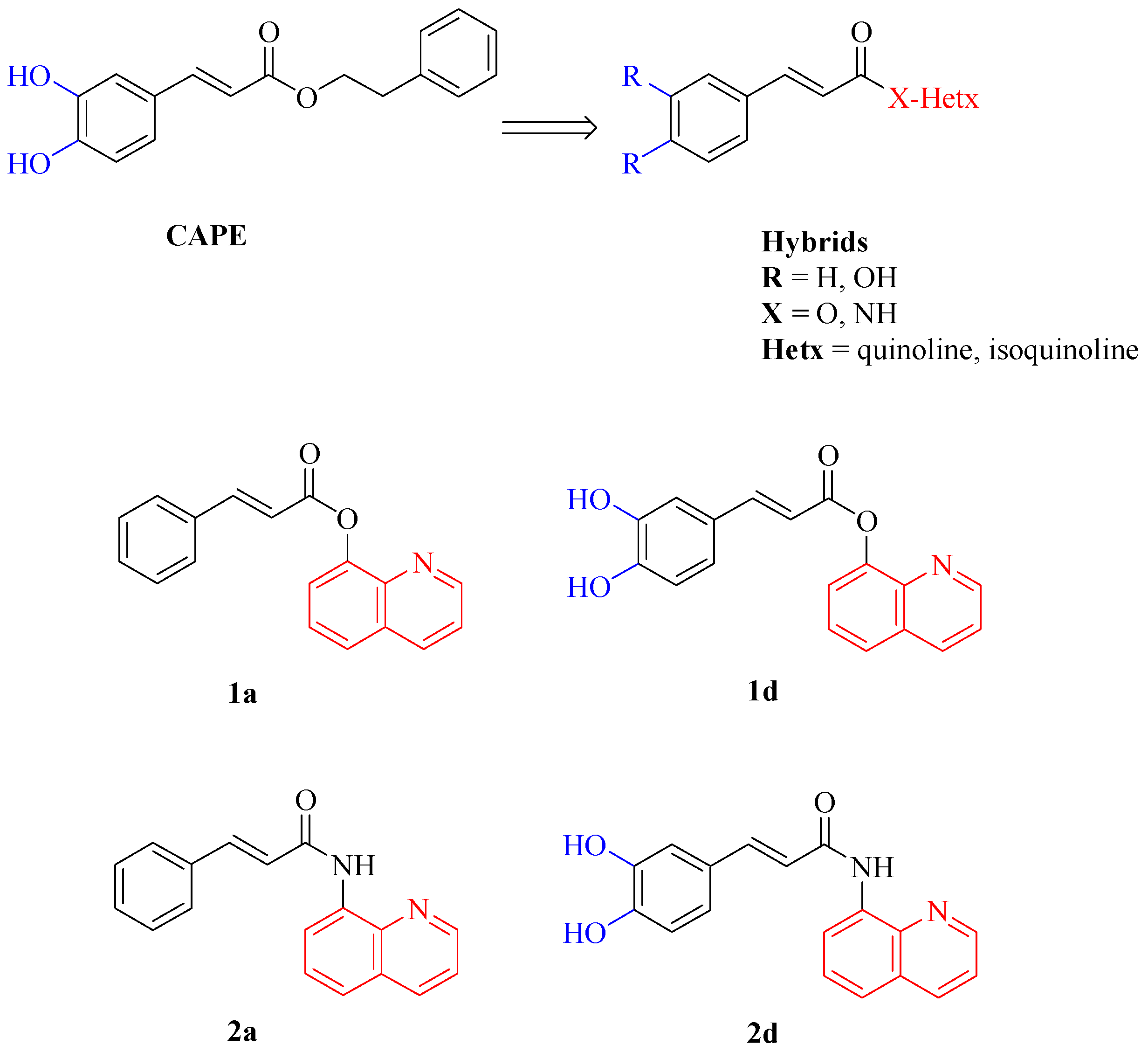
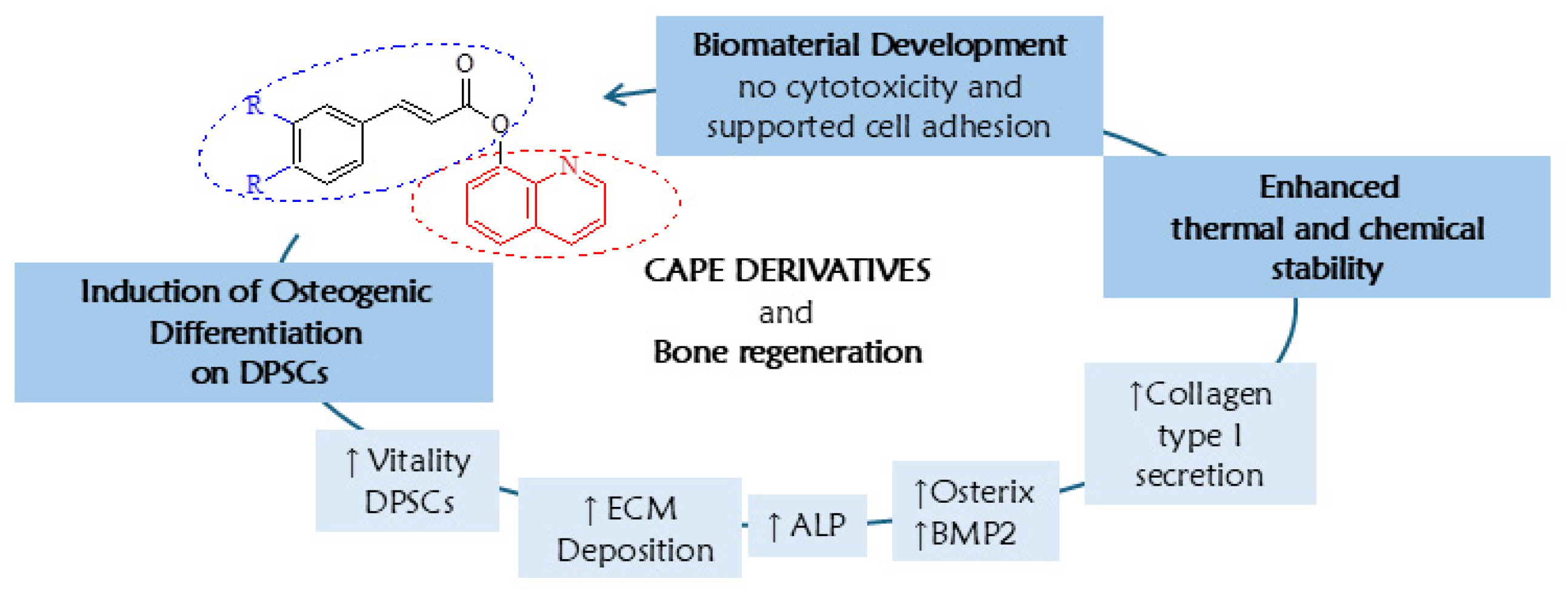
CAPE Derivatives as Potent Agents for Induction of Osteogenic Differentiation in DPSCs and Biomaterial Development
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.1.1. Culture of Dental Pulp Stem Cells
2.1.2. Human Fetal Osteoblast Cell Line
2.2. Crystal Violet Assay
2.3. Osteogenic Differentiation
2.3.1. Alizarin Red S (ARS) Staining
2.3.2. Alkaline Phosphatase (ALP) Activity
2.3.3. ELISA Analysis of Collagen Type I
2.4. Real-Time RT-PCR
2.4.1. RNA Extraction
2.4.2. Reverse Transcription (RT) and Real-Time RT-Polymerase Chain Reaction (Real-Time RT-PCR)
2.5. Manufacture of Biomaterials Enriched with CAPE Derivatives
2.6. Biomaterial Cytotoxicity Assessment
2.7. Pharmacokinetics
2.7.1. Thermal Stability
2.7.2. Chemical Stability
2.7.3. Kinetic of Chemical Hydrolysis
2.8. Statistical Analysis
3. Results and Discussions
3.1. Bone Regenerative Ability
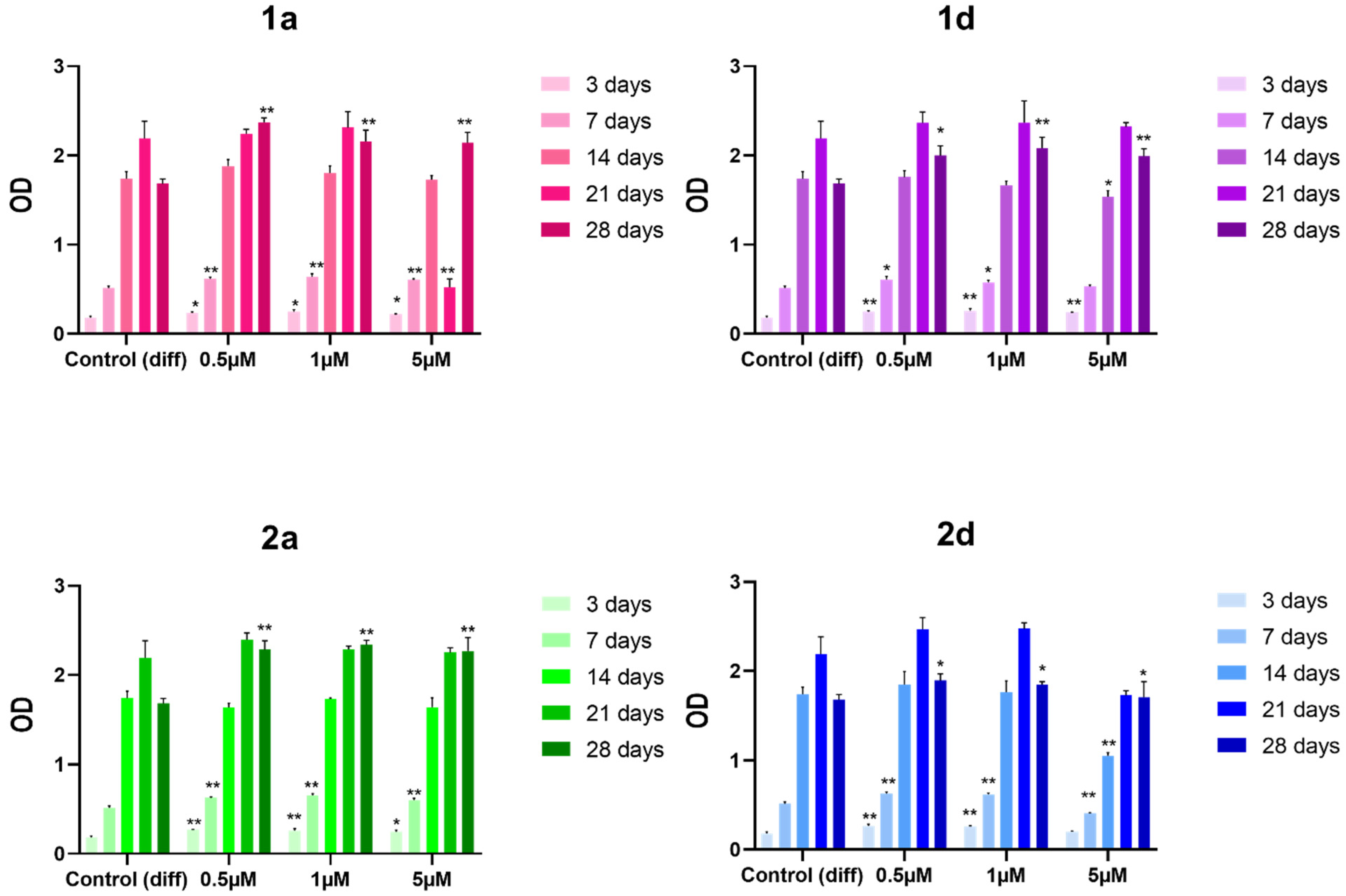
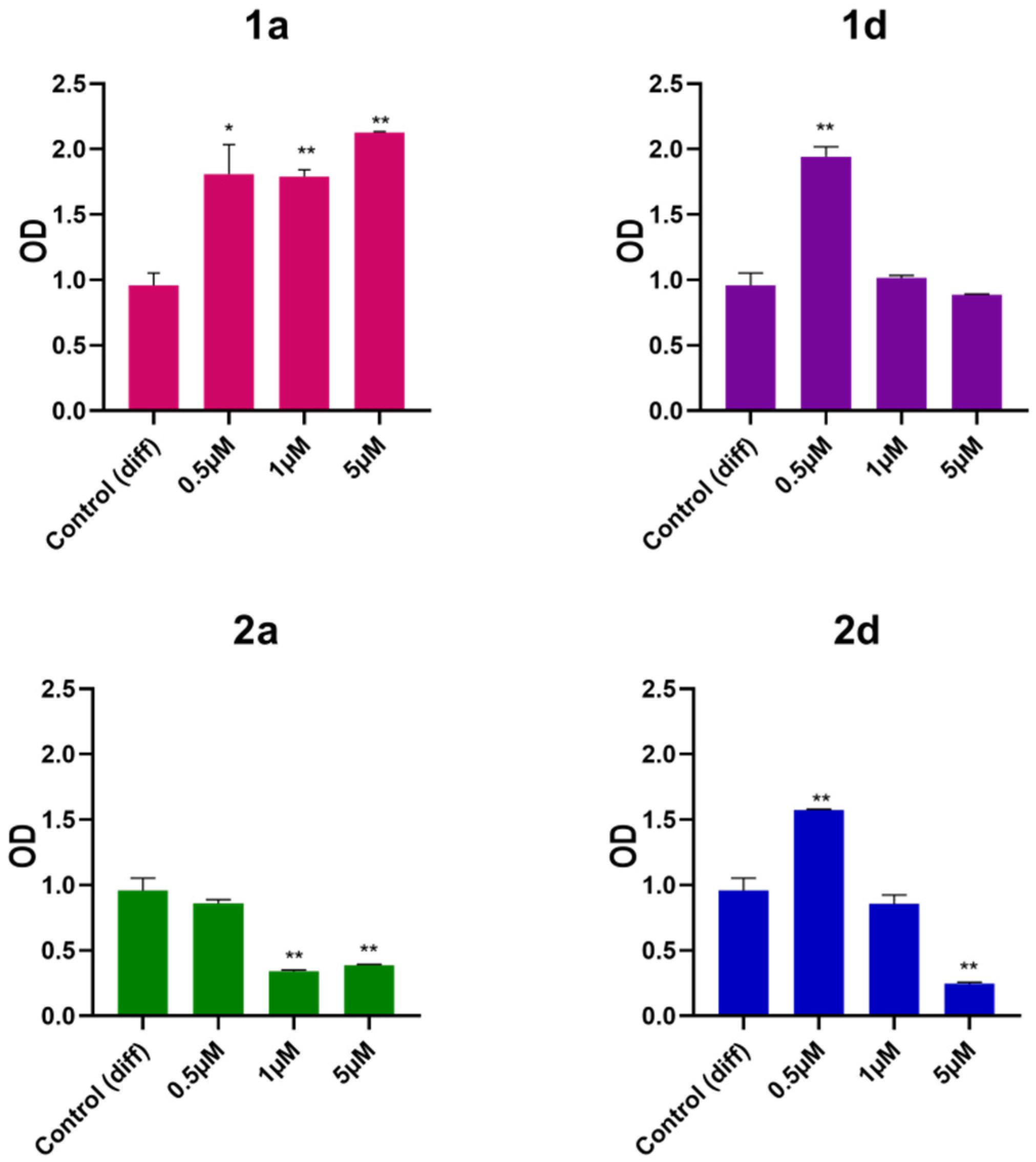
3.1.1. Cell Viability
3.1.2. Extracellular Matrix Deposition Measurement
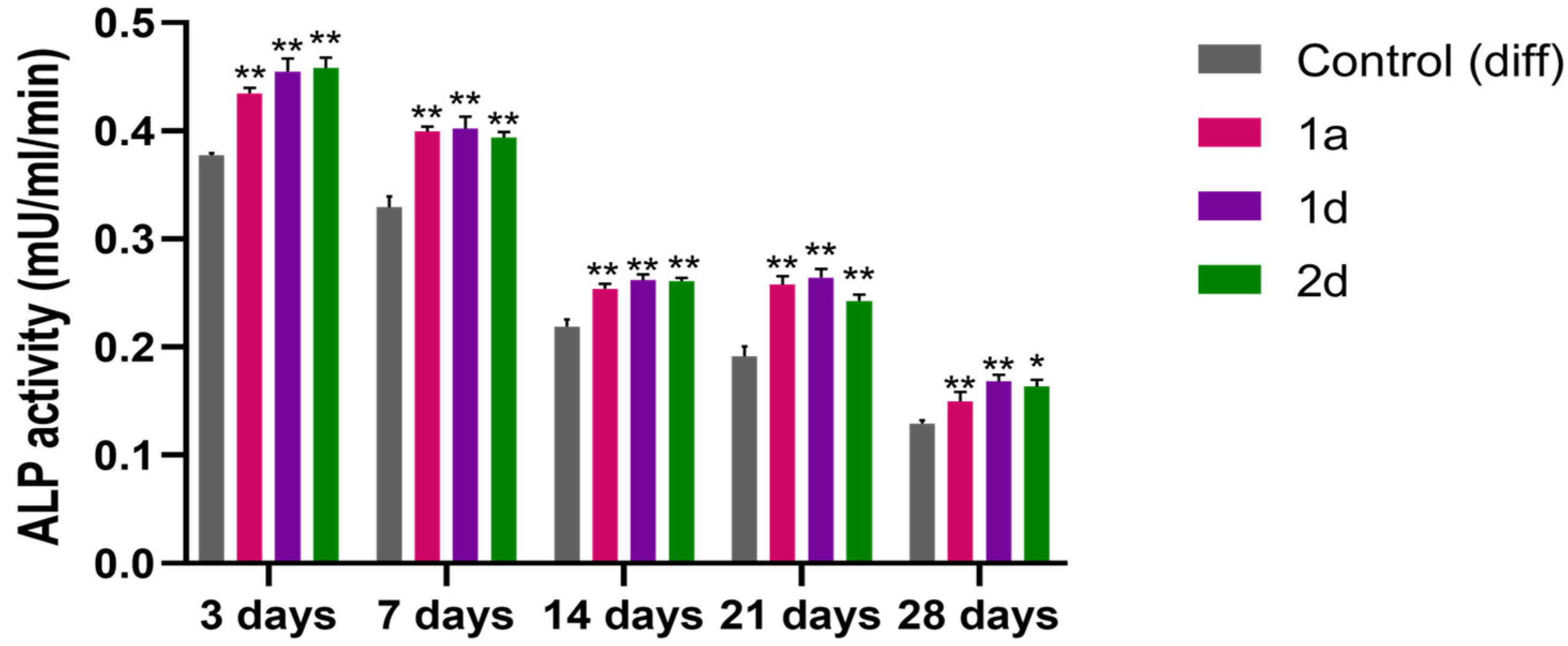
3.1.3. Alkaline Phosphatase (ALP) Activity
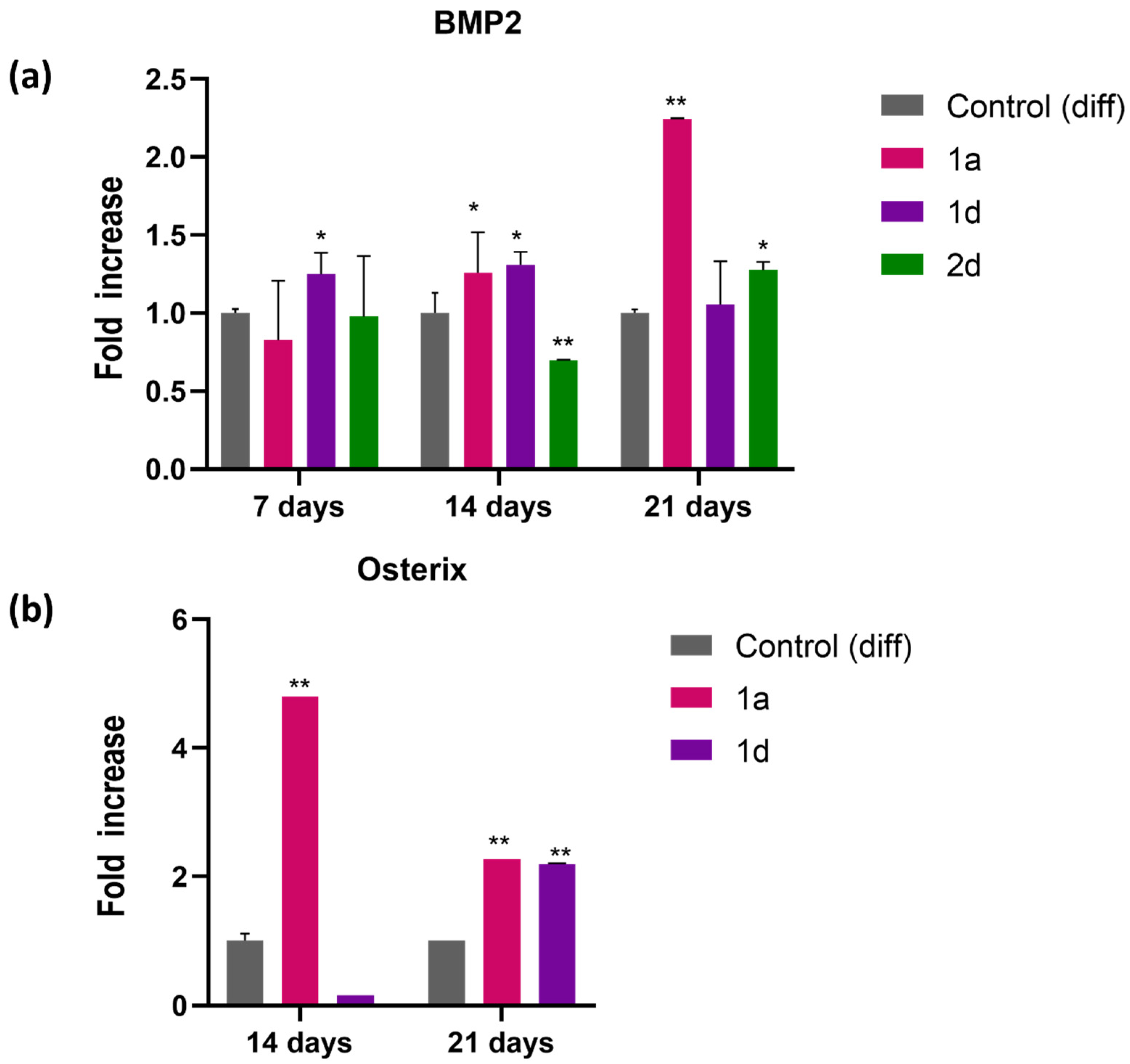
3.1.4. Gene Expression Profile of Mineralization-Related Markers
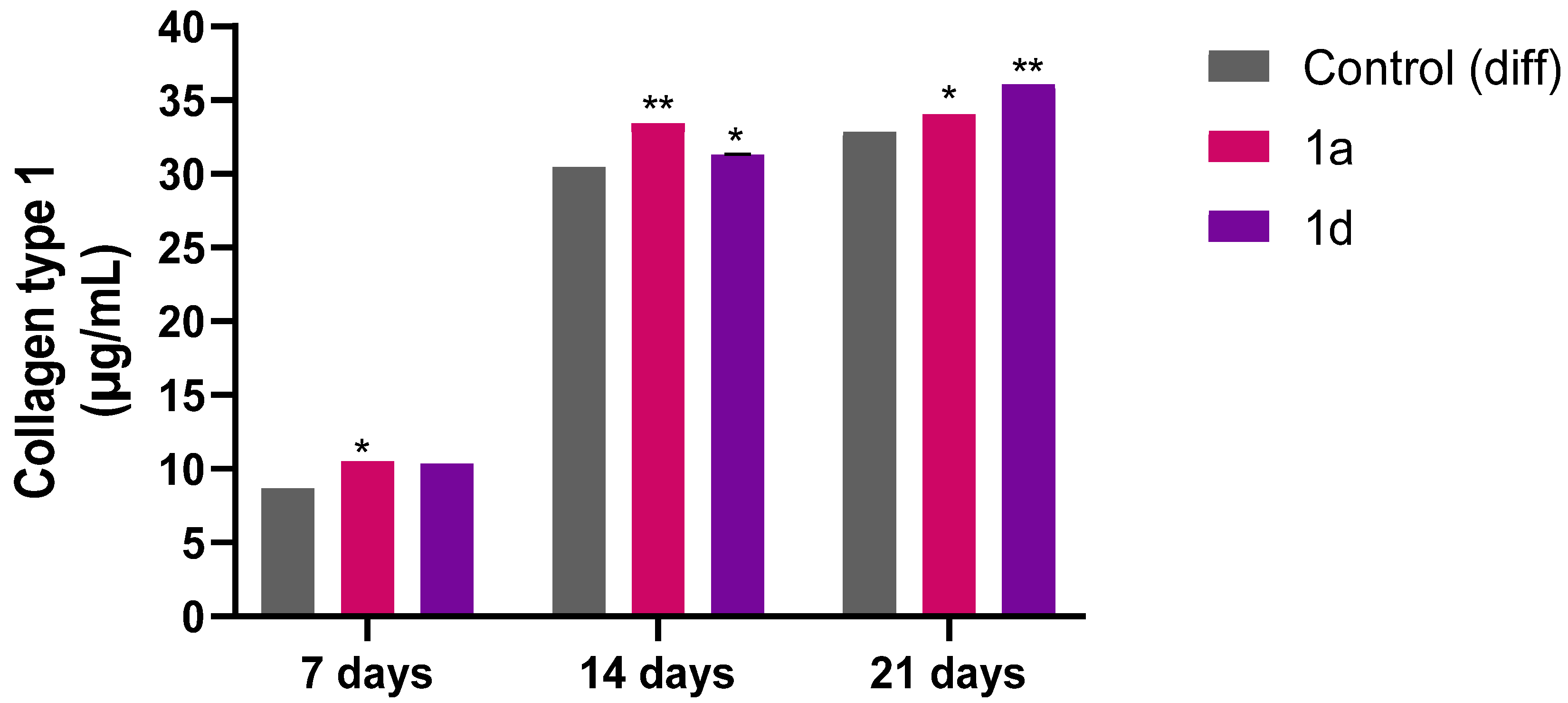
3.1.5. Collagen Type I Release in DPSC Medium
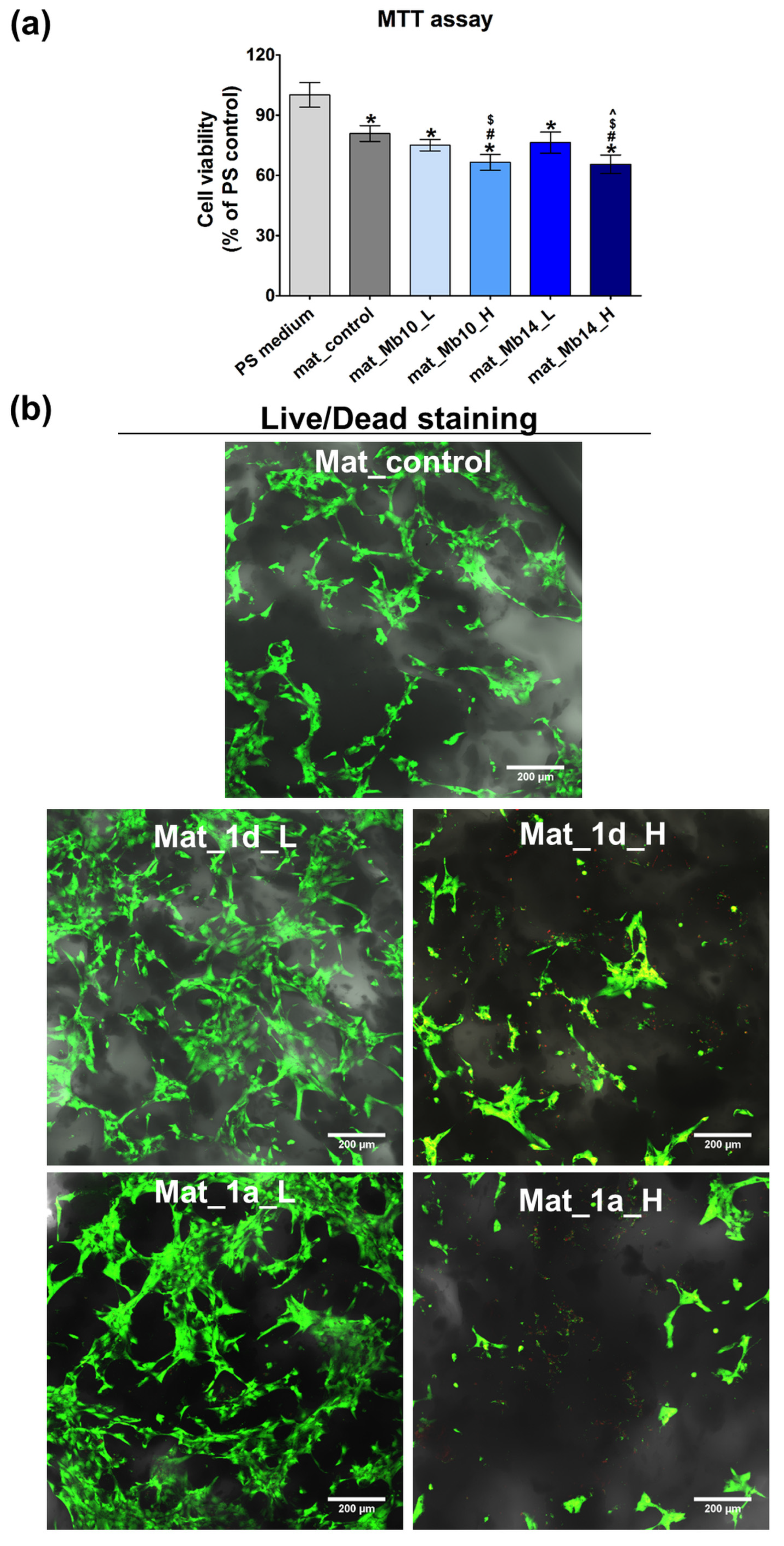
3.2. Bone Biomaterials Enriched with Compound 1a and 1d
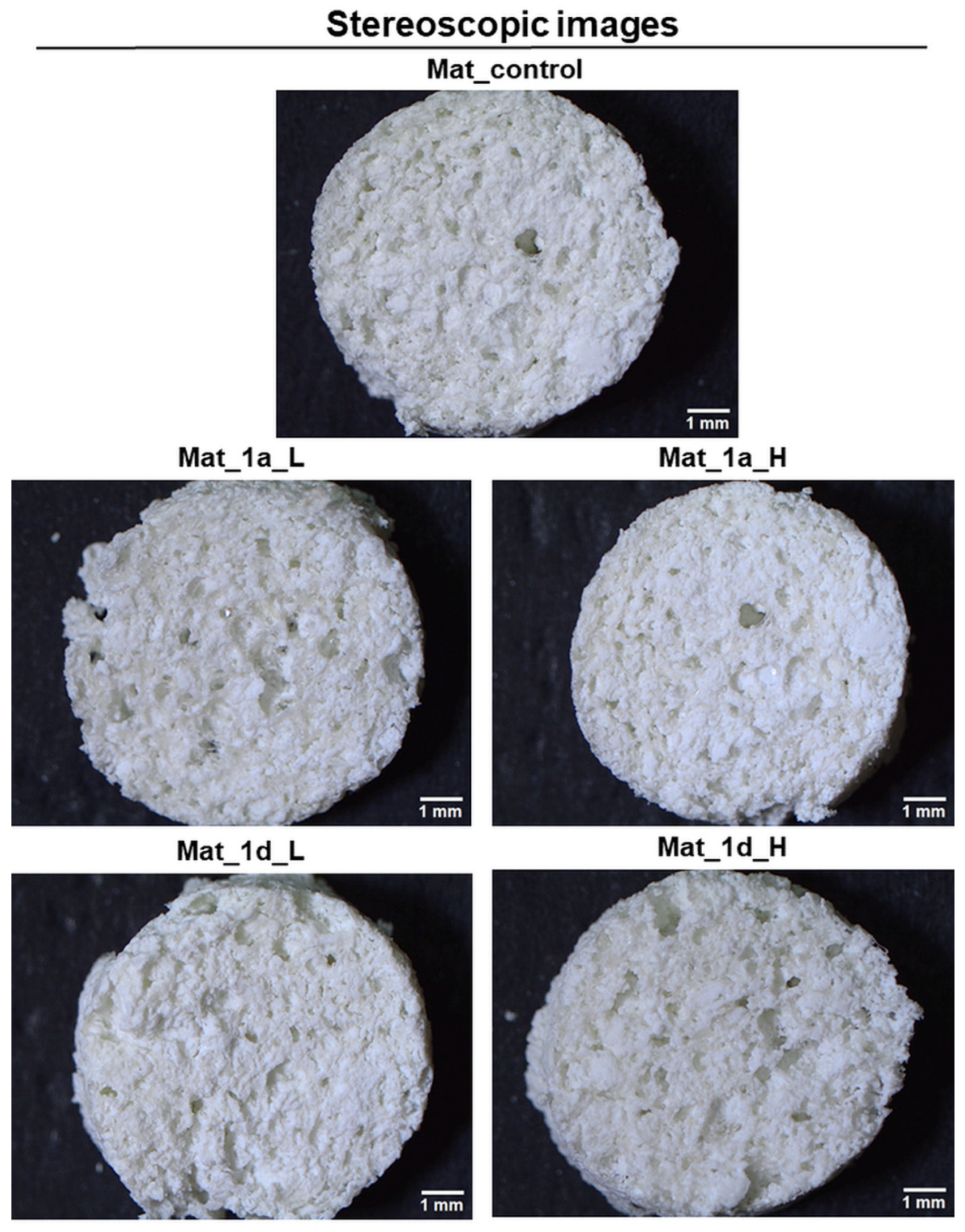
Characterization of Fabricated Bone Biomaterials
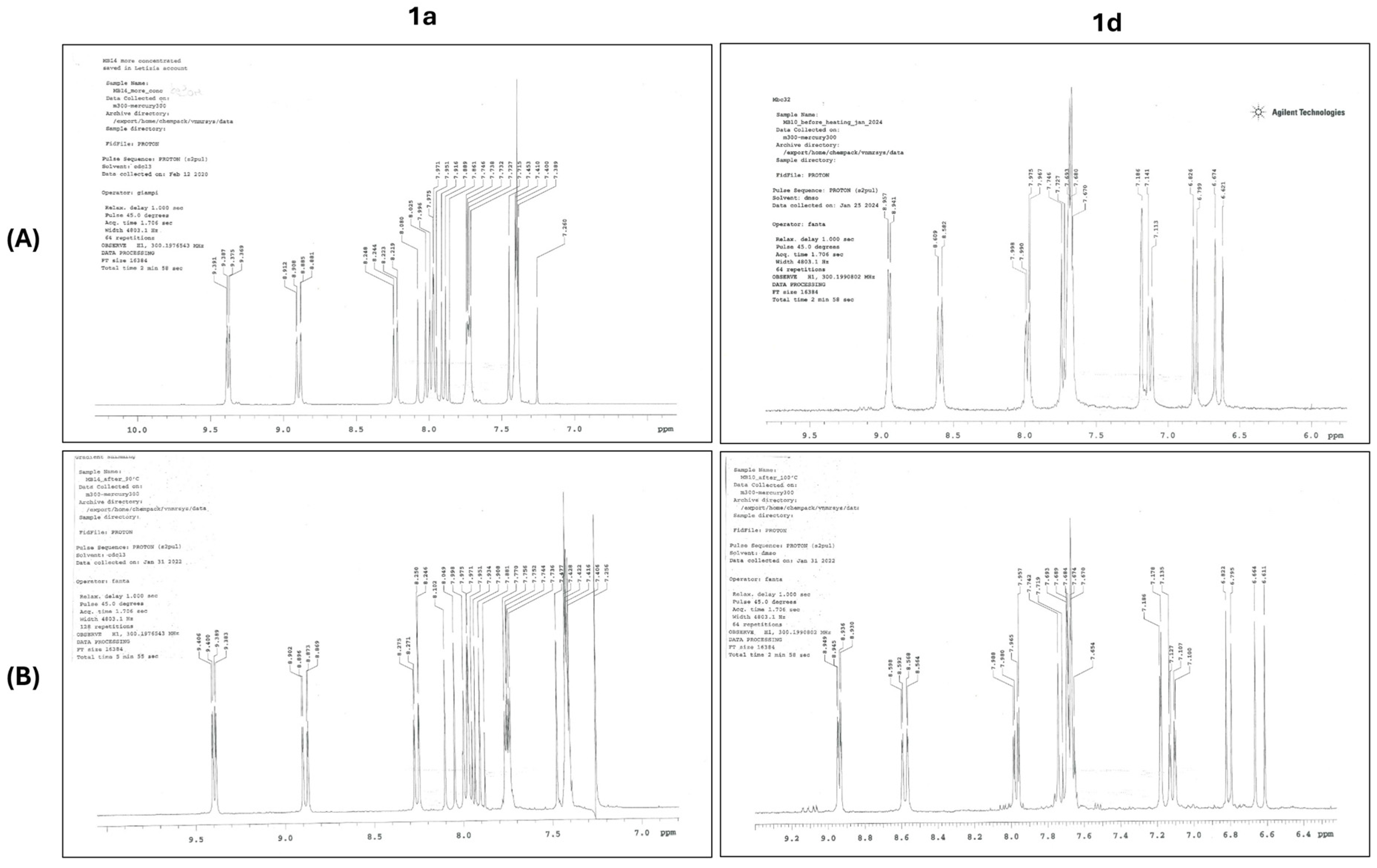
3.3. Chemical and Thermal Stability
3.3.1. Thermal Stability
3.3.2. Chemical Stability
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ALP | Alkaline Phosphatase activity |
| BMP | Bone Morphogenetic Protein |
| CA | Caffeic Acid |
| CAPE | Caffeic Acid Phenethyl Ester |
| CFU-O | Colony-Forming Unit-Osteoprogenitor |
| DPSCs | Dental Pulp Stem Cells |
| ECM | Extracellular Matrix |
| FBS | Fetal Bovine Serum |
| hFOB | Human Fetal Osteoblast Cell Line |
| OSC | Osteocalcin |
| Osx | Osterix |
| PB | Phosphate Buffer |
| PCL | Polycaprolactone |
| RM | Regenerative Medicine |
| SD | Standard Deviation |
| SAR | Structure–Activity Relationship |
References
- Chaparro, O.; Linero, I. Regenerative medicine: A new paradigm in bone regeneration. In Advanced Techniques in Bone Regeneration; InTech: Singapore, 2016. [Google Scholar]
- Codrea, C.I.; Croitoru, A.-M.; Baciu, C.C.; Melinescu, A.; Ficai, D.; Fruth, V.; Ficai, A. Advances in Osteoporotic Bone Tissue Engineering. J. Clin. Med. 2021, 10, 253. [Google Scholar]
- Oryan, A.; Alidadi, S.; Moshiri, A.; Maffulli, N. Bone regenerative medicine: Classic options, novel strategies, and future directions. J. Orthop. Surg. Res. 2014, 9, 18. [Google Scholar]
- Nandi, S.; Roy, S.; Mukherjee, P.; Kundu, B.; De, D.; Basu, D. Orthopaedic applications of bone graft & graft substitutes: A review. Indian J. Med. Res. 2010, 132, 15–30. [Google Scholar]
- Shrivats, A.R.; Alvarez, P.; Schutte, L.; Hollinger, J.O. Bone regeneration. In Principles of Tissue Engineering; Elsevier: Amsterdam, The Netherlands, 2014; pp. 1201–1221. [Google Scholar]
- Elsalanty, M.E.; Genecov, D.G. Bone grafts in craniofacial surgery. Craniomaxillofac. Trauma Reconstr. 2009, 2, 125–134. [Google Scholar] [PubMed]
- Brydone, A.; Meek, D.; Maclaine, S. Bone grafting, orthopaedic biomaterials, and the clinical need for bone engineering. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2010, 224, 1329–1343. [Google Scholar]
- Dimitriou, R.; Jones, E.; McGonagle, D.; Giannoudis, P.V. Bone regeneration: Current concepts and future directions. BMC Med. 2011, 9, 66–76. [Google Scholar]
- Kim, B.-S.; Baez, C.E.; Atala, A. Biomaterials for tissue engineering. World J. Urol. 2000, 18, 2–9. [Google Scholar] [PubMed]
- Tabata, Y. Current status of regenerative medical therapy based on drug delivery technology. Reprod. Biomed. Online 2008, 16, 70–80. [Google Scholar] [PubMed]
- Taylor, D.A.; Sampaio, L.C.; Ferdous, Z.; Gobin, A.S.; Taite, L.J. Decellularized matrices in regenerative medicine. Acta Biomater. 2018, 74, 74–89. [Google Scholar]
- Pina, S.; Ribeiro, V.P.; Marques, C.F.; Maia, F.R.; Silva, T.H.; Reis, R.L.; Oliveira, J.M. Scaffolding strategies for tissue engineering and regenerative medicine applications. Materials 2019, 12, 1824. [Google Scholar]
- Sadtler, K.; Singh, A.; Wolf, M.T.; Wang, X.; Pardoll, D.M.; Elisseeff, J.H. Design, clinical translation and immunological response of biomaterials in regenerative medicine. Nat. Rev. Mater. 2016, 1, 16040. [Google Scholar]
- Jaklenec, A.; Stamp, A.; Deweerd, E.; Sherwin, A.; Langer, R. Progress in the tissue engineering and stem cell industry “are we there yet?”. Tissue Eng. Part B Rev. 2012, 18, 155–166. [Google Scholar]
- Mao, A.S.; Mooney, D.J. Regenerative medicine: Current therapies and future directions. Proc. Natl. Acad. Sci. USA 2015, 112, 14452–14459. [Google Scholar]
- Dzobo, K.; Thomford, N.E.; Senthebane, D.A.; Shipanga, H.; Rowe, A.; Dandara, C.; Pillay, M.; Motaung, K. Advances in Regenerative Medicine and Tissue Engineering: Innovation and Transformation of Medicine. Stem Cells Int. 2018, 2018, 2495848. [Google Scholar]
- Lu, B.; Atala, A. Small molecules and small molecule drugs in regenerative medicine. Drug Discov. Today 2014, 19, 801–808. [Google Scholar] [PubMed]
- Goonoo, N.; Bhaw-Luximon, A. Mimicking growth factors: Role of small molecule scaffold additives in promoting tissue regeneration and repair. RSC Adv. 2019, 9, 18124–18146. [Google Scholar] [PubMed]
- Sedgley, C.M.; Botero, T.M. Dental stem cells and their sources. Dent. Clin. N. Am. 2012, 56, 549–561. [Google Scholar] [PubMed]
- Volponi, A.A.; Pang, Y.; Sharpe, P.T. Stem cell-based biological tooth repair and regeneration. Trends Cell Biol. 2010, 20, 715–722. [Google Scholar]
- Chen, F.-M.; Sun, H.-H.; Lu, H.; Yu, Q. Stem cell-delivery therapeutics for periodontal tissue regeneration. Biomaterials 2012, 33, 6320–6344. [Google Scholar]
- Catón, J.; Bostanci, N.; Remboutsika, E.; De Bari, C.; Mitsiadis, T.A. Future dentistry: Cell therapy meets tooth and periodontal repair and regeneration. J. Cell. Mol. Med. 2011, 15, 1054–1065. [Google Scholar]
- d’Aquino, R.; De Rosa, A.; Lanza, V.; Tirino, V.; Laino, L.; Graziano, A.; Desiderio, V.; Laino, G.; Papaccio, G. Human mandible bone defect repair by the grafting of dental pulp stem/progenitor cells and collagen sponge biocomplexes. Eur. Cells Mater. 2009, 18, 75–83. [Google Scholar]
- Patil, R.; Kumar, B.M.; Lee, W.-J.; Jeon, R.-H.; Jang, S.-J.; Lee, Y.-M.; Park, B.-W.; Byun, J.-H.; Ahn, C.-S.; Kim, J.-W. Multilineage potential and proteomic profiling of human dental stem cells derived from a single donor. Exp. Cell Res. 2014, 320, 92–107. [Google Scholar]
- Kadar, K.; Kiraly, M.; Porcsalmy, B.; Molnar, B.; Racz, G.Z.; Blazsek, J.; Kallo, K.; Szabo, E.L.; Gera, I.; Gerber, G.; et al. Differentiation potential of stem cells from human dental origin-promise for tissue engineering. J. Physiol. Pharmacol. Off. J. Pol. Physiol. Soc. 2009, 60, 167–175. [Google Scholar]
- Sugiyama, M.; Iohara, K.; Wakita, H.; Hattori, H.; Ueda, M.; Matsushita, K.; Nakashima, M. Dental pulp-derived CD31−/CD146− side population stem/progenitor cells enhance recovery of focal cerebral ischemia in rats. Tissue Eng. Part A 2011, 17, 1303–1311. [Google Scholar] [PubMed]
- Ishkitiev, N.; Yaegaki, K.; Imai, T.; Tanaka, T.; Nakahara, T.; Ishikawa, H.; Mitev, V.; Haapasalo, M. High-purity hepatic lineage differentiated from dental pulp stem cells in serum-free medium. J. Endod. 2012, 38, 475–480. [Google Scholar]
- Ellis, K.M.; O’Carroll, D.C.; Lewis, M.D.; Rychkov, G.Y.; Koblar, S.A. Neurogenic potential of dental pulp stem cells isolated from murine incisors. Stem Cell Res. Ther. 2014, 5, 30. [Google Scholar]
- Spath, L.; Rotilio, V.; Alessandrini, M.; Gambara, G.; De Angelis, L.; Mancini, M.; Mitsiadis, T.; Vivarelli, E.; Naro, F.; Filippini, A. Explant-derived human dental pulp stem cells enhance differentiation and proliferation potentials. J. Cell. Mol. Med. 2010, 14, 1635–1644. [Google Scholar]
- About, I. Dentin–pulp regeneration: The primordial role of the microenvironment and its modification by traumatic injuries and bioactive materials. Endod. Top. 2013, 28, 61–89. [Google Scholar]
- Park, J.H.; Lee, J.K.; Kim, H.S.; Chung, S.T.; Eom, J.H.; Kim, K.A.; Chung, S.J.; Paik, S.Y.; Oh, H.Y. Immunomodulatory effect of caffeic acid phenethyl ester in Balb/c mice. Int. Immunopharmacol. 2004, 4, 429–436. [Google Scholar]
- Erdemli, H.K.; Akyol, S.; Armutcu, F.; Akyol, O. Antiviral properties of caffeic acid phenethyl ester and its potential application. J. Intercult. Ethnopharmacol. 2015, 4, 344–347. [Google Scholar] [PubMed]
- Akyol, S.; Ozturk, G.; Ginis, Z.; Armutcu, F.; Yigitoglu, M.R.; Akyol, O. In vivo and in vitro antıneoplastic actions of caffeic acid phenethyl ester (CAPE): Therapeutic perspectives. Nutr. Cancer 2013, 65, 515–526. [Google Scholar]
- Balaha, M.; De Filippis, B.; Cataldi, A.; di Giacomo, V. CAPE and Neuroprotection: A Review. Biomolecules 2021, 11, 176. [Google Scholar]
- Uçan, M.; Koparal, M.; Ağaçayak, S.; Gunay, A.; Ozgoz, M.; Atilgan, S.; Yaman, F. Influence of caffeic acid phenethyl ester on bone healing in a rat model. J. Int. Med. Res. 2013, 41, 1648–1654. [Google Scholar]
- Kazancioglu, H.O.; Aksakalli, S.; Ezirganli, S.; Birlik, M.; Esrefoglu, M.; Acar, A.H. Effect of caffeic acid phenethyl ester on bone formation in the expanded inter-premaxillary suture. Drug Des. Dev. Ther. 2015, 9, 6483–6488. [Google Scholar]
- Kazancioglu, H.O.; Bereket, M.C.; Ezirganli, S.; Aydin, M.S.; Aksakalli, S. Effects of caffeic acid phenethyl ester on wound healing in calvarial defects. Acta Odontol. Scand. 2015, 73, 21–27. [Google Scholar]
- Hanga-Farcas, A.; Miere, F.; Filip, G.A.; Clichici, S.; Fritea, L.; Vicas, L.G.; Marian, E.; Pallag, A.; Jurca, T.; Filip, S.M.; et al. Phytochemical Compounds Involved in the Bone Regeneration Process and Their Innovative Administration: A Systematic Review. Plants 2023, 12, 2055–2087. [Google Scholar]
- Bai, X.C.; Lu, D.; Bai, J.; Zheng, H.; Ke, Z.Y.; Li, X.M.; Luo, S.Q. Oxidative stress inhibits osteoblastic differentiation of bone cells by ERK and NF-kappaB. Biochem. Biophys. Res. Commun. 2004, 314, 197–207. [Google Scholar] [PubMed]
- Ang, E.S.; Pavlos, N.J.; Chai, L.Y.; Qi, M.; Cheng, T.S.; Steer, J.H.; Joyce, D.A.; Zheng, M.H.; Xu, J. Caffeic acid phenethyl ester, an active component of honeybee propolis attenuates osteoclastogenesis and bone resorption via the suppression of RANKL-induced NF-kappaB and NFAT activity. J. Cell. Physiol. 2009, 221, 642–649. [Google Scholar] [PubMed]
- Ha, J.; Choi, H.-S.; Lee, Y.; Lee, Z.H.; Kim, H.-H. Caffeic acid phenethyl ester inhibits osteoclastogenesis by suppressing NFκB and downregulating NFATc1 and c-Fos. Int. Immunopharmacol. 2009, 9, 774–780. [Google Scholar] [PubMed]
- Celli, N.; Dragani, L.K.; Murzilli, S.; Pagliani, T.; Poggi, A. In vitro and in vivo stability of caffeic acid phenethyl ester, a bioactive compound of propolis. J. Agric. Food Chem. 2007, 55, 3398–3407. [Google Scholar]
- Wang, X.; Bowman, P.D.; Kerwin, S.M.; Stavchansky, S. Stability of caffeic acid phenethyl ester and its fluorinated derivative in rat plasma. Biomed. Chromatogr. 2007, 21, 343–350. [Google Scholar]
- Balaha, M.; Cataldi, A.; Ammazzalorso, A.; Cacciatore, I.; De Filippis, B.; Di Stefano, A.; Maccallini, C.; Rapino, M.; Korona-Glowniak, I.; Przekora, A.; et al. CAPE derivatives: Multifaceted agents for chronic wound healing. Arch. Pharm. 2024, 357, e2400165. [Google Scholar]
- ISO 10993-5; Biological Evaluation of Medical Devices. Part 5: Tests for in Vitro Cytotoxicity. International Organization for Standardization: Geneva, Switzerland, 2009.
- Gurtner, G.C.; Chapman, M.A. Regenerative Medicine: Charting a New Course in Wound Healing. Adv. Wound Care 2016, 5, 314–328. [Google Scholar]
- Davies, S.G.; Kennewell, P.D.; Russell, A.J.; Silpa, L.; Westwood, R.; Wynne, G.M. 1.13-Regenerative Medicine. In Comprehensive Medicinal Chemistry III; Chackalamannil, S., Rotella, D., Ward, S.E., Eds.; Elsevier: Oxford, UK, 2017; pp. 379–435. [Google Scholar]
- Davies, S.G.; Kennewell, P.D.; Russell, A.J.; Seden, P.T.; Westwood, R.; Wynne, G.M. Stemistry: The control of stem cells in situ using chemistry. J. Med. Chem. 2015, 58, 2863–2894. [Google Scholar]
- Ursu, A.; Schöler, H.R.; Waldmann, H. Small-molecule phenotypic screening with stem cells. Nat. Chem. Biol. 2017, 13, 560–563. [Google Scholar]
- Przekora, A.; Czechowska, J.; Pijocha, D.; Ślósarczyk, A.; Ginalska, G. Do novel cement-type biomaterials reveal ion reactivity that affects cell viability in vitro? Open Life Sci. 2014, 9, 277–289. [Google Scholar]
- Gnanasegaran, N.; Govindasamy, V.; Abu Kasim, N.H. Differentiation of stem cells derived from carious teeth into dopaminergic-like cells. Int. Endod. J. 2016, 49, 937–949. [Google Scholar]
- Mortada, I.; Mortada, R. Dental pulp stem cells and osteogenesis: An update. Cytotechnology 2018, 70, 1479–1486. [Google Scholar] [PubMed]
- Santos, P.H.N.; Silva, H.L.; Martinez, E.F.; Joly, J.C.; Demasi, A.P.D.; de Castro Raucci, L.M.S.; Teixeira, L.N. Low concentrations of caffeic acid phenethyl ester stimulate osteogenesis in vitro. Tissue Cell 2021, 73, 101618. [Google Scholar] [PubMed]
- Jun, J.H.; Lee, S.H.; Kwak, H.B.; Lee, Z.H.; Seo, S.B.; Woo, K.M.; Ryoo, H.M.; Kim, G.S.; Baek, J.H. N-acetylcysteine stimulates osteoblastic differentiation of mouse calvarial cells. J. Cell. Biochem. 2008, 103, 1246–1255. [Google Scholar] [PubMed]
- Kingsley, K. Caffeic Acid Phenethyl Ester (CAPE) Effects on Dental Pulp Stem Cell (DPSC) Proliferation and Viability. EC Dent. Sci. 2022, 21, 61–71. [Google Scholar]
- Kuramoto, H.; Nakanishi, T.; Takegawa, D.; Mieda, K.; Hosaka, K. Caffeic Acid Phenethyl Ester Induces Vascular Endothelial Growth Factor Production and Inhibits CXCL10 Production in Human Dental Pulp Cells. Curr. Issues Mol. Biol. 2022, 44, 5691–5699. [Google Scholar]
- Tien, N.; Lee, J.J.; Lee, A.K.; Lin, Y.H.; Chen, J.X.; Kuo, T.Y.; Shie, M.Y. Additive Manufacturing of Caffeic Acid-Inspired Mineral Trioxide Aggregate/Poly-ε-Caprolactone Scaffold for Regulating Vascular Induction and Osteogenic Regeneration of Dental Pulp Stem Cells. Cells 2021, 10, 2911. [Google Scholar]
- McGee-Russell, S. Histochemical methods for calcium. J. Histochem. Cytochem. 1958, 6, 22–42. [Google Scholar]
- Cataldi, A.; Amoroso, R.; di Giacomo, V.; Zara, S.; Maccallini, C.; Gallorini, M. The Inhibition of the Inducible Nitric Oxide Synthase Enhances the DPSC Mineralization under LPS-Induced Inflammation. Int. J. Mol. Sci. 2022, 23, 14560. [Google Scholar] [PubMed]
- Liu, M.; Li, F.; Huang, Y.; Zhou, T.; Chen, S.; Li, G.; Shi, J.; Dong, N.; Xu, K. Caffeic Acid Phenethyl Ester Ameliorates Calcification by Inhibiting Activation of the AKT/NF-κB/NLRP3 Inflammasome Pathway in Human Aortic Valve Interstitial Cells. Front. Pharmacol. 2020, 11, 826. [Google Scholar]
- de Matos, I.A.F.; Fernandes, N.A.R.; Cirelli, G.; de Godoi, M.A.; de Assis, L.R.; Regasini, L.O.; Rossa Junior, C.; Guimarães-Stabili, M.R. Chalcone T4 Inhibits RANKL-Induced Osteoclastogenesis and Stimulates Osteogenesis In Vitro. Int. J. Mol. Sci. 2023, 24, 7624. [Google Scholar]
- Song, C.Y.; Guo, Y.; Chen, F.Y.; Liu, W.G. Resveratrol Promotes Osteogenic Differentiation of Bone Marrow-Derived Mesenchymal Stem Cells Through miR-193a/SIRT7 Axis. Calcif. Tissue Int. 2022, 110, 117–130. [Google Scholar] [PubMed]
- Buchet, R.; Millán, J.L.; Magne, D. Multisystemic functions of alkaline phosphatases. Phosphatase Modul. 2013, 1053, 27–51. [Google Scholar]
- Zara, S.; De Colli, M.; di Giacomo, V.; Zizzari, V.L.; Di Nisio, C.; Di Tore, U.; Salini, V.; Gallorini, M.; Tetè, S.; Cataldi, A. Zoledronic acid at subtoxic dose extends osteoblastic stage span of primary human osteoblasts. Clin. Oral Investig. 2015, 19, 601–611. [Google Scholar]
- Vimalraj, S. Alkaline phosphatase: Structure, expression and its function in bone mineralization. Gene 2020, 754, 144855. [Google Scholar]
- Siller, A.F.; Whyte, M.P. Alkaline phosphatase: Discovery and naming of our favorite enzyme. J. Bone Miner. Res. 2018, 33, 362–364. [Google Scholar] [PubMed]
- Melguizo-Rodríguez, L.; Manzano-Moreno, F.J.; De Luna-Bertos, E.; Rivas, A.; Ramos-Torrecillas, J.; Ruiz, C.; García-Martínez, O. Effect of olive oil phenolic compounds on osteoblast differentiation. Eur. J. Clin. Investig. 2018, 48, e12904. [Google Scholar]
- Tolba, M.F.; Azab, S.S.; Khalifa, A.E.; Abdel-Rahman, S.Z.; Abdel-Naim, A.B. Caffeic acid phenethyl ester, a promising component of propolis with a plethora of biological activities: A review on its anti-inflammatory, neuroprotective, hepatoprotective, and cardioprotective effects. IUBMB Life 2013, 65, 699–709. [Google Scholar] [PubMed]
- Yiğit, U.; Kırzıoğlu, F.Y.; Özmen, Ö. Effects of low dose doxycycline and caffeic acid phenethyl ester on sclerostin and bone morphogenic protein-2 expressions in experimental periodontitis. Biotech. Histochem. 2022, 97, 567–575. [Google Scholar]
- Edgar, C.M.; Chakravarthy, V.; Barnes, G.; Kakar, S.; Gerstenfeld, L.C.; Einhorn, T.A. Autogenous regulation of a network of bone morphogenetic proteins (BMPs) mediates the osteogenic differentiation in murine marrow stromal cells. Bone 2007, 40, 1389–1398. [Google Scholar] [PubMed]
- Ai-Aql, Z.; Alagl, A.S.; Graves, D.T.; Gerstenfeld, L.C.; Einhorn, T.A. Molecular mechanisms controlling bone formation during fracture healing and distraction osteogenesis. J. Dent. Res. 2008, 87, 107–118. [Google Scholar]
- Yonezawa, H.; Harada, K.; Ikebe, T.; Shinohara, M.; Enomoto, S. Effect of recombinant human bone morphogenetic protein-2 (rhBMP-2) on bone consolidation on distraction osteogenesis: A preliminary study in rabbit mandibles. J. Cranio-Maxillofac. Surg. 2006, 34, 270–276. [Google Scholar]
- Baek, S.-h.; Choi, S.-W.; Park, S.-J.; Lee, S.-H.; Chun, H.-S.; Kim, S.H. Quinoline Compound KM11073 Enhances BMP-2-Dependent Osteogenic Differentiation of C2C12 Cells via Activation of p38 Signaling and Exhibits In Vivo Bone Forming Activity. PLoS ONE 2015, 10, e0120150. [Google Scholar]
- Ekeuku, S.O.; Pang, K.-L.; Chin, K.-Y. Effects of caffeic acid and its derivatives on bone: A systematic review. Drug Des. Dev. Ther. 2021, 15, 259–275. [Google Scholar]
- Hong, S.; Cha, K.H.; Park, J.h.; Jung, D.S.; Choi, J.-H.; Yoo, G.; Nho, C.W. Cinnamic acid suppresses bone loss via induction of osteoblast differentiation with alteration of gut microbiota. J. Nutr. Biochem. 2022, 101, 108900. [Google Scholar]
- Ulsamer, A.; Ortuño, M.J.; Ruiz, S.; Susperregui, A.R.; Osses, N.; Rosa, J.L.; Ventura, F. BMP-2 induces Osterix expression through up-regulation of Dlx5 and its phosphorylation by p38. J. Biol. Chem. 2008, 283, 3816–3826. [Google Scholar]
- Sinha, K.M.; Zhou, X. Genetic and molecular control of osterix in skeletal formation. J. Cell. Biochem. 2013, 114, 975–984. [Google Scholar]
- Sancilio, S.; Gallorini, M.; Di Nisio, C.; Marsich, E.; Di Pietro, R.; Schweikl, H.; Cataldi, A. Alginate/Hydroxyapatite-Based Nanocomposite Scaffolds for Bone Tissue Engineering Improve Dental Pulp Biomineralization and Differentiation. Stem Cells Int. 2018, 2018, 9643721. [Google Scholar]
- Çolak, S.; Erdil, A.; Gevrek, F. Effects of systemic Anatolian propolis administration on a rat-irradiated osteoradionecrosis model. J. Appl. Oral Sci. 2023, 31, e20230231. [Google Scholar]
- Patent Office of the Republic of Poland. Cryogel Bone Scaffold Based on Chitosan and Calcium-Phosphate Bioceramic and Its Method of Production. Polish Patent No. 235822, 2 November 2020. [Google Scholar]
- Agata Agata Kazimierczak, P.; Balaha, M.; Palka, K.; Wessely-Szponder, J.; Wojcik, M.; di Giacomo, V.; De Filippis, B.; Przekora, A. Macroporous Hydroxyapatite-Based Bone Scaffolds Loaded with CAPE Derivatives: A Strategy to Reduce Oxidative Stress and Biofilm Formation. Materials 2025, 18, 5074. [Google Scholar] [PubMed]
- Nasrullah, M.Z. Caffeic Acid Phenethyl Ester Loaded PEG–PLGA Nanoparticles Enhance Wound Healing in Diabetic Rats. Antioxidants 2022, 12, 60. [Google Scholar] [PubMed]
- Kazimierczak, P.; Benko, A.; Palka, K.; Canal, C.; Kolodynska, D.; Przekora, A. Novel synthesis method combining a foaming agent with freeze-drying to obtain hybrid highly macroporous bone scaffolds. J. Mater. Sci. Technol. 2020, 43, 52–63. [Google Scholar]
- Przekora, A. The summary of the most important cell-biomaterial interactions that need to be considered during in vitro biocompatibility testing of bone scaffolds for tissue engineering applications. Mater. Sci. Eng. C 2019, 97, 1036–1051. [Google Scholar]
- Karageorgiou, V.; Kaplan, D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 2005, 26, 5474–5491. [Google Scholar]
- Malafaya, P.B.; Reis, R.L. Bilayered chitosan-based scaffolds for osteochondral tissue engineering: Influence of hydroxyapatite on in vitro cytotoxicity and dynamic bioactivity studies in a specific double-chamber bioreactor. Acta Biomater. 2009, 5, 644–660. [Google Scholar] [PubMed]
- Yuan, Q.; Bao, B.; Li, M.; Li, L.; Zhang, X.; Tang, Y. Bioactive Conjugated Polymer-Based Biodegradable 3D Bionic Scaffolds for Facilitating Bone Defect Repair. Adv. Healthc. Mater. 2024, 13, 2302818. [Google Scholar] [PubMed]
- Yang, J.; Kerwin, S.M.; Bowman, P.D.; Stavchansky, S. Stability of caffeic acid phenethyl amide (CAPA) in rat plasma. Biomed. Chromatogr. 2012, 26, 594–598. [Google Scholar] [PubMed]
- Hill, P. Bone remodelling. Br. J. Orthod. 1998, 25, 101–107. [Google Scholar]
- Takegahara, N.; Kim, H.; Choi, Y. Unraveling the intricacies of osteoclast differentiation and maturation: Insight into novel therapeutic strategies for bone-destructive diseases. Exp. Mol. Med. 2024, 56, 264–272. [Google Scholar]
| Gene | Sequence (5′ to 3′) |
|---|---|
| 18S_FOR | CATGGCCGTTCTTAGTTGGT |
| 18S_REV | CGCTGAGCCAGTCAGTGTAG |
| BMP2_FOR | CACTTGGCTGGGGACTTCTT |
| BMP2_REV | CGCGCAGTCTCTCTTTTCAC |
| SP7_FOR | CTCAGGCCACCCGTTG |
| SP7_REV | CATAGTGAACTTCCTCCTCAAGC |
| Time (min) | A (%) | B (%) |
|---|---|---|
| 0 | 90 | 10 |
| 6 | 10 | 90 |
| 10 | 10 | 90 |
| 12 | 90 | 10 |
| 15 | 90 | 10 |
| CAPE | 1a | 1d | ||||
|---|---|---|---|---|---|---|
| t1/2 (h) a | Kobs (h−1) a | t1/2 (h) a | Kobs (h−1) a | t1/2 (h) a | Kobs (h−1) a | |
| pH 4.5 | 117.5 (±2.10) | 0.006 (±0.0009) | 80.6 (±2.3) | 0.009 (±0.0008) | stable | - |
| pH 7.4 | 38.5 (±0.41) | 0.018 (±0.004) | stable | - | 21.19 (±0.37) | 0.033 (±0.002) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balaha, M.; De Filippis, B.; Rapino, M.; Kazimierczak, P.; Przekora, A.; Esmail, T.; Toto, E.C.; Petrucci, G.; Canal, C.; Cataldi, A.; et al. CAPE Derivatives as Potent Agents for Induction of Osteogenic Differentiation in DPSCs and Biomaterial Development. Biomedicines 2025, 13, 3039. https://doi.org/10.3390/biomedicines13123039
Balaha M, De Filippis B, Rapino M, Kazimierczak P, Przekora A, Esmail T, Toto EC, Petrucci G, Canal C, Cataldi A, et al. CAPE Derivatives as Potent Agents for Induction of Osteogenic Differentiation in DPSCs and Biomaterial Development. Biomedicines. 2025; 13(12):3039. https://doi.org/10.3390/biomedicines13123039
Chicago/Turabian StyleBalaha, Marwa, Barbara De Filippis, Monica Rapino, Paulina Kazimierczak, Agata Przekora, Tamer Esmail, Eleonora Chiara Toto, Giulia Petrucci, Cristina Canal, Amelia Cataldi, and et al. 2025. "CAPE Derivatives as Potent Agents for Induction of Osteogenic Differentiation in DPSCs and Biomaterial Development" Biomedicines 13, no. 12: 3039. https://doi.org/10.3390/biomedicines13123039
APA StyleBalaha, M., De Filippis, B., Rapino, M., Kazimierczak, P., Przekora, A., Esmail, T., Toto, E. C., Petrucci, G., Canal, C., Cataldi, A., & di Giacomo, V. (2025). CAPE Derivatives as Potent Agents for Induction of Osteogenic Differentiation in DPSCs and Biomaterial Development. Biomedicines, 13(12), 3039. https://doi.org/10.3390/biomedicines13123039












