Mitochondrial Dynamics in Aging Heart
Abstract
1. Introduction
2. Mitochondrial Morphological and Functional Alterations in the Aging Heart
3. Mitochondrial Turnover and Quality Control in Cardiac Aging
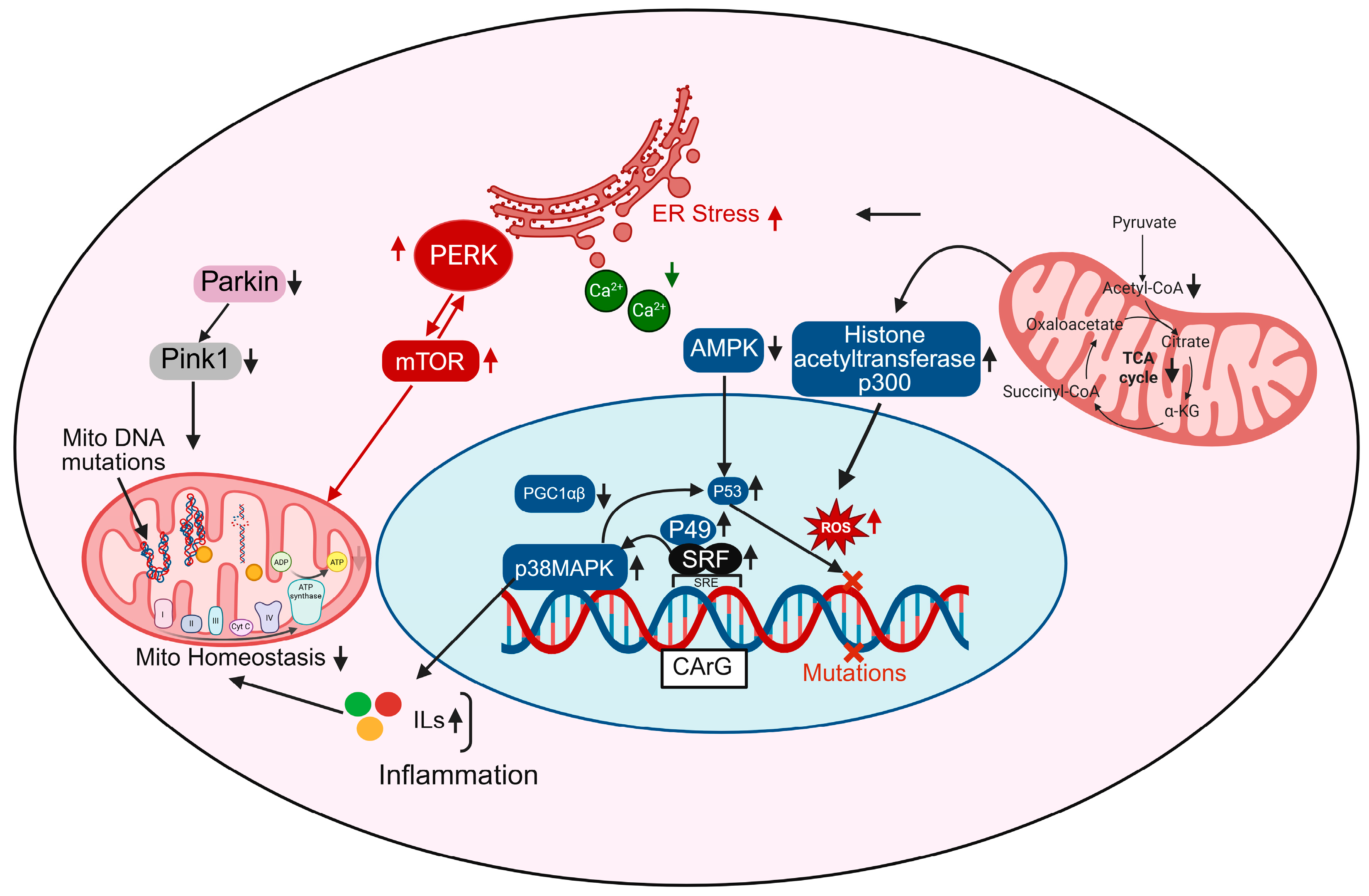
4. Mitochondrial ROS and mtDNA
5. Transcriptional Regulation of Mitochondria in Cardiac Aging
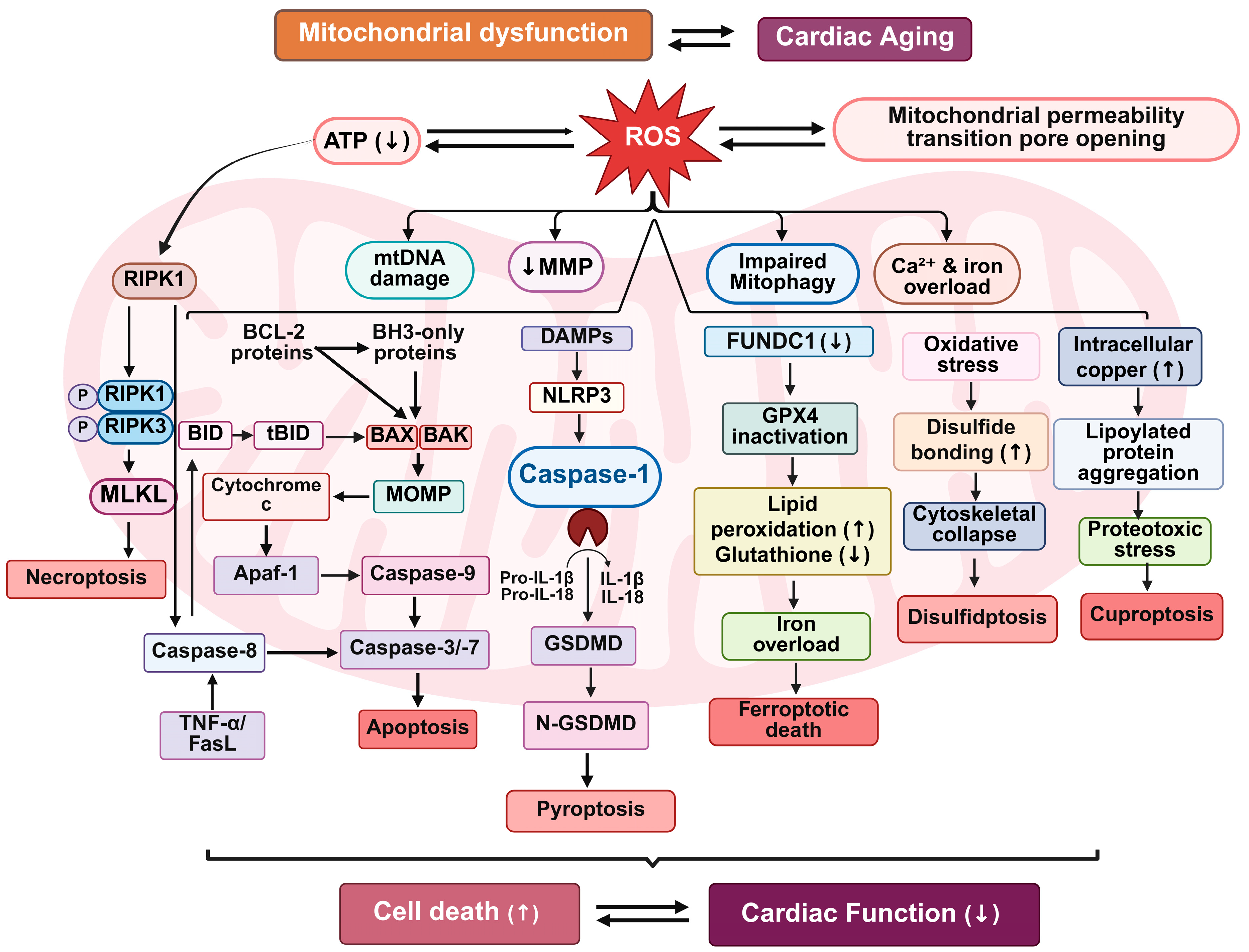
6. Mitochondrial Dysfunction Orchestrates Multimodal Cell Death in Cardiac Aging
6.1. Apoptosis and Mitochondrial Dysfunction
6.2. Necroptosis and Mitochondrial Permeability
6.3. Pyroptosis and Mitochondrial Inflammasomes
6.4. Mitophagy Impairment and Ferroptosis
6.5. Cuproptosis and Disulfidptosis
7. Mitochondrial Sirtuins in Cardiac Aging
8. Therapeutic Potential of Targeting Mitochondria to Combat Age-Related Cardiac Dysfunction
8.1. Amino Acid Metabolism in Maintaining Cardiac Mitochondrial Function
8.2. Enhancing Mitophagy
8.3. Promoting Mitochondrial Biogenesis
8.4. Modulating Mitochondrial Dynamics
8.5. Mitochondria-Targeted Antioxidants
8.6. Small-Molecule Mitochondrial Inhibitors
8.7. Emerging Therapies: Mitochondrial Transplantation and Gene Editing
8.8. Challenges and Future Perspectives
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ribeiro, A.S.F.; Zerolo, B.E.; López-Espuela, F.; Sánchez, R.; Fernandes, V.S. Cardiac System during the Aging Process. Aging Dis. 2023, 14, 1105–1122. [Google Scholar] [CrossRef]
- Tenchov, R.; Sasso, J.M.; Wang, X.; Zhou, Q.A. Aging Hallmarks and Progression and Age-Related Diseases: A Landscape View of Research Advancement. ACS Chem. Neurosci. 2024, 15, 1–30. [Google Scholar] [CrossRef]
- Boyman, L.; Karbowski, M.; Lederer, W.J. Regulation of Mitochondrial ATP Production: Ca2+ Signaling and Quality Control. Trends Mol. Med. 2020, 26, 21–39. [Google Scholar] [CrossRef] [PubMed]
- Popoiu, T.-A.; Maack, C.; Bertero, E. Mitochondrial Calcium Signaling and Redox Homeostasis in Cardiac Health and Disease. Front. Mol. Med. 2023, 3, 1235188. [Google Scholar] [CrossRef]
- Tocchi, A.; Quarles, E.K.; Basisty, N.; Gitari, L.; Rabinovitch, P.S. Mitochondrial Dysfunction in Cardiac Aging. Biochim. Biophys. Acta 2015, 1847, 1424–1433. [Google Scholar] [CrossRef] [PubMed]
- Wei, P.; Zhang, X.; Yan, C.; Sun, S.; Chen, Z.; Lin, F. Mitochondrial dysfunction and aging: Multidimensional mechanisms and therapeutic strategies. Biogerontology 2025, 26, 142. [Google Scholar] [CrossRef] [PubMed]
- Quiles, J.M.; Gustafsson, Å.B. The Role of Mitochondrial Fission in Cardiovascular Health and Disease. Nat. Rev. Cardiol. 2022, 19, 723–736. [Google Scholar] [CrossRef]
- Liang, W.J.; Gustafsson, Å.B. The Aging Heart: Mitophagy at the Center of Rejuvenation. Front. Cardiovasc. Med. 2020, 7, 18. [Google Scholar] [CrossRef]
- Ding, W.; Chen, J.; Zhao, L.; Wu, S.; Chen, X.; Chen, H. Mitochondrial DNA Leakage Triggers Inflammation in Age-Related Cardiovascular Diseases. Front. Cell Dev. Biol. 2024, 12, 1287447. [Google Scholar] [CrossRef]
- Sagar, S.; Gustafsson, A.B. Cardiovascular Aging: The Mitochondrial Influence. J. Cardiovasc. Aging 2023, 3, 33. [Google Scholar] [CrossRef]
- Sheng, S.-Y.; Li, J.-M.; Hu, X.-Y.; Wang, Y. Regulated Cell Death Pathways in Cardiomyopathy. Acta Pharmacol. Sin. 2023, 44, 1521–1535. [Google Scholar] [CrossRef]
- Yu, Y.; Yan, Y.; Niu, F.; Wang, Y.; Chen, X.; Su, G.; Liu, Y.; Zhao, X.; Qian, L.; Liu, P.; et al. Ferroptosis: A Cell Death Connecting Oxidative Stress, Inflammation and Cardiovascular Diseases. Cell Death Discov. 2021, 7, 193. [Google Scholar] [CrossRef]
- Lombard, D.B.; Tishkoff, D.X.; Bao, J. Mitochondrial Sirtuins in the Regulation of Mitochondrial Activity and Metabolic Adaptation. Handb. Exp. Pharmacol. 2011, 206, 163–188. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Hoppe, T. Role of Amino Acid Metabolism in Mitochondrial Homeostasis. Front. Cell Dev. Biol. 2023, 11, 1127618. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Shen, W.; Yao, K.; Wang, H.; Liu, B.; Li, T.; Song, L.; Diao, D.; Mao, G.; Huang, P.; et al. Fine-Tuning of PGC1α Expression Regulates Cardiac Function and Longevity. Circ. Res. 2019, 125, 707–719. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Long, H.; Hou, L.; Feng, B.; Ma, Z.; Wu, Y.; Zeng, Y.; Cai, J.; Zhang, D.-W.; Zhao, G. The Mitophagy Pathway and Its Implications in Human Diseases. Signal Transduct. Target. Ther. 2023, 8, 304. [Google Scholar] [CrossRef]
- Hernández-Camacho, J.D.; Fernández-Ayala, D.J.M.; Vicente-García, C.; Navas-Enamorado, I.; López-Lluch, G.; Oliva, C.; Artuch, R.; Garcia-Villoria, J.; Ribes, A.; de Cabo, R.; et al. Calorie Restriction Rescues Mitochondrial Dysfunction in Adck2-Deficient Skeletal Muscle. Front. Physiol. 2022, 13, 898792. [Google Scholar] [CrossRef]
- Ren, J.; Zhang, Y. Targeting Autophagy in Aging and Aging-Related Cardiovascular Diseases. Trends Pharmacol. Sci. 2018, 39, 1064–1076. [Google Scholar] [CrossRef]
- Chen, L.; Chen, M.; Yang, X.; Hu, Y.; Qiu, C.; Fu, Y.; Lan, X.; Luo, G.; Liu, Q.; Liu, M. Energy Metabolism in Cardiovascular Diseases: Unlocking the Hidden Powerhouse of Cardiac Pathophysiology. Front. Endocrinol. 2025, 16, 1617305. [Google Scholar] [CrossRef]
- Sun, Q.; Karwi, Q.G.; Wong, N.; Lopaschuk, G.D. Advances in Myocardial Energy Metabolism: Metabolic Remodelling in Heart Failure and Beyond. Cardiovasc. Res. 2024, 120, 1996–2016. [Google Scholar] [CrossRef]
- Aon, M.A.; Cortassa, S. Mitochondrial Network Energetics in the Heart. Wiley Interdiscip. Rev. Syst. Biol. Med. 2012, 4, 599–613. [Google Scholar] [CrossRef] [PubMed]
- Hinton, A.; Claypool, S.M.; Neikirk, K.; Senoo, N.; Wanjalla, C.N.; Kirabo, A.; Williams, C.R. Mitochondrial Structure and Function in Human Heart Failure. Circ. Res. 2024, 135, 372–396. [Google Scholar] [CrossRef]
- Mone, P.; Agyapong, E.D.; Morciano, G.; Jankauskas, S.S.; De Luca, A.; Varzideh, F.; Pinton, P.; Santulli, G. Dysfunctional mitochondria elicit bioenergetic decline in the aged heart. J. Cardiovasc. Aging 2024, 4, 13. [Google Scholar] [CrossRef] [PubMed]
- Boengler, K.; Kosiol, M.; Mayr, M.; Schulz, R.; Rohrbach, S. Mitochondria and Ageing: Role in Heart, Skeletal Muscle and Adipose Tissue. J. Cachexia Sarcopenia Muscle 2017, 8, 349–369. [Google Scholar] [CrossRef]
- Nakano, K.; Yamamoto, M.; Yamada, Y.; Nakatsukasa, T.; Kawamatsu, N.; Sato, K.; Machino-Ohtsuka, T.; Murakoshi, N.; Ishizu, T. Mitochondrial Structural Abnormalities and Cardiac Reverse Remodeling in Patients With Systolic Dysfunction. Circ. J. 2024, 89, 101–108. [Google Scholar] [CrossRef]
- Huang, C.; Deng, K.; Wu, M. Mitochondrial Cristae in Health and Disease. Int. J. Biol. Macromol. 2023, 235, 123755. [Google Scholar] [CrossRef] [PubMed]
- Riva, A.; Tandler, B.; Lesnefsky, E.J.; Conti, G.; Loffredo, F.; Vazquez, E.; Hoppel, C.L. Structure of cristae in cardiac mitochondria of aged rat. Mech. Ageing Dev. 2006, 127, 917–921. [Google Scholar] [CrossRef]
- Collins, H.E.; Kane, M.S.; Litovsky, S.H.; Darley-Usmar, V.M.; Young, M.E.; Chatham, J.C.; Zhang, J. Mitochondrial Morphology and Mitophagy in Heart Diseases: Qualitative and Quantitative Analyses Using Transmission Electron Microscopy. Front. Aging 2021, 2, 670267. [Google Scholar] [CrossRef]
- Chen, Q.; Samidurai, A.; Thompson, J.; Hu, Y.; Das, A.; Willard, B.; Lesnefsky, E.J. Endoplasmic Reticulum Stress-Mediated Mitochondrial Dysfunction in Aged Hearts. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165899. [Google Scholar] [CrossRef]
- Xu, X.; Pang, Y.; Fan, X. Mitochondria in Oxidative Stress, Inflammation and Aging: From Mechanisms to Therapeutic Advances. Signal Transduct. Target. Ther. 2025, 10, 190. [Google Scholar] [CrossRef]
- Miró, O.; Casademont, J.; Casals, E.; Perea, M.; Urbano-Márquez, A.; Rustin, P.; Cardellach, F. Aging is associated with increased lipid peroxidation in human hearts, but not with mitochondrial respiratory chain enzyme defects. Cardiovasc. Res. 2000, 47, 624–631. [Google Scholar] [CrossRef]
- Chen, Q.; Thompson, J.; Hu, Y.; Wang, H.; Slotabec, L.; Nguyen, J.D.; Rouhi, N.; Li, J.; Lesnefsky, E.J. High-dose metformin treatment to inhibit complex I during early reperfusion protects the aged mouse heart via decreased mitochondrial permeability transition pore opening. J. Pharmacol. Exp. Ther. 2024, 392, 100529. [Google Scholar] [CrossRef]
- Chen, Q.; Thompson, J.; Hu, Y.; Lesnefsky, E.J. Aging-Induced Mitochondrial Dysfunction: Two Distinct Populations of Mitochondria versus a Combined Population. Am. J. Physiol. Heart Circ. Physiol. 2024, 326, H385–H395. [Google Scholar] [CrossRef]
- Dai, D.-F.; Chen, T.; Wanagat, J.; Laflamme, M.; Marcinek, D.J.; Emond, M.J.; Ngo, C.P.; Prolla, T.A.; Rabinovitch, P.S. Age-Dependent Cardiomyopathy in Mitochondrial Mutator Mice Is Attenuated by Overexpression of Catalase Targeted to Mitochondria. Aging Cell 2010, 9, 536–544. [Google Scholar] [CrossRef]
- Sun, N.; Youle, R.J.; Finkel, T. The Mitochondrial Basis of Aging. Mol. Cell 2016, 61, 654–666. [Google Scholar] [CrossRef]
- Gabillard-Lefort, C.; Thibault, T.; Lenaers, G.; Wiesner, R.J.; Mialet-Perez, J.; Baris, O.R. Heart of the Matter: Mitochondrial Dynamics and Genome Alterations in Cardiac Aging. Mech. Ageing Dev. 2025, 224, 112044. [Google Scholar] [CrossRef] [PubMed]
- Tezze, C.; Romanello, V.; Desbats, M.A.; Fadini, G.P.; Albiero, M.; Favaro, G.; Ciciliot, S.; Soriano, M.E.; Morbidoni, V.; Cerqua, C.; et al. Age-Associated Loss of OPA1 in Muscle Impacts Muscle Mass, Metabolic Homeostasis, Systemic Inflammation, and Epithelial Senescence. Cell Metab. 2017, 25, 1374–1389.e6. [Google Scholar] [CrossRef]
- Sebastián, D.; Sorianello, E.; Segalés, J.; Irazoki, A.; Ruiz-Bonilla, V.; Sala, D.; Planet, E.; Berenguer-Llergo, A.; Muñoz, J.P.; Sánchez-Feutrie, M.; et al. Mfn2 Deficiency Links Age-Related Sarcopenia and Impaired Autophagy to Activation of an Adaptive Mitophagy Pathway. EMBO J. 2016, 35, 1677–1693. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Yu, F.; Tian, Z.; Jia, D. Cardiolipin Remodeling in Cardiovascular Diseases: Implication for Mitochondrial Dysfunction. Acta Physiol. 2025, 241, e70073. [Google Scholar] [CrossRef]
- Jin, J.-Y.; Wei, X.-X.; Zhi, X.-L.; Wang, X.-H.; Meng, D. Drp1-Dependent Mitochondrial Fission in Cardiovascular Disease. Acta Pharmacol. Sin. 2021, 42, 655–664. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.J.; McIntyre, R.L.; Janssens, G.E.; Houtkooper, R.H. Mitochondrial Fission and Fusion: A Dynamic Role in Aging and Potential Target for Age-Related Disease. Mech. Ageing Dev. 2020, 186, 111212. [Google Scholar] [CrossRef]
- Liu, B.-H.; Xu, C.-Z.; Liu, Y.; Lu, Z.-L.; Fu, T.-L.; Li, G.-R.; Deng, Y.; Luo, G.-Q.; Ding, S.; Li, N.; et al. Mitochondrial Quality Control in Human Health and Disease. Mil. Med. Res. 2024, 11, 32. [Google Scholar] [CrossRef]
- Zha, Z.; Wang, J.; Wang, X.; Lu, M.; Guo, Y. Involvement of PINK1/Parkin-Mediated Mitophagy in AGE-Induced Cardiomyocyte Aging. Int. J. Cardiol. 2017, 227, 201–208. [Google Scholar] [CrossRef]
- Qi, X.-M.; Qiao, Y.-B.; Zhang, Y.-L.; Wang, A.-C.; Ren, J.-H.; Wei, H.-Z.; Li, Q.-S. PGC-1α/NRF1-Dependent Cardiac Mitochondrial Biogenesis: A Druggable Pathway of Calycosin against Triptolide Cardiotoxicity. Food Chem. Toxicol. 2023, 171, 113513. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, X.; Wen, Y.; Li, S.; Lu, X.; Xu, R.; Li, C. Endoplasmic Reticulum-Mitochondria Contacts: A Potential Therapy Target for Cardiovascular Remodeling-Associated Diseases. Front. Cell Dev. Biol. 2021, 9, 774989. [Google Scholar] [CrossRef]
- Chen, Q.; Thompson, J.; Hu, Y.; Lesnefsky, E.J. Reversing Mitochondrial Defects in Aged Hearts: Role of Mitochondrial Calpain Activation. Am. J. Physiol. Cell Physiol. 2022, 322, C296–C310. [Google Scholar] [CrossRef]
- Mendoza, A.; Karch, J. Keeping the Beat against Time: Mitochondrial Fitness in the Aging Heart. Front. Aging 2022, 3, 951417. [Google Scholar] [CrossRef]
- Kaludercic, N.; Mialet-Perez, J.; Paolocci, N.; Parini, A.; Di Lisa, F. Monoamine Oxidases as Sources of Oxidants in the Heart. J. Mol. Cell Cardiol. 2014, 73, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Ungvari, Z.; Kaley, G.; de Cabo, R.; Sonntag, W.E.; Csiszar, A. Mechanisms of Vascular Aging: New Perspectives. J. Gerontol. A Biol. Sci. Med. Sci. 2010, 65, 1028–1041. [Google Scholar] [CrossRef] [PubMed]
- Ungvari, Z.; Orosz, Z.; Labinskyy, N.; Rivera, A.; Xiangmin, Z.; Smith, K.; Csiszar, A. Increased Mitochondrial H2O2 Production Promotes Endothelial NF-κB Activation in Aged Rat Arteries. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H37–H47. [Google Scholar] [CrossRef]
- Peoples, J.N.; Saraf, A.; Ghazal, N.; Pham, T.T.; Kwong, J.Q. Mitochondrial Dysfunction and Oxidative Stress in Heart Disease. Exp. Mol. Med. 2019, 51, 1–13. [Google Scholar] [CrossRef]
- Koutouroushis, C.; Sarkar, O. Role of Autophagy in Cardiovascular Disease and Aging. Cureus 2021, 13, e20042. [Google Scholar] [CrossRef]
- Green, A.P.; Klimm, F.; Marshall, A.S.; Leetmaa, R.; Aryaman, J.; Gómez-Durán, A.; Chinnery, P.F.; Jones, N.S. Cryptic Mitochondrial DNA Mutations Coincide with Mid-Late Life and Are Pathophysiologically Informative in Single Cells across Tissues and Species. Nat. Commun. 2025, 16, 2250. [Google Scholar] [CrossRef]
- Luan, Y.; Zhu, X.; Jiao, Y.; Liu, H.; Huang, Z.; Pei, J.; Xu, Y.; Yang, Y.; Ren, K. Cardiac Cell Senescence: Molecular Mechanisms, Key Proteins and Therapeutic Targets. Cell Death Discov. 2024, 10, 78. [Google Scholar] [CrossRef]
- Patyal, P.; Azhar, G.; Zhang, X.; Verma, A.; Wei, J.Y. Cardiac-Specific Overexpression of Serum Response Factor Regulates Age-Associated Decline in Mitochondrial Function. Geroscience 2025. online ahead of print. [Google Scholar] [CrossRef]
- Jeon, S.-M. Regulation and Function of AMPK in Physiology and Diseases. Exp. Mol. Med. 2016, 48, e245. [Google Scholar] [CrossRef] [PubMed]
- Borodkina, A.; Shatrova, A.; Abushik, P.; Nikolsky, N.; Burova, E. Interaction between ROS Dependent DNA Damage, Mitochondria and P38 MAPK Underlies Senescence of Human Adult Stem Cells. Aging 2014, 6, 481–495. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Williams, E.D.; Azhar, G.; Rogers, S.C.; Wei, J.Y. Does P49/STRAP, a SRF-Binding Protein (SRFBP1), Modulate Cardiac Mitochondrial Function in Aging? Exp. Gerontol. 2016, 82, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Azhar, G.; Zhong, Y.; Wei, J.Y. Identification of a Novel Serum Response Factor Cofactor in Cardiac Gene Regulation. J. Biol. Chem. 2004, 279, 55626–55632. [Google Scholar] [CrossRef]
- Krošel, M.; Gabathuler, M.; Moser, L.; Maciukiewicz, M.; Züllig, T.; Seifritz, T.; Tomšič, M.; Distler, O.; Ospelt, C.; Klein, K. The Histone Acetyl Transferases CBP and P300 Regulate Stress Response Pathways in Synovial Fibroblasts at Transcriptional and Functional Levels. Sci. Rep. 2023, 13, 17112. [Google Scholar] [CrossRef]
- Dabravolski, S.A.; Nikiforov, N.G.; Zhuravlev, A.D.; Orekhov, N.A.; Grechko, A.V.; Orekhov, A.N. Role of the mtDNA Mutations and Mitophagy in Inflammaging. Int. J. Mol. Sci. 2022, 23, 1323. [Google Scholar] [CrossRef]
- Shirakabe, A.; Ikeda, Y.; Sciarretta, S.; Zablocki, D.K.; Sadoshima, J. Aging and Autophagy in the Heart. Circ. Res. 2016, 118, 1563–1576. [Google Scholar] [CrossRef]
- Liu, X.; Si, W.; He, L.; Yang, J.; Peng, Y.; Ren, J.; Liu, X.; Jin, T.; Yu, H.; Zhang, Z.; et al. The Existence of a Nonclassical TCA Cycle in the Nucleus That Wires the Metabolic-Epigenetic Circuitry. Signal Transduct. Target. Ther. 2021, 6, 375. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, F.; Zeng, Y.; Li, A.; Yan, J.; Li, P.; Qin, K.; Zhang, T.; Huang, J.; Zhao, M.; et al. Mitochondrial Dysfunction-Mediated Metabolic Remodeling of TCA Cycle Promotes Parkinson’s Disease through Inhibition of H3K4me3 Demethylation. Cell Death Discov. 2025, 11, 351. [Google Scholar] [CrossRef]
- Wen, H.; Deng, H.; Li, B.; Chen, J.; Zhu, J.; Zhang, X.; Yoshida, S.; Zhou, Y. Mitochondrial Diseases: From Molecular Mechanisms to Therapeutic Advances. Signal Transduct. Target. Ther. 2025, 10, 9. [Google Scholar] [CrossRef]
- Tait, S.W.G.; Green, D.R. Mitochondrial Regulation of Cell Death. Cold Spring Harb. Perspect. Biol. 2013, 5, a008706. [Google Scholar] [CrossRef] [PubMed]
- Tian, C.; Liu, Y.; Li, Z.; Zhu, P.; Zhao, M. Mitochondria Related Cell Death Modalities and Disease. Front. Cell Dev. Biol. 2022, 10, 832356. [Google Scholar] [CrossRef]
- Picca, A.; Mankowski, R.T.; Burman, J.L.; Donisi, L.; Kim, J.-S.; Marzetti, E.; Leeuwenburgh, C. Mitochondrial Quality Control Mechanisms as Molecular Targets in Cardiac Ageing. Nat. Rev. Cardiol. 2018, 15, 543–554. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, M.; Ahmad, R.; Tantry, I.Q.; Ahmad, W.; Siddiqui, S.; Alam, M.; Abbas, K.; Moinuddin; Hassan, M.I.; Habib, S.; et al. Apoptosis: A Comprehensive Overview of Signaling Pathways, Morphological Changes, and Physiological Significance and Therapeutic Implications. Cells 2024, 13, 1838. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.T.; Wei, S.; Nguyen, T.H.; Jo, Y.; Zhang, Y.; Park, W.; Gariani, K.; Oh, C.-M.; Kim, H.H.; Ha, K.-T.; et al. Mitochondria-Associated Programmed Cell Death as a Therapeutic Target for Age-Related Disease. Exp. Mol. Med. 2023, 55, 1595–1619. [Google Scholar] [CrossRef]
- Kim, H.-E.; Du, F.; Fang, M.; Wang, X. Formation of Apoptosome Is Initiated by Cytochrome C-Induced dATP Hydrolysis and Subsequent Nucleotide Exchange on Apaf-1. Proc. Natl. Acad. Sci. USA 2005, 102, 17545–17550. [Google Scholar] [CrossRef]
- Kwak, H.-B. Effects of Aging and Exercise Training on Apoptosis in the Heart. J. Exerc. Rehabil. 2013, 9, 212–219, Erratum in J. Exerc. Rehabil. 2013, 9, 549. [Google Scholar] [CrossRef]
- Kale, J.; Osterlund, E.J.; Andrews, D.W. BCL-2 Family Proteins: Changing Partners in the Dance towards Death. Cell Death Differ. 2018, 25, 65–80. [Google Scholar] [CrossRef]
- Roufayel, R.; Younes, K.; Al-Sabi, A.; Murshid, N. BH3-Only Proteins Noxa and Puma Are Key Regulators of Induced Apoptosis. Life 2022, 12, 256. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Azhar, G.; Gao, W.; Zhang, X.; Wei, J.Y. Bcl-2 and Bax Expression in Adult Rat Hearts after Coronary Occlusion: Age-Associated Differences. Am. J. Physiol. 1998, 275, R315–R322. [Google Scholar] [CrossRef]
- Azhar, G.; Liu, L.; Zhang, X.; Wei, J.Y. Influence of Age on Hypoxia/Reoxygenation-Induced DNA Fragmentation and Bcl-2, Bcl-Xl, Bax and Fas in the Rat Heart and Brain. Mech. Ageing Dev. 1999, 112, 5–25. [Google Scholar] [CrossRef]
- Borrás, C.; Mas-Bargues, C.; Román-Domínguez, A.; Sanz-Ros, J.; Gimeno-Mallench, L.; Inglés, M.; Gambini, J.; Viña, J. BCL-xL, a Mitochondrial Protein Involved in Successful Aging: From C. Elegans to Human Centenarians. Int. J. Mol. Sci. 2020, 21, 418. [Google Scholar] [CrossRef] [PubMed]
- Summer, S.; Borrell-Pages, M.; Bruno, R.-M.; Climie, R.E.; Dipla, K.; Dogan, A.; Eruslanova, K.; Fraenkel, E.; Mattace-Raso, F.; Pugh, C.J.A.; et al. Centenarians-the Way to Healthy Vascular Ageing and Longevity: A Review from VascAgeNet. Geroscience 2025, 47, 685–702. [Google Scholar] [CrossRef] [PubMed]
- Guerrache, A.; Micheau, O. TNF-Related Apoptosis-Inducing Ligand: Non-Apoptotic Signalling. Cells 2024, 13, 521. [Google Scholar] [CrossRef]
- Hung, C.-L.; Chang, H.-H.; Lee, S.W.; Chiang, Y.-W. Stepwise Activation of the Pro-Apoptotic Protein Bid at Mitochondrial Membranes. Cell Death Differ. 2021, 28, 1910–1925. [Google Scholar] [CrossRef]
- DeRoo, E.; Zhou, T.; Liu, B. The Role of RIPK1 and RIPK3 in Cardiovascular Disease. Int. J. Mol. Sci. 2020, 21, 8174. [Google Scholar] [CrossRef]
- Chen, B.; Xie, K.; Zhang, J.; Yang, L.; Zhou, H.; Zhang, L.; Peng, R. Comprehensive Analysis of Mitochondrial Dysfunction and Necroptosis in Intracranial Aneurysms from the Perspective of Predictive, Preventative, and Personalized Medicine. Apoptosis 2023, 28, 1452–1468. [Google Scholar] [CrossRef]
- Zhang, X.; Gao, Y.; Zhang, S.; Wang, Y.; Pei, X.; Chen, Y.; Zhang, J.; Zhang, Y.; Du, Y.; Hao, S.; et al. Mitochondrial Dysfunction in the Regulation of Aging and Aging-Related Diseases. Cell Commun. Signal. 2025, 23, 290. [Google Scholar] [CrossRef]
- Yang, X.; Li, G.; Lou, P.; Zhang, M.; Yao, K.; Xiao, J.; Chen, Y.; Xu, J.; Tian, S.; Deng, M.; et al. Excessive Nucleic Acid R-Loops Induce Mitochondria-Dependent Epithelial Cell Necroptosis and Drive Spontaneous Intestinal Inflammation. Proc. Natl. Acad. Sci. USA 2024, 121, e2307395120. [Google Scholar] [CrossRef]
- Verma, A.; Azhar, G.; Zhang, X.; Patyal, P.; Kc, G.; Sharma, S.; Che, Y.; Wei, J.Y. P. gingivalis-LPS Induces Mitochondrial Dysfunction Mediated by Neuroinflammation through Oxidative Stress. Int. J. Mol. Sci. 2023, 24, 950. [Google Scholar] [CrossRef]
- Verma, A.; Azhar, G.; Patyal, P.; Zhang, W.; Zhang, X.; Wei, J.Y. Proteomic Analysis of P. Gingivalis-Lipopolysaccharide Induced Neuroinflammation in SH-SY5Y and HMC3 Cells. Geroscience 2024, 46, 4315–4332. [Google Scholar] [CrossRef]
- Verma, A.; Azhar, G.; Patyal, P.; Zhang, X.; Wei, J.Y. Porphyromonas Gingivalis-Lipopolysaccharide Induced Caspase-4 Dependent Noncanonical Inflammasome Activation Drives Alzheimer’s Disease Pathologies. Cells 2025, 14, 804. [Google Scholar] [CrossRef] [PubMed]
- Azhar, G.; Nagano, K.; Patyal, P.; Zhang, X.; Verma, A.; Wei, J.Y. Deletion of Interleukin-1β Converting Enzyme Alters Mouse Cardiac Structure and Function. Biology 2024, 13, 172. [Google Scholar] [CrossRef] [PubMed]
- Evavold, C.L.; Hafner-Bratkovič, I.; Devant, P.; D’Andrea, J.M.; Ngwa, E.M.; Boršić, E.; Doench, J.G.; LaFleur, M.W.; Sharpe, A.H.; Thiagarajah, J.R.; et al. Control of Gasdermin D Oligomerization and Pyroptosis by the Ragulator-Rag-mTORC1 Pathway. Cell 2021, 184, 4495–4511.e19. [Google Scholar] [CrossRef]
- Miao, R.; Jiang, C.; Chang, W.Y.; Zhang, H.; An, J.; Ho, F.; Chen, P.; Zhang, H.; Junqueira, C.; Amgalan, D.; et al. Gasdermin D Permeabilization of Mitochondrial Inner and Outer Membranes Accelerates and Enhances Pyroptosis. Immunity 2023, 56, 2523–2541.e8. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Jia, Y.-C.; Ding, Y.-X.; Bai, J.; Cao, F.; Li, F. The Crosstalk between Ferroptosis and Mitochondrial Dynamic Regulatory Networks. Int. J. Biol. Sci. 2023, 19, 2756–2771. [Google Scholar] [CrossRef]
- Bi, Y.; Liu, S.; Qin, X.; Abudureyimu, M.; Wang, L.; Zou, R.; Ajoolabady, A.; Zhang, W.; Peng, H.; Ren, J.; et al. FUNDC1 Interacts with GPx4 to Govern Hepatic Ferroptosis and Fibrotic Injury through a Mitophagy-Dependent Manner. J. Adv. Res. 2024, 55, 45–60. [Google Scholar] [CrossRef]
- Fratta Pasini, A.M.; Stranieri, C.; Busti, F.; Di Leo, E.G.; Girelli, D.; Cominacini, L. New Insights into the Role of Ferroptosis in Cardiovascular Diseases. Cells 2023, 12, 867. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Chen, X.-Z.; Wang, Y.-H.; Cheng, X.-L.; Zhao, Y.; Zhou, L.-Y.; Wang, K. Emerging Roles of Ferroptosis in Cardiovascular Diseases. Cell Death Discov. 2022, 8, 394. [Google Scholar] [CrossRef] [PubMed]
- Stockwell, B.R.; Jiang, X.; Gu, W. Emerging Mechanisms and Disease Relevance of Ferroptosis. Trends Cell Biol. 2020, 30, 478–490. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chen, Z.; Shang, H.; Guo, J. The Molecular Mechanisms of Cuproptosis and Its Relevance to Atherosclerosis. Biomol. Biomed. 2025, 25, 1709–1722. [Google Scholar] [CrossRef]
- Chen, L.; Wei, J.; Deng, G.; Xu, G. Disulfidptosis-Related Gene in Acute Myocardial Infarction and Its Diagnostic Value and Functions Based on Bioinformatics Analysis and Machine Learning. Front. Cardiovasc. Med. 2025, 12, 1513342. [Google Scholar] [CrossRef]
- Carollo, C.; Sorce, A.; Cirafici, E.; Mulè, G.; Caimi, G. Sirtuins and Resveratrol in Cardiorenal Diseases: A Narrative Review of Mechanisms and Therapeutic Potential. Nutrients 2025, 17, 1212. [Google Scholar] [CrossRef]
- Ding, Y.-N.; Wang, H.-Y.; Chen, X.-F.; Tang, X.; Chen, H.-Z. Roles of Sirtuins in Cardiovascular Diseases: Mechanisms and Therapeutics. Circ. Res. 2025, 136, 524–550. [Google Scholar] [CrossRef]
- Patyal, P.; Ameer, F.S.; Verma, A.; Zhang, X.; Azhar, G.; Shrivastava, J.; Sharma, S.; Zhang, R.; Wei, J.Y. The Role of Sirtuin-1 Isoforms in Regulating Mitochondrial Function. Curr. Issues Mol. Biol. 2024, 46, 8835–8851. [Google Scholar] [CrossRef]
- Perico, L.; Morigi, M.; Pezzotta, A.; Corna, D.; Brizi, V.; Conti, S.; Zanchi, C.; Sangalli, F.; Trionfini, P.; Buttò, S.; et al. Post-Translational Modifications by SIRT3 de-2-Hydroxyisobutyrylase Activity Regulate Glycolysis and Enable Nephrogenesis. Sci. Rep. 2021, 11, 23580. [Google Scholar] [CrossRef]
- Mathias, R.A.; Greco, T.M.; Oberstein, A.; Budayeva, H.G.; Chakrabarti, R.; Rowland, E.A.; Kang, Y.; Shenk, T.; Cristea, I.M. Sirtuin 4 Is a Lipoamidase Regulating Pyruvate Dehydrogenase Complex Activity. Cell 2014, 159, 1615–1625. [Google Scholar] [CrossRef] [PubMed]
- Du, J.; Zhou, Y.; Su, X.; Yu, J.J.; Khan, S.; Jiang, H.; Kim, J.; Woo, J.; Kim, J.H.; Choi, B.H.; et al. Sirt5 Is a NAD-Dependent Protein Lysine Demalonylase and Desuccinylase. Science 2011, 334, 806–809. [Google Scholar] [CrossRef]
- Sidorova-Darmos, E.; Sommer, R.; Eubanks, J.H. The Role of SIRT3 in the Brain Under Physiological and Pathological Conditions. Front. Cell Neurosci. 2018, 12, 196. [Google Scholar] [CrossRef] [PubMed]
- Hafner, A.V.; Dai, J.; Gomes, A.P.; Xiao, C.-Y.; Palmeira, C.M.; Rosenzweig, A.; Sinclair, D.A. Regulation of the mPTP by SIRT3-Mediated Deacetylation of CypD at Lysine 166 Suppresses Age-Related Cardiac Hypertrophy. Aging 2010, 2, 914–923. [Google Scholar] [CrossRef]
- Porter, G.A.; Urciuoli, W.R.; Brookes, P.S.; Nadtochiy, S.M. SIRT3 Deficiency Exacerbates Ischemia-Reperfusion Injury: Implication for Aged Hearts. Am. J. Physiol. Heart Circ. Physiol. 2014, 306, H1602–H1609. [Google Scholar] [CrossRef] [PubMed]
- Ahn, B.-H.; Kim, H.-S.; Song, S.; Lee, I.H.; Liu, J.; Vassilopoulos, A.; Deng, C.-X.; Finkel, T. A Role for the Mitochondrial Deacetylase Sirt3 in Regulating Energy Homeostasis. Proc. Natl. Acad. Sci. USA 2008, 105, 14447–14452. [Google Scholar] [CrossRef]
- Liu, Y.-P.; Wen, R.; Liu, C.-F.; Zhang, T.-N.; Yang, N. Cellular and Molecular Biology of Sirtuins in Cardiovascular Disease. Biomed. Pharmacother. 2023, 164, 114931. [Google Scholar] [CrossRef]
- Wu, Y.-T.; Lee, H.-C.; Liao, C.-C.; Wei, Y.-H. Regulation of Mitochondrial FoF1ATPase Activity by Sirt3-Catalyzed Deacetylation and Its Deficiency in Human Cells Harboring 4977bp Deletion of Mitochondrial DNA. Biochim. Biophys. Acta 2013, 1832, 216–227. [Google Scholar] [CrossRef]
- Guo, L.; Yin, A.; Zhang, Q.; Zhong, T.; O’Rourke, S.T.; Sun, C. Angiotensin-(1-7) Attenuates Angiotensin II-Induced Cardiac Hypertrophy via a Sirt3-Dependent Mechanism. Am. J. Physiol. Heart Circ. Physiol. 2017, 312, H980–H991. [Google Scholar] [CrossRef]
- Feng, X.; Wang, Y.; Chen, W.; Xu, S.; Li, L.; Geng, Y.; Shen, A.; Gao, H.; Zhang, L.; Liu, S. SIRT3 Inhibits Cardiac Hypertrophy by Regulating PARP-1 Activity. Aging 2020, 12, 4178–4192. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-J.; Fu, Y.-C.; Yu, W.; Wang, W. SIRT3 Protects Cardiomyocytes from Oxidative Stress-Mediated Cell Death by Activating NF-κB. Biochem. Biophys. Res. Commun. 2013, 430, 798–803. [Google Scholar] [CrossRef]
- Farhadi, Z.; Esmailidehaj, M.; Masoumi, S.; Azizian, H. Sirtuins as Endogenous Regulators of Cardiac Fibrosis: A Current Perspective. Cardiovasc. Toxicol. 2025, 25, 1634–1649. [Google Scholar] [CrossRef] [PubMed]
- Hirschey, M.D.; Shimazu, T.; Goetzman, E.; Jing, E.; Schwer, B.; Lombard, D.B.; Grueter, C.A.; Harris, C.; Biddinger, S.; Ilkayeva, O.R.; et al. SIRT3 Regulates Mitochondrial Fatty-Acid Oxidation by Reversible Enzyme Deacetylation. Nature 2010, 464, 121–125. [Google Scholar] [CrossRef]
- Shimazu, T.; Hirschey, M.D.; Hua, L.; Dittenhafer-Reed, K.E.; Schwer, B.; Lombard, D.B.; Li, Y.; Bunkenborg, J.; Alt, F.W.; Denu, J.M.; et al. SIRT3 Deacetylates Mitochondrial 3-Hydroxy-3-Methylglutaryl CoA Synthase 2 and Regulates Ketone Body Production. Cell Metab. 2010, 12, 654–661. [Google Scholar] [CrossRef]
- Min, Z.; Gao, J.; Yu, Y. The Roles of Mitochondrial SIRT4 in Cellular Metabolism. Front. Endocrinol. 2018, 9, 783. [Google Scholar] [CrossRef] [PubMed]
- Laurent, G.; German, N.J.; Saha, A.K.; de Boer, V.C.J.; Davies, M.; Koves, T.R.; Dephoure, N.; Fischer, F.; Boanca, G.; Vaitheesvaran, B.; et al. SIRT4 Coordinates the Balance between Lipid Synthesis and Catabolism by Repressing Malonyl CoA Decarboxylase. Mol. Cell 2013, 50, 686–698. [Google Scholar] [CrossRef]
- Rardin, M.J.; He, W.; Nishida, Y.; Newman, J.C.; Carrico, C.; Danielson, S.R.; Guo, A.; Gut, P.; Sahu, A.K.; Li, B.; et al. SIRT5 Regulates the Mitochondrial Lysine Succinylome and Metabolic Networks. Cell. Metab. 2013, 18, 920–933. [Google Scholar] [CrossRef]
- Nakagawa, T.; Guarente, L. Urea Cycle Regulation by Mitochondrial Sirtuin, SIRT5. Aging 2009, 1, 578–581. [Google Scholar] [CrossRef]
- Fabbrizi, E.; Fiorentino, F.; Carafa, V.; Altucci, L.; Mai, A.; Rotili, D. Emerging Roles of SIRT5 in Metabolism, Cancer, and SARS-CoV-2 Infection. Cells 2023, 12, 852. [Google Scholar] [CrossRef]
- Shen, R.; Zhang, Y. Relationship between Amino Acid Metabolism and Inflammation in Coronary Heart Disease (Review). Int. J. Mol. Med. 2025, 56, 120. [Google Scholar] [CrossRef]
- Azhar, G.; Verma, A.; Zhang, X.; Pangle, A.; Patyal, P.; Zhang, W.; Che, Y.; Coker, K.; Wolfe, R.R.; Wei, J.Y. Differential Plasma Protein Expression after Ingestion of Essential Amino Acid-Based Dietary Supplement Verses Whey Protein in Low Physical Functioning Older Adults. Geroscience 2023, 45, 1729–1743. [Google Scholar] [CrossRef]
- Azhar, G.; Verma, A.; Robeson, M.S.; Patyal, P.; Nookaew, I.; Sharma, S.; Pangle, A.; Che, Y.; Wolfe, R.R.; Wei, J.Y. Short-Term Ingestion of Essential Amino Acid Based Nutritional Supplements or Whey Protein Improves the Physical Function of Older Adults Independently of Gut Microbiome. Mol. Nutr. Food Res. 2024, 68, e2300716. [Google Scholar] [CrossRef] [PubMed]
- D’Antona, G.; Ragni, M.; Cardile, A.; Tedesco, L.; Dossena, M.; Bruttini, F.; Caliaro, F.; Corsetti, G.; Bottinelli, R.; Carruba, M.O.; et al. Branched-Chain Amino Acid Supplementation Promotes Survival and Supports Cardiac and Skeletal Muscle Mitochondrial Biogenesis in Middle-Aged Mice. Cell Metab. 2010, 12, 362–372. [Google Scholar] [CrossRef]
- Buondonno, I.; Sassi, F.; Carignano, G.; Dutto, F.; Ferreri, C.; Pili, F.G.; Massaia, M.; Nisoli, E.; Ruocco, C.; Porrino, P.; et al. From Mitochondria to Healthy Aging: The Role of Branched-Chain Amino Acids Treatment: MATeR a Randomized Study. Clin. Nutr. 2020, 39, 2080–2091. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Liu, W.-J.; Yang, J.; Zhao, S.-S.; Liu, H.-X. The Role of Branched-Chain Amino Acids and Branched-Chain α-Keto Acid Dehydrogenase Kinase in Metabolic Disorders. Front. Nutr. 2022, 9, 932670. [Google Scholar] [CrossRef] [PubMed]
- Blair, M.C.; Neinast, M.D.; Arany, Z. Whole-Body Metabolic Fate of Branched-Chain Amino Acids. Biochem. J. 2021, 478, 765–776. [Google Scholar] [CrossRef]
- Bo, T.; Fujii, J. Primary Roles of Branched Chain Amino Acids (BCAAs) and Their Metabolism in Physiology and Metabolic Disorders. Molecules 2024, 30, 56. [Google Scholar] [CrossRef]
- Sharma, S.; Zhang, X.; Azhar, G.; Patyal, P.; Verma, A.; Kc, G.; Wei, J.Y. Valine Improves Mitochondrial Function and Protects against Oxidative Stress. Biosci. Biotechnol. Biochem. 2024, 88, 168–176. [Google Scholar] [CrossRef]
- Sun, H.; Olson, K.C.; Gao, C.; Prosdocimo, D.A.; Zhou, M.; Wang, Z.; Jeyaraj, D.; Youn, J.-Y.; Ren, S.; Liu, Y.; et al. Catabolic Defect of Branched-Chain Amino Acids Promotes Heart Failure. Circulation 2016, 133, 2038–2049. [Google Scholar] [CrossRef]
- Schwalb, H.; Kushnir, T.; Navon, G.; Yaroslavsky, E.; Borman, J.B.; Uretzky, G. The Protective Effect of Enriched Branched Chain Amino Acid Formulation in the Ischemic Heart: A Phosphorous-31 Nuclear Magnetic Resonance Study. J. Mol. Cell. Cardiol. 1987, 19, 991–998. [Google Scholar] [CrossRef]
- Hatazawa, Y.; Tadaishi, M.; Nagaike, Y.; Morita, A.; Ogawa, Y.; Ezaki, O.; Takai-Igarashi, T.; Kitaura, Y.; Shimomura, Y.; Kamei, Y.; et al. PGC-1α-Mediated Branched-Chain Amino Acid Metabolism in the Skeletal Muscle. PLoS ONE 2014, 9, e91006. [Google Scholar] [CrossRef]
- Hotta, K.; Taniguchi, R.; Nakayama, H.; Yamaguchi, F.; Sato, Y. The Effects of an Oral Nutritional Supplement with Whey Peptides and Branched-Chain Amino Acids for Cardiac Rehabilitation of Patients with Chronic Heart Failure. Int. Heart J. 2021, 62, 1342–1347. [Google Scholar] [CrossRef]
- Lu, G.; Sun, H.; She, P.; Youn, J.Y.; Warburton, S.; Ping, P.; Vondriska, T.M.; Cai, H.; Lynch, C.J.; Wang, Y. Protein phosphatase 2Cm is a critical regulator of branched-chain amino acid catabolism in mice and cultured cells. J. Clin. Investig. 2009, 119, 1678–1687. [Google Scholar] [CrossRef]
- Xiong, Y.; Jiang, L.; Li, T. Aberrant Branched-Chain Amino Acid Catabolism in Cardiovascular Diseases. Front. Cardiovasc. Med. 2022, 9, 965899. [Google Scholar] [CrossRef] [PubMed]
- Murashige, D.; Jung, J.W.; Neinast, M.D.; Levin, M.G.; Chu, Q.; Lambert, J.P.; Garbincius, J.F.; Kim, B.; Hoshino, A.; Marti-Pamies, I.; et al. Extra-Cardiac BCAA Catabolism Lowers Blood Pressure and Protects from Heart Failure. Cell Metab. 2022, 34, 1749–1764.e7. [Google Scholar] [CrossRef]
- Lian, K.; Guo, X.; Wang, Q.; Liu, Y.; Wang, R.-T.; Gao, C.; Li, C.-Y.; Li, C.-X.; Tao, L. PP2Cm Overexpression Alleviates MI/R Injury Mediated by a BCAA Catabolism Defect and Oxidative Stress in Diabetic Mice. Eur. J. Pharmacol. 2020, 866, 172796. [Google Scholar] [CrossRef] [PubMed]
- Durante, W. The Emerging Role of L-Glutamine in Cardiovascular Health and Disease. Nutrients 2019, 11, 2092. [Google Scholar] [CrossRef]
- Fung, T.S.; Ryu, K.W.; Thompson, C.B. Arginine: At the Crossroads of Nitrogen Metabolism. EMBO J. 2025, 44, 1275–1293. [Google Scholar] [CrossRef] [PubMed]
- Ryu, D.; Mouchiroud, L.; Andreux, P.A.; Katsyuba, E.; Moullan, N.; Nicolet-Dit-Félix, A.A.; Williams, E.G.; Jha, P.; Lo Sasso, G.; Huzard, D.; et al. Urolithin A Induces Mitophagy and Prolongs Lifespan in C. Elegans and Increases Muscle Function in Rodents. Nat. Med. 2016, 22, 879–888. [Google Scholar] [CrossRef]
- Eisenberg, T.; Abdellatif, M.; Schroeder, S.; Primessnig, U.; Stekovic, S.; Pendl, T.; Harger, A.; Schipke, J.; Zimmermann, A.; Schmidt, A.; et al. Cardioprotection and Lifespan Extension by the Natural Polyamine Spermidine. Nat. Med. 2016, 22, 1428–1438. [Google Scholar] [CrossRef]
- Tan, M.; Yin, Y.; Ma, X.; Zhang, J.; Pan, W.; Tan, M.; Zhao, Y.; Yang, T.; Jiang, T.; Li, H. Glutathione System Enhancement for Cardiac Protection: Pharmacological Options against Oxidative Stress and Ferroptosis. Cell Death Dis. 2023, 14, 131. [Google Scholar] [CrossRef]
- Zhang, H.; Ryu, D.; Wu, Y.; Gariani, K.; Wang, X.; Luan, P.; D’Amico, D.; Ropelle, E.R.; Lutolf, M.P.; Aebersold, R.; et al. NAD+ Repletion Improves Mitochondrial and Stem Cell Function and Enhances Life Span in Mice. Science 2016, 352, 1436–1443. [Google Scholar] [CrossRef] [PubMed]
- Palikaras, K.; Lionaki, E.; Tavernarakis, N. Coordination of Mitophagy and Mitochondrial Biogenesis during Ageing in C. Elegans. Nature 2015, 521, 525–528. [Google Scholar] [CrossRef] [PubMed]
- Scarpulla, R.C.; Vega, R.B.; Kelly, D.P. Transcriptional Integration of Mitochondrial Biogenesis. Trends Endocrinol. Metab. 2012, 23, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Colman, R.J.; Beasley, T.M.; Kemnitz, J.W.; Johnson, S.C.; Weindruch, R.; Anderson, R.M. Caloric Restriction Reduces Age-Related and All-Cause Mortality in Rhesus Monkeys. Nat. Commun. 2014, 5, 3557. [Google Scholar] [CrossRef]
- Kemnitz, J.W. Calorie Restriction and Aging in Nonhuman Primates. ILAR J. 2011, 52, 66–77. [Google Scholar] [CrossRef]
- Lagouge, M.; Argmann, C.; Gerhart-Hines, Z.; Meziane, H.; Lerin, C.; Daussin, F.; Messadeq, N.; Milne, J.; Lambert, P.; Elliott, P.; et al. Resveratrol Improves Mitochondrial Function and Protects against Metabolic Disease by Activating SIRT1 and PGC-1alpha. Cell 2006, 127, 1109–1122. [Google Scholar] [CrossRef]
- Fan, W.; Evans, R.M. Exercise Mimetics: Impact on Health and Performance. Cell Metab. 2017, 25, 242–247. [Google Scholar] [CrossRef]
- Chan, D.C. Mitochondrial Dynamics and Its Involvement in Disease. Annu. Rev. Pathol. 2020, 15, 235–259. [Google Scholar] [CrossRef]
- Ruiz, A.; Alberdi, E.; Matute, C. Mitochondrial Division Inhibitor 1 (Mdivi-1) Protects Neurons against Excitotoxicity through the Modulation of Mitochondrial Function and Intracellular Ca2+ Signaling. Front. Mol. Neurosci. 2018, 11, 3. [Google Scholar] [CrossRef]
- Poznyak, A.V.; Kirichenko, T.V.; Borisov, E.E.; Shakhpazyan, N.K.; Kartuesov, A.G.; Orekhov, A.N. Mitochondrial Implications in Cardiovascular Aging and Diseases: The Specific Role of Mitochondrial Dynamics and Shifts. Int. J. Mol. Sci. 2022, 23, 2951. [Google Scholar] [CrossRef]
- Murphy, M.P.; Smith, R.A.J. Targeting Antioxidants to Mitochondria by Conjugation to Lipophilic Cations. Annu. Rev. Pharmacol. Toxicol. 2007, 47, 629–656. [Google Scholar] [CrossRef] [PubMed]
- Gioscia-Ryan, R.A.; Battson, M.L.; Cuevas, L.M.; Eng, J.S.; Murphy, M.P.; Seals, D.R. Mitochondria-Targeted Antioxidant Therapy with MitoQ Ameliorates Aortic Stiffening in Old Mice. J. Appl. Physiol. 2018, 124, 1194–1202. [Google Scholar] [CrossRef] [PubMed]
- Olgar, Y.; Billur, D.; Tuncay, E.; Turan, B. MitoTEMPO Provides an Antiarrhythmic Effect in Aged-Rats through Attenuation of Mitochondrial Reactive Oxygen Species. Exp. Gerontol. 2020, 136, 110961. [Google Scholar] [CrossRef]
- Chiao, Y.A.; Zhang, H.; Sweetwyne, M.; Whitson, J.; Ting, Y.S.; Basisty, N.; Pino, L.K.; Quarles, E.; Nguyen, N.-H.; Campbell, M.D.; et al. Late-Life Restoration of Mitochondrial Function Reverses Cardiac Dysfunction in Old Mice. eLife 2020, 9, e55513. [Google Scholar] [CrossRef]
- Zikaki, K.; Kiachaki, E.; Gaitanaki, C.; Aggeli, I.-K. “Villains” Turning Good: Antimycin A and Rotenone, Mitochondrial Respiratory Chain Inhibitors, Protect H9c2 Cardiac Cells Against Insults Triggering the Intrinsic Apoptotic Pathway. Int. J. Mol. Sci. 2025, 26, 2435. [Google Scholar] [CrossRef]
- Miwa, S.; Kashyap, S.; Chini, E.; von Zglinicki, T. Mitochondrial Dysfunction in Cell Senescence and Aging. J. Clin. Investig. 2022, 132, e158447. [Google Scholar] [CrossRef] [PubMed]
- Symersky, J.; Osowski, D.; Walters, D.E.; Mueller, D.M. Oligomycin Frames a Common Drug-Binding Site in the ATP Synthase. Proc. Natl. Acad. Sci. USA 2012, 109, 13961–13965. [Google Scholar] [CrossRef]
- Cadenas, S. Mitochondrial Uncoupling, ROS Generation and Cardioprotection. Biochim. Biophys. Acta Bioenerg. 2018, 1859, 940–950. [Google Scholar] [CrossRef]
- Patyal, P.; Nguyen, B.; Zhang, X.; Azhar, G.; Ameer, F.S.; Verma, A.; Crane, J.; Kc, G.; Che, Y.; Wei, J.Y. Rho/SRF Inhibitor Modulates Mitochondrial Functions. Int. J. Mol. Sci. 2022, 23, 11536. [Google Scholar] [CrossRef]
- Patyal, P.; Zhang, X.; Verma, A.; Azhar, G.; Wei, J.Y. Inhibitors of Rho/MRTF/SRF Transcription Pathway Regulate Mitochondrial Function. Cells 2024, 13, 392. [Google Scholar] [CrossRef]
- Masuzawa, A.; Black, K.M.; Pacak, C.A.; Ericsson, M.; Barnett, R.J.; Drumm, C.; Seth, P.; Bloch, D.B.; Levitsky, S.; Cowan, D.B.; et al. Transplantation of Autologously Derived Mitochondria Protects the Heart from Ischemia-Reperfusion Injury. Am. J. Physiol. Heart Circ. Physiol. 2013, 304, H966–H982. [Google Scholar] [CrossRef]
- Yin, T.; Luo, J.; Huang, D.; Li, H. Current Progress of Mitochondrial Genome Editing by CRISPR. Front. Physiol. 2022, 13, 883459. [Google Scholar] [CrossRef]
- Song, M.; Ye, L.; Yan, Y.; Li, X.; Han, X.; Hu, S.; Yu, M. Mitochondrial Diseases and mtDNA Editing. Genes Dis. 2024, 11, 101057. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhou, M.; Li, H.; Liu, D.; Liao, P.; Zong, Y.; Zhang, C.; Zou, W.; Gao, J. Mitochondrial Heterogeneity in Diseases. Signal Transduct. Target. Ther. 2023, 8, 311. [Google Scholar] [CrossRef]
- Gropman, A.L.; Uittenbogaard, M.N.; Chiaramello, A.E. Challenges and Opportunities to Bridge Translational to Clinical Research for Personalized Mitochondrial Medicine. Neurotherapeutics 2024, 21, e00311. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, S.; Qiu, Y.; Zhou, M.; Chen, M.; Hu, Y.; Hong, S.; Jiang, L.; Guo, Y. Circulating FGF21 and GDF15 as Biomarkers for Screening, Diagnosis, and Severity Assessment of Primary Mitochondrial Disorders in Children. Front. Pediatr. 2022, 10, 851534. [Google Scholar] [CrossRef] [PubMed]
- Mengozzi, A.; Armenia, S.; De Biase, N.; Punta, L.D.; Cappelli, F.; Duranti, E.; Nannipieri, V.; Remollino, R.; Tricò, D.; Virdis, A.; et al. Circulating Mitochondrial DNA Signature in Cardiometabolic Patients. Cardiovasc. Diabetol. 2025, 24, 106. [Google Scholar] [CrossRef] [PubMed]
- Steele, H.E.; Horvath, R.; Lyon, J.J.; Chinnery, P.F. Monitoring Clinical Progression with Mitochondrial Disease Biomarkers. Brain 2017, 140, 2530–2540. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patyal, P.; Azhar, G.; Verma, A.; Sharma, S.; Shrivastava, J.; Abdi, S.A.H.; Zhang, X.; Wei, J.Y. Mitochondrial Dynamics in Aging Heart. Biomedicines 2025, 13, 2603. https://doi.org/10.3390/biomedicines13112603
Patyal P, Azhar G, Verma A, Sharma S, Shrivastava J, Abdi SAH, Zhang X, Wei JY. Mitochondrial Dynamics in Aging Heart. Biomedicines. 2025; 13(11):2603. https://doi.org/10.3390/biomedicines13112603
Chicago/Turabian StylePatyal, Pankaj, Gohar Azhar, Ambika Verma, Shakshi Sharma, Jyotsna Shrivastava, Sayed Aliul Hasan Abdi, Xiaomin Zhang, and Jeanne Y. Wei. 2025. "Mitochondrial Dynamics in Aging Heart" Biomedicines 13, no. 11: 2603. https://doi.org/10.3390/biomedicines13112603
APA StylePatyal, P., Azhar, G., Verma, A., Sharma, S., Shrivastava, J., Abdi, S. A. H., Zhang, X., & Wei, J. Y. (2025). Mitochondrial Dynamics in Aging Heart. Biomedicines, 13(11), 2603. https://doi.org/10.3390/biomedicines13112603





