1. Introduction
Refractive errors represent an emerging ophthalmological domain, with a growing understanding of their importance and impact on vision. Firstly, myopia is the refractive error with the most rapidly increasing prevalence. The World Health Organisation warns that 52% of the world’s population will be myopic by 2050 [
1,
2]. In the European region, the current prevalence, in the 2020–2030 decade, is estimated to vary from 32.2% in Eastern Europe to 36.7% in Western Europe, with a value of 34.6% in Central Europe, to which Romania, in which the current study was performed, belongs [
2]. Moreover, the prevalence varies greatly between European countries: a recent meta-analysis reveals the lower prevalence of 11.9% in Finland and 49.7% in Sweden. In terms of age groups, the highest prevalence is in adolescents (25.2%), followed by adults (24.3%), and lowest in children between 6 and 11 years old, at 5.5% [
3]. Data in Asian countries point to an even bigger problem—myopia is diagnosed in 91% of first year students in Taiwan universities [
4], and in 96% of army recruits in South Korea [
5], with over 20% of these cases being high myopia [
4,
5].
High myopia is a known risk factor for several ophthalmic pathologies, such as myopic macular degeneration and retinal detachment. Even a small refractive error increases the risk: an eye with a refractive error of −3.00 diopters (D) has a three times higher risk of retinal detachment compared with a −1.00 D refractive error [
6]. Myopic macular degeneration is the main cause of blindness among myopic patients [
7,
8]. Another chronic disease associated with myopia is primary open angle glaucoma (POAG), the risk of developing POAG being 2.26 times higher compared to the general population [
9].
Another significant refractive error, followed in the present study, is hyperopia, which is associated with a high risk of lowered quality of life [
10]. Prevalence worldwide is 4.6% in children and 30.9% in adults, with a high degree of variation between geographical regions [
11]. Uncorrected hyperopia, particularly anisometropia (difference of more than one diopter of spherical equivalent between eyes [
12]) raises the risk of amblyopia in children (defined as a decreased visual acuity, in the absence of organic ocular disease, caused by sensory deprivation throughout the development of the eye, most commonly caused by uncorrected strabismus and refractive errors [
13]). This hyperopia–amblyopia association was identified in a pediatric population in Romania as well [
12]. Uncorrected amblyopia brings also an altered perception of personal wellbeing, particularly in young people, but also an altered perception of general and mental health [
14]. In terms of visual adverse effects, hyperopia raises the risk for adult patients to develop primary angle closure glaucoma (PACG)—a spherical equivalent of 1–3 diopters involves a 58% higher risk of PACG, with values over 3 diopters involving a 3.33 times higher risk, and even more in young patients under 65 years old [
15].
In the process of myopic progression, the axial length axis increases, and a flattening of the cornea has been described in the literature as a compensatory phenomenon in some cases [
16], a change described since 1988 by Grosvenor [
17]. As an imbalance between axial elongation and corneal compensation occurs, the actual refractive error, myopia, is developed, which has also been described as a mismatch between the refractive power of the ocular dioptric apparatus (cornea, lens) and the elongated axial length [
16,
18]. In the recent literature, the ratio between axial length (in millimeters) and corneal curvature radius (in millimeters) (AL/CR) is intensely studied [
19]. A high AL/CR ratio was also associated with another important myopia risk factor: the parental myopia [
19]. The interaction between axial elongation and corneal flattening may also give us clues about future complications of myopia—in a study that included over 1000 children with low myopia (SE between −3.00 D and −0.50 D), there was observed an association between a flatter cornea, a larger axial length, and a higher frequency and severity of the initial form of myopic maculopathy, with fundus tessellation [
20].
Not only do biometric ocular data offer us insight into the risk of the above-mentioned complications, but also biomechanical properties of the cornea, which have previously been proven valuable in pathology, such as glaucoma or keratoconus [
21,
22], and also in the subject of our research, hyperopia and myopia [
23,
24]. As such, our hypothesis is that, in the present Romanian population of young myopes and hyperopes, the AL/CR ratio will correlate both with ocular biometrics and corneal biomechanics. The objective of the present study is to study the morphological ocular data in relation to the biomechanical properties of the cornea, namely the corneal hysteresis and resistance factor, in both myopic and hyperopic eyes.
2. Methods
This study was performed using a non-randomized cross-sectional methodology. The study group was constituted by evaluating inclusion and exclusion criteria regarding all patients who presented to a private ophthalmology clinic in Bucharest, Romania, in the period February–June 2023. The study was conducted in accordance with the Declaration of Helsinki and approved by the Carol Davila University of Medicine and Pharmacy Research Ethics Committee (protocol code PO-35-F-03/16.01.2023). All patients (and their legal guardians for patients under the age of 18) offered informed consent.
The inclusion criterion was the spherical equivalent (SE) (spherical refractive error + 1/2 cylindrical refractive error), measured after pharmacological cycloplegia (cyclopentolate or tropicamide, instilled 3 times at 5 min intervals in each eye). The myopic group had SE lower than −0.50 D [
25], hyperopic group had SE over 0.50 D [
26], and emmetropia represented an SE in the ±0.50 D range [
27], also acting as a control group.
Patients were excluded if they presented any other ocular pathology, other than the refractive errors mentioned above (hyperopia and myopia). They were excluded if they presented presbyopia, corneal disease such as keratoconus, amblyopia, strabismus, glaucoma or ocular hypertension, cataract, retinal disease, or a history of refractive surgery. Also, systemic diseases such as diabetes mellitus, autoimmune disorders, arterial hypertension, and dyslipidemia constituted contraindications, together with pregnancy and breastfeeding.
A complete ophthalmological examination was performed for all patients, including visual acuity testing using the Snellen chart, a complete slit-lamp exam, intraocular pressure measurement using Goldmann tonometer, and autorefractometry after pharmacological cycloplegia, using the Topcon KR800 device (Topcon, Tokyo, Japan) to measure the spherical equivalent by directing infrared light into the eye and measuring the reflection of the light from the retina [
28].
The patients also underwent a series of measurements: corneal biomechanical properties were measured using the Ocular Response Analyzer (ORA) (Reichert Ophthalmic Instruments Inc., Depew, NY, USA), which results in corneal hysteresis (CH), corneal resistance factor (CRF), and the Goldmann-correlated intraocular pressure IOP (IOPg). ORA is a non-contact tonometer, using infrared light to detect the deformation of the cornea, which is caused by an air puff emitted by the device. The cornea becomes applanated and then concave, before resuming the initial shape. The device records the pressures corresponding to the two applanation moments and calculates the intraocular pressure of two parameters of the corneal response to the mechanical deformation: CH, representing the corneal capacity to absorb and dissipate energy (the difference between the two applanations), and CRF, reflecting the corneal resistance and elasticity (similar to CH, the second applanation multiplied with a constant) [
29].
Ocular biometry was performed using the Aladdin biometer (Topcon, Tokyo, Japan), which utilizes low-coherence light [
30] and was used to measure the axial length (AL), average corneal curvature radius (CR), anterior chamber depth (ACD), and central corneal thickness (CCT). The AL/CR ratio was calculated as follows:
Statistical Analysis
The right eye of every patient was randomly chosen to be included in the analysis. Only quality measurements were included (for instance, Waveform score over 7 for the ORA reading). Statistical analysis of the data was performed using the statistical package IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, NY, USA).
This study includes both categorical and numerical, continuous data. The absolute and relative frequencies were calculated for categorical data. For numerical data, the average and standard deviation (SD) were determined. The age was classified into several age groups: 6–10 years old, 11–14 years old, 15–18 years old, and over 18 years old. The normal distribution of the numeric variables was verified and confirmed using the Kolmogorov–Smirnov Test.
To find significant differences between any two groups (hyperopic and emmetropic, myopic and emmetropic, male and female, children and adults), an independent samples t-test was used, preceded by the Levene’s Test for Equality of variances (as a homogenous variance of the means in the two compared samples is an assumption of the independent samples
t-test) [
31]. In order to find significant differences between more than two groups (age brackets 6–10 years old, 11–14 years old, 15–18 years old, and over 18 years old), the one-way ANOVA analysis was performed, followed by the post hoc Bonferroni analysis.
The degree of correlation between variables was ascertained by computing Pearson’s correlation coefficient, known as “Pearson’s r”, which can vary between 1 and −1. A moderate correlation is between 0.3 and 0.5 or between −0.3 and −0.5, a strong correlation is over 0.5 or below −0.5, and a weak correlation is between 0.3 and −0.3, according to Pearson’s r. A p-value of 0.05 is regarded as the cutoff point for statistical significance.
4. Discussion
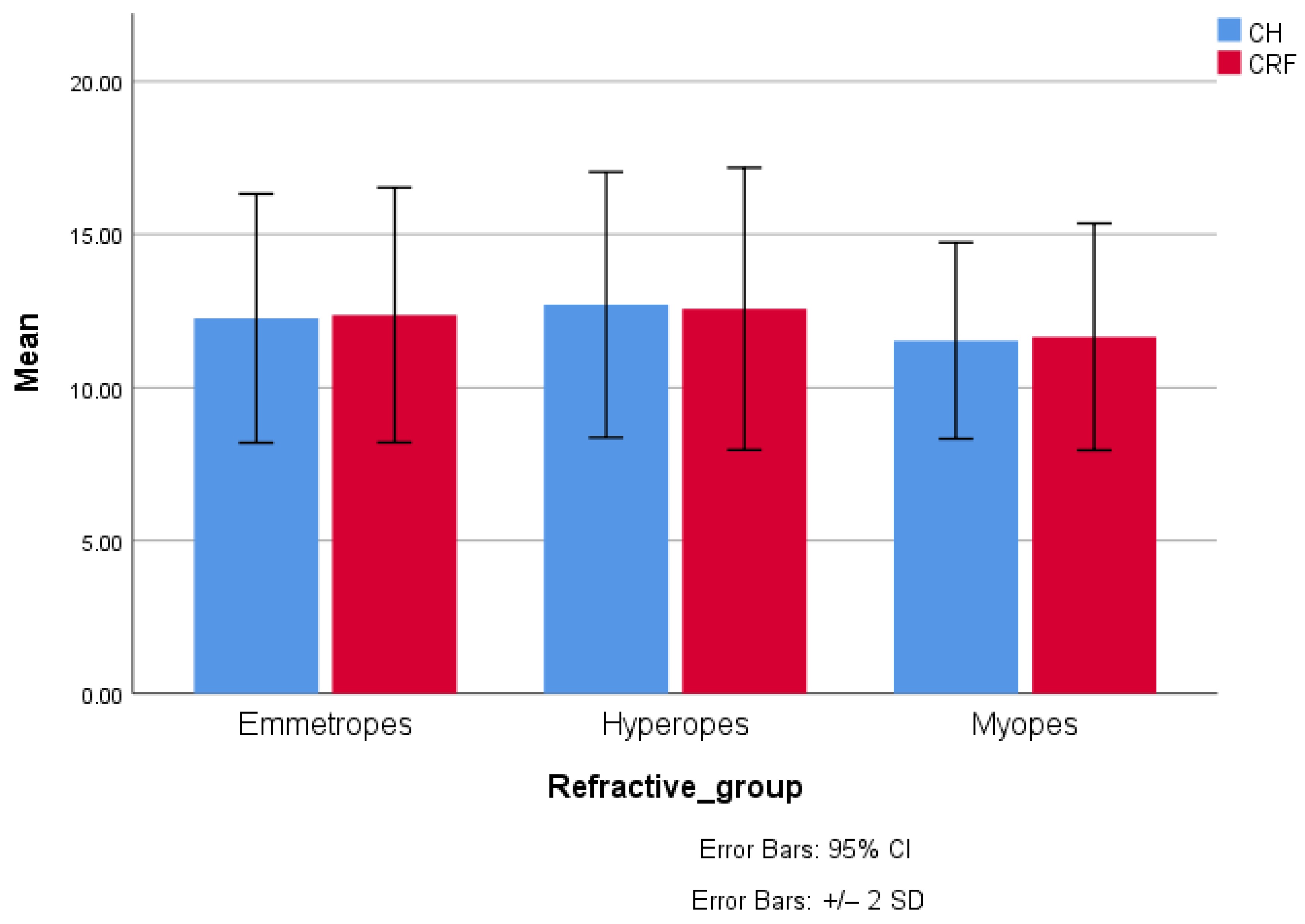
As far as we are aware, this is the first study investigating the AL/CR ratio in a Romanian population involving both adults and children and both myopic and hyperopic eyes. The strong connections found between this ratio and corneal biomechanical properties, ocular parameters, and particularly ones involved in the follow-up of refractive errors (axial length and spherical equivalent) make it a valuable biomarker for our patients. In the myopic group, corneal hysteresis (CH) and the corneal resistance factor (CRF) are significantly higher in adolescents (11–14 years) compared to adults (>18 years), suggesting a decrease in ocular biomechanical properties with age, an aspect correlated with the progression of myopia. Also, anterior chamber depth (ACD) is significantly greater in adolescents than in adults, which may reflect ocular morphological changes specific to growth and myopic progression. In emmetropes, a reduction in corneal biomechanical properties is observed in adults (>18 years) compared to younger groups. Also, axial length (AL) and AL/CR ratio increase during childhood, reaching a plateau in adolescence and adulthood. Lastly, in hypermetropes, higher CCT and ACD values are found in the pediatric and adolescent groups compared to adults. These variations suggest the involvement of anatomical factors in the maintenance of hypermetropia at young ages, with a tendency to reduce the depth of the anterior chamber with advancing age.
In our cohort, we note an average SE of −3.75 D in the young school aged myopes (6–10 years old), therefore suggesting that the process of myopization debuts at a very young age. Moreover, it is known that the rate of progression is greatest in the 6–10 age bracket [
32], therefore supporting the need for screening for early myopia development in pre-school and primary school children.
Interestingly, the AL/CR ratio was significantly lower in younger children compared to adolescents and adults amongst emmetropes (2.96, versus values over 3). As the risk of SE progression in the 6–10 age group of emmetropes is high, and may evolve towards myopia [
33], it is particularly important to follow young emmetropes who may develop subsequent myopia.
As expected, myopic eyes differed significantly in terms of ocular morphology, with lower SE and CCT and higher AL and ACD. Conversely, hyperopes had significantly higher SE and lower ACD and AL. The difference in CCT, detected only in myopes, has been previously described [
34], and may have a direct relationship with SE—a large study detected a decrease in CCT of 1 micrometer for each 1.00 D of SE [
35]. The difference in ACD reflects the connection between hyperopia and a shallow anterior chamber, with a higher risk of PACG [
15,
36]. Data from the literature suggest that the steepest decrease in ACD appears in the 20–30 age group (similar to our cohort) [
37].
In terms of corneal biomechanics, the myopic group differed significantly, but the hyperopic one did not, compared to emmetropes, therefore suggesting a particular behavior of the myopic cornea. This characteristic of the myopic eye may prove a valuable biomarker for refractive progression, as research is starting to describe low CH as correlated to a greater AL increase in myopic children using single vision spectacles [
38]. On the other hand, in children undergoing orthokeratology, the baseline CH did not associate with AL progression, suggesting a benefit in molding the cornea and, implicitly, altering the corneal biomechanics in young myopes [
38]. Furthermore, other biomechanical properties, measured with the Corvis ST device, have correlated with AL progression: a high corneal amplitude of deformation (DA) correlates with faster myopic progression [
39].
The importance of the AL/CR ratio has been previously studied: it was shown that AL/CR percentiles are a better predictor of myopia than AL percentiles, and a value over 3 can be used as a diagnostic criterion for myopia [
40]. In accordance, the values in our study were 3.2 in myopes, 3.03 in emmetropes, and 2.94 in hyperopes, with similar averages in other studies [
41].
Similarly to other studies [
19], the correlation with SE was stronger for the AL/CR ratio compared to the AL, in both refractive error groups. Interestingly, in emmetropes, SE did not correlate with either AL or CR, but it did correlate with the ratio between them, supporting this biomarker’s role in understanding the evolution of refractive errors. Interestingly, the correlation AL/CR–ACD was strongest in the hyperopic group, supporting the potential role of the ratio in the early detection of hyperopes at risk of acute angle closure and PACG. However, as the study is cross-sectional and the cohort of hyperopes is the smallest of the three compared in the present study, more research is needed in order to draw a firm conclusion.
In our cohort, children and adults were significantly different. A decrease in CH and CRF has been described in the literature with aging, and may be related to the decrease in elasticity due to protein glycation and oxidative stress which contributes to physiological crosslinking [
42], this correlation being significant even when taking into account gender, corneal thickness, intraocular pressure, and refractive error [
43]. Further, a genome-wide association study has also found that CH and CRF decrease with age, identifying a difference between sexes which was absent in our cohort [
44]. The difference in ACD may prove valuable, as advanced age is a known risk factor for angle closure glaucoma [
36,
45]. Also, adults are known to have thinner corneas, both in a Caucasian cohort [
46] and in an Asian cohort [
47]. As a theoretical consideration, beyond the scope of our study, this phenomenon of crosslinking has been investigated as a potential therapeutic option for progressive myopia [
48]; however, it is not yet established as secure and efficacious as in other ocular diseases, primarily in keratoconus [
49].
Male and female patients differed only in terms of morphological parameters, not in terms of the AL/CR ratio or the biomechanical properties: females have a lower CCT, ACD, and AL and a higher CR. However, there are conflicting results in the literature: large scale studies have either found no difference in AL and CCT [
47,
50], a difference only in CH and CRF, but not in CCT [
51], an increase in CCT in men only in the 18–29 age group [
46], or in all age groups in myopes [
52,
53]. However, gender has been described as an important factor in myopia: annual progression is faster in girls than in boys [
54], differences being evident starting from the age of nine [
55]. A steeper cornea has been previously described in females [
52,
53], including children—a study in which for the same refractive error, girls had a steeper cornea and shorter axial length [
40]. This interesting observation has not been replicated in our cohort—while female patients had a lower AL and higher CR, AL/CR did not significantly differ—showing that there is more research needed to determine the role of refractive value and ethnicity on the AL/CR gender difference.
In tandem with the lower ACD in adult patients, women also present a lower ACD. Both represent risk factors for PACG [
37,
45], suggesting a need for closer follow-up of female patients, particularly hyperopic ones, as they age.
The study of refractive errors is of paramount importance, as their impact has been documented starting from young ages: children with uncorrected refractive errors have lower reading and writing test scores [
56]. Public health measures and raising awareness have been proven to help—a study which involved the visual acuity correction of a cohort of children has led to improvements in testing scores [
57].
In terms of myopia, several behavioral risk factors have been identified: long time spent performing near work (reading, writing, and using electronic devices up close) and short time spent outdoors [
58] and alterations enhanced by the COVID-19 prevention measures [
59], with reliable data showing accelerated myopic progression during isolation [
60]. The development and progression of myopia involve several factors and are incompletely understood mechanisms [
61]. In humans, it is currently believed that the mechanism for myopic progression is peripheral retinal hyperopic defocus. An image, if formed clearly on the fovea, in the periphery is projected posterior to the retina, and therefore a hyperopic defocus is created, which acts as a trigger for axial lengthening of the eye [
62]. In animal models, the phenomenon of form deprivation myopia has also been proven important, in which the absence of normal light stimuli to the eye during its development leads to severe axial elongation and choroidal and scleral thinning. This proves that adequate light stimulation of the retina is involved in the normal pathway of eye growth [
61,
63]. In the relationship with the peripheral defocus described in humans, an important mechanism described in animal models is the induction of myopia by placing a divergent lens in front of the animal’s eye, with this hyperopic defocus leading to choroidal thinning, increased axial length, and, ultimately, a myopic refractive error [
63].
The biochemical pathways triggered by peripheral defocus involve neurotransmitters such as dopamine and GABA, growth modulators such as retinoic acid and insulin, and also nitric oxide and melanopsin at the retinal level. The choroid and retinal pigmentary epithelium face changes in the blood flow, ion transport, and growth modulation (TGFβ, FGF) [
61,
64]. The scleral remodeling contributing to the axial elongation has been characterized by an increase in matrix metalloproteinases and a decrease in tissue inhibitors of metalloproteinases, and therefore a loss of collagen and proteoglycans [
65]. This scleral thinning also involves the transformation of fibroblasts into myofibroblasts and an up-regulation of ischemic signaling cascades [
66].
On the other hand, hyperopia involves a short axial length relative to the ocular dioptric power; therefore, the image does not form on the fovea, but behind it, particularly if the object is at a near distance to the eye [
67]. During the early years of life, the eye undergoes the process of emmetropisation—the eye is hyperopic at birth and the refractive error decreases during childhood, mainly through axial lengthening, on average reaching emmetropia around the age of seven [
61]. It is believed that persistent hyperopia is due to a disturbance in the normal process and persistence of initial positive refractive errors [
68].
This study presents a series of limitations: as the study was performed in a single clinical center, it presents the risk of limited external validity, and more research in diverse populations is needed in order to generalize the findings herein. The cross-sectional design inhibits the ability to create time predictions, and the small hyperopic group reduces the statistical power for hyperopia-specific analyses. Most importantly, due to time constraints and the presentation of the patients to the clinic, the cohort is skewed, with a lower number of hyperopic eyes in the analysis.