively [
22]. For both constructs, another glycine was inserted after the HA sequence. The VAPA-EGFP construct was obtained from Addgene (Watertown, MA, USA, 18874). All mutants in this study, including the single nucleotide polymorphism Ile489Val of Kv9.1, Kv9.1(G423S)-Kv2.1, Kv9.1-Kv2.1(G379S) and Kv9.1(G423S) were generated by PCR amplification using either the GeneART (ThermoFisher Scientific, Cambridge, UK, A13310) or the Q5 site-directed mutagenesis kit (New England Biolabs, Herts, UK, M0554S) and mutant primers. Primers, ordered from Merck (Dorset, UK) and used to generate the mutations in this study are listed in
Table 1. DNA sequencing by Eurofins Genomics (Ebersberg, Germany) was employed to verify the presence of the desired modification and to ensure the accuracy of the final sequence.
2.6. Live Cell Confocal Imaging
For confocal imaging, a coverslip with live cells was mounted into the imaging chamber using the P4 platform and RC-25 chamber (Warner Instruments, Holliston, MA, USA). Cells were incubated in HBSS and imaged at room temperature with a 63×/oil objective and a Leica SP8 confocal microscope using excitation and emission settings as follows: EGFP and Alexa Fluor 488 were both excited with a 488 nm Argona laser, and emission light was detected between 500 and 550 nm. DsRed was excited with a 561 nm DPSS laser, and emission was collected between 580 and 620 nm. FusionRed and mCherry were excited with a 561 nm DPSS laser, and emission was captured between 600 and 640 nm. Far Red 647 was excited with a 633 nm He/Ne laser, and the emission detection range was set between 660 and 700 nm.
2.7. Immunostaining and Confocal Imaging
The detection of the cell surface HA-Kv2.1 was performed by incubating live cells for 1 h at 37 °C with anti-HA antibodies (Biolegend, London, UK, 901501) diluted in conditioned media (media previously incubated with cells) at a final concentration of 5 µg/mL. Following antibody incubation, cells were washed twice with prewarmed 1× phosphate buffered saline (PBS) and then fixed with 4% paraformaldehyde. After fixation, cells were washed three times with PBS and maintained in PBS until the secondary antibody application. Alexa Fluor 448 (ThermoFisher Scientific, Cambridge, UK, A11029) or 647 (ThermoFisher Scientific, Cambridge, UK, A21235) conjugated goat anti-mouse IgG were used for secondary detection. Cells were incubated with the secondary antibodies for 1 h at room temperature at a final concentration of 4 µg/mL, followed by three washes with PBS. For imaging, covers lips were mounted either onto microscope slides in Fluoroshield (Merck, Dorset, UK, F6057) or into the imaging chamber (P4 platform and RC-25) and covered in PBS. The fluorescence signal was detected using a Leica SP8 confocal microscope. Gain and laser intensity were kept constant across all groups and experiments to ensure comparable intensity readings and enable quantitative analysis. To avoid potential bias, images used for analysis were randomly selected from different fields of view for each condition.
2.8. Image and Statistical Analysis
The analysis of all fluorescence images was carried out using Fiji (1.53i). To measure the surface expression of HA-Kv2.1 in HeLa cells from confocal images, the background was subtracted, and then an ROI was drawn immediately around the cell, and the integrated density was measured per cell. The analysis of confocal images from hippocampal neurons was carried out in a similar way, but this time the ROI was drawn around the soma only. Clusters of HA-Kv2.1 smaller than 0.1 µm2 were excluded from the analysis of the mean cluster size.
GraphPad Prism 8.0.2 (GraphPad Software) was used for all statistical analyses of imaging data. Data were log-transformed for a normal distribution. Nested one-way ANOVA was used to compare the groups, followed by Tukey’s analysis for the multiple comparisons test. A nested t-test was used to compare the total fluorescence intensity of Kv9.1 variants. Data are presented as mean values ± SEM or with a 95% CI. A p value of less than 0.05 was considered statistically significant. Data from HeLa cells were obtained from three independent cultured passages, each derived from separate thawings of the parental cell line, while data from neurons were derived from three independent isolation procedures.
Co-localisation analysis was performed in neurons co-transfected with EGFP-Kv2.1 and mCherry-Kv9.1(Ile) or mCherry-Kv9.1(Val). Images were acquired at a resolution of 1024 × 1024 pixels, with a pixel size of 0.2 × 0.2 µm2. Using Fiji (1.53i), ROIs were drawn in the soma, and the Pearson’s correlation coefficient was measured using the JCaOP plugin. This method evaluates the correlation of intensity distributions between the two channels based on the degree of signal overlap on a pixel-by-pixel basis. A nested t-test was used to compare the PC between the Kv9.1 variants colocalised with Kv2.1.
2.9. Patch-Clamp Electrophysiology
Current recordings were obtained in the whole cell configuration at room temperature (20−23 °C) with an Axopatch−200B amplifier (Axon Instruments, Union City, CA, USA). The current recordings were low−pass filtered through a Bessel filter at 1 kHz, sampled at 1–10 kHz with a Digidata 1550B data acquisition system (Axon™ Digidata®® 1550B Low Noise Data Acquisition System) (Axon Instruments, Union City, CA, USA), and online series resistance compensation was performed. Data storage and command voltages were controlled with the pClamp10.7 software (Axon Instruments, Union City, CA, USA). Online leak current subtraction was carried out with leak currents recorded as a fraction of the current evoked on the opposite polarity. Pipettes were pulled using a P-97 Flaming/Brown Micropipette Puller (Sutter Instruments, Novato, CA, USA) from borosilicate glass capillaries (Warner Instruments, Holliston, MA, USA) and afterward heat polished to obtain patch pipettes with a resistance between 2.5–5 MΩ. The patch pipettes were filled with an intracellular solution (ICS) containing 60 mM KCl, 20 mM KF, 60 mM K-gluconate 1 mM Mg-ATP, 10 mM EGTA, 1.5 mM MgCl2, 1 mM CaCl2, and 10 mM HEPES, and adjusted to pH 7.32 with KOH (adjusted to 320 mosm). Pipette solutions were prepared in batches, aliquoted, and stored at −20 °C until the day of use. All solutions were equilibrated at room temperature before the experiments were performed. Transfected HEK93 cells were continuously perfused with an extracellular solution (ECS) containing 140 mM NaCl, 5 mM KCl, 2 mM MgCl2, 2 mM CaCl2, 10 mM HEPES, and 10 mM D-glucose, and adjusted to pH 7.35 with NaOH (adjusted to 300 mosm). Junction potentials between the ICS and ECS were zeroed with the filled pipette in the bath solution. A stock solution of A769662 (MedChemExpress, Cambridge, UK, HY-50662) was made in 100% dimethyl sulfoxide (DMSO) and stored at −20 °C until the day of the experiment. The desired working concentrations of A769662 were made by diluting these stock solutions in ECS solution with a final DMSO concentration of 0.3% and were applied to the bath using a fast perfusion system (RSC200 Rapid Perfusion system and EVH-9 rapid valve system) (BioLogic Science Instruments, Seyssinet-Pariset, France). The recording chamber was grounded directly by an Ag/AgCl pellet. All the chemicals and reagents were purchased from Merck, Dorset, UK.
Voltage protocols were generated using pCLAMP 10.7 software (Axon Instruments, Union City, CA, USA). To generate current families, the voltage was stepped from a holding potential of −90 mV to between −80 mV and +80 in 10 mV steps for either 300 ms or 3000 ms, and this was applied every 10 s (0.1 Hz). Tail currents were measured by stepping back to −40 mV. To measure steady-state inactivation, the voltage was stepped for 30 s from between −80 mV and +25 mV in 15 mV steps. A 300 ms test pulse to +50 mV was applied immediately before and after this, and the peak amplitudes of the currents were compared.
2.10. Analysis of Patch Clamp Data
The voltage dependence of activation and inactivation was fitted with a single Boltzmann function according to y = 1/(1 + exp (−(V–V1/2)/k)), with V representing the voltage applied, V0.5 the voltage at which 50% of the channels are activated or inactivated, and k the slope factor. The time constants of activation (from −90 to −20 mV) and deactivation (−40 to −90 mV) were obtained by fitting the raw current traces of either the activation or deactivation protocol with a single or double exponential function. Dose−response curves were obtained by plotting y, the fraction of current modulated at −20 mV, as a function of drug concentration, [D], and fitted with the Hill equation: 1 − y = 1/(1 + (EC50/[D])nH), where EC50 is the concentration that generates 50% maximum activation and nH the Hill coefficient. The results are expressed as mean ± S.E.M. GraphPad Prism 10 was used to obtain graphs and perform the statistical analysis. Statistical significance was determined using ordinary one-way ANOVA and Welch ANOVA followed by Dunnett’s multiple comparison test. p < 0.05 was considered significant. Data from HEK293 cells were obtained from at least three independent cultured passages of cells.
2.11. Western Blot
HEK293 cells were harvested 48 h after transfection and lysed in 20 mM HEPES pH 7.5, 20 mM NaCl, 1 mM MgCl2, and 1% Triton X-100 supplemented with a protease inhibitor (Merck, Dorset, UK, 5892791001), and benzonase (Merck, Dorset, UK, E1014-5KU) at 4 °C for 30 min. Lysates were centrifuged at 13000×
g for 10 min, and protein concentrations were measured using a BCA assay (ThermoFisher Scientific, Cambridge, UK, 23225) with bovine serum albumin (BSA) as standard. Then, 30 μg of total protein in Laemmli buffer was separated on a 4–12% Bis/Tris Gel (ThermoFisher Scientific, Cambridge, UK, NW04125BOX) and transferred to a nitrocellulose membrane. Concatamers were separated on a 3–8% Tris acetate gel (ThermoFisher Scientific, Cambridge, UK, EA03755BOX). The membrane was blocked with 5% BSA in Tris-buffered saline for 1 h at room temperature and probed overnight at 4 °C with anti Kv2.1 antibody (1 in 2000) (Abcam, Cambridge, UK, Ab192761), anti Myc antibody to detect Myc-Kv9.1 (1 in 1000) (Cell Signalling Technology, Danvers, MA, USA, 2276), and GAPDH (1 in 1000) (Cell Signalling Technology, Danvers, MA, USA, 97166). HRP conjugated secondary antibodies (DAKO, Cambridge, UK, P0447 and P0448) were incubated at room temperature for 1 h to detect proteins. All antibody incubations and washes in Tris-buffered saline with Tween (TBS) between incubations were carried out with rotation. Visualisation was with chemiluminescent reagents (Geneflow, Lichfield, UK, K1-0170). Images were acquired and quantified using GE Healthcare Cytiva ImageQuant 4000, normalising for loading differences with GAPDH [
39]. Statistical significance was tested using either a one-way ANOVA with repeated measures or a paired two-tailed
t-test.
2.12. Biotinylation and Streptavidin Pulldown
Cells in a 6-well plate were rinsed twice with ice-cold PBS and transferred to Eppendorf tubes. Cells were incubated with 800 µL of 0.2 mg/mL EZ-Link sulfo-NHS-LC-biotin (ThermoFisher Scientific, Cambridge, UK, A39257) in normal extracellular solution (NES; 140 mM NaCl, 5 mM KCl, 2 mM CaCl2, 1 mM MgCl2, 10 mM D-glucose, 10 mM HEPES, pH 7.3) with rotation for 1 h at 4 °C. Cells were spun for 5 min at 500× g and biotin solution was removed; non-reactive biotin was quenched by incubating cells with stock buffer (25 mM Tris-HCl, 150 mM NaCl, 10 mM EDTA, pH 7.5) for 5 min at 4 °C. Cells were washed twice with stock buffer, spinning between washes, then solubilised in 150 µL solubilisation buffer (stock buffer, 1% Triton X-100, 1 mM PMSF, protease inhibitor cocktail). Samples were transferred to Eppendorf tubes and rotated for 30 min at 4 °C, then centrifuged at 16,000× g. A 30 µL aliquot of the supernatant was diluted in 4× Laemmli sample buffer and stored at −20 °C as the ‘total’ protein sample, while the remaining supernatant was added to 30 µL of washed Pierce Streptavidin UltraLink Resin (ThermoFisher Scientific, Cambridge, UK, 53113) and rotated for 2 h at 4 °C. Resin was centrifuged at 500× g and washed in stock buffer with 1% Triton four times to remove any unbound protein. Proteins were eluted by the addition of 40 µL 1× Laemmli sample buffer and stored at −20 °C. Protein was separated as above with 4 μL of total and 8 μL of biotinylated sample per well.
4. Discussion
Mouse and human genetic evidence links the sensory neuron Kv2.1 and Kv9.1 channels to chronic pain sensitivity [
1,
5,
10,
11,
13,
14], but the underlying mechanisms remain unclear because Kv2.1 has important non-conducting as well as conducting properties [
19,
20,
29] and Kv9.1 acts as a modulatory subunit with Kv2.1 and Kv2.2 but does not function alone [
8]. Validation of these channels as targets for new analgesics requires an improved understanding of how the human variants of Kv9.1 affect Kv2 channel behaviour. Here, we show that both variants of Kv9.1 can assemble with Kv2.1 subunits and locate within surface clusters, but they both act to reduce the surface expression of Kv2.1 and to reduce the size of channel clusters. Both variants altered the biophysical properties of Kv2.1-mediated currents in a similar way, producing a reduction in the peak current density and equivalent hyperpolarising shifts in the voltage dependence of channel activation and inactivation. The suppression of Kv2.1 PM expression was more pronounced for Kv9.1Val compared to Kv9.1Ile in both HeLa cells and hippocampal neurons suggesting that the link between Kv9.1Val and pain is the inhibition of Kv2 PM expression, consistent with reports of downregulation of Kv2.1 in pain models [
5].
For the Kv9.1 variants, their suppression of Kv2.1 PM expression was manifested by a reduction in the peak current density along with a reduction in the size of channel clusters. For Kv2.1 channels, a linear relationship between PM expression and current density is not expected, with previous studies showing that only a small proportion of PM Kv2.1 channels conduct K
+ and that this is also dependent upon channel clustering, with enhanced clustering reducing conduction [
31]. The major impact of reducing levels of Kv2 within PM clusters might therefore be upon the structure and function of Kv2-stabilised ER-PM junctions. Given the established role of these junctions in Ca
2+ homeostatic mechanisms, vesicle secretion, and delivery of ion channels to the cell surface [
32,
33,
36,
37], any change in junction stability is expected to impact the transmission of signals from the peripheral pain-sensing neurons.
Our results with the dimer concatamers, showing an inhibition of expression and function combined with the hyperpolarising shift in the voltage dependence of activation upon substituting Kv9.1 for the first Kv2.1 subunit within the dimer, support our findings from co-expression studies and suggest that these are of physiological relevance. The fact that individually expressed subunits behaved similarly to the linked subunits suggests that both variants of Kv9.1 readily associate with Kv2.1 to suppress the number of functional channels at the cell surface. If Kv2.1 subunits displayed a much greater tendency to associate with other Kv2.1 rather than Kv9.1, then we would expect that linking the subunits within the dimer would alter how Kv9.1 affected Kv2.1. channel behaviour. The low PM expression of these complexes suggests either a greater tendency for misfolding and/or the misassembly of 9.1–2.1 heteromers with a 2:2 stoichiometry or greater ER retention of these complexes versus the homotetramers. Our findings with the 9.1–3×(2.1) tetramer need to be interpreted with caution because we did not compare them alongside other tetramers; however, they suggest that the formation of heteromers with a 1:3 ratio of Kv9.1 to Kv2.1 is permitted and that they traffic more efficiently to the PM compared to complexes with a 2:2 ratio. Other studies have also reported that for KvS-Kv2 channels expressed at the PM, the preferred stoichiometry is 1:3 ratio [
15,
16]. This was shown, for example, for Kv2.1-Kv9.3 channels using FRET analysis [
15], and Pisupati et al. reached a similar conclusion for Kv2.1-Kv6.4 channels by measuring the bleaching of GFP-tagged Kv subunits [
16]. By contrast, Moller et al. [
17] also examined the bleaching of GFP-tagged subunits and combined this with the analysis of dimeric and tetrameric concatemers, and concluded that the preferred stoichiometry of Kv2.1–Kv6.4 complexes was 2:2, although 3 Kv2.1 with 1 Kv6.4 was also permitted.
Several of the KvS subunits have been shown to contribute to physiological and pathophysiological processes, and they share in common their ability to produce a hyperpolarising shift in the voltage dependence of Kv2.1 channel activation and inactivation and to reduce the current density [
8,
42,
43,
44,
45,
46]. The impact of these changes will be dependent upon the firing properties of the cell, with the shift in voltage dependence of channel activation expected to reduce firing frequency and action potential width, whereas the effects on steady-state inactivation and current density are expected to have the opposite effect [
6,
47]. For the Kv6.4 SNP associated with altered pain sensitivity in human labour, the amino acid substitution within the selectivity filter of the pore disrupts its ability to form a complex with Kv2.1 and reach the PM [
13]. Therefore, its modulatory impact upon Kv2.1 channel currents is lost, resulting in a decrease in the firing frequency of sensory neurons, which leads to reduced pain sensitivity. For Kv9.1Ile and Val variants, both were able to traffic from the ER to the PM when co-expressed with Kv2.1 or Kv2.2, and they altered the biophysical properties of Kv2.1 currents in a similar way. The Ile489Val substitution occurs within the middle of the cytoplasmic C-terminal region of Kv9.1 and relatively little is known about how this region affects channel properties. Interestingly, although the key determinant of subfamily-specific assembly of Kv channels is the N-terminal tetramerization domain, for Kv2.1 and Kv6.4 heteromultimers, their subfamily-specific co-assembly was shown to also be dependent upon an interaction between the N-terminus of Kv2.1 and the C-terminus of Kv6.4 [
48]. Another KvS subunit that contributes to a pathological process, but this time in mice, is Kv8.2. The Kv8.2 variant with H205 and R252 substituted for R205 and Q252 is associated with an epilepsy phenotype, but both variants form heteromeric assemblies with Kv2.1 and exhibit only minor differences in the heteromeric channel currents, which does not explain the severity of the phenotype [
49,
50]. The key difference between the two variants appears to be their expression levels within the hippocampus. With mRNA levels for the Kv8.2H205, R252 variant found to be threefold higher, it is thought that this produces an enhanced suppression of the Kv2.1 current density, resulting in increased neuronal firing frequency. Whether or not there are similar differences in the expression of Kv9.1Val versus Kv9.1Ile in human DRG neurons that contribute to the altered activity of these neurons remains to be established.