Resveratrol-Loaded Solid Lipid Nanoparticles Reinforced Hyaluronic Hydrogel: Multitarget Strategy for the Treatment of Diabetes-Related Periodontitis
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Synthesis and Characterization of SLN
RSV-SLN Formulation and Characterization
2.3. Preparation and Characterization of RSV-SLN Loaded Cross Linked Hydrogel (RSV@CLgel)
2.3.1. Synthesis of Cross-Linked Hyaluronic Acid Hydrogel with RSV-SLN
2.3.2. Fourier-Transform Infrared (FTIR) Spectroscopy of RSV@CLgel
2.3.3. Rheological Characterization of RSV@CLgel
2.3.4. Water Absorption and Water Retention Capacity of RSV@CLgel
2.3.5. Release Efficiency
2.4. Cell Culture and Treatment
2.5. RSV@CLgel Biocompatibility
2.6. Assessment of Oxidative Stress and Mitochondrial Function
2.6.1. Intracellular ROS Detection
2.6.2. Intracellular Malondialdehyde (MDA) Detection
2.6.3. Total SOD-like, GPx, and CAT Activities
2.6.4. Measurement of ATP Levels
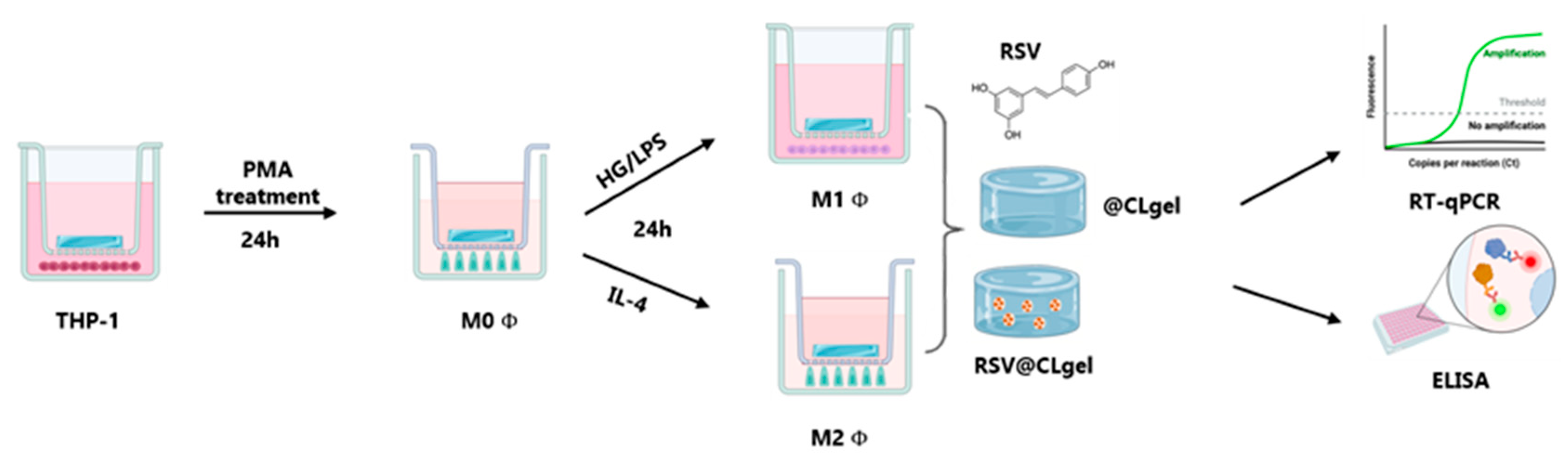
2.7. Macrophage Polarization
2.8. Effects of Conditioned Medium Generated by Polarized Macrophages on hDPSCs
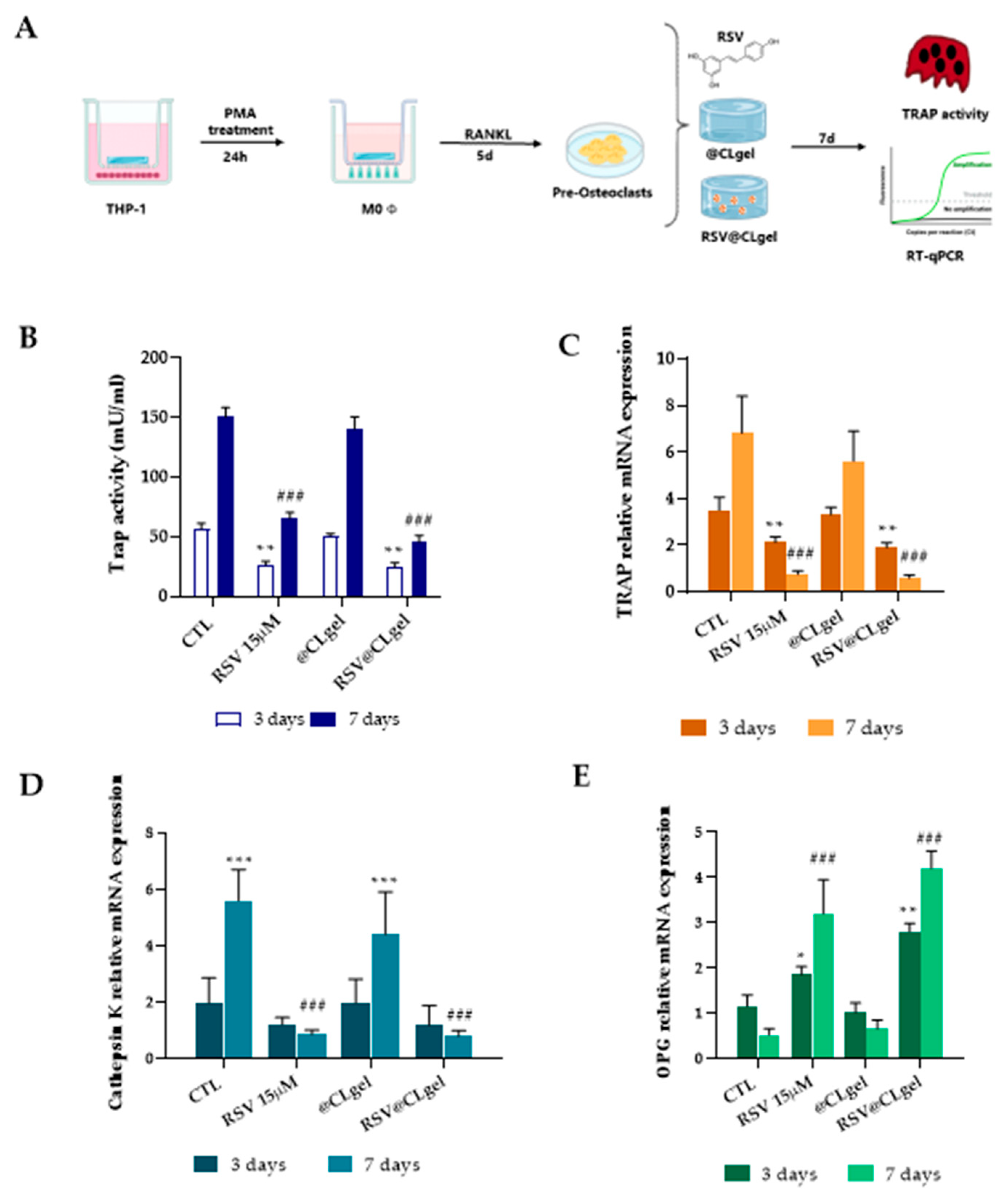
2.9. Osteoclast Differentiation and TRAP Staining
2.10. Statistical Analysis
3. Results and Discussion
3.1. Preparation and Physicochemical Characterization of Resveratrol-Loaded Nanoparticles (RSV-SLN)
3.2. Rheological and Mechanical Characterization of Hydrogel Formulations (RSV@CLgel)
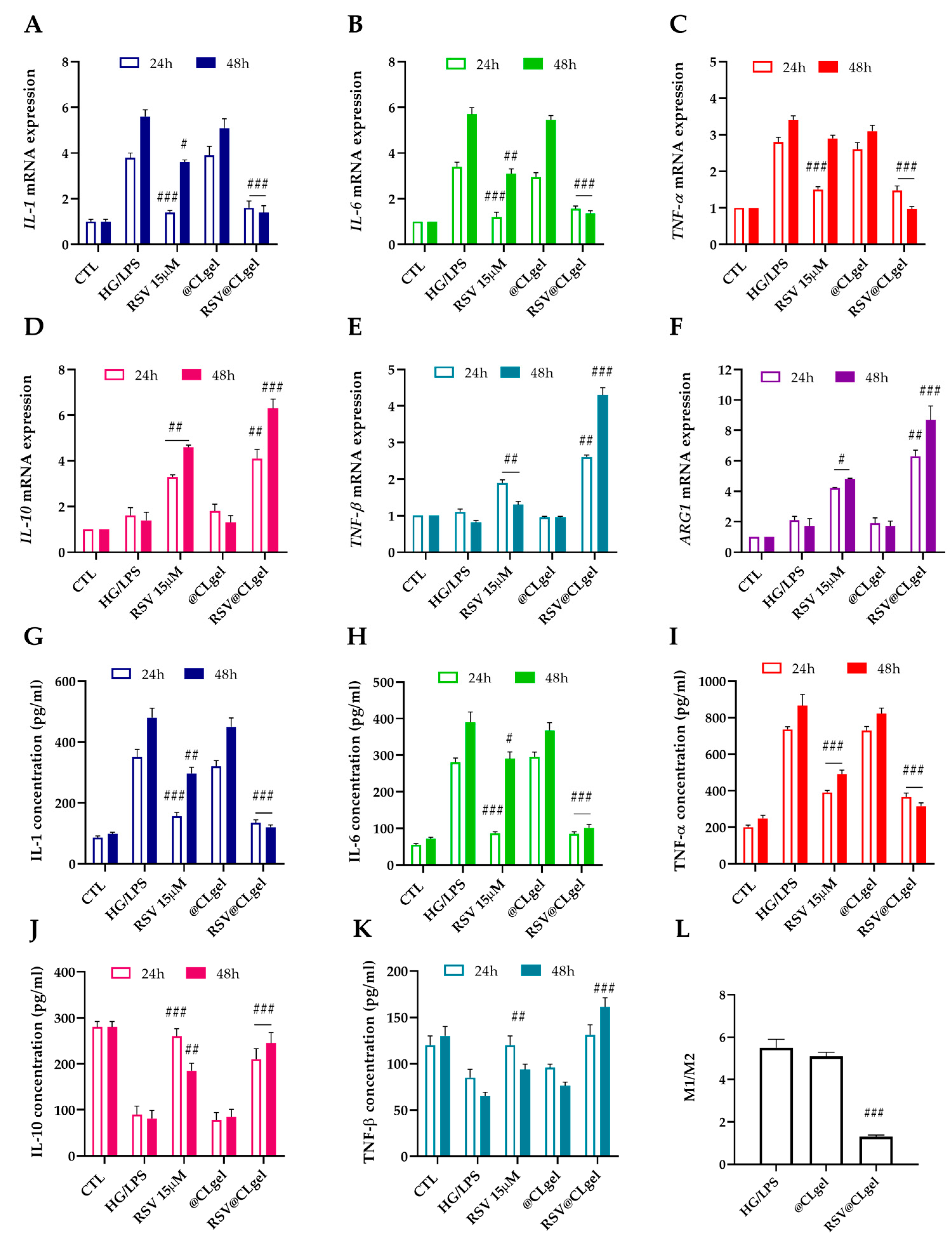
3.3. RSV@CLgel Modulates the Macrophages Polarization Under High Glucose and Pro-Inflammatory Environment
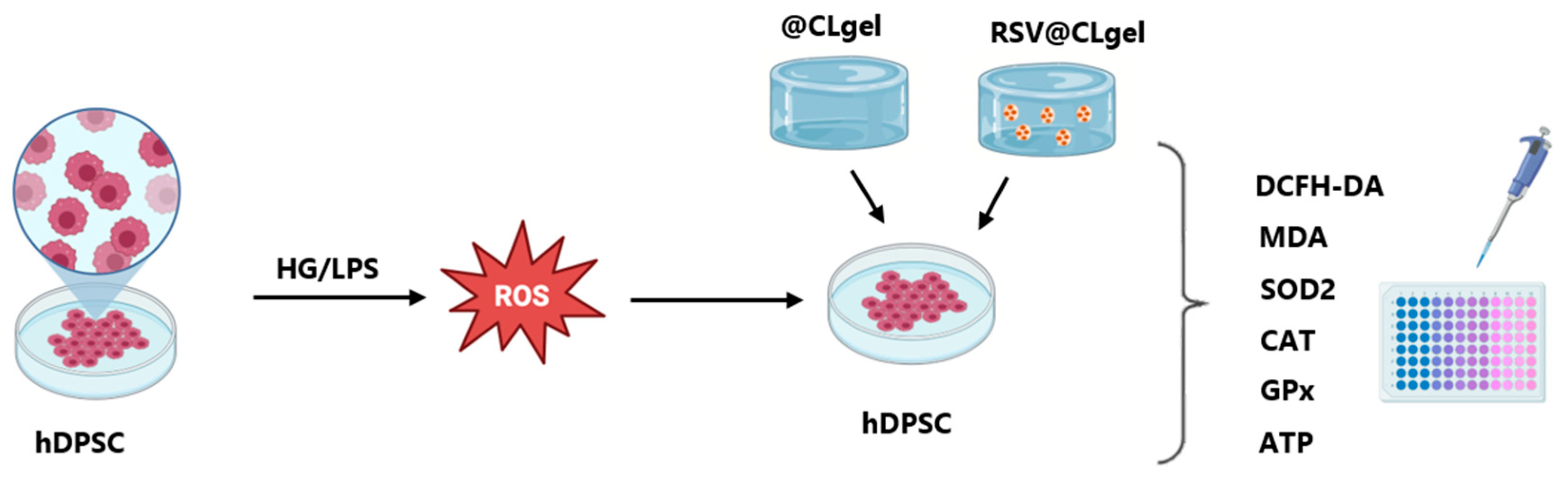
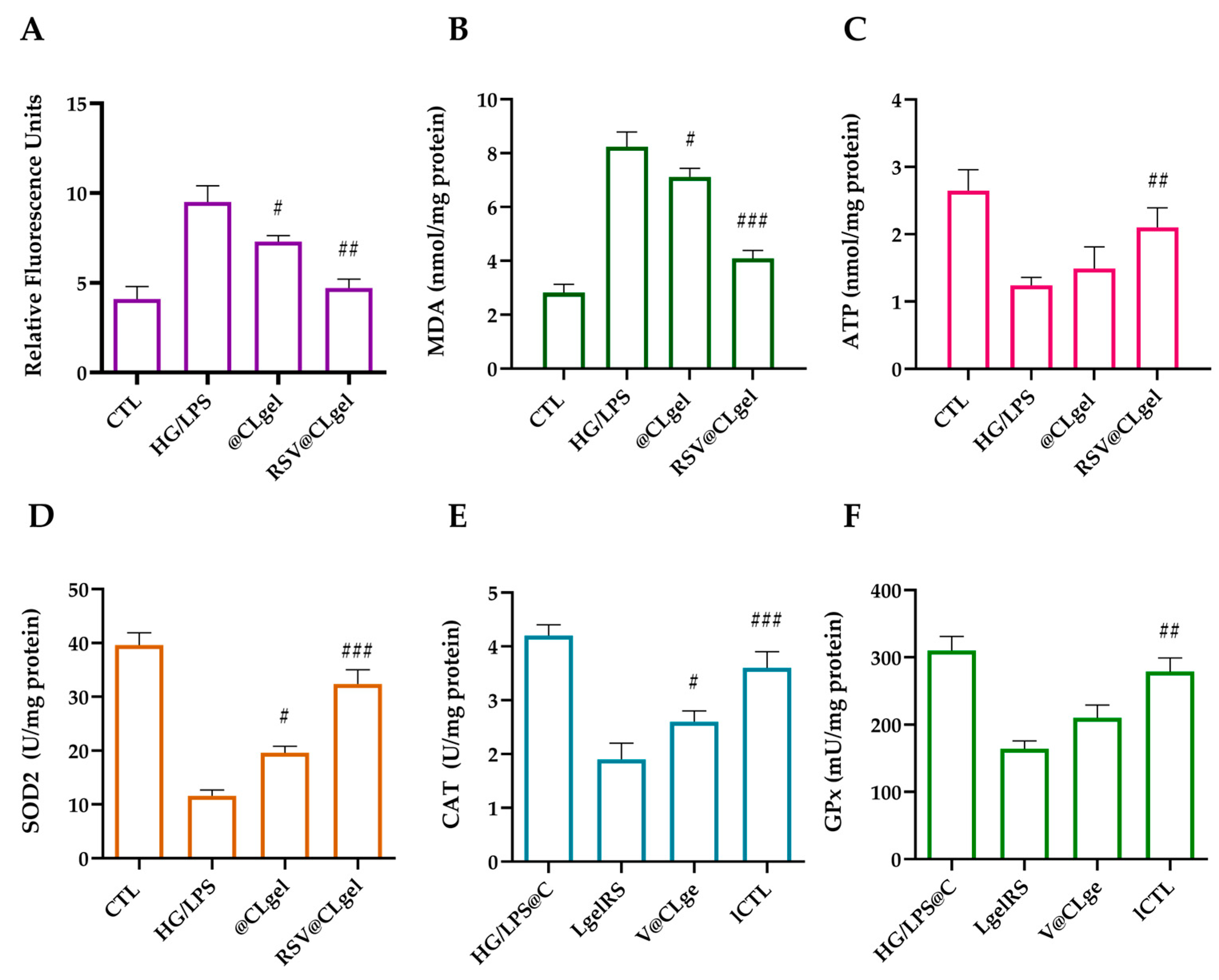
3.4. ROS-Scavenging Ability of RSV@CLgel In Vitro
3.5. RSV@CLgel Restored the Osteogenic Differentiation Capability of hDPSCs in Macrophages Microenvironment
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhao, M.; Xie, Y.; Gao, W.; Li, C.; Ye, Q.; Li, Y. Diabetes mellitus promotes susceptibility to periodontitis—Novel insight into the molecular mechanisms. Front. Endocrinol. 2023, 14, 1192625. [Google Scholar] [CrossRef] [PubMed]
- Kwon, T.; Lamster, I.B.; Levin, L. Current Concepts in the Management of Periodontitis. Int. Dent. J. 2021, 71, 462–476. [Google Scholar] [CrossRef]
- Cardoso, E.M.; Reis, C.; Manzanares-Céspedes, M.C. Chronic periodontitis, inflammatory cytokines, and interrelationship with other chronic diseases. Postgrad. Med. 2018, 130, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Winning, L.; Linden, G.J. Periodontitis and systemic disease. BDJ Team 2015, 2, 15163. [Google Scholar] [CrossRef]
- López-Valverde, N.; Rueda, J.A.B. Effect of Periodontal Treatment in Patients with Periodontitis and Diabetes: Review of Systematic Reviews with Meta-Analyses in the Last Five Years. Healthcare 2024, 12, 1844. [Google Scholar] [CrossRef]
- Su, N.Y.; Ng, M.Y.; Liao, H.Y.; Liao, Y.-W.; Wu, M.; Chao, S.-C.; Yu, C.-C.; Chang, Y.-C. Ganoderma Microsporum Immunomodulatory Protein Alleviates Inflammaging and Oxidative Stress in Diabetes-Associated Periodontitis via Nrf2 Signaling Activation: An In Vitro Study. Antioxidants 2024, 13, 817. [Google Scholar] [CrossRef]
- Arbildo-Vega, H.I.; Cruzado-Oliva, F.H.; Infantes-Ruíz, E.D.; Coronel-Zubiate, F.T.; Becerra-Atoche, E.G.; Terrones-Campos, W.; Herrera-Plasencia, P.M.; Seminario-Trelles, O.A.; Ortega-Gallegos, R.E. An Umbrella Review of the Association Between Periodontal Disease and Diabetes Mellitus. Healthcare 2024, 12, 2311. [Google Scholar] [CrossRef]
- Yin, L.; Li, X.; Hou, J. Macrophages in periodontitis: A dynamic shift between tissue destruction and repair. Jpn. Dent. Sci. Rev. 2022, 58, 336–347. [Google Scholar] [CrossRef]
- Wang, G.; Peng, C.; Tang, M.; Wang, Y.; Li, J.; Chen, H.; Chang, X.; Shu, Z.; He, N.; Guo, J.; et al. Simultaneously boosting inflammation resolution and osteogenic differentiation in periodontitis using folic acid-modified liposome-thermosensitive hydrogel composites. Mater. Des. 2023, 234, 112314. [Google Scholar] [CrossRef]
- Wang, X.; Wang, H.; Zhang, T.; Cai, L.; Kong, C.; He, J. Current Knowledge Regarding the Interaction Between Oral Bone Metabolic Disorders and Diabetes Mellitus. Front. Endocrinol. 2020, 11, 536. [Google Scholar] [CrossRef]
- Kim, J.M.; Lin, C.; Stavre, Z.; Greenblatt, M.B.; Shim, J.H. Osteoblast-Osteoclast Communication and Bone Homeostasis. Cells 2020, 9, 2073. [Google Scholar] [CrossRef] [PubMed]
- Bousch, J.F.; Beyersdorf, C.; Schultz, K.; Windolf, J.; Suschek, C.V.; Maus, U. Proinflammatory Cytokines Enhance the Mineralization, Proliferation, and Metabolic Activity of Primary Human Osteoblast-like Cells. Int. J. Mol. Sci. 2024, 25, 12358. [Google Scholar] [CrossRef]
- Xing, B.; Yu, J.; Zhang, H.; Li, Y. RANKL inhibition: A new target of treating diabetes mellitus? Ther. Adv. Endocrinol. Metab. 2023, 14, 20420188231170754. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Li, J.; Xie, X.; Gu, F.; Sui, Z.; Zhang, K.; Yu, T. Macrophage-Osteoclast Associations: Origin, Polarization, and Subgroups. Front. Immunol. 2021, 12, 778078. [Google Scholar] [CrossRef]
- Listari, K.M.; Pusporini, R.; Nugraeni, Y.; Hidayat, L.H.; Festari, V.D.; Firdaus, J.D. Increasing the Number of Osteoblasts and Decreasing RANKL Expression on Diabetic Periodontitis in Rats Post-Administration of Nanoliposome Papaya Seed Extract. Pesqui. Bras. Odontopediatria Clín. Integr. 2025, 25, e230002. [Google Scholar]
- Tan, Y.J.; Li, X.; Zhang, W.J.; Cao, Y.-M.; Zou, J.-K.; Jing, L.; Gan, D.; Chen, Y.-Z.; Xu, M.; An, Y.; et al. Mitochondria-targeted delivery of zinc-coordinated resveratrol nanoparticles rescues the osteogenic potential of periodontal ligament stem cells compromised by inflammation for periodontal wound healing. Chem. Eng. J. 2025, 503, 158296. [Google Scholar] [CrossRef]
- Xu, L.; Botchway, B.O.A.; Zhang, S.; Zhou, J.; Liu, X. Inhibition of NF-κB Signaling Pathway by Resveratrol Improves Spinal Cord Injury. Front. Neurosci. 2018, 12, 690. [Google Scholar] [CrossRef]
- Omraninava, M.; Razi, B.; Aslani, S.; Imani, D.; Jamialahmadi, T.; Sahebkar, A. Effect of resveratrol on inflammatory cytokines: A meta-analysis of randomized controlled trials. Eur. J. Pharmacol. 2021, 908, 174380. [Google Scholar] [CrossRef]
- Meng, T.; Xiao, D.; Muhammed, A.; Deng, J.; Chen, L.; He, J. Anti-Inflammatory Action and Mechanisms of Resveratrol. Molecules 2021, 26, 229. [Google Scholar] [CrossRef]
- Tamaki, N.; Cristina Orihuela-Campos, R.; Inagaki, Y.; Fukui, M.; Nagata, T.; Ito, H.O. Resveratrol improves oxidative stress and prevents the progression of periodontitis via the activation of the Sirt1/AMPK and the Nrf2/antioxidant defense pathways in a rat periodontitis model. Free Radic. Biol. Med. 2014, 75, 222–229. [Google Scholar] [CrossRef]
- Omidian, M.; Abdolahi, M.; Daneshzad, E.; Sedighiyan, M.; Aghasi, M.; Abdollahi, H.; Omidian, P.; Dabiri, S.; Mahmoudi, M.; Hadavi, S.; et al. The Effects of Resveratrol on Oxidative Stress Markers: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Endocr. Metab. Immune Disord. Drug Targets 2020, 20, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Borsani, E.; Bonazza, V.; Buffoli, B.; Nocini, P.F.; Albanese, M.; Zotti, F.; Inchingolo, F.; Rezzani, R.; Rodella, L.F. Beneficial Effects of Concentrated Growth Factors and Resveratrol on Human Osteoblasts In Vitro Treated with Bisphosphonates. Biomed. Res. Int. 2018, 2018, 4597321. [Google Scholar] [CrossRef]
- Peng, H.; Qiu, X.; Cheng, M.; Zhao, Y.; Song, L.; Zhu, B.; Li, Y.; Liu, C.; Ren, S.; Miao, L. Resveratrol-loaded nanoplatform RSV@DTPF promote alveolar bone regeneration in OVX rat through remodeling bone-immune microenvironment. Chem. Eng. J. 2023, 476, 146615. [Google Scholar] [CrossRef]
- De Luca, I.; Di Cristo, F.; Conte, R.; Peluso, G.; Cerruti, P.; Calarco, A. In-Situ Thermoresponsive Hydrogel Containing Resveratrol-Loaded Nanoparticles as a Localized Drug Delivery Platform for Dry Eye Disease. Antioxidants 2023, 12, 993. [Google Scholar] [CrossRef]
- Lamont, R.J.; Koo, H.; Hajishengallis, G. The oral microbiota: Dynamic communities and host interactions. Nat. Rev. Microbiol. 2018, 16, 745–759. [Google Scholar] [CrossRef] [PubMed]
- Fratila, D.N.; Virvescu, D.I.; Luchian, I.; Hancianu, M.; Baciu, E.R.; Butnaru, O.; Budala, D.G. Advances and Functional Integration of Hydrogel Composites as Drug Delivery Systems in Contemporary Dentistry. Gels 2024, 10, 661. [Google Scholar] [CrossRef]
- Han, M.; Tang, K.; Chen, Z. Preparation of NIR responsive resveratrol@Au nanocages using for regulating oxidative stress microenvironment of periodontitis. Chem. Eng. J. 2025, 504, 158774. [Google Scholar] [CrossRef]
- Conte, R.; Valentino, A.; De Luca, I.; Soares Pontes, G.; Calarco, A.; Cerruti, P. Thermo-Responsive Hydrogel Containing Microfluidic Chitosan Nanoparticles Loaded with Opuntia ficus-indica Extract for Periodontitis Treatment. Int. J. Mol. Sci. 2024, 25, 9374. [Google Scholar] [CrossRef]
- Spagnuolo, G.; De Luca, I.; Iaculli, F.; Barbato, E.; Valletta, A.; Calarco, A.; Valentino, A.; Riccitiello, F. Regeneration of dentin-pulp complex: Effect of calcium-based materials on hDPSCs differentiation and gene expression. Dent. Mater. 2023, 39, 485–491. [Google Scholar] [CrossRef]
- Zhang, B.; Yang, Y.; Yi, J.; Zhao, Z.; Ye, R. Hyperglycemia modulates M1/M2 macrophage polarization via reactive oxygen species overproduction in ligature-induced periodontitis. J. Periodontal Res. 2021, 56, 991–1005. [Google Scholar] [CrossRef]
- Li, Y.; Ma, Y.; Yu, J.; Li, C.; Yu, D.; Dai, R.; Li, Q.; Cao, C.Y. A dual functional polypeptide with antibacterial and anti-inflammatory properties for the treatment of periodontitis. Int. J. Biol. Macromol. 2023, 242, 124920. [Google Scholar] [CrossRef]
- Riccitiello, F.; De Luise, A.; Conte, R.; D’Aniello, S.; Vittoria, V.; Di Salle, A.; Calarco, A.; Peluso, G. Effect of resveratrol release kinetic from electrospun nanofibers on osteoblast and osteoclast differentiation. Eur. Polym. J. 2018, 99, 289–297. [Google Scholar] [CrossRef]
- Dhiman, N.; Awasthi, R.; Sharma, B.; Kharkwal, H.; Kulkarni, G.T. Lipid Nanoparticles as Carriers for Bioactive Delivery. Front. Chem. 2021, 9, 580118. [Google Scholar] [CrossRef] [PubMed]
- Sastri, K.T.; Radha, G.V.; Pidikiti, S.; Vajjhala, P. Solid lipid nanoparticles: Preparation techniques, their characterization, and an update on recent studies. J. Appl. Pharm. Sci. 2020, 10, 126–141. [Google Scholar] [CrossRef]
- Burdock, G.A.; Carabin, I.G. Generally recognized as safe (GRAS): History and description. Toxicol. Lett. 2004, 150, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Nobari Azar, F.A.; Pezeshki, A.; Ghanbarzadeh, B.; Hamishehkar, H.; Mohammadi, M. Nanostructured lipid carriers: Promising delivery systems for encapsulation of food ingredients. J. Agric. Food Res. 2020, 2, 100084. [Google Scholar] [CrossRef]
- Tang, C.H.; Chen, H.L.; Dong, J.R. Solid Lipid Nanoparticles (SLNs) and Nanostructured Lipid Carriers (NLCs) as Food-Grade Nanovehicles for Hydrophobic Nutraceuticals or Bioactives. Appl. Sci. 2023, 13, 1726. [Google Scholar] [CrossRef]
- Salvia-Trujillo, L.; Verkempinck, S.; Rijal, S.K.; Van Loey, A.; Grauwet, T.; Hendrickx, M. Lipid nanoparticles with fats or oils containing β-carotene: Storage stability and in vitro digestibility kinetics. Food Chem. 2019, 278, 396–405. [Google Scholar] [CrossRef]
- Schubert, M.A.; Müller-Goymann, C.C. Characterisation of surface-modified solid lipid nanoparticles (SLN): Influence of lecithin and nonionic emulsifier. Eur. J. Pharm. Biopharm. 2005, 61, 77–86. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, Y.; Yu, T.; Song, G.; Xu, T.; Xin, T.; Lin, Y.; Han, B. Nano-Based Drug Delivery Systems for Periodontal Tissue Regeneration. Pharmaceutics 2022, 14, 2250. [Google Scholar] [CrossRef]
- Allaker, R.P. The Use of Antimicrobial Nanoparticles to Control Oral Infections. In Nano-Antimicrobials; Springer: Berlin/Heidelberg, Germany, 2012; pp. 395–425. [Google Scholar] [CrossRef]
- Vigani, B.; Rossi, S.; Sandri, G.; Bonferoni, M.C.; Caramella, C.M. Mucoadhesive polymers in substance-based medical devices: Functional ingredients or what else? Front. Drug Saf. Regul. 2023, 3, 1227763. [Google Scholar] [CrossRef]
- Conte, R.; De Luca, I.; Valentino, A.; Cerruti, P.; Pedram, P.; Cabrera-Barjas, G.; Moeini, A.; Calarco, A. Hyaluronic Acid Hydrogel Containing Resveratrol-Loaded Chitosan Nanoparticles as an Adjuvant in Atopic Dermatitis Treatment. J. Funct. Biomater. 2023, 14, 82. [Google Scholar] [CrossRef]
- Dahiya, P.; Kamal, R. Hyaluronic acid: A boon in periodontal therapy. N. Am. J. Med. Sci. 2013, 5, 309. [Google Scholar] [CrossRef]
- Zhang, T.; Zhao, S.; Chen, Y.; Wang, J.; Zhang, W.; Liu, J.; Kan, Y.; Li, J.-P.; Guo, X.; Li, H. In-depth characterization of 1,4-butanediol diglycidyl ether substituted hyaluronic acid hydrogels. Carbohydr. Polym. 2023, 307, 120611. [Google Scholar] [CrossRef] [PubMed]
- Jung, H. Hyaluronidase: An overview of its properties, applications, and side effects. Arch. Plast. Surg. 2020, 47, 297–300. [Google Scholar] [CrossRef]
- Berkó, S.; Maroda, M.; Bodnár, M.; Erős, G.; Hartmann, P.; Szentner, K.; Szabó-Révész, P.; Kemény, L.; Borbély, J.; Csányi, E. Advantages of cross-linked versus linear hyaluronic acid for semisolid skin delivery systems. Eur. Polym. J. 2013, 49, 2511–2517. [Google Scholar] [CrossRef]
- Jeong, C.H.; Kim, D.H.; Yune, J.H.; Kwon, H.C.; Shin, D.-M.; Sohn, H.; Lee, K.H.; Choi, B.; Kim, E.S.; Kang, J.H.; et al. In vitro toxicity assessment of crosslinking agents used in hyaluronic acid dermal filler. Toxicol. Vitr. 2021, 70, 105034. [Google Scholar] [CrossRef] [PubMed]
- de la Guardia, C.; Virno, A.; Musumeci, M.; Bernardin, A.; Silberberg, M.B. Rheologic and Physicochemical Characteristics of Hyaluronic Acid Fillers: Overview and Relationship to Product Performance. Facial Plast. Surg. 2022, 38, 116–123. [Google Scholar] [CrossRef]
- Rwei, S.P.; Chen, S.W.; Mao, C.F.; Fang, H.W. Viscoelasticity and wearability of hyaluronate solutions. Biochem. Eng. J. 2008, 40, 211–217. [Google Scholar] [CrossRef]
- Zöller, K.; To, D.; Bernkop-Schnürch, A. Biomedical applications of functional hydrogels: Innovative developments, relevant clinical trials and advanced products. Biomaterials 2025, 312, 122718. [Google Scholar] [CrossRef]
- Wu, Y.Y.; Xiao, E.; Graves, D.T. Diabetes mellitus related bone metabolism and periodontal disease. Int. J. Oral. Sci. 2015, 7, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Mirnic, J.; Djuric, M.; Brkic, S.; Gusic, I.; Stojilkovic, M.; Tadic, A.; Veljovic, T. Pathogenic Mechanisms That May Link Periodontal Disease and Type 2 Diabetes Mellitus—The Role of Oxidative Stress. Int. J. Mol. Sci. 2024, 25, 9806. [Google Scholar] [CrossRef] [PubMed]
- Nazir, G.; Amin, J. Diabetes mellitus and periodontal diseases: A two way relationship. Int. J. Dent. Res. 2021, 6, 43–56. [Google Scholar] [CrossRef]
- Lawrence, T.; Natoli, G. Transcriptional regulation of macrophage polarization: Enabling diversity with identity. Nat. Rev. Immunol. 2011, 11, 750–761. [Google Scholar] [CrossRef]
- Zhao, P.; Yue, Z.; Nie, L.; Zhao, Z.; Wang, Q.; Chen, J.; Wang, Q. Hyperglycaemia-associated macrophage pyroptosis accelerates periodontal inflamm-aging. J. Clin. Periodontol. 2021, 48, 1379–1392. [Google Scholar] [CrossRef] [PubMed]
- Shi, N.; Kong, C.; Yuan, L.; Liu, L.; Zhao, K.; Lü, J.; Wang, X. The bidirectional relationship between periodontitis and diabetes: New prospects for stem cell-derived exosomes. Biomed. Pharmacother. 2023, 165, 115219. [Google Scholar] [CrossRef]
- Saeb, A.T.M.; Al-Rubeaan, K.A.; Aldosary, K.; Raja, G.U.; Mani, B.; Abouelhoda, M.; Tayeb, H.T. Relative reduction of biological and phylogenetic diversity of the oral microbiota of diabetes and pre-diabetes patients. Microb. Pathog. 2019, 128, 215–229. [Google Scholar] [CrossRef]
- Moganti, K.; Li, F.; Schmuttermaier, C.; Riemann, S.; Klüter, H.; Gratchev, A.; Harmsen, M.C.; Kzhyshkowska, J. Hyperglycemia induces mixed M1/M2 cytokine profile in primary human monocyte-derived macrophages. Immunobiology 2017, 222, 952–959. [Google Scholar] [CrossRef]
- Preshaw, P.M.; Alba, A.L.; Herrera, D.; Jepsen, S.; Konstantinidis, A.; Makrilakis, K.; Taylor, R. Periodontitis and diabetes: A two-way relationship. Diabetologia 2012, 55, 21–31. [Google Scholar] [CrossRef]
- Chang, Z.; Wang, Y.; Liu, C.; Smith, W.; Kong, L. Natural Products for Regulating Macrophages M2 Polarization. Curr. Stem Cell Res. Ther. 2020, 15, 559–569. [Google Scholar] [CrossRef]
- Tan, Y.; Feng, J.; Xiao, Y.; Bao, C. Grafting resveratrol onto mesoporous silica nanoparticles towards efficient sustainable immunoregulation and insulin resistance alleviation for diabetic periodontitis therapy. J. Mater. Chem. B 2022, 10, 4840–4855. [Google Scholar] [CrossRef] [PubMed]
- Canton, M.; Sánchez-Rodríguez, R.; Spera, I.; Venegas, F.C.; Favia, M.; Viola, A.; Castegna, A. Reactive Oxygen Species in Macrophages: Sources and Targets. Front. Immunol. 2021, 12, 4840–4855. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Reyes, I.; Chandel, N.S. Mitochondrial TCA cycle metabolites control physiology and disease. Nat. Commun. 2020, 11, 102. [Google Scholar] [CrossRef] [PubMed]
- Kocher, T.; König, J.; Borgnakke, W.S.; Pink, C.; Meisel, P. Periodontal complications of hyperglycemia/diabetes mellitus: Epidemiologic complexity and clinical challenge. Periodontol. 2000 2018, 78, 59–97. [Google Scholar] [CrossRef]
- Önder, C.; Kurgan, Ş.; Altıngöz, S.M.; Bağış, N.; Uyanık, M.; Serdar, M.A.; Kantarcı, A.; Günhan, M. Impact of non-surgical periodontal therapy on saliva and serum levels of markers of oxidative stress. Clin. Oral. Investig. 2017, 21, 1961–1969. [Google Scholar] [CrossRef]
- Trivedi, S.; Lal, N.; Mahdi, A.A.; Mittal, M.; Singh, B.; Pandey, S. Evaluation of Antioxidant Enzymes Activity and Malondialdehyde Levels in Patients with Chronic Periodontitis and Diabetes Mellitus. J. Periodontol. 2014, 85, 713–720. [Google Scholar] [CrossRef]
- Trivedi, S.; Lal, N.; Mahdi, A.; Singh, B.; Pandey, S. Association of Salivary Lipid Peroxidation Levels, Antioxidant Enzymes, and Chronic Periodontitis. Int. J. Periodontics Restor. Dent. 2015, 35, e14–e19. [Google Scholar] [CrossRef]
- Hu, H.C.; Lei, Y.H.; Zhang, W.H.; Luo, X.Q. Antioxidant and Anti-inflammatory Properties of Resveratrol in Diabetic Nephropathy: A Systematic Review and Meta-analysis of Animal Studies. Front. Pharmacol. 2022, 13, 841818. [Google Scholar] [CrossRef]
- Cabanillas-Balsera, D.; Martín-González, J.; Montero-Miralles, P.; Sánchez-Domínguez, B.; Jiménez-Sánchez, M.C.; Segura-Egea, J.J. Association between diabetes and nonretention of root filled teeth: A systematic review and meta-analysis. Int. Endod. J. 2019, 52, 297–306. [Google Scholar] [CrossRef]
- Taylor, G.W.; Burt, B.A.; Becker, M.P.; Genco, R.J.; Shlossman, M. Glycemic Control and Alveolar Bone Loss Progression in Type 2 Diabetes. Ann. Periodontol. 1998, 3, 30–39. [Google Scholar] [CrossRef]
- Li, Y.; Shrestha, A.; Zhang, H.; Li, L.; Li, D.; Fu, T.; Song, J.; Ji, P.; Huang, Y.; Chen, T. Impact of diabetes mellitus simulations on bone cell behavior through in vitro models. J. Bone Miner. Metab. 2020, 38, 607–619. [Google Scholar] [CrossRef] [PubMed]
- Figeac, F.; Tencerova, M.; Ali, D.; Andersen, T.L.; Appadoo, D.R.C.; Kerckhofs, G.; Ditzel, N.; Kowal, J.M.; Rauch, A.; Kassem, M. Impaired Bone Fracture Healing in Type 2 Diabetes Is Caused by Defective Functions of Skeletal Progenitor Cells. Stem Cells 2022, 40, 149–164. [Google Scholar] [CrossRef]
- Park, S.Y.; Choi, K.H.; Jun, J.E.; Chung, H.Y. Effects of Advanced Glycation End Products on Differentiation and Function of Osteoblasts and Osteoclasts. J. Korean Med. Sci. 2021, 36, e239. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, E.; Tanaka, D.; Glogauer, M.; Tenenbaum, H.C.; Ikeda, Y. Healing effects of monomer and dimer resveratrol in a mouse periodontitis model. BMC Oral. Health 2022, 22, 460. [Google Scholar] [CrossRef] [PubMed]
- Andrade, E.F.; Orlando, D.R.; Araújo, A.M.S.; de Andrade, J.N.B.M.; Azzi, D.V.; de Lima, R.R.; Lobo-Júnior, A.R.; Pereira, L.J. Can Resveratrol Treatment Control the Progression of Induced Periodontal Disease? A Systematic Review and Meta-Analysis of Preclinical Studies. Nutrients 2019, 11, 953. [Google Scholar] [CrossRef]
- Vidoni, C.; Ferraresi, A.; Secomandi, E.; Vallino, L.; Gardin, C.; Zavan, B.; Mortellaro, C.; Isidoro, C. Autophagy drives osteogenic differentiation of human gingival mesenchymal stem cells. Cell Commun. Signal. 2019, 17, 98. [Google Scholar] [CrossRef]
- Bartold, P.M.; Cantley, M.D.; Haynes, D.R. Mechanisms and control of pathologic bone loss in periodontitis. Periodontol. 2000 2010, 53, 55–69. [Google Scholar] [CrossRef]
- Huang, X.; Xie, M.; Xie, Y.; Mei, F.; Lu, X.; Li, X.; Chen, L. The roles of osteocytes in alveolar bone destruction in periodontitis. J. Transl. Med. 2020, 18, 479. [Google Scholar] [CrossRef]



| Code | Drug-to-Oil Ratio | Size (nm) | PDI | ζ-Potential (mV) | Encapsulation Efficiency (EE%) |
|---|---|---|---|---|---|
| RSV-SLN | 0.1 | 148.7 ± 2.22 | 0.24 ± 0.02 | −31 ± 1.07 | 34.4 ± 5.92 |
| RSV2-SLN | 0.2 | 110.1 ± 1.23 | 0.10 ± 0.01 | −35 ± 1.04 | 66.4 ± 2.51 |
| RSV3-SLN | 0.3 | 120.3 ± 1.85 | 0.15 ± 0.02 | −32 ± 1.07 | 50.3 ± 3.13 |
| RSV4-SLN | 0.4 | 130.5 ± 2.06 | 0.14 ± 0.01 | −33 ± 1.01 | 45.2 ± 3.57 |
| RSV5-SLN | 0.5 | 135.2 ± 2.17 | 0.18 ± 0.02 | −34 ± 1.08 | 40.7 ± 4.29 |
| RSV6-SLN | 0.6 | 140.6 ± 2.26 | 0.20 ± 0.02 | −34 ± 1.03 | 37.8 ± 4.82 |
| RSV7-SLN | 0.7 | 144.8 ± 2.34 | 0.21 ± 0.02 | −33 ± 1.02 | 36.0 ± 5.02 |
| RSV8-SLN | 0.8 | 146.5 ± 2.39 | 0.22 ± 0.02 | −32 ± 1.06 | 35.2 ± 5.54 |
| RSV9-SLN | 0.9 | 147.6 ± 2.22 | 0.23 ± 0.02 | −31 ± 1.05 | 34.6 ± 5.75 |
| RSV10-SLN | 1.0 | 148.7 ± 2.21 | 0.24 ± 0.02 | −31 ± 1.04 | 34.4 ± 5.97 |
| Sample | G′ (Pa) at 1.59 Hz | G″ (Pa) at 1.59 Hz | Tan δ at 1.59 Hz | ή* (Pa x s) at 1.59 Hz |
|---|---|---|---|---|
| Cross linked HA gel (@CLgel) | 3016 | 811 | 0.269 | 322 |
| RSV@CLgel | 3136 | 834 | 0.266 | 324 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conte, R.; Valentino, A.; Sepe, F.; Gianfreda, F.; Condò, R.; Cerroni, L.; Calarco, A.; Peluso, G. Resveratrol-Loaded Solid Lipid Nanoparticles Reinforced Hyaluronic Hydrogel: Multitarget Strategy for the Treatment of Diabetes-Related Periodontitis. Biomedicines 2025, 13, 1059. https://doi.org/10.3390/biomedicines13051059
Conte R, Valentino A, Sepe F, Gianfreda F, Condò R, Cerroni L, Calarco A, Peluso G. Resveratrol-Loaded Solid Lipid Nanoparticles Reinforced Hyaluronic Hydrogel: Multitarget Strategy for the Treatment of Diabetes-Related Periodontitis. Biomedicines. 2025; 13(5):1059. https://doi.org/10.3390/biomedicines13051059
Chicago/Turabian StyleConte, Raffaele, Anna Valentino, Fabrizia Sepe, Francesco Gianfreda, Roberta Condò, Loredana Cerroni, Anna Calarco, and Gianfranco Peluso. 2025. "Resveratrol-Loaded Solid Lipid Nanoparticles Reinforced Hyaluronic Hydrogel: Multitarget Strategy for the Treatment of Diabetes-Related Periodontitis" Biomedicines 13, no. 5: 1059. https://doi.org/10.3390/biomedicines13051059
APA StyleConte, R., Valentino, A., Sepe, F., Gianfreda, F., Condò, R., Cerroni, L., Calarco, A., & Peluso, G. (2025). Resveratrol-Loaded Solid Lipid Nanoparticles Reinforced Hyaluronic Hydrogel: Multitarget Strategy for the Treatment of Diabetes-Related Periodontitis. Biomedicines, 13(5), 1059. https://doi.org/10.3390/biomedicines13051059







