Magnetic Resonance Imaging Predictors of Surgical Difficulty in Transforaminal Endoscopic Lumbar Discectomy for Far-Lateral Disc Herniation Under Local Anesthesia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
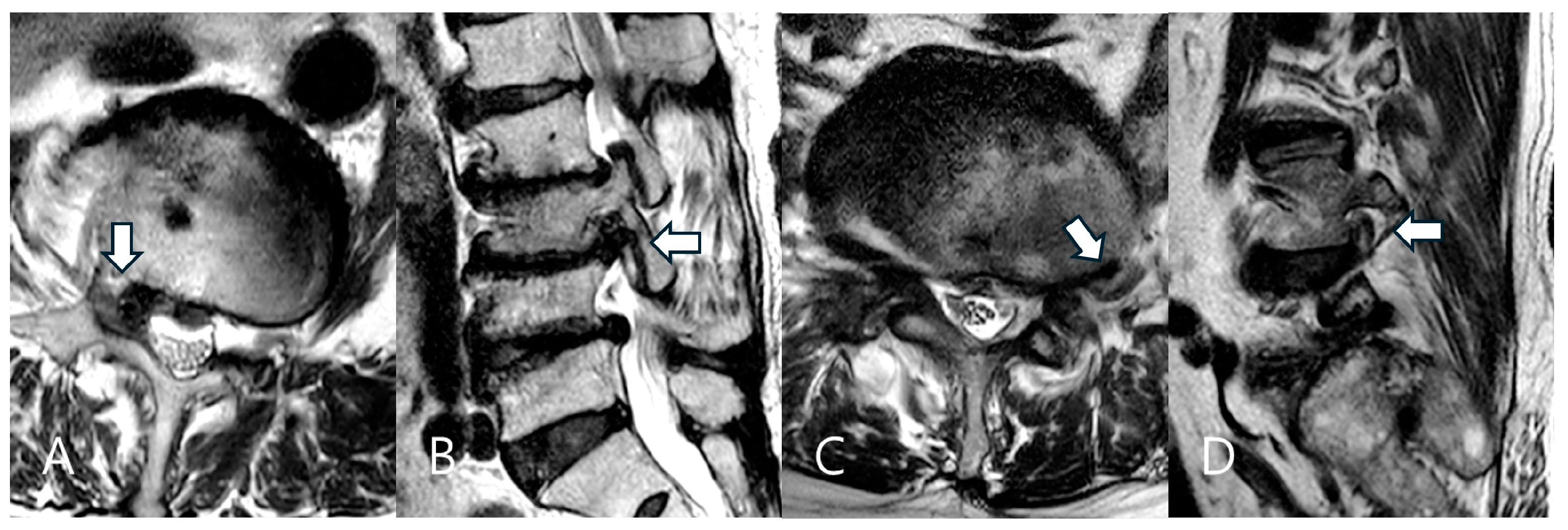
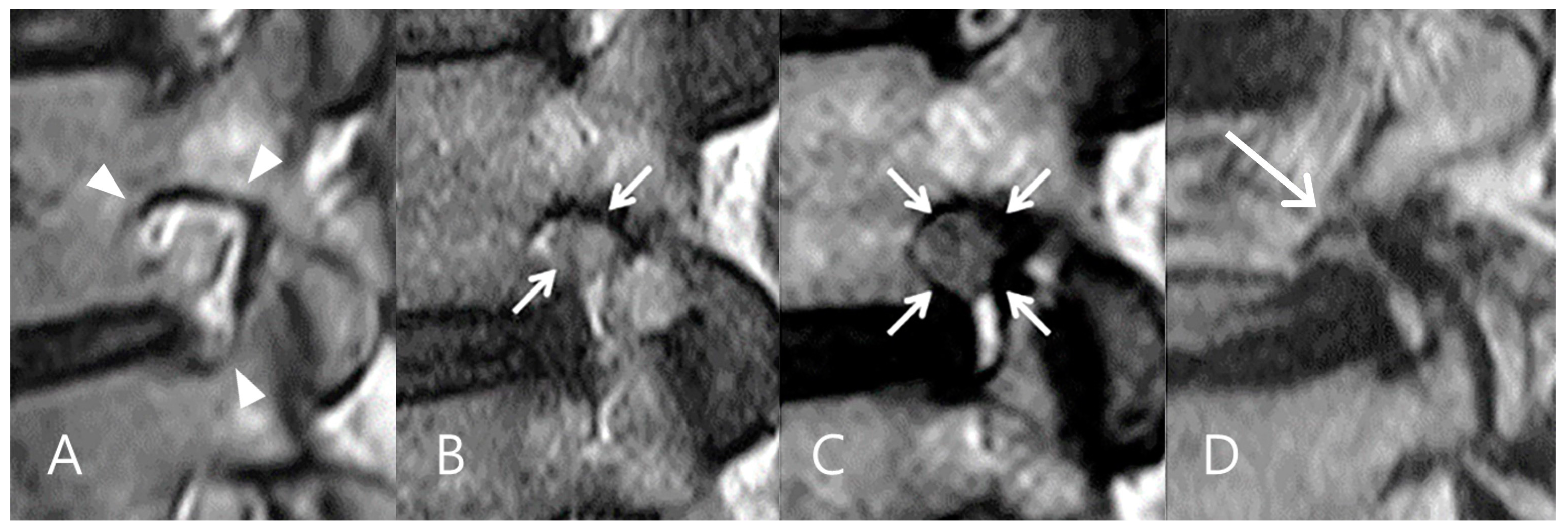
2.2. Preoperative Assessment
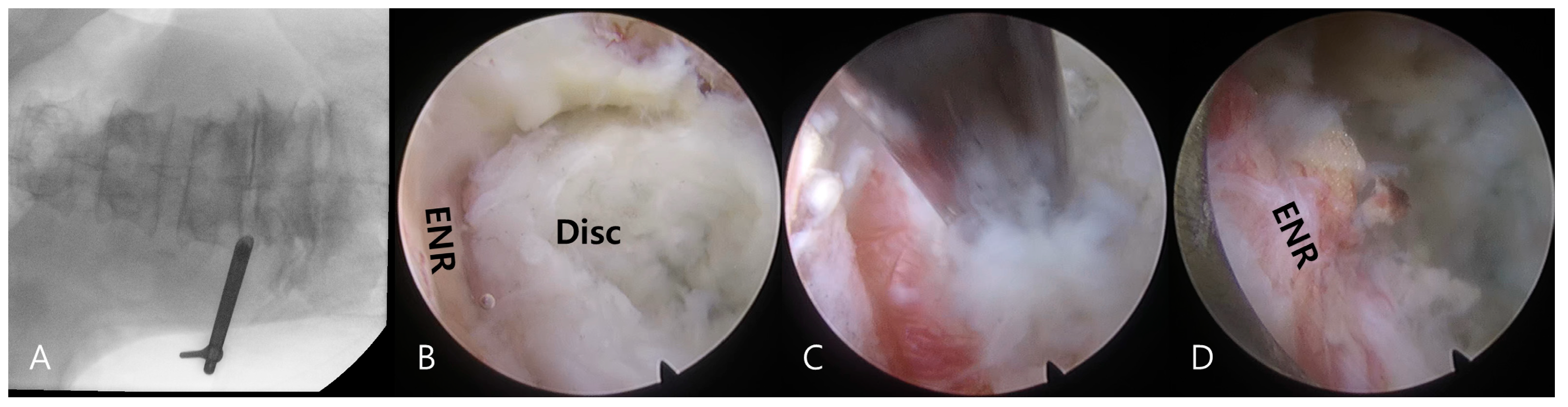
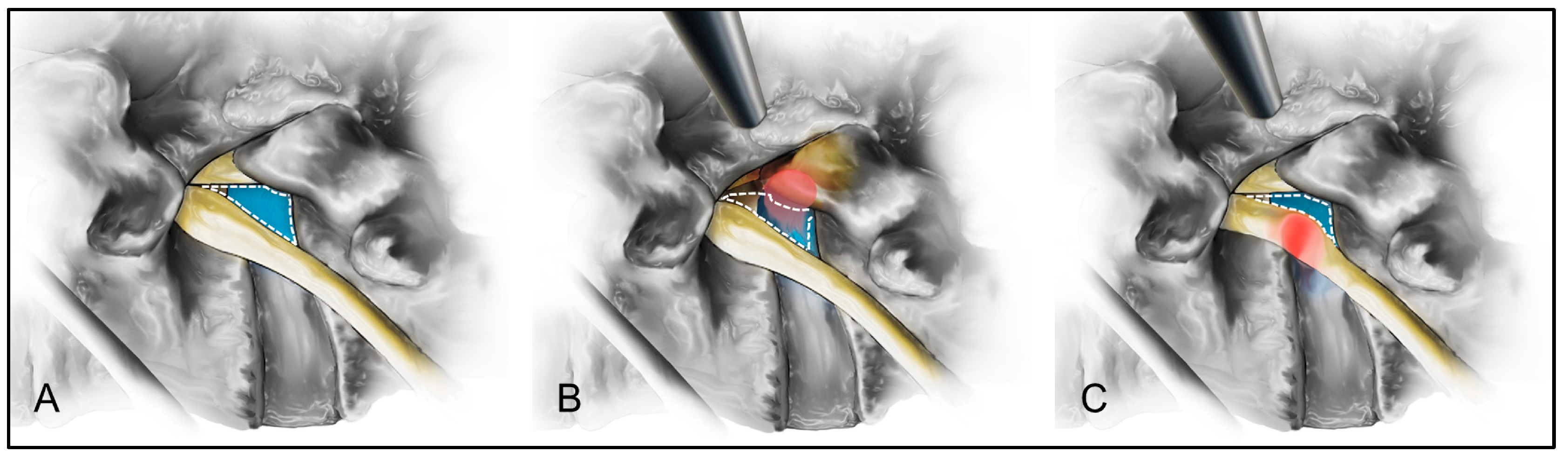
2.3. Surgical Technique
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. Demographics and Clinical Outcome
3.2. Univariate Analysis of Predictors of Surgical Difficulty
3.3. Multivariate Analysis of Predictors of Surgical Difficulty
4. Discussion
4.1. Prediction of Surgical Difficulty in TELD for Far-Lateral LDH
4.2. Impact of Foraminal Stenosis Grade on Perioperative Data
4.3. Foraminal vs. Extraforaminal LDH: Impact on Surgical Complexity
4.4. Inherent Difficulties of the Transforaminal Endoscopic Approach
4.5. Strategies to Reduce Access Pain and Operative Time
4.6. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mayer, H.M.; Brock, M. Percutaneous endoscopic discectomy: Surgical technique and preliminary results compared to microsurgical discectomy. J. Neurosurg. 1993, 78, 216–225. [Google Scholar] [PubMed]
- Hermantin, F.U.; Peters, T.; Quartararo, L.; Kambin, P. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J. Bone Jt. Surg. Am. 1999, 81, 958–965. [Google Scholar]
- Hoogland, T.; Schubert, M.; Miklitz, B.; Ramirez, A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: A prospective randomized study in 280 consecutive cases. Spine 2006, 31, E890–E897. [Google Scholar] [CrossRef] [PubMed]
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine 2008, 33, 931–939. [Google Scholar] [CrossRef]
- Nellensteijn, J.; Ostelo, R.; Bartels, R.; Peul, W.; van Royen, B.; van Tulder, M. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: A systematic review of the literature. Eur. Spine J. 2010, 19, 181–204. [Google Scholar]
- Cong, L.; Zhu, Y.; Tu, G. A meta-analysis of endoscopic discectomy versus open discectomy for symptomatic lumbar disk herniation. Eur. Spine J. 2016, 25, 134–143. [Google Scholar] [CrossRef]
- Li, X.C.; Zhong, C.F.; Deng, G.B.; Liang, R.W.; Huang, C.M. Full-Endoscopic procedures versus traditional discectomy surgery for discectomy: A systematic review and meta-analysis of current global clinical trials. Pain Physician 2016, 19, 103–118. [Google Scholar]
- Ruan, W.; Feng, F.; Liu, Z.; Xie, J.; Cai, L.; Ping, A. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: A meta-analysis. Int. J. Surg. 2016, 31, 86–92. [Google Scholar]
- Ding, W.; Yin, J.; Yan, T.; Nong, L.; Xu, N. Meta-analysis of percutaneous transforaminal endoscopic discectomy vs. fenestration discectomy in the treatment of lumbar disc herniation. Orthopade 2018, 47, 574–584. [Google Scholar]
- Zhang, B.; Liu, S.; Liu, J.; Yu, B.; Guo, W.; Li, Y.; Liu, Y.; Ruan, W.; Ning, G.; Feng, S. Transforaminal endoscopic discectomy versus conventional microdiscectomy for lumbar discherniation: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2018, 13, 169. [Google Scholar]
- Barber, S.M.; Nakhla, J.; Konakondla, S.; Fridley, J.S.; Oyelese, A.A.; Gokaslan, Z.L.; Telfeian, A.E. Outcomes of endoscopic discectomy compared with open microdiscectomy and tubular microdiscectomy for lumbar disc herniations: A meta-analysis. J. Neurosurg. Spine 2019, 31, 802–815. [Google Scholar] [CrossRef] [PubMed]
- Gadjradj, P.S.; Harhangi, B.S.; Amelink, J.; van Susante, J.; Kamper, S.; van Tulder, M.; Peul, W.C.; Vleggeert-Lankamp, C.; Rubinstein, S.M. Percutaneous transforaminal endoscopic discectomy versus open microdiscectomy for lumbar disc herniation: A systematic review and meta-analysis. Spine 2021, 46, 538–549. [Google Scholar] [CrossRef]
- Li, W.S.; Yan, Q.; Cong, L. Comparison of endoscopic discectomy versus non-endoscopic discectomy for symptomatic lumbar disc herniation: A systematic review and meta-analysis. Glob. Spine J. 2022, 12, 1012–1026. [Google Scholar] [CrossRef] [PubMed]
- Kambin, P.; Sampson, S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin. Orthop. Relat. Res. 1986, 207, 37–43. [Google Scholar] [CrossRef]
- Hijikata, S. Percutaneous nucleotomy. A new concept technique and 12 years’ experience. Clin. Orthop. Relat. Res. 1989, 238, 9–23. [Google Scholar]
- Yeung, A.T.; Tsou, P.M. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine 2002, 27, 722–731. [Google Scholar]
- Ahn, Y.; Lee, S.H.; Park, W.M.; Lee, H.Y.; Shin, S.W.; Kang, H.Y. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: Surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine 2004, 29, E326–E332. [Google Scholar] [CrossRef] [PubMed]
- Birkenmaier, C.; Komp, M.; Leu, H.F.; Wegener, B.; Ruetten, S. The current state of endoscopic disc surgery: Review of controlled studies comparing full-endoscopic procedures for disc herniations to standard procedures. Pain Physician 2013, 16, 335–344. [Google Scholar]
- Hofstetter, C.P.; Ahn, Y.; Choi, G.; Gibson, J.N.A.; Ruetten, S.; Zhou, Y.; Li, Z.Z.; Siepe, C.J.; Wagner, R.; Lee, J.H.; et al. AOSpine consensus paper on nomenclature for working-channel endoscopic spinal procedures. Glob. Spine J. 2020, 10, 111S–121S. [Google Scholar] [CrossRef]
- Cho, J.Y.; Lee, S.H.; Lee, H.Y. Prevention of development of postoperative dysesthesia in transforaminal percutaneous endoscopic lumbar discectomy for intracanalicular lumbar disc herniation: Floating retraction technique. Minim. Invasive Neurosurg. 2011, 54, 214–218. [Google Scholar] [CrossRef]
- Choi, I.; Ahn, J.O.; So, W.S.; Lee, S.J.; Choi, I.J.; Kim, H. Exiting root injury in transforaminal endoscopic discectomy: Preoperative image considerations for safety. Eur. Spine J. 2013, 22, 2481–2487. [Google Scholar]
- Ahn, Y.; Yoo, B.R.; Jung, J.M. The irony of the transforaminal approach: A comparative cohort study of transforaminal endoscopic lumbar discectomy for foraminal versus paramedian lumbar disc herniation. Medicine 2021, 100, e27412. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.B.; Lee, S.H.; Ahn, Y.; Kim, J.M. Risk factor for unsatisfactory outcome after lumbar foraminal and far lateral microdecompression. Spine 2006, 31, 1163–1167. [Google Scholar]
- Bae, J.S.; Kang, K.H.; Park, J.H.; Lim, J.H.; Jang, I.T. Postoperative clinical outcome and risk factors for poor outcome of foraminal and extraforaminal lumbar disc herniation. J. Korean Neurosurg. Soc. 2016, 59, 143–148. [Google Scholar] [PubMed]
- Dennis, R. Optimal magnetic resonance imaging of the spine. Vet. Radiol. Ultrasound 2011, 52, S72–S80. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Zhu, L.; Jiang, Z.L.; Wu, X.T. Radiological risk factors for recurrent lumbar disc herniation after percutaneous transforaminal endoscopic discectomy: A retrospective matched case-control study. Eur. Spine J. 2021, 30, 886–892. [Google Scholar]
- Fardon, D.F.; Milette, P.C.; Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine 2001, 26, E93–E113. [Google Scholar]
- Lee, S.; Lee, J.W.; Yeom, J.S.; Kim, K.J.; Kim, H.J.; Chung, S.K.; Kang, H.S. A practical MRI grading system for lumbar foraminal stenosis. Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef]
- Park, H.J.; Kim, S.S.; Lee, S.Y.; Park, N.H.; Rho, M.H.; Hong, H.P.; Kwag, H.J.; Kook, S.H.; Choi, S.H. Clinical correlation of a new MR imaging method for assessing lumbar foraminal stenosis. Am. J. Neuroradiol. 2012, 33, 818–822. [Google Scholar]
- Macnab, I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J. Bone Jt. Surg. Am. 1971, 53, 891–903. [Google Scholar] [CrossRef]
- de Carvalho, P.S.T.; Ramos, M.R.F.; da Silva Meireles, A.C.; Peixoto, A.; de Carvalho, P., Jr.; Ramírez León, J.F.; Yeung, A.; Lewandrowski, K.U. Feasibility of using intraoperative neuromonitoring in the prophylaxis of dysesthesia in transforaminal endoscopic discectomies of the lumbar spine. Brain Sci. 2020, 10, 522. [Google Scholar] [CrossRef] [PubMed]
- Jeong, T.S.; Ahn, Y.; Lee, S.G.; Kim, W.K.; Son, S.; Kwon, J.H. Correlation between MRI grading system and surgical findings for lumbar foraminal stenosis. J. Korean Neurosurg. Soc. 2017, 60, 465–470. [Google Scholar] [PubMed]
| Items | Total (N = 75) | ||
|---|---|---|---|
| Age (years), mean, SD | 61.2 | 10.5 | |
| Sex | Male | 24 | 32.0% |
| Female | 51 | 68.0% | |
| BMI (kg/m2), mean, SD | 23.7 | 3.5 | |
| Symptom Duration | Acute | 8 | 10.7% |
| Subacute | 11 | 14.7% | |
| Chronic | 56 | 74.6% | |
| Level | L2–3 | 3 | 4.0% |
| L3–4 | 12 | 16.0% | |
| L4–5 | 31 | 41.3% | |
| L5–S1 | 29 | 38.7% | |
| Side | Left | 39 | 52.0% |
| Right | 36 | 48.0% | |
| LDH Type | Extruded | 64 | 85.3% |
| Protruded | 9 | 12.0% | |
| Bulging, diffuse | 2 | 2.7% | |
| LDH Zone | Foraminal | 53 | 70.7% |
| Extraforaminal | 22 | 29.3% | |
| Grade (foraminal narrowing) | 1 | 8 | 10.7% |
| 2 | 26 | 34.7% | |
| 3 | 41 | 54.6% | |
| Items | Variables | Coefficient (β) | 95% CI | p-Value | Model Fit |
|---|---|---|---|---|---|
| Operative time | FS grade | 21.77 | [6.65, 36.89] | 0.005 | R2 = 0.165 |
| Hospital stay | FS grade | 1.16 | [0.35, 1.98] | 0.006 | R2 = 0.184 |
| Access pain | Zone of LDH | 2.44 | [0.80, 4.08] | 0.003 | Rp2 = 0.2737 |
| Procedure pain | No predictors | - | - | >0.05 | Rp2 = 0.0776 |
| Macnab | No predictors | - | - | >0.05 | Rp2 = 0.1198 |
| Items | Variables | Coefficient (β) | 95% CI | p-Value | Model Fit |
|---|---|---|---|---|---|
| Operative time | Access pain | 21.78 | [9.54, 34.02] | 0.001 | R2 = 0.159 |
| Procedure pain | −1.29 | [−13.11, 10.52] | 0.828 | ||
| Hospital stay | Access pain | 1.50 | [0.40, 2.60] | 0.008 | R2 = 0.101 |
| Procedure pain | −0.88 | [−1.94, 0.18] | 0.101 | ||
| Macnab | Access pain | 0.73 | [−0.86, 2.32] | 0.365 | Rp2 = 0.0113 |
| Procedure pain | −0.43 | [−2.21, 1.35] | 0.637 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, Y.; Bae, S.; Jo, D.-J.; Yoo, B.-R. Magnetic Resonance Imaging Predictors of Surgical Difficulty in Transforaminal Endoscopic Lumbar Discectomy for Far-Lateral Disc Herniation Under Local Anesthesia. Biomedicines 2025, 13, 778. https://doi.org/10.3390/biomedicines13040778
Ahn Y, Bae S, Jo D-J, Yoo B-R. Magnetic Resonance Imaging Predictors of Surgical Difficulty in Transforaminal Endoscopic Lumbar Discectomy for Far-Lateral Disc Herniation Under Local Anesthesia. Biomedicines. 2025; 13(4):778. https://doi.org/10.3390/biomedicines13040778
Chicago/Turabian StyleAhn, Yong, Sungsoo Bae, Dae-Jean Jo, and Byung-Rhae Yoo. 2025. "Magnetic Resonance Imaging Predictors of Surgical Difficulty in Transforaminal Endoscopic Lumbar Discectomy for Far-Lateral Disc Herniation Under Local Anesthesia" Biomedicines 13, no. 4: 778. https://doi.org/10.3390/biomedicines13040778
APA StyleAhn, Y., Bae, S., Jo, D.-J., & Yoo, B.-R. (2025). Magnetic Resonance Imaging Predictors of Surgical Difficulty in Transforaminal Endoscopic Lumbar Discectomy for Far-Lateral Disc Herniation Under Local Anesthesia. Biomedicines, 13(4), 778. https://doi.org/10.3390/biomedicines13040778





