Abstract
Purpose: The purpose of this study was to assess the relationship between the radiological criteria determining an primary empty or primary partial empty sella and the pituitary hormone levels. Methods: Out of 594 patients who underwent pituitary magnetic resonance imaging (MRI), we selected 43 patients with primarily empty and partial empty sella and conducted a prospective evaluation of pituitary MRI in 2022. Pituitary craniocaudal (CC) diameter, pituitary volume, sellar volume, pituitary volume expressed as a percentage of sellar volume (bony sella), and pituitary height expressed as a percentage of sellar height (craniocaudal) were assessed. Serum pituitary hormone concentrations were measured, and a logistic regression analysis was performed to assess a relationship between the radiological and hormonal parameters. Results: Only six patients (14%) exhibited abnormal hormone levels. None of the assessed radiological parameters were correlated with the presence of the hormonal disorders either in the univariate or multivariate logistic regression analysis. The univariate logistic regression analysis revealed a significant relationship between age and the hormonal disorders (OR 0.916 [0.844–0.993]; p = 0.034), but this was not confirmed in the multivariate analysis. Conclusions: These findings suggest that radiological parameters alone are insufficient to predict hormonal dysfunction in patients with empty or partial empty sella. However, younger patients may be at a higher risk, warranting closer hormonal monitoring.
1. Introduction
Located in the middle cranial fossa, the sella turcica is formed by the middle part of the superior surface of the sphenoid body, which is posterior to the tuberculum sellae and prechiasmatic sulcus, anterior to the dorsum sellae, and medial to the carotid sulcus on either side. An indentation in the sella turcica, known as the hypophyseal fossa, houses the pituitary gland [1,2,3]. The anterior lobe of the pituitary (adenohypophysis) is composed of cell lines producing hormones (growth hormone, prolactin, adrencorticotropic hormone, thyroid-stimulating hormone, luteinizing hormone, and follicle-stimulating hormone), whereas its posterior lobe (neurohypophysis) stores and releases oxytocin and antidiuretic hormone [4]. The formation of the pituitary gland from the Rathke’s pouch and from an elevation in the floor of the third ventricle precedes the formation of the sella turcica and thus affects its structure. As a result, the close relationship between these two structures begins during embryogenesis. Sellar enlargement may be associated with pituitary pathologies, such as adenomas or cysts; conversely, a reduced sellar size may be associated with primary hypopituitarism or growth hormone deficiency [4,5].
An empty or partial empty sella results from the subarachnoid space becoming herniated into the sella turcica and compressing the pituitary gland [6]. This condition may be caused by congenital absence or weakening of the diaphragma sellae due to changes in intracranial pressure or pituitary volume (e.g., during pregnancy). Such conditions are classified as a primary empty or partial empty sella [6,7,8,9]. In contrast, a secondary empty or partial empty sella may be due to a neurosurgical intervention, cranial injury, pituitary apoplexy, tumor, hyperplasia, or inflammation [6,7,8,9]. The prevalence of empty sella based on pituitary magnetic resonance imaging (MRI) or on clinical criteria varies in various reports, ranging from 2% to 35% [10,11,12]. Up to 79% of empty sella diagnoses are incidental, with as many as 50% of these patients exhibiting hypopituitarism [4]. An empty sella has been revealed in 5.5–12% of postmortem examinations and in up to approximately 12% of imaging studies, while its prevalence in patients with idiopathic intracranial hypertension may reach 70–94% [4,10]. The discrepancies in the reported rates of empty or partial empty sellae may be due to adopting various criteria in defining the condition [7]. An empty sella is usually defined as a herniation of the subarachnoid space into the hypophyseal fossa to take up more than 50% of its volume and flattening the pituitary to less than 3 mm craniocaudally, whereas a partial empty sella is characterized by the pituitary measuring at least 3 mm craniocaudally, with less than 50% of the sella volume filled with the cerebrospinal fluid [7,9,13,14,15]. The discrepancies in the reported prevalence of empty sella may be due to the adopted definition using a fixed cutoff pituitary height or proportion of the pituitary–sella volume; alternatively, they may be due to the varying resolution of the scans, which has changed over time. Pituitary height (i.e., its CC diameter) is not the only radiological feature of empty or partial empty sella. The effects of the suprasellar cistern compression, such as pituitary flattening, infundibular displacement or bending, and sellar volume enlargement, are not only additional radiological features of empty or partial empty sella but may also be predictors of endocrine disorders [16,17]. Apart from these established radiological features, there are also others that are not commonly considered, such as pituitary anteroposterior (AP) and transverse diameters, pituitary volume, sellar diameters, sellar volume, and correlations between pituitary volume and sellar volume.
The purpose of this study was to radiologically assess patients with empty and partial empty sella and to assess the relationship between the radiological criteria that define an empty or partial empty sella and hormonal disorders—not only by determining the prevalence of these phenomena but also by calculating the risk of endocrine disorders in this patient population.
2. Material and Methods
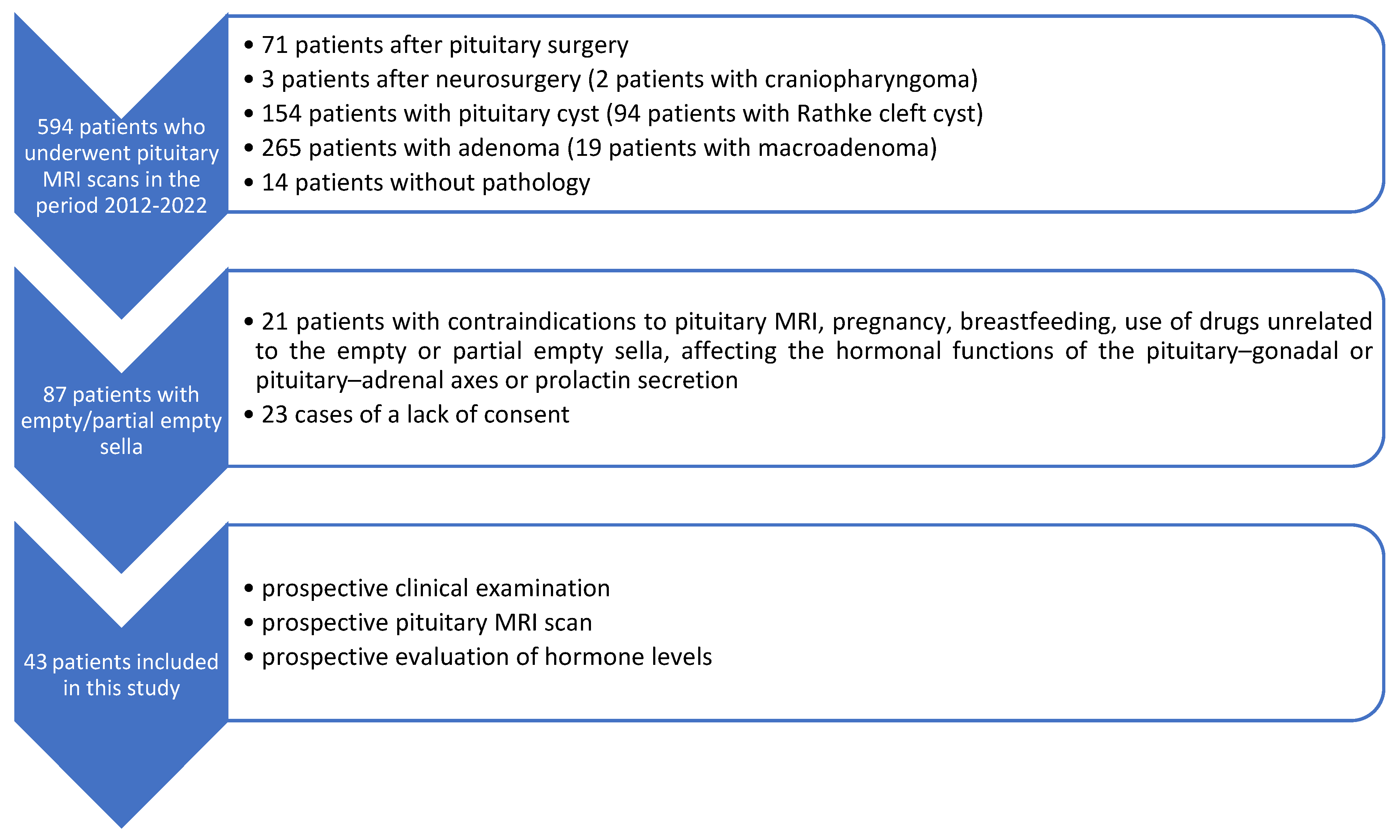
In order to conduct this study, we reviewed data from the Department of Diagnostic Radiology (National Medical Institute of the Ministry of the Interior and Administration, Warsaw, Poland) database from the years 2012–2022. We found 594 cases of patients who underwent pituitary MRI scans in order to visualize (a) primary or secondary empty or partial empty sella previously detected with MRI of the central nervous system; (b) status post neurosurgery on the central nervous system, including craniopharyngioma surgery; (c) status post pituitary surgery; (d) Rathke’s cleft cyst; and (e) pituitary adenoma (Figure 1). Eighty-seven of those patients exhibited morphological features of an empty or partial empty sella. These 87 patients were then assessed prospectively in terms of study inclusion criteria. The study inclusion criteria were age over 18 years and primary empty or primary partial empty sella in pituitary MRI. The study exclusion criteria were history of surgical interventions or irradiation of the central nervous system, a tumor of the pituitary gland or central nervous system, pregnancy, breastfeeding, the use of medications unconnected with empty or partial empty sella affecting endocrine function of the pituitary–gonadal or pituitary–adrenal axes or prolactin secretion, contraindications to pituitary MRI, and a lack of patient’s consent.

Figure 1.
Flow diagram presenting the process of collecting the data included in this study.
Out of the patients with primary empty or partial empty sella, we ultimately included 43 patients who underwent another prospective pituitary MRI scan performed by an experienced radiologist, the same one each time. The time interval between the previous and the current pituitary MRI scans was 3.651 ± 1.675 years; there were no differences between these scans. Based on the existing definitions, we defined an empty sella as a herniation of the subarachnoid space into the sella turcica exceeding 50% of its volume and leading to the flattening of the pituitary to a craniocaudal diameter of less than 3 mm, whereas partial empty sella was diagnosed when the craniocaudal diameter of the pituitary was greater than or equal to 3 mm and less than 50% of the sella turcica volume was occupied by the cerebrospinal fluid [9,13,14,15,17].
Each patient underwent pituitary and optic nerve MRI at the Department of Diagnostic Radiology with the use of a 3.0 Tesla scanner, with a slice thickness of 2 mm, slice gap of 0, field of view 150/150, matrix 240/300, and pixel alimentation of 0.5 × 0.625 mm. A pituitary protocol was used, with T1-weighted (+Dixon), T2-weighted, FLAIR, T2 STIR, and contrast-enhanced T1-weighted sequences being obtained. The AP, coronal (right–left, RL), and CC diameters of the pituitary, the sella turcica, and the optic nerve sheath were measured. Tortuous optic nerves, enlarged cerebrospinal fluid spaces, and critical stenosis of the transverse or sigmoid sinus were taken into consideration. The pituitary volume was calculated manually based on a simplified ellipsoid formula (volume = 0.5 × AP × RL × CC). The sellar volume was calculated based on a simplified ellipsoid formula (volume = 0.5 × AP × RL × CC). The craniocaudal diameter of the sella turcica was based either on the bony landmarks or, alternatively, only on the location of the diaphragma sellae. Taking into account previous diagnoses and current medications, the patients included in this study underwent hormone profile assessments, fasting blood tests in the morning at about 8:00 a.m. after sleeping through the night, and a urine test from a morning sample. In order to assess anterior pituitary function, adrenocorticotropic hormone (ACTH), cortisol, growth hormone, insulin-like growth factor 1 (IGF-1), prolactin, thyroid-stimulating hormone (TSH), free triiodothyronine (fT3), free thyroxine (fT4), follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol, and testosterone levels were measured; to indirectly assess posterior pituitary function, urine-specific gravity, serum osmolality, urine osmolality, and sodium and potassium levels were measured.
Previously diagnosed hormonal disorders due to empty or partial empty sella were taken into account during clinical examination in accordance with current standards [18]. Hyperprolactinemia was diagnosed when routine blood samples (morning fasting, after a night of regular sleep, and after a rest) showed elevated prolactin levels or when such a finding had been observed on previous clinical assessments and other potential causes (e.g., stress or medication) had been excluded. Diagnosis of secondary adrenocortical insufficiency was based on low ACTH and cortisol levels in conjunction with manifestations of adrenocortical insufficiency (orthostatic hypotension, syncope, nausea, vomiting, anorexia, weight loss, skin hypopigmentation, and hypoglycemia) and, in case of any uncertainties, was additionally confirmed with synthetic corticotropin-releasing hormone tests. The criteria adopted for diagnosing secondary hypothyroidism were low TSH levels together with low fT3 and fT4 levels and associated symptoms (hair loss, dry skin, cold intolerance, psychomotor retardation, constipation, bradycardia, hoarseness, anemia, or hyperlipidemia), and uncertain cases were decided with a thyrotropin-releasing hormone test. Growth hormone deficiency was diagnosed based on the following criteria: low IGF-1 levels in conjunction with symptoms (hypoglycemia, hyperlipidemia, weakness, low muscle mass, abdominal obesity, and low bone mineral density) or a test with insulin. The criteria adopted for determining sex hormone deficiency were low LH and FSH levels in conjunction with low estradiol levels and symptoms (amenorrhea in women of reproductive age; low libido; and a lack of or atrophy of secondary sex characteristics, namely, pubic hair) in females and low LH levels in conjunction with low testosterone levels and symptoms (low libido; erectile dysfunction; and a lack of or atrophy of secondary sex characteristics, namely, pubic hair) in males. Diabetes insipidus was excluded based on such criteria as a serum osmolality of <295 mOsm/kg H2O concurrent with a urine osmolality of >600 mOsm/kg H2O while taking into consideration that this diagnosis can be only established based on a water-deprivation–vasopressin test.
Based on these homogeneous criteria, the selected patients were divided into 2 groups: Group 1: patients with no hormonal disorders (n = 37) and Group 2: patients with hormonal disorders (n = 6).
The statistical analysis was conducted with Statistica® software (13.3), licensed for use by the Medical University of Warsaw. Statistical significance was determined with the use of tests suitable for the nature of data and the type of data distribution (verified with the Shapiro–Wilk W test) and variance homogeneity (verified with Brown–Forsythe’s test). Continuous variables were presented as means ± SD and medians and ranges, and the comparisons were made using either Student’s t-test for normally distributed variables with homogeneous variances or the Mann–Whitney U test for dependent variables showing departures from either normal distribution or variance homogeneity. Nominal variables were presented as absolute numbers and percentages and compared using either the chi-square test or Fisher’s exact test. A multivariate and univariate logistic regression models was used to determine the statistical significance of the evaluated variables in predicting hormonal disorders (adrenocortical insufficiency and hyperprolactinemia). The regression results were presented as odds ratios (OR) with 95% confidence intervals (95% CIs).
This study was approved by the ethics committee at the Medical University of Warsaw (approval No. KB/66/2022 of 16 May 2022). Each patient signed a written informed consent. This study was conducted according to the current standards, such as the Declaration of Helsinki.
3. Results
A total of six patients were found to have hormonal disorders. Four patients with hormonal disorders were found to have an empty sella (with the pituitary measuring less than 3 mm craniocaudally), and two were found to have a partial empty sella. The volume of suprasellar cistern herniation into the sella turcica exceeded 50% of sellar volume in all patients.
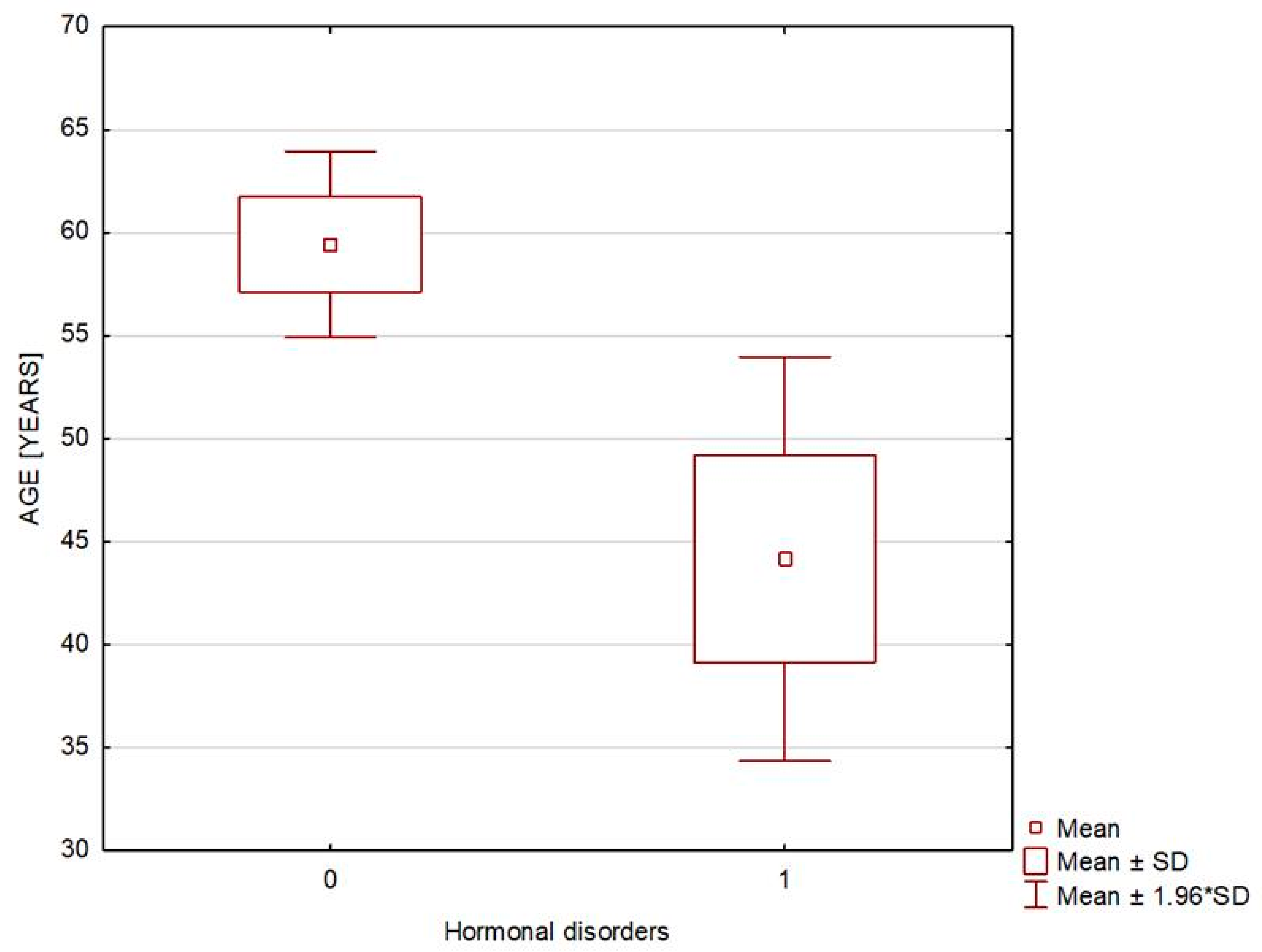
The patients from both study groups had good hormonal control, and the two groups differed only in electrolyte levels, which—nonetheless—stayed within normal limits. There was also a statistically significant difference in the waist circumference, body weight, and body mass index, all of which were higher in Group 1; however, there were no demonstrable differences in the rates of overweight or obesity. The two study groups differed in terms of patient age, with the hormonal disorder group significantly younger (Table 1 and Figure 2). Hyperprolactinemia was detected in four and secondary adrenocortical insufficiency in three of the patients with endocrine disorders. Two patients were receiving dopaminergic receptor agonists due to previously diagnosed hyperprolactinemia (associated with empty sella in one patient and with partial empty sella in the other). The two remaining patients, who were newly diagnosed with hyperprolactinemia (associated with empty sella in one patient and with partial empty sella in the other), were recommended to undergo outpatient follow-up assessments. All the patients with secondary adrenocortical insufficiency demonstrated an empty sella on MRI and were already receiving glucocorticoid replacement (Hydrocortisonum) due to the diagnosis having been established previously. None of the evaluated patients met the diagnostic criteria of growth hormone deficiency, hypogonadotropic hypogonadism, or diabetes insipidus (Table 2 and Table 3).

Table 1.
Clinical characteristics. Group 1: patients without hormonal disorders (n = 37); Group 2: patients with hormonal disorders (n = 6).

Figure 2.
In figure, 0—patients without hormonal disorders (Group 1) and 1—patients with hormonal disorders (Group 2), broken down by age.

Table 2.
Group 1 and Group 2 characteristics; Group 1: patients without hormonal disorders (n = 37), and Group 2: patients with hormonal disorders (n = 6).

Table 3.
Hormone levels in patients with endocrine disorders.
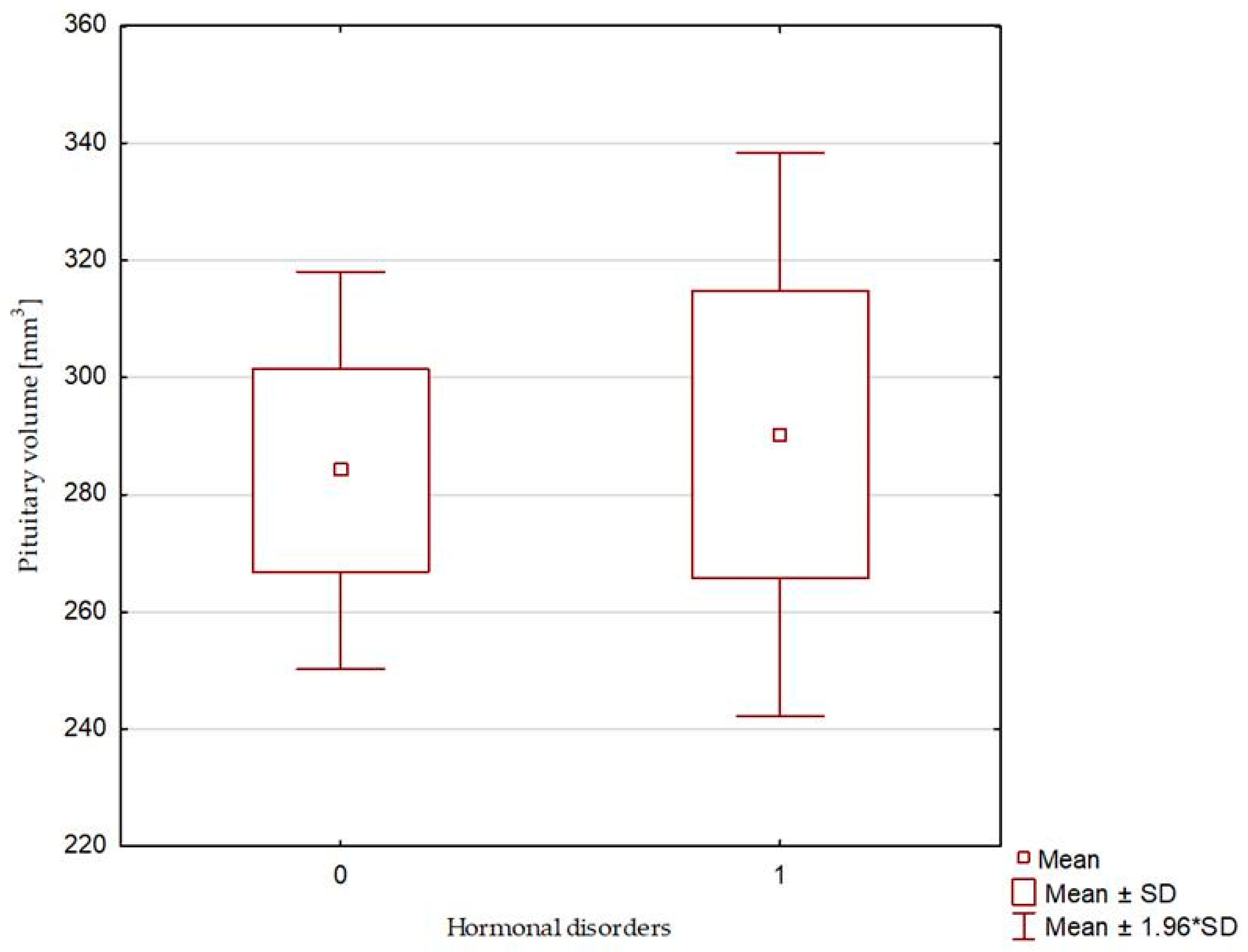
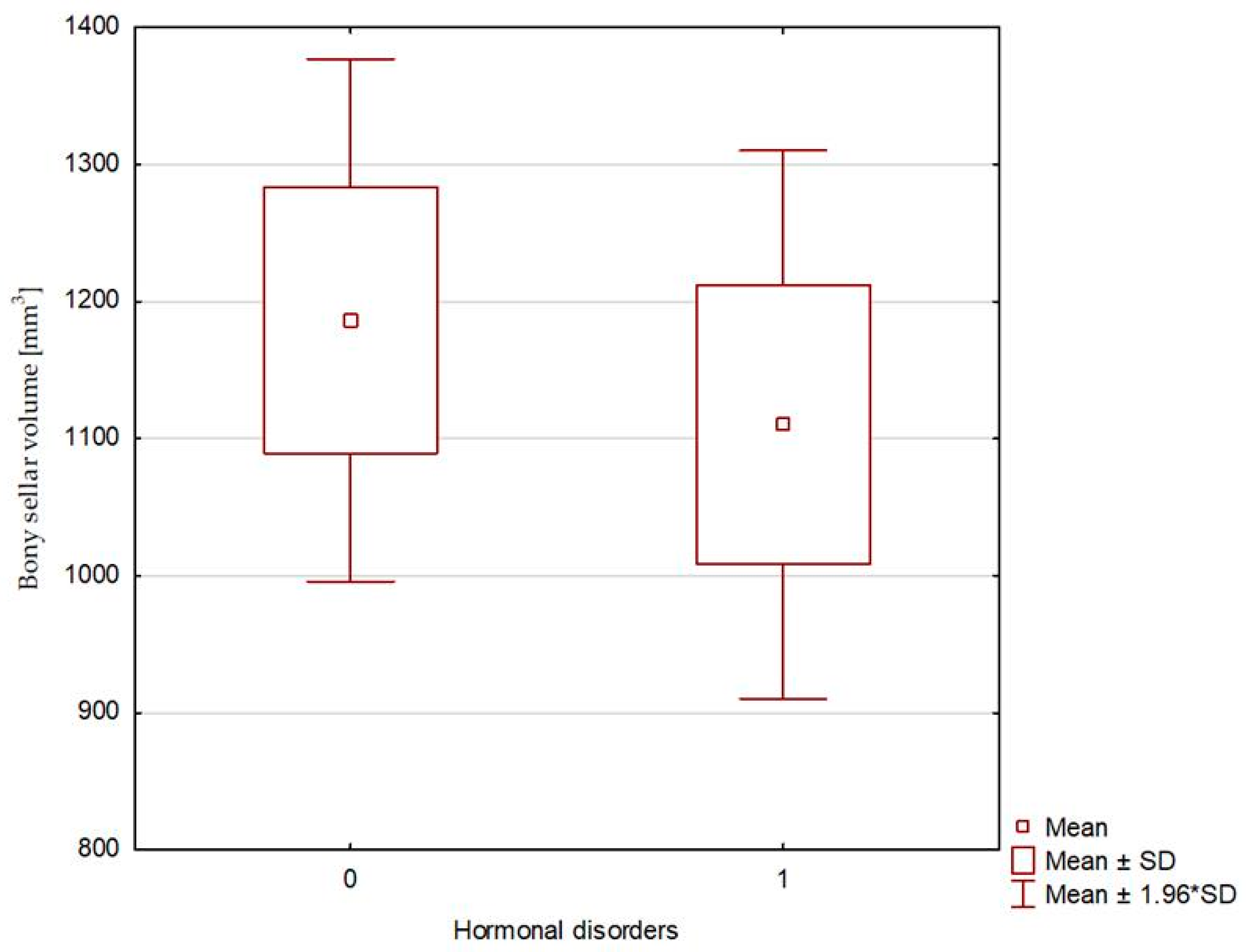
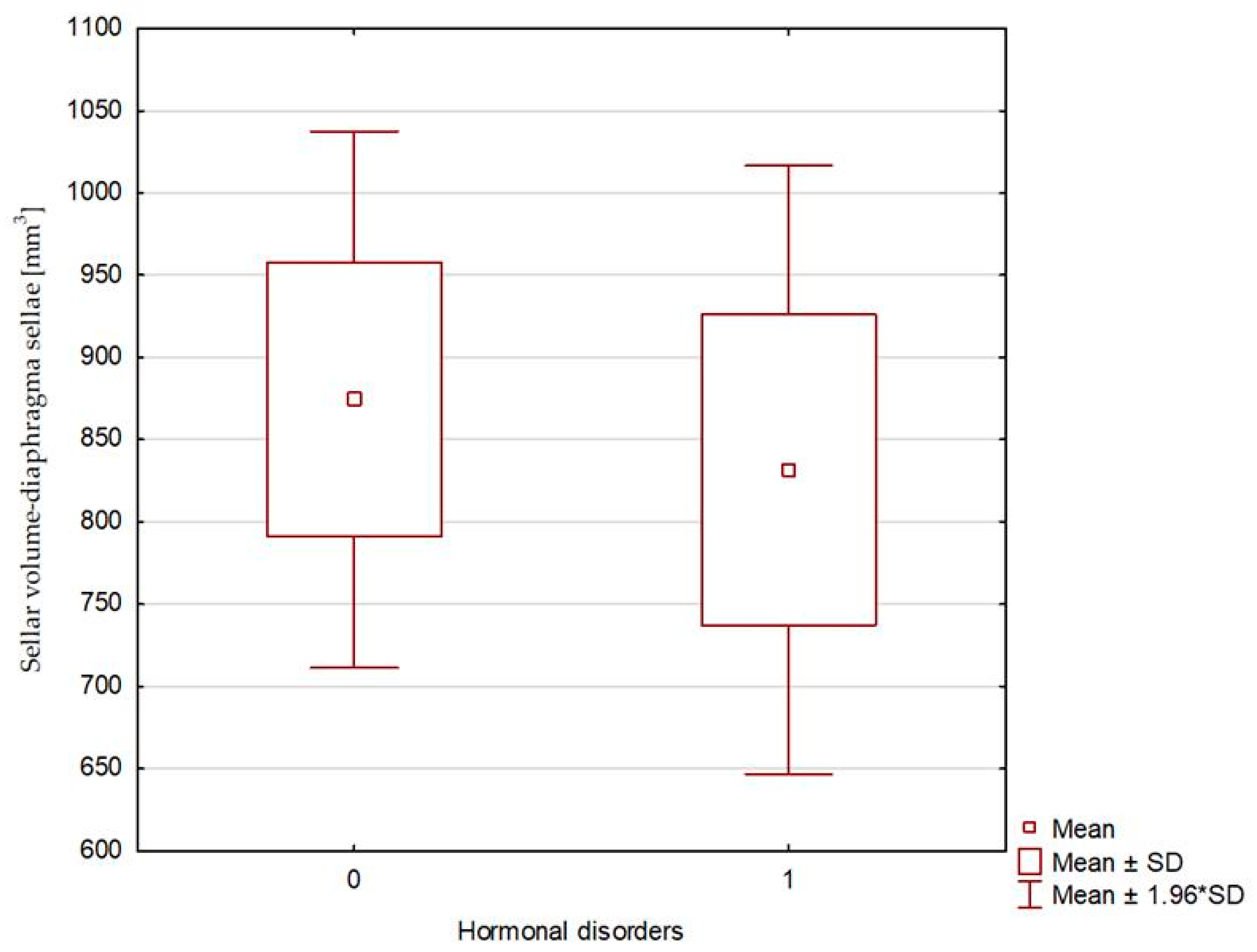
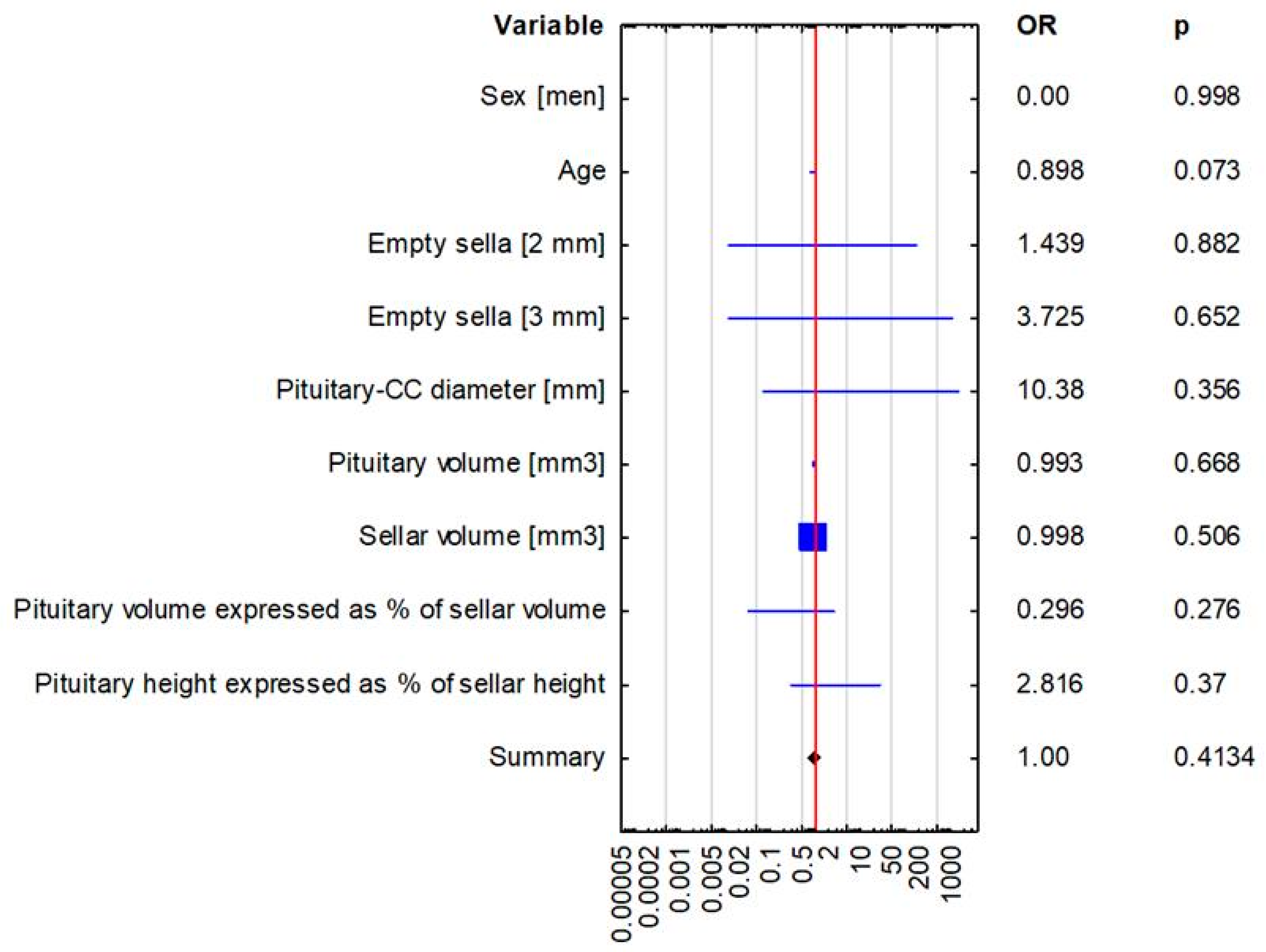
The compared study groups showed no differences in terms of the radiological parameters of either the pituitary or the sella turcica, or the relative pituitary-to-sellar volume or height (Table 4 and Figure 3, Figure 4 and Figure 5). Multivariate logistic regression showed no significant relationship between the evaluated radiological parameters and the development of hormonal disorders. The univariate logistic regression analysis revealed a significant relationship between age and the hormonal disorders (OR 0.916 [0.844–0.993]; p = 0.034), but this was not confirmed in the multivariate analysis (Table 5 and Figure 6). In our study, no patient exhibited evidence of posterior scleral flattening or critical transverse or sigmoid sinus stenosis; 11 patients showed enlarged cerebrospinal fluid spaces (dilated ventricles).

Table 4.
Radiologic characteristics of the patients. Group 1: patients without hormonal disorders (n = 37), and Group 2: patients with hormonal disorders (n = 6).

Figure 3.
Pituitary volume. 0—patients without hormonal disorders (Group 1), and 1—patients with hormonal disorders (Group 2).

Figure 4.
Sellar volume—calculated based on bony landmarks: 0—patients without hormonal disorders (Group 1), and 1—patients with hormonal disorders (Group 2).

Figure 5.
Sellar volume—calculated based on the location of the diaphragma sellae: 0—patients without hormonal disorders (Group 1), and 1—patients with hormonal disorders (Group 2).

Table 5.
Multivariate and univariate logistic regression in the assessment of the predictors of hormonal disorders (adrenocortical insufficiency and hyperprolactinemia).

Figure 6.
Multivariate logistic regression analysis in the assessment of predictors of hormonal disorders (adrenocortical insufficiency and hyperprolactinemia).
4. Discussion
Empty sella syndrome may produce neurological symptoms, such as headaches or visual disturbances, and endocrine manifestations, such as hyperprolactinemia or hypopituitarism [6,8]. These abnormalities usually prompt pituitary MRI, which may show evidence of empty or partial empty sella. However, in clinical practice, an empty or partial empty sella is more commonly detected incidentally on a scan performed for another reason on MRI and the patient is subsequently referred for further clinical evaluations and hormone tests [14,19,20]. In such cases, the radiological criteria for diagnosing an empty or partial empty sella and their correlation with hormonal disorders are of utmost importance.
Generally, an empty sella has been defined as herniation of the subarachnoid space into the sella turcica occupying more than 50% of its volume, which leads to pituitary flattening to less than 3 mm craniocaudally, whereas a partial empty sella has been characterized by the craniocaudal diameter of the pituitary being equal to or greater than 3 mm, with the cerebrospinal fluid occupying less than 50% of sellar volume [5,13,14,15]. Some authors have adopted the cutoff craniocaudal diameter of the pituitary to be 2 mm [9,15]. Moreover, some authors consider only either the criterion of pituitary craniocaudal diameter or the percentage of the sella occupied by the suprasellar cistern, with the latter most commonly determined by a cutoff of 50%, but other cutoff percentages, for example, 60%, have also been reported [14]. Depending on the pituitary height in relation to the sellar height measured in midsagittal T1-weighted images, the following grades of pituitary height loss have been defined: I—no pituitary height loss, II—mild loss of pituitary height by <1/3 of sellar height, III—moderate loss of pituitary height (between 1/3 and 2/3 of sellar height), IV—severe loss of pituitary height of more than 2/3 of sellar height, and V—total empty sella [21]. The radiological finding of an empty or a partial empty sella may be a manifestation of idiopathic intracranial hypertension. Other manifestations include flattening of the posterior scleral surface, transverse or sigmoid sinus stenosis, optic nerve sheath dilation, and optic nerve tortuosity [17]. The etiology of idiopathic increase in cerebrospinal fluid pressure above 250 mmHg H2O is unknown; however, risk factors of this condition are similar to those of empty or partial empty sella, which are obesity, the female sex, and reproductive age [22,23]. One of the suspected risk factors for idiopathic intracranial hypertension in patients with obesity is hyperaldosteronism. Aldosterone is known to increase the activity of the sodium–potassium pump that transports sodium ions from the cytoplasm of choroid epithelial cells into the cerebrospinal fluid, which causes the cerebrospinal fluid to experience an influx of sodium ions and, consequently, to increase in volume [22,23,24]. Another known effect of hyperaldosteronism is a drop in serum potassium levels. Our patients with empty and partial empty sella and endocrine disorders showed low normal serum potassium levels, which may be associated either with aldosterone levels in these patients or with the dose of hydrocortisone used as glucocorticoid replacement due to adrenocortical insufficiency. Hormonal disorders are not only known to result from empty or partial empty sella but also to be a risk factor for its development via their effects on intracranial pressure [17,25,26]. Examples of hormones with this potential effect are estrogens, which reduce aquaporin expression in hepatocytes and may theoretically exert a similar effect on the permeability of nervous system cells and increasing intracranial pressure [7,25,26,27]. Young women are known to have high estrogen levels, which is consistent with the characteristics of our study group with endocrine disorders, who comprised only women—young and overweight—although less overweight than patients without hormonal disorders.
Hormonal disorders were detected in six of the patients taking part in our study. Four were diagnosed with hyperprolactinemia and three with secondary adrenocortical insufficiency. Hyperprolactinemia is the most common endocrine disorder in patients with empty (or partial empty) sella syndrome, affecting 10–37.5% of patients with this diagnosis. Hyperprolactinemia may be associated with pituitary stalk compression and inhibition of hypothalamic dopamine release, while dopamine acts as a prolactostatin [7,28,29]. Adrenocortical insufficiency may affect up to 37.5% of patients, being more common in patients with empty sella than in those with partial empty sella. The pathogenesis of corticotropic cell dysfunction may be associated with their location in the anterior pituitary, which seems to make them more prone to compression by the suprasellar cistern [30,31].
The two evaluated groups did not differ significantly either in terms of an AP, an RL, or a CC diameter of the pituitary or in terms of pituitary volume. Similarly, there were no inter-group differences in terms of sellar dimensions or volume. The evaluated groups showed no differences in the relative pituitary-to-sellar volume, which determines the degree to which the sella is filled by the suprasellar cistern.
The multivariate logistic regression analysis conducted in our study showed no evidence to support that pituitary or sellar volume or any other radiographic parameters may be independent risk factors of hormonal disorders in patients with an empty or partial empty sella. The univariate logistic regression analysis revealed the patient’s age to be a risk factor of hormonal disorders, with younger patients with an empty or partial empty sella being at a significantly greater risk of developing hormonal disorders.
Similar conclusions regarding pituitary volume have been presented by other authors. A study evaluating the pituitary volume in the elderly showed no relationship between hormonal disorders and either empty sella or pituitary volume [32]. Another study showed age- and sex-related differences in pituitary volume between patients with empty and partial empty sella and patients without such a diagnosis, with an empty or partial empty sella associated with a more rapid loss of pituitary volume with increasing age. However, there was no demonstrable relationship between hormonal disorders and pituitary volume [33]. Pituitary volume is known to change with age and as a result of specific clinical situations associated with pituitary hormone secretion, such as pregnancy or menopause in women [33,34,35]. Generally, a normal pituitary measures up to 12 mm in width, 8 mm in the AP diameter, and 9 mm in height [36]. More specifically, normal pituitary height is up to 6 mm in children under 12 years old, up to 10 mm in adolescents, up to 9 mm in young adult women, up to 8 mm in young adult men, and up to 12 mm during pregnancy. After the age of 50 years, pituitary dimensions usually diminish; however, in the perimenopausal period, they may increase, although not to the extent observed during pregnancy [36]. The adopted dimensions of a normal sella turcica are 15 mm in length and 12 mm in depth, which nonetheless has no effect on hormonal disorders [37,38,39]. A different source provides the following morphometric parameters of the sella turcica—anterior height 6.71 mm (SE = 0.52); posterior height 6.93 (SE = 0.22); overall length 9.06 mm (SE = 0.15), specifically 8.94 mm (SE = 0.22) in females and 9.19 mm (SE = 0.26) in males; overall width 9.74 mm (SE = 0.31), specifically 9.78 mm (SE = 0.39) in females and 9.51 mm (SE = 0.4) in males; overall depth 8.00 mm (SE = 0.13); and overall volume 845.8 mm3. (SE = 0.5) [1]. According to these data, the sellae turcicae in our patients were enlarged, especially when bony sella dimensions are considered. We calculated the pituitary and sellar volume with the use of a simplified ellipsoid formula, since it is the most readily accessible one, particularly in everyday clinical practice. At the same time, we took into consideration reports on normal pituitary glands that stated that this method of calculating pituitary volume may yield underestimated results in comparison with stereological approaches, such as the point-counting method and the planimetric method; we also took into consideration other reports, which showed planimetric and linear methods to yield overestimated results [35,40].
A detailed assessment of the pituitary gland is an important part of every MRI examination of the central nervous system. The dimensions and volume not only of the pituitary but also of the sella turcica are helpful in diagnosing and assessing patients with empty or partial empty sella but do not conclusively determine hormonal disorders. In light of the above, the currently used, simple definitions of empty and partial empty sella, where the diagnostic criteria are pituitary size and the percentage of sellar volume occupied by the suprasellar cistern, seem to be still valid and highly reproducible. Due to the fact that hormonal imbalances have been detected in patients with empty and partial empty sella, this group of patients may require endocrine testing. It is worth noting that younger patients with empty or partial empty sella are at an increased risk of developing hormonal disorders, which should be considered in planning hormone level tests.
One limitation of our study is a small sample size; however, the study population was selected from a larger population, in which the evaluated condition is uncommon.
In the future, prospective multicenter studies should be carried out on a large group of patients newly diagnosed with empty or partial empty sella, with long follow-up periods, calculation of pituitary volume by different methods, and potential risk factor assessment, including assessment of the renin–angiotensin–aldosterone system.
5. Conclusions
Although radiologic parameters of the pituitary and sella turcica help assess and diagnose patients with empty or partial empty sella, they do not conclusively determine hormonal disorders. Younger patients with empty or partial empty sella seem (at least in the univariate analysis) to have a higher odds ratio for developing hormonal disorders, which should be considered while planning hormone level tests. These findings suggest that radiological parameters alone are insufficient to predict hormonal dysfunction in patients with empty or partial empty sella. However, younger patients may be at higher risk, warranting closer hormonal monitoring.
Author Contributions
B.K., E.F. and M.F. conceived the idea for this study. B.K., E.F. and M.F. contributed to the design of this research. All the authors were involved in data collection. B.K. analyzed the data. B.K. coordinated funding for this project. All authors have read and agreed to the published version of the manuscript.
Funding
The Polish Ministry of Education and Science from state budget resources as part of the “Student science clubs create innovations” program [grant number: SKN/SP/534669/2022].
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee at the Medical University of Warsaw (approval No. KB/66/2022 of 16 May 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated during and/or analyzed during the present study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Iskra, T.; Stachera, B.; Możdżeń, K.; Murawska, A.; Ostrowski, P.; Bonczar, M.; Gregorczyk-Maga, I.; Walocha, J.; Koziej, M.; Wysiadecki, G.; et al. Morphology of the Sella Turcica: A Meta-Analysis Based on the Results of 18,364 Patients. Brain Sci. 2023, 13, 1208. [Google Scholar] [CrossRef] [PubMed]
- Jankowski, T.; Jedliński, M.; Grocholewicz, K.; Janiszewska-Olszowska, J. Sella Turcica Morphology on Cephalometric Radiographs and Dental Abnormalities-Is There Any Association?—Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4456. [Google Scholar] [CrossRef] [PubMed]
- Bonczar, M.; Wysiadecki, G.; Ostrowski, P.; Michalczak, M.; Plutecki, D.; Wilk, J.; Michalik, W.; Walocha, J.; Balawender, K.; Iskra, T.; et al. The Morphology of the Pituitary Gland: A Meta-Analysis with Implications for Diagnostic Imaging. Brain Sci. 2023, 13, 89. [Google Scholar] [CrossRef]
- Rice-Canetto, T.E.; Carroll, P.; Reier, L.; Siddiqi, J. Asymptomatic Empty Sella: A Literature Review and Suggestions for Evaluation in Clinical Practice. Cureus 2024, 16, e75965. [Google Scholar] [CrossRef]
- Önal, V.; Evren, A.; Chatzioglou, G.O.N.; Tellioğlu, A.M. Anatomical features of sella turcica with comprehensive literature review. Rev. Assoc. Med. Bras. (1992) 2023, 69, e20230402. [Google Scholar] [CrossRef] [PubMed]
- Chiloiro, S.; Giampietro, A.; Bianchi, A.; Tartaglione, T.; Capobianco, A.; Anile, C.; De Marinis, L. Diagnosis of endocrine disease: Primary empty sella: A comprehensive review. Eur. J. Endocrinol. 2017, 177, 275–285. [Google Scholar] [CrossRef]
- Auer, M.K.; Stieg, M.R.; Crispin, A.; Sievers, C.; Stalla, G.K.; Kopczak, A. Primary Empty Sella Syndrome and the Prevalence of Hormonal Dysregulation. Dtsch. Arztebl. Int. 2018, 115, 99–105. [Google Scholar] [CrossRef]
- Guitelman, M.; Garcia Basavilbaso, N.; Vitale, M.; Chervin, A.; Katz, D.; Miragaya, K.; Herrera, J.; Cornalo, D.; Servidio, M.; Boero, L.; et al. Primary empty sella (PES): A review of 175 cases. Pituitary 2013, 16, 270–274. [Google Scholar] [CrossRef]
- Zuhur, S.S.; Kuzu, I.; Ozturk, F.Y.; Uysal, E.; Altuntas, Y. Anterior pituitary hormone deficiency in subjects with total and partial primary empty sella: Do all cases need endocrinological evaluation? Turk. Neurosurg. 2014, 24, 374–379. [Google Scholar] [CrossRef]
- Padovano Sorrentino, F.; Chiloiro, S.; Giampietro, A.; Bianchi, A.; Pontecorvi, A.; De Marinis, L. Empty sella syndrome: An update. Pituitary 2024, 28, 13. [Google Scholar] [CrossRef]
- Foresti, M.; Guidali, A.; Susanna, P. Primary empty sella. Incidence in 500 asymptomatic subjects examined with magnetic resonance. Radiol. Med. 1991, 81, 803–807. [Google Scholar] [PubMed]
- Gallardo, E.; Schächter, D.; Cáceres, E.; Becker, P.; Colin, E.; Martínez, C.; Henríquez, C. The empty sella: Results of treatment in 76 successive cases and high frequency of endocrine and neurological disturbances. Clin. Endocrinol. 1992, 37, 529–533. [Google Scholar] [CrossRef]
- Lupi, I.; Manetti, L.; Raffaelli, V.; Grasso, L.; Sardella, C.; Cosottini, M.; Iannelli, A.; Gasperi, M.; Bogazzi, F.; Caturegli, P.; et al. Pituitary autoimmunity is associated with hypopituitarism in patients with primary empty sella. J. Endocrinol. Investig. 2011, 34, 240–244. [Google Scholar]
- Cannavò, S.; Curtò, L.; Venturino, M.; Squadrito, S.; Almoto, B.; Narbone, M.C.; Rao, R.; Trimarchi, F. Abnormalities of hypothalamic-pituitary-thyroid axis in patients with primary empty sella. J. Endocrinol. Investig. 2002, 25, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Colao, A.; Cotta, O.R.; Ferone, D.; Torre, M.L.; Ferraù, F.; Di Somma, C.; Boschetti, M.; Teti, C.; Maria CSavanelli Alibrandi, A.; Trimarchi, F.; et al. Role of pituitary dysfunction on cardiovascular risk in primary empty sella patients. Clin. Endocrinol. 2013, 79, 211–216. [Google Scholar] [CrossRef]
- Chiloiro, S.; Giampietro, A.; Bianchi, A.; De Marinis, L. Empty sella syndrome: Multiple endocrine disorders. Handb. Clin. Neurol. 2021, 181, 29–40. [Google Scholar]
- Prabhat, N.; Kaur, K.; Takkar, A.; Ahuja, C.; Katoch, D.; Goyal, M.; Dutta, P.; Bhansali, A.; Lal, V. Pituitary Dysfunction in Idiopathic Intracranial Hypertension: An Analysis of 80 Patients. Can. J. Neurol. Sci. 2024, 51, 265–271. [Google Scholar] [CrossRef]
- Fleseriu, M.; Hashim, I.A.; Karavitaki, N.; Melmed, S.; Murad, H.M.; Salvatori, R.; Samuels, M.H. Hormonal Replacement in Hypopituitarism in Adults: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2016, 101, 3888–3921. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.; He, H.; Chen, Y.; Wang, C.; Zhu, Y.; Ye, X. Osteoporotic fractures and persistent non-fusion of the hand epiphyses caused by empty sella syndrome in an adult: A case report. J. Int. Med. Res. 2013, 41, 1768–1772. [Google Scholar] [CrossRef]
- Carosi, G.; Brunetti, A.; Mangone, A.; Baldelli, R.; Tresoldi, A.; Del Sindaco, G.; Lavezzi, E.; Sala, E.; Mungari, R.; Fatti, L.M.; et al. A multicenter Cohort Study in Patients with Primary Empty Sella: Hormonal and Neuroradiological Features Over a Long Follow-Up. Front. Endocrinol. 2022, 13, 925378. [Google Scholar] [CrossRef]
- Yuh, W.T.; Zhu, M.; Taoka, T.; Quets, J.P.; Maley, J.E.; Muhonen, M.G.; Schuster, M.E.; Kardon, R.H. MR imaging of pituitary morphology in idiopathic intracranial hypertension. J. Magn. Reson. Imaging JMRI 2000, 12, 808–813. [Google Scholar] [CrossRef] [PubMed]
- Barkatullah, A.F.; Leishangthem, L.; Moss, H.E. MRI findings as markers of idiopathic intracranial hypertension. Curr. Opin. Neurol. 2021, 34, 75–83. [Google Scholar] [CrossRef]
- Weber, K.T.; Singh, K.D.; Hey, J.C. Idiopathic intracranial hypertension with primary aldosteronism: Report of 2 cases. Am. J. Med. Sci. 2002, 324, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.U.; Khalid, H.; Salpietro, V.; Weber, K.T. Idiopathic intracranial hypertension associated with either primary or secondary aldosteronism. Am. J. Med. Sci. 2013, 346, 194–198. [Google Scholar] [CrossRef]
- Thaller, M.; Homer, V.; Sassani, M.; Mollan, S.P.; Sinclair, A.J. Longitudinal prospective cohort study evaluating prognosis in idiopathic intracranial hypertension patients with and without comorbid polycystic ovarian syndrome. Eye 2023, 37, 3621–3628. [Google Scholar] [CrossRef] [PubMed]
- Rzewuska, N.; Kunicki, J.; Pieniak, K.; Laskus, P.; Zabielska, B.; Smolarczyk, R.; Kunicki, M. A systematic review on idiopathic intracranial hypertension comorbid with polycystic ovarian syndrome and its consequences. Eur. J. Obstet. Gynecol. Reprod. Biol. 2024, 292, 1–7. [Google Scholar] [CrossRef]
- Thaller M, Mytton J, Wakerley BR, Mollan SP, Sinclair AJ. Idiopathic intracranial hypertension: Evaluation of births and fertility through the Hospital Episode Statistics dataset. BJOG 2022, 129, 2019–2027. [CrossRef] [PubMed] [PubMed Central]
- Leca, B.M.; Mytilinaiou, M.; Tsoli, M.; Epure, A.; Aylwin, S.J.B.; Kaltsas, G.; Randeva, H.S.; Dimitriadis, G.K. Identification of an optimal prolactin threshold to determine prolactinma size using receiver perating characteristic analysis. Sci. Rep. 2021, 11, 9801. [Google Scholar] [CrossRef]
- Alyami, N.; Alhenaki, G.; Al Atwah, S.; Alhenaki, N.; Smaisem, F.; Alotaibi, A.; Abu Risheh j Smaisem, M.; Alhenaki, A.; Alanazi, S.; Alshammeri, M.; et al. Correlation between MRI findings of pituitary gland and prolactin level among hyperprolactinemia adult female Saudi patients in rural areas: A retrospective multicentric study. Medicine 2025, 104, e40686. [Google Scholar] [CrossRef]
- Chen, H.C.; Sung, C.C. A young man with secondary adrenal insufficiency due to empty sella syndrome. BMC Nephrol. 2022, 23, 81. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Del Monte, P.; Foppiani, L.; Cafferata, C.; Marugo, A.; Bernasconi, D. Primary “empty sella” in adults: Endocrine findings. Endocr. J. 2006, 53, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Terano, T.; Seya, A.; Tamura, Y.; Yoshida, S.; Hirayama, T. Characteristic of the pituitary gland in elderly subjects from magnetic resonance images: Relationship to pituitary hormone secretion. Clin. Endocrinol. 1996, 45, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Akkus, G.; Sözütok, S.; Odabaş, F.; Onan, B.; Evran, M.; Karagun, B.; Sert, M.; Tetiker, T. Pituitary Volume in Patients with Primary Empty Sella and Clinical Relevance to Pituitary Hormone Secretion: A Retrospective Single Center Study. Curr. Med. Imaging 2021, 17, 1018–1024. [Google Scholar] [CrossRef]
- Kaess, M.; Simmons, J.G.; Whittle, S.; Jovev, M.; Chanen, A.M.; Yücel, M.; Pantelis Ch Allen, N.B. Sex-specific prediction of hypothalamic-pituitary-adrenal axis activity by pituitary volume during adolescence: A longitudinal study from 12 to 17 years of age. Psychoneuroendocrinolog 2013, 38, 2694–2704. [Google Scholar] [CrossRef]
- Ertekin, T.; Acer, N.; Turgut, A.T.; Aycan, K.; Ozçelik, O.; Turgut, M. Comparison of three methods for the estimation of the pituitary gland volume using magnetic resonance imaging: A stereological study. Pituitary 2011, 14, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Tsunoda, A.; Okuda, O.; Sato, K. MR Height of the Pituitary Gland as a Function of Age and Sex: Especially Physiological Hypertrophy in Adolescence and in Climacterium. AJNR Am. J. Neuroradiol. 1997, 18, 551–554. [Google Scholar] [PubMed]
- Destrieux, C.; Kakou, M.K.; Velut, S.; Lefrancq, T.; Jan, M. Microanatomy of the hypophyseal fossa boundaries. J. Neurosurg. 1998, 88, 743–752. [Google Scholar] [CrossRef]
- Peker, S.; Kurtkaya-Yapicier, O.; Kiliç, T.; Pamir, M.N. Microsurgical anatomy of the lateral walls of the pituitary fossa. Acta Neurochir. 2005, 147, 641–648. [Google Scholar] [CrossRef]
- Yasuda, A.; Campero, A.; Martins, C.; Rhoton, A.L.; Ribas, G.C. The medial wall of the cavernous sinus: Microsurgical anatomy. Neurosurgery 2004, 55, 179–189. [Google Scholar] [CrossRef]
- Dos Santos Silva, J.; Schreiner, C.A.; de Lima, L.; Brigido, C.E.P.L.; Wilson, C.D.; McVeigh, L.; Acchiardo, J.; Landeiro, J.A.; Acioly, M.A.; Cohen-Gadol, A. Volumetric measurement of intracranial meningiomas: A comparison between linear, planimetric, and machine learning with multiparametric voxel-based morphometry methods. J. Neurooncol. 2023, 161, 235–243. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).