Comparative Analysis of Rescue-In Vitro-Maturation (r-IVM) Outcomes in Women with Diminished Ovarian Reserve (DOR) Versus Normal Ovarian Reserve (NOR)
Abstract
1. Introduction
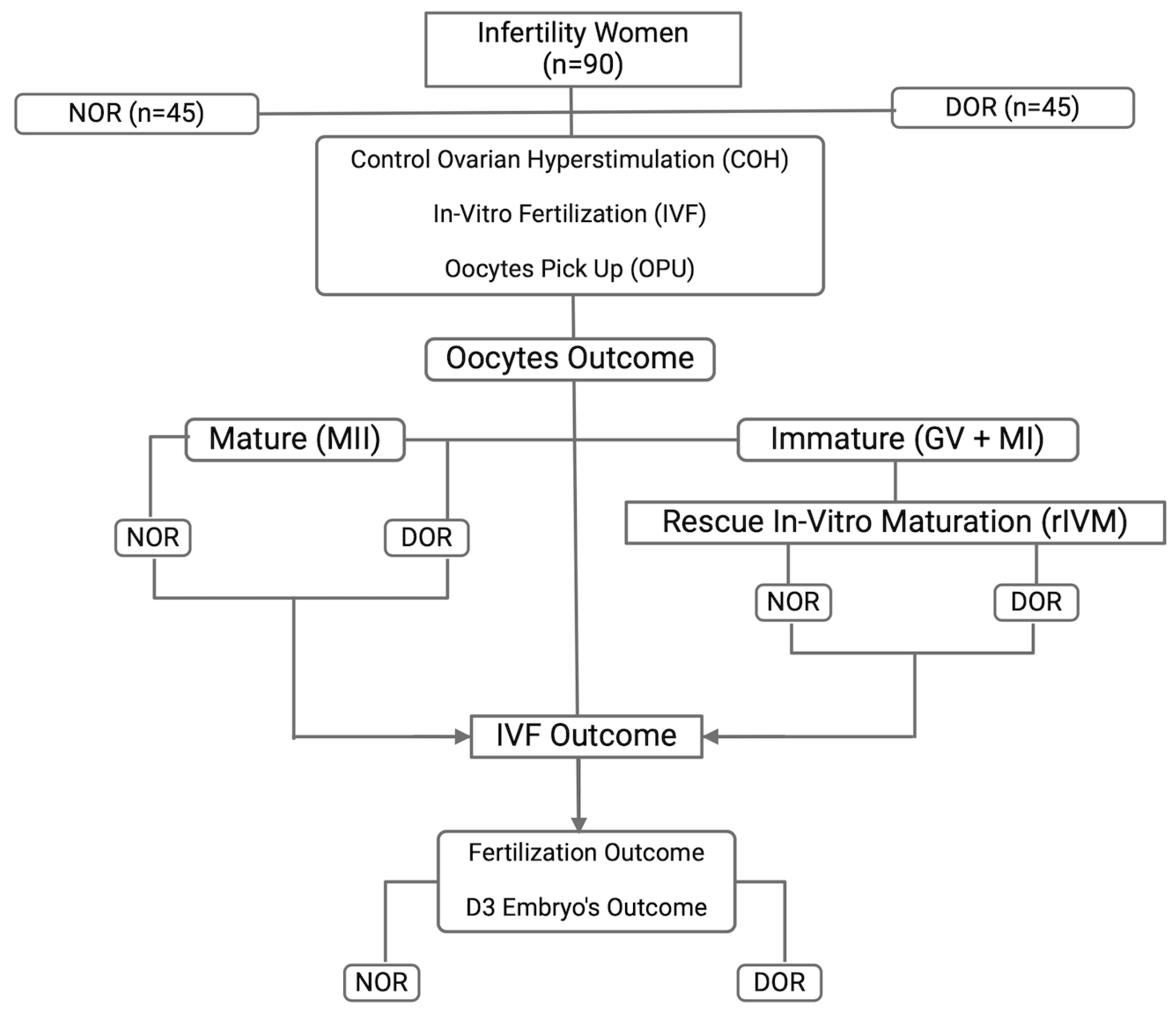
2. Materials and Methods
2.1. Study Design
2.2. COS, r-IVM, and IVF Protocols
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ART | Artificial Reproductive Technique |
| cAMP | Cyclic Adenosine Monophosphate |
| COC | Cumulus-oocyte Complexes |
| DOR | Diminished Ovarian Reserve |
| FSH | Follicular Stimulating Hormone |
| GnRH | Gonadotrophin Releasing Hormone |
| GV | Germinal Vesicle |
| GVBD | Germinal Vesicle Breakdown |
| hCG | Human Chorionic Gonadotrophin |
| ICSI | Intra Cytoplasmic Sperm Injection |
| IVM | In Vitro Maturation |
| IQR | Interquartile Range |
| LH | Luteinizing Hormone |
| M1 | Meiosis 1 |
| MII | Meiosis II |
| OHSS | Ovarian Hyperstimulation Syndrome |
| OMR | Oocyte Maturation Rate |
| OTO-IVM | Ovarian Tissue Oocyte In Vitro Maturation |
| PB1 | First Polar Body |
| PCOS | Polycystic Ovarian Syndrome |
| rIVM | Rescue IVM |
| 2PN | 2 Pronuclei |
References
- Kawwass, J.F.; Hipp, H.S.; Session, D.R.; Kissin, D.M.; Jamieson, D.J.; National ART Surveillance System Group. Severity of Diminished Ovarian Reserve and Chance of Success with Assisted Reproductive Technology. J. Reprod. Med. 2017, 62, 153–160. [Google Scholar] [PubMed]
- Ozelci, R.; Aldemir, O.; Dilbaz, S.; Ozkaya, E.; Kahyaoglu, I.; Dilbaz, B.; Moraloglu Tekin, O. The impact of different etiologies of diminished ovarian reserve on pregnancy outcome in IVF-ET cycles. Turk. J. Med. Sci. 2019, 49, 1138–1144. [Google Scholar] [CrossRef] [PubMed]
- Kesharwani, D.K.; Mohammad, S.; Acharya, N.; Joshi, K.S. Fertility With Early Reduction of Ovarian Reserve. Cureus 2022, 14, e30326. [Google Scholar] [CrossRef] [PubMed]
- Ferraretti, A.P.; La Marca, A.; Fauser, B.C.; Tarlatzis, B.; Nargund, G.; Gianaroli, L.; ESHRE Working Group on Poor Ovarian Response Definition. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: The Bologna criteria. Hum. Reprod. 2011, 26, 1616–1624. [Google Scholar] [CrossRef]
- Man, L.; Lustgarten Guahmich, N.; Vyas, N.; Tsai, S.; Arazi, L.; Lilienthal, D.; Schattman, G.; Rosenwaks, Z.; James, D. Ovarian Reserve Disorders, Can We Prevent Them? A Review. Int. J. Mol. Sci. 2022, 23, 15426. [Google Scholar] [CrossRef]
- Ulrich, N.D.; Marsh, E.E. Ovarian Reserve Testing: A Review of the Options, Their Applications, and Their Limitations. Clin. Obstet. Gynecol. 2019, 62, 228–237. [Google Scholar] [CrossRef]
- de Souza, E.B.; Marin, D.D.; Ramos, A.S.; Homobono, B.P.; Ramos, P.; de Brito, V.C.; da Cruz, G.S.; da Costa, N.N.; Cordeiro, M.D.S.; Santos, S. Use of platelet-rich plasma on in vitro maturation during bovine embryo production. Anim. Reprod. 2024, 21, e20230107. [Google Scholar] [CrossRef]
- Yu, T.N.; Chen, M.J.; Lee, T.H.; Chen, Y.C.; Cheng, E.H.; Huang, C.C.; Chen, C.I.; Lee, C.I.; Lee, M.S.; Lin, P.Y. Intraovarian platelet-rich plasma injection significantly improves blastocyst yield and quality in IVF patients. Sci. Rep. 2025, 15, 1301. [Google Scholar] [CrossRef]
- Lin, Y.; Xie, B.; Li, X.; Li, R.; Ma, C.; Zhu, J.; Qiao, J. Supplementation of the In Vitro Maturation Culture Medium of Mouse Oocytes with Growth Hormone Improves Pregnancy Outcomes. Reprod. Sci. 2021, 28, 2540–2549. [Google Scholar] [CrossRef]
- Magon, N.; Agrawal, S.; Malik, S.; Babu, K.M. Growth hormone in the management of female infertility. Indian J. Endocrinol. Metab. 2011, 15 (Suppl. 3), S246–S247. [Google Scholar] [CrossRef]
- Das, M.; Son, W.Y.; Buckett, W.; Tulandi, T.; Holzer, H. In-vitro maturation versus IVF with GnRH antagonist for women with polycystic ovary syndrome: Treatment outcome and rates of ovarian hyperstimulation syndrome. Reprod. Biomed. Online 2014, 29, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Kotlyar, A.M.; Seifer, D.B. Women with PCOS who undergo IVF: A comprehensive review of therapeutic strategies for successful outcomes. Reprod. Biol. Endocrinol. 2023, 21, 70. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Xu, B.; Sun, Y.; Lu, X.; Niu, Z.; Chen, Q.; Feng, Y.; Xu, C. The effect of human cumulus cells on the maturation and developmental potential of immature oocytes in ICSI cycles. J. Assist. Reprod. Genet. 2012, 29, 313–319. [Google Scholar] [CrossRef]
- Tharasanit, T.; Thuwanut, P. Oocyte Cryopreservation in Domestic Animals and Humans: Principles, Techniques and Updated Outcomes. Animals 2021, 11, 2949. [Google Scholar] [CrossRef]
- Oktay, K.; Buyuk, E.; Rodriguez-Wallberg, K.A.; Sahin, G. In vitro maturation improves oocyte or embryo cryopreservation outcome in breast cancer patients undergoing ovarian stimulation for fertility preservation. Reprod. Biomed. Online 2010, 20, 634–638. [Google Scholar] [CrossRef]
- Lee, H.J.; Jee, B.C.; Suh, C.S.; Kim, S.H.; Moon, S.Y. Oocyte maturity in relation to woman’s age in in vitro fertilization cycles stimulated by single regimen. Yonsei Med. J. 2012, 53, 181–185. [Google Scholar] [CrossRef]
- Levi-Setti, P.E.; Zerbetto, I.; Baggiani, A.; Zannoni, E.; Sacchi, L.; Smeraldi, A.; Morenghi, E.; De Cesare, R.; Drovanti, A.; Santi, D. An Observational Retrospective Cohort Trial on 4,828 IVF Cycles Evaluating Different Low Prognosis Patients Following the POSEIDON Criteria. Front. Endocrinol. 2019, 10, 282. [Google Scholar] [CrossRef]
- Chian, R.C.; Li, J.H.; Lim, J.H.; Yoshida, H. IVM of human immature oocytes for infertility treatment and fertility preservation. Reprod. Med. Biol. 2023, 22, e12524. [Google Scholar] [CrossRef]
- Das, M.; Son, W.Y. In vitro maturation (IVM) of human immature oocytes: Is it still relevant? Reprod. Biol. Endocrinol. 2023, 21, 110. [Google Scholar] [CrossRef]
- Ahmad, M.F.; Elias, M.H.; Mat Jin, N.; Abu, M.A.; Syafruddin, S.E.; Zainuddin, A.A.; Suzuki, N.; Abdul Karim, A.K. The spectrum of in vitro maturation in clinical practice: The current insight. Front. Endocrinol. 2023, 14, 1192180. [Google Scholar] [CrossRef]
- Lee, H.J.; Barad, D.H.; Kushnir, V.A.; Shohat-Tal, A.; Lazzaroni-Tealdi, E.; Wu, Y.G.; Gleicher, N. Rescue in vitro maturation (IVM) of immature oocytes in stimulated cycles in women with low functional ovarian reserve (LFOR). Endocrine 2016, 52, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Tang-Pedersen, M.; Westergaard, L.G.; Erb, K.; Mikkelsen, A.L. Combination of IVF and IVM in naturally cycling women. Reprod. Biomed. Online 2012, 24, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, C.; Darmon, S.; Patrizio, P.; Albertini, D.F.; Barad, D.H.; Gleicher, N. Changing clinical significance of oocyte maturity grades with advancing female age advances precision medicine in IVF. iScience 2023, 26, 107308. [Google Scholar] [CrossRef]
- Yang, J.; Gao, J.; Wang, Y.; Liu, H.; Lian, X. Impact of follicular size categories on oocyte quality at trigger day in young and advanced-age patients undergoing GnRH-ant therapy. Front. Endocrinol. 2023, 14, 1167395. [Google Scholar] [CrossRef]
- Gilchrist, R.B.; Smitz, J. Oocyte in vitro maturation: Physiological basis and application to clinical practice. Fertil. Steril. 2023, 119, 524–539. [Google Scholar] [CrossRef]
- Sanchez, F.; Le, A.H.; Ho, V.N.A.; Romero, S.; Van Ranst, H.; De Vos, M.; Gilchrist, R.B.; Ho, T.M.; Vuong, L.N.; Smitz, J. Biphasic in vitro maturation (CAPA-IVM) specifically improves the developmental capacity of oocytes from small antral follicles. J. Assist. Reprod. Genet. 2019, 36, 2135–2144. [Google Scholar] [CrossRef]
- Wang, X.; Wang, L.; Xiang, W. Mechanisms of ovarian aging in women: A review. J. Ovarian Res. 2023, 16, 67. [Google Scholar] [CrossRef]
- Abbara, A.; Clarke, S.A.; Dhillo, W.S. Novel Concepts for Inducing Final Oocyte Maturation in In Vitro Fertilization Treatment. Endocr. Rev. 2018, 39, 593–628. [Google Scholar] [CrossRef]
- Wei, J.; Luo, Z.; Dong, X.; Jin, H.; Zhu, L.; Ai, J. Cut-off point of mature oocyte for routine clinical application of rescue IVM: A retrospective cohort study. J. Ovarian Res. 2023, 16, 226. [Google Scholar] [CrossRef]
- Zhu, Q.; Li, Y.; Ma, J.; Ma, H.; Liang, X. Potential factors result in diminished ovarian reserve: A comprehensive review. J. Ovarian Res. 2023, 16, 208. [Google Scholar] [CrossRef]
- Esencan, E.; Beroukhim, G.; Seifer, D.B. Age-related changes in Folliculogenesis and potential modifiers to improve fertility outcomes—A narrative review. Reprod. Biol. Endocrinol. 2022, 20, 156. [Google Scholar] [CrossRef] [PubMed]
- Park, S.U.; Walsh, L.; Berkowitz, K.M. Mechanisms of ovarian aging. Reproduction 2021, 162, R19–R33. [Google Scholar] [CrossRef] [PubMed]
- Ju, W.; Zhao, Y.; Yu, Y.; Zhao, S.; Xiang, S.; Lian, F. Mechanisms of mitochondrial dysfunction in ovarian aging and potential interventions. Front. Endocrinol. 2024, 15, 1361289. [Google Scholar] [CrossRef]
- Weissman, A.; Horowitz, E.; Ravhon, A.; Steinfeld, Z.; Mutzafi, R.; Golan, A.; Levran, D. Spontaneous ovulation versus HCG triggering for timing natural-cycle frozen-thawed embryo transfer: A randomized study. Reprod. Biomed. Online 2011, 23, 484–489. [Google Scholar] [CrossRef]
- Lin, M.H.; Wu, F.S.; Hwu, Y.M.; Lee, R.K.; Li, R.S.; Li, S.H. Dual trigger with gonadotropin releasing hormone agonist and human chorionic gonadotropin significantly improves live birth rate for women with diminished ovarian reserve. Reprod. Biol. Endocrinol. 2019, 17, 7. [Google Scholar] [CrossRef]
- Arroyo, A.; Kim, B.; Yeh, J. Luteinizing Hormone Action in Human Oocyte Maturation and Quality: Signaling Pathways, Regulation, and Clinical Impact. Reprod. Sci. 2020, 27, 1223–1252. [Google Scholar] [CrossRef]
- Gotschel, F.; Sonigo, C.; Becquart, C.; Sellami, I.; Mayeur, A.; Grynberg, M. New Insights on In Vitro Maturation of Oocytes for Fertility Preservation. Int. J. Mol. Sci. 2024, 25, 10605. [Google Scholar] [CrossRef]
- Liu, Y.; Jiang, H.; Du, X.; Huang, J.; Wang, X.; Hu, Y.; Ni, F.; Liu, C. Contribution of rescue in-vitro maturation versus double ovarian stimulation in ovarian stimulation cycles of poor-prognosis women. Reprod. Biomed. Online 2020, 40, 511–517. [Google Scholar] [CrossRef]
- Ahmad, M.F.; Elias, M.H.; Mat Jin, N.; Abu, M.A.; Syafruddin, S.E.; Zainuddin, A.A.; Suzuki, N.; Abdul Karim, A.K. Oocytes Quality Assessment-The Current Insight: A Systematic Review. Biology 2024, 13, 978. [Google Scholar] [CrossRef]
- Baldini, G.M.; Ferri, D.; Malvasi, A.; Lagana, A.S.; Vimercati, A.; Dellino, M.; Baldini, D.; Trojano, G. Genetic Abnormalities of Oocyte Maturation: Mechanisms and Clinical Implications. Int. J. Mol. Sci. 2024, 25, 13002. [Google Scholar] [CrossRef]
- McCoy, C.E. Understanding the Intention-to-treat Principle in Randomized Controlled Trials. West. J. Emerg. Med. 2017, 18, 1075–1078. [Google Scholar] [CrossRef] [PubMed]


| Clinical Characteristic | NOR (Mean, SD) | DOR (Mean, SD) | p-Value |
|---|---|---|---|
| No of cycle | 45 | 45 | - |
| Age | 35.2 (±4.88) | 36.5 (±4.24) | 0.68 |
| Duration of infertility | 6.8 (±4.5) | 7.0 (±4.8) | 0.77 |
| AMH (ng/mL) | 2.47 (±2.3) | 1.08 (±0.5) | 0.035 * |
| AFC | 13.3 (±8.1) | 2.4 (±1.06) | |
| No of follicle aspirated | 932 (11, ±5) | 109 (2, ±1.5) | |
| Retrieved oocyte number | 714 (8, ±3) | 77 (2, ±1) | |
| Follicular oocyte Index (FOI) | 76.6% (±2.8) | 70.6% (±2.1) | 0.54 |
| Causes of Infertility | NOR n, (%) | DOR n, (%) | p-Value |
| Primary | 25 (55.6) | 17 (37.8) | 0.048 * |
| Secondary | 3 (6.7) | 1 (2.2) | 0.38 |
| Male factor | 3 (6.7) | 2 (4.4) | 0.91 |
| PCOS | 8 (17.8) | 0 (0) | 0.002 * |
| Endometriosis | 1 (2.2) | 9 (20.0) | 0.037 * |
| Tubal factor | 3 (6.7) | 1 (2.2) | 0.16 |
| Unexplained | 2 (4.4) | 3 (6.7) | 0.48 |
| Others (Age, Oncofertility) | 0 (0) | 12 (26.7) | 0.001 * |
| Trigger Agent | NOR n, (%) | DOR n, (%) | |
| hCG | 37 (82.2) | 30 (66.7) | - |
| Decapeptide | 8 (17.8) | 0 | |
| Dual trigger | 0 | 15 (33.3) |
| Oocytes Outcome | NOR (n:45) n(%) | DOR (n:45) n(%) | p-Value |
|---|---|---|---|
| No of oocyte retrieved | 714 (100) | 77 (100) | - |
| No of oocyte per patient (mean) | 15.8 | 1.71 | |
| No of MII day 0 | 516 (72.3) | 50 (64.9) | |
| No of MI day 0 | 99 (13.9) | 17 (22) | |
| No of GV day 0 | 57 (7.98) | 3 (3.9) | |
| No of abnormal oocytes | 38 (5.3) | 7 (9.1) | |
| No of matured oocytes in vivo (MII day 1) | 73 (46.8) | 12 (60) | |
| No of matured oocyte (MII day 2) | 1 (0.6) | 0 | |
| No of matured oocytes In vitro (IVM) | 74 (100) | 12 (100) | |
| In vivo maturity rate | 72.3% | 64.94% | 0.074 |
| In vitro maturation rate | 47.4% | 60% | 0.006 * |
| Fertilization Outcome | In Vivo Group | p-Value | In Vitro Group | p-Value | ||
|---|---|---|---|---|---|---|
| NOR n (%) | DOR n (%) | NOR n (%) | DOR n (%) | |||
| No of ICSI | 516 (100) | 50 (100) | p = 0.78 | 74 (100) | 12 (100) | p = 0.042 # |
| No of fertilization (2PN) | 282 (54.7) | 25 (50) | 28 (37.8) | 9 (66.7) | ||
| Fertilization rate | 54.7% | 50% | 37.8% | 66.7% | ||
| Day 3 embryo | 166 (58.9) | 12 (48) | 11 (39.3) | 7 (77.8) | ||
| Embryo Quality Outcome | In Vivo Group | p Value | In Vitro Group | p-Value | ||
|---|---|---|---|---|---|---|
| NOR | DOR | NOR | DOR | |||
| Good | 101 (60.8) | 6 (50.0) | p = 0.76 | 1 (9) | 1 (14.3) | p = 0.033 # |
| Fair | 34 (20.5) | 4 (33.3) | 3 (27.3) | 5 (71.4) | ||
| Poor | 31 (18.7) | 2 (16.7) | 7 (63.6) | 1 (14.3) | ||
| Successful Oocyte Maturation | Simple Logistic Regression | |
|---|---|---|
| OR (95% CI) | p-Value | |
| Age | ||
| <35 years 35–40 years >45 years | 1 1.074 (0.588–1.964) 1.388 (0.672–2.865) | - 0.816 0.375 |
| Factor of infertility | ||
| Unexplained Single factor Two factors | 1 0.6 (0.229–1.571) 0.269 (0.051–1.42) | 0.298 0.122 |
| Ovarian reserve (ng/mL) | ||
| Normal ovarian reserve Diminished ovarian reserve | 1 1.875 (0.880–3.995) | 0.104 |
| Type of trigger | ||
| Dual trigger Decapeptide hCG | 1 1.520 (0.348–6.644) 2.190 (1.197–4.007) | 0.578 0.011 ^ |
| Successful Oocyte Maturation | Multiple Logistic Regression | |
|---|---|---|
| aOR (95% CI) | p-Value | |
| Age <35 years 35–40 years >45 years | 1 1.054 (0.560–1.983) 1.059 (0.482–2.323) | - 0.870 0.887 |
| Factor of infertility Unexplained Single factor Two factors | 1 0.713 (0.264–1.923) 0.306 (0.055–1.696) | 0.504 0.175 |
| Ovarian reserve (ng/mL) Normal ovarian reserve Diminished ovarian reserve | 1 1.845 (0.805–4.229) | 0.148 |
| Type of trigger Dual trigger Decapeptide hCG | 1 1.437 (0.318–6.489) 2.021 (1.085–3.766) | 0.637 0.027 ^ |
| Group | In Vivo (MII) | In Vitro (MII) | NNT | ||
|---|---|---|---|---|---|
| No of Oocyte | No of Embryo | No of Oocyte | No of Embryo | ||
| NOR | 516 | 166 | 74 | 11 | 1:909 |
| DOR | 50 | 12 | 12 | 7 | 1:169 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmad, M.F.; Mohd Nor, N.Y.; Mohammad Ramadneh, M.M.; Roseli, N.I.; Elias, M.H.; Mat Jin, N.; Abu, M.A.; Syafruddin, S.E.; Zainuddin, A.A.; Azhar, S.S.; et al. Comparative Analysis of Rescue-In Vitro-Maturation (r-IVM) Outcomes in Women with Diminished Ovarian Reserve (DOR) Versus Normal Ovarian Reserve (NOR). Biomedicines 2025, 13, 1084. https://doi.org/10.3390/biomedicines13051084
Ahmad MF, Mohd Nor NY, Mohammad Ramadneh MM, Roseli NI, Elias MH, Mat Jin N, Abu MA, Syafruddin SE, Zainuddin AA, Azhar SS, et al. Comparative Analysis of Rescue-In Vitro-Maturation (r-IVM) Outcomes in Women with Diminished Ovarian Reserve (DOR) Versus Normal Ovarian Reserve (NOR). Biomedicines. 2025; 13(5):1084. https://doi.org/10.3390/biomedicines13051084
Chicago/Turabian StyleAhmad, Mohd Faizal, Nurul Yaqin Mohd Nor, Mohammad Mahmoud Mohammad Ramadneh, Nurul Izyani Roseli, Marjanu Hikmah Elias, Norazilah Mat Jin, Muhammad Azrai Abu, Saiful Effendi Syafruddin, Ani Amelia Zainuddin, Shah Shamsul Azhar, and et al. 2025. "Comparative Analysis of Rescue-In Vitro-Maturation (r-IVM) Outcomes in Women with Diminished Ovarian Reserve (DOR) Versus Normal Ovarian Reserve (NOR)" Biomedicines 13, no. 5: 1084. https://doi.org/10.3390/biomedicines13051084
APA StyleAhmad, M. F., Mohd Nor, N. Y., Mohammad Ramadneh, M. M., Roseli, N. I., Elias, M. H., Mat Jin, N., Abu, M. A., Syafruddin, S. E., Zainuddin, A. A., Azhar, S. S., Suzuki, N., & Abdul Karim, A. K. (2025). Comparative Analysis of Rescue-In Vitro-Maturation (r-IVM) Outcomes in Women with Diminished Ovarian Reserve (DOR) Versus Normal Ovarian Reserve (NOR). Biomedicines, 13(5), 1084. https://doi.org/10.3390/biomedicines13051084







