Incidence Rate and Determinants of Recurrent Cholesteatoma Following Surgical Management: A Systematic Review, Subgroup, and Meta-Regression Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Study Selection and Data Extraction
2.4. Risk of Bias and Quality Assessment
2.5. Statistical Analysis
3. Results
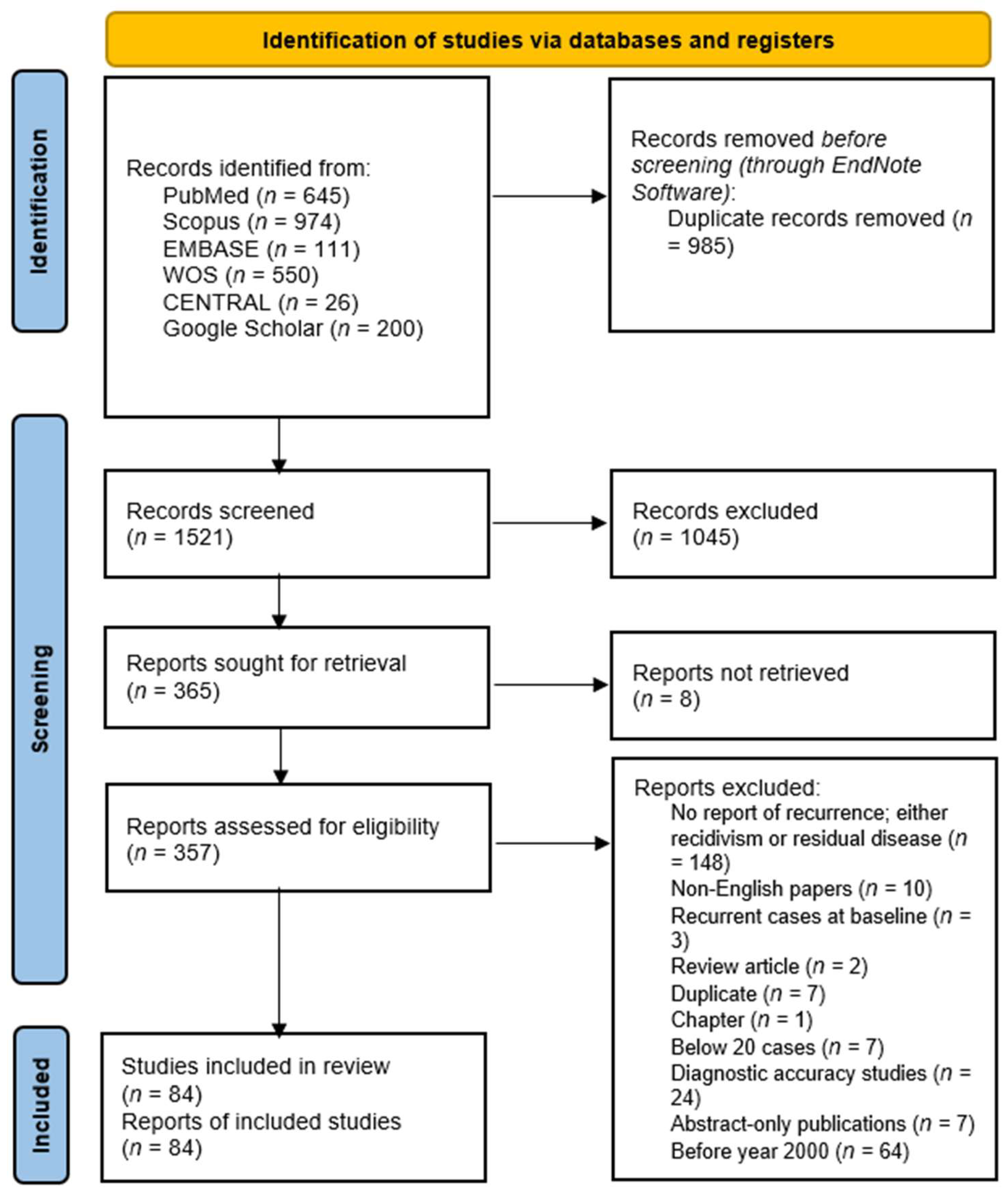
3.1. Literature Search Results
3.2. Characteristics of Included Studies
3.3. Methodological Quality of Included Studies
3.4. Incidence Rate of Cholesteatoma Recurrence
3.4.1. Country-Based Recurrence Rates
3.4.2. Age-, Gender-, and Laterality-Based Recurrence Rate
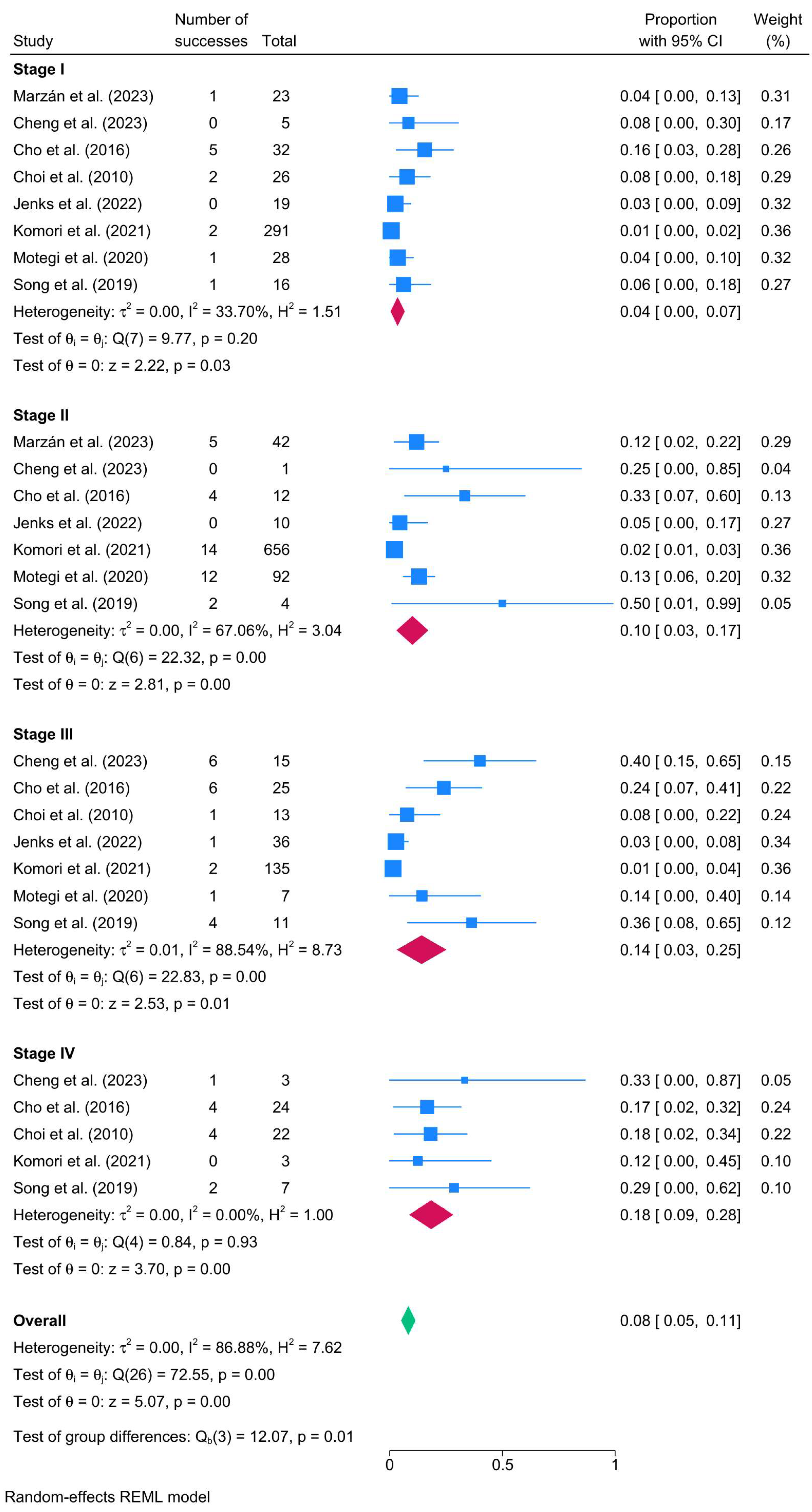
3.4.3. Recurrence Rate Based on Cholesteatoma-Related Characteristics
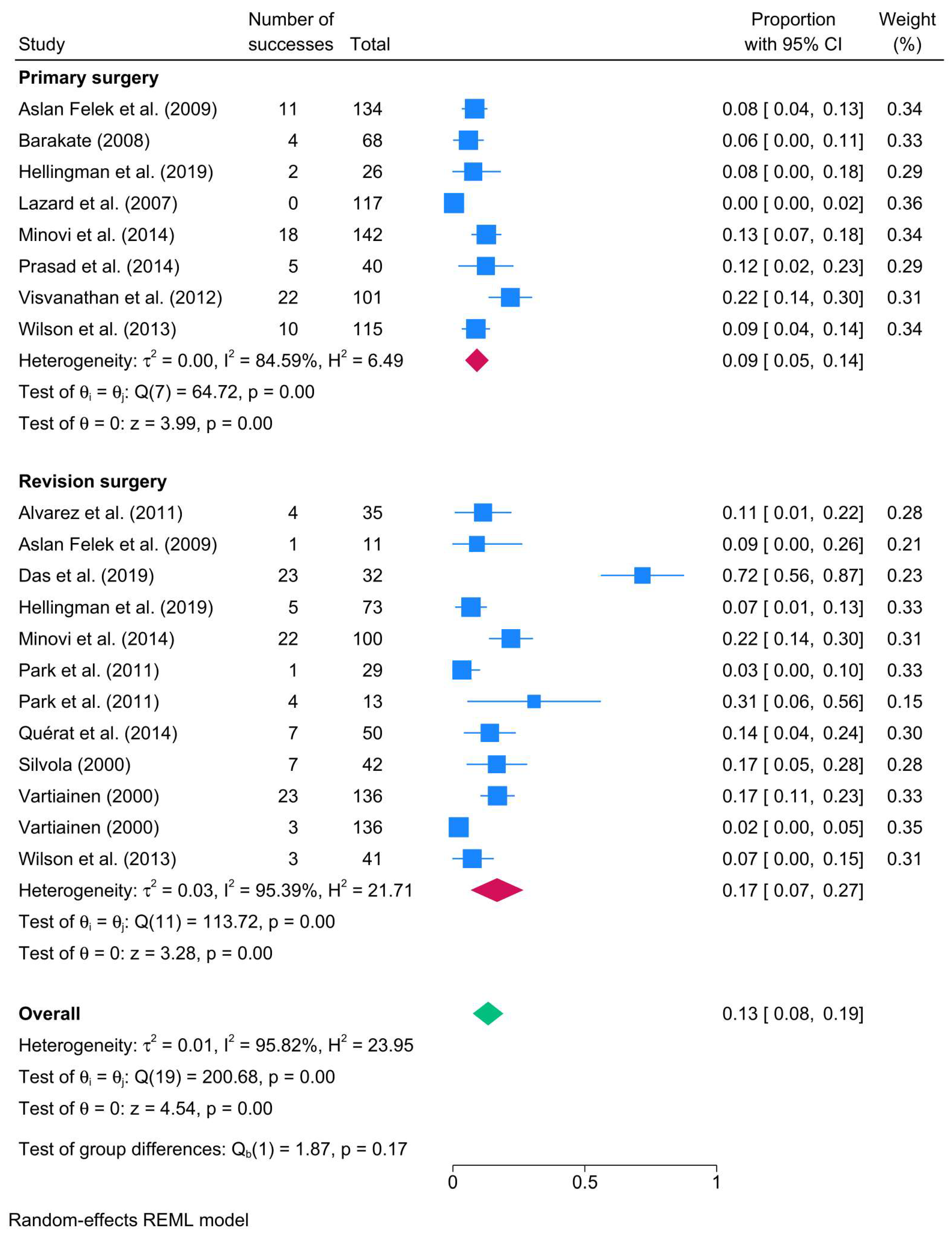
3.4.4. Surgical Intent-Based Recurrence Rates
3.4.5. Surgical Technique-Based Recurrence Rates
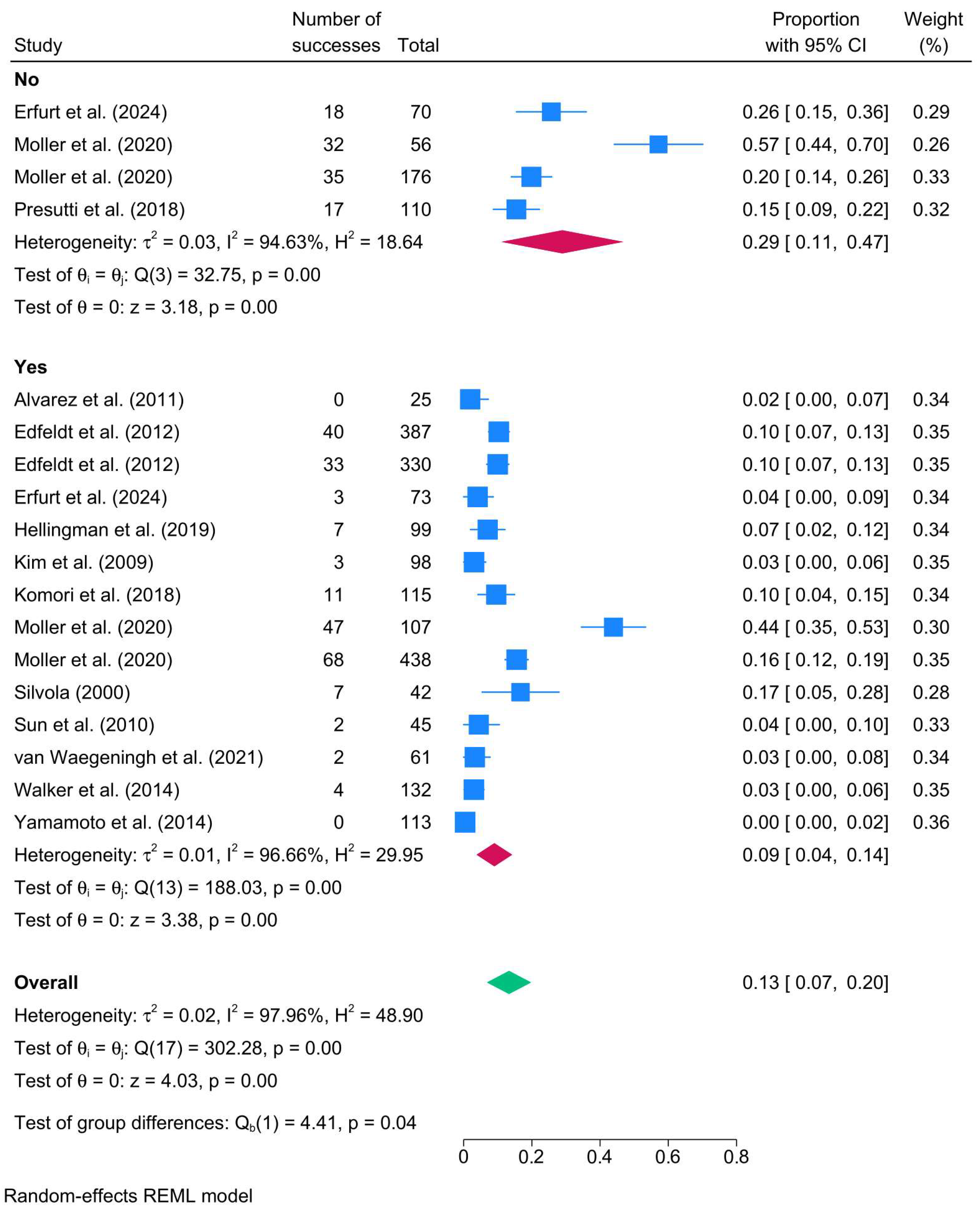
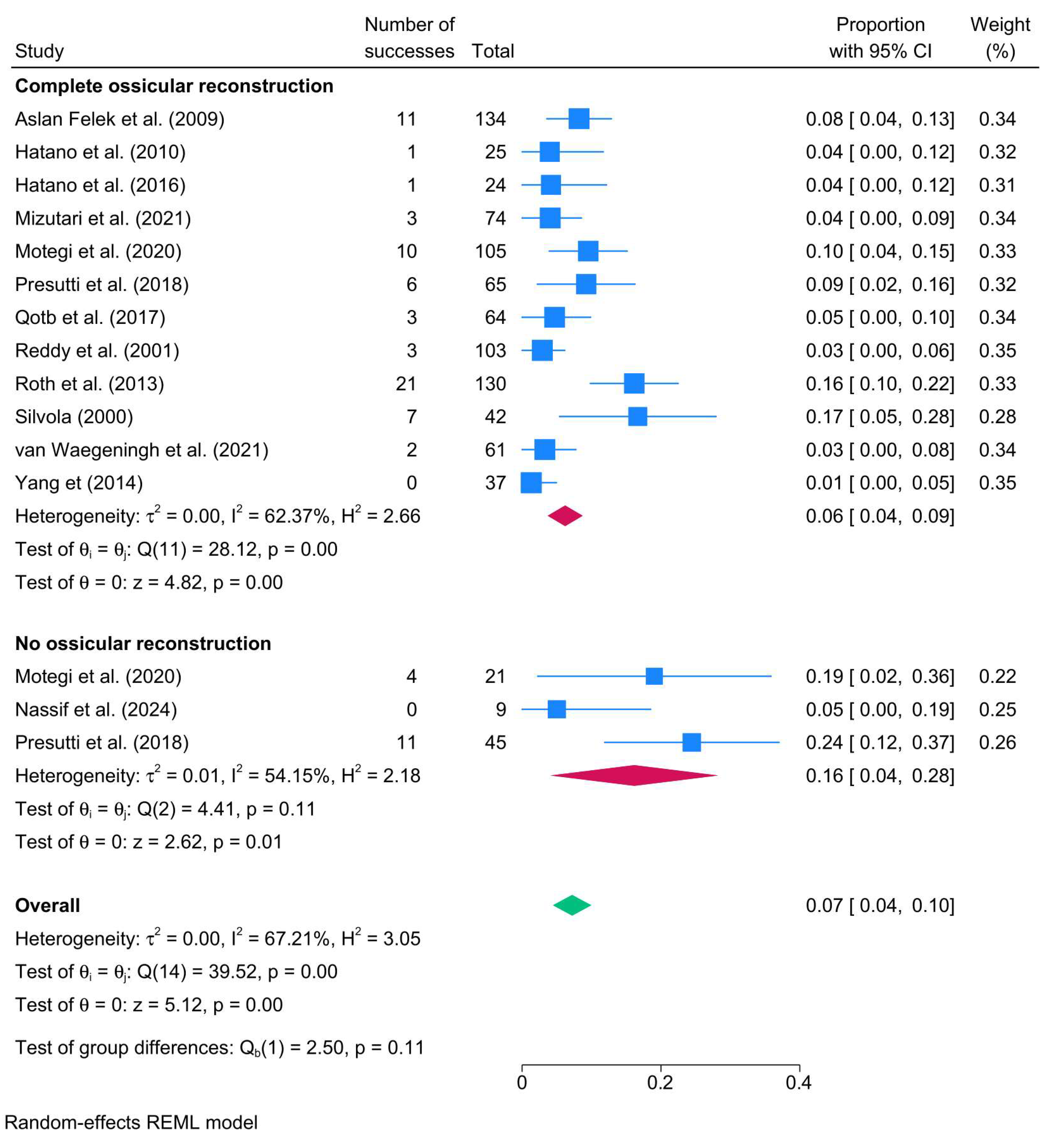
3.4.6. Mastoid Obliteration, Ossicular Reconstruction, and Perioperative Ventilation Tube-Based Rates
3.4.7. Follow-Up Based Recurrence Rate
3.5. Meta-Regression Findings
4. Discussion
4.1. Geographic Variation and Demographics
4.2. Disease Characteristics and Staging
4.3. Surgical Technique and Intent
4.4. Follow-Up Duration and Recurrence Trends
4.5. Role of Imaging in Recurrence Detection
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CENTRAL | Cochrane Central Register of Controlled Trials |
| CI | Confidence interval |
| CWDM | Canal wall down mastoidectomy |
| CWDT | Canal wall down tympanoplasty |
| CWDTM | Canal wall down tympanomastoidectomy |
| CWU | Canal wall up |
| CWUM | Canal wall up mastoidectomy |
| CWUT | Canal wall up tympanoplasty |
| CWUTM | Canal wall up tympanomastoidectomy |
| CWD | Canal wall down |
| DWI | Diffusion-weighted imaging |
| EAONO | European Academy of Otology and Neurotology |
| iCW | Intact Canal Wall |
| I2 | I-squared |
| JOS | Japan Ontological Society |
| MeSH | Medical Subject Headings |
| MRI | Magnetic Resonance Imaging |
| NOS | Newcastle Ottawa Scale |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| RCT | Randomized controlled trial |
| TEA | Trans-external auditory canal |
| USA | United States of America |
References
- Kuo, C.-L.; Shiao, A.-S.; Yung, M.; Sakagami, M.; Sudhoff, H.; Wang, C.-H.; Hsu, C.-H.; Lien, C.-F. Updates and knowledge gaps in cholesteatoma research. BioMed Res. Int. 2015, 2015, 854024. [Google Scholar] [CrossRef]
- Castle, J.T. Cholesteatoma pearls: Practical points and update. Head Neck Pathol. 2018, 12, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Aljehani, M.J.; Mukhtar, R.M.; AlFallaj, R.; Alhusayni, R.A.; Alraddadi, R.M.; Alhussaini, R. A spot review on relations between socioeconomic aspect and clinical recurrence of cholesteatoma. Eur. Arch. Oto-Rhino-Laryngol. 2024, 282, 895–905. [Google Scholar] [CrossRef] [PubMed]
- Molinari, G.; Reale, M.; Albera, A.; Russo, F.Y.; Di Lullo, A.M.; Gaffuri, M.; Ralli, M.; Turri-Zanoni, M.; Simon, F.; Anschuetz, L.; et al. Follow-up strategies in pediatric cholesteatoma: A systematic review. Eur. Arch. Oto-Rhino-Laryngol. 2025, 282, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Rayneau, P.; Aussedat, C.; Trinh, T.; Bobillier, C.; Lescanne, E.; Robier, A.; Bakhos, D. Influence of surgical technique on residual cholesteatoma location and prevalence. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2020, 137, 13–16. [Google Scholar] [CrossRef]
- Solis-Pazmino, P.; Siepmann, T.; Scheffler, P.; Ali, N.-E.-S.; Lincango-Naranjo, E.; Valdez, T.A.; Prokop, L.J.; Illigens, B.M.-W.; Ponce, O.J.; Ahmad, I.N. Canal wall up versus canal wall down mastoidectomy techniques in the pediatric population with cholesteatoma: A systematic review and meta-analysis of comparative studies. Int. J. Pediatr. Otorhinolaryngol. 2023, 173, 111658. [Google Scholar] [CrossRef]
- Salem, J.; Bakundukize, J.; Milinis, K.; Sharma, S. Mastoid obliteration versus canal wall down or canal wall up mastoidectomy for cholesteatoma: Systematic review and meta-analysis. Am. J. Otolaryngol. 2023, 44, 103751. [Google Scholar] [CrossRef]
- Amoodi, H.; Mofti, A.; Fatani, N.H.; Alhatem, H.; Zabidi, A.; Ibrahim, M.; Fatani, N.; Alhatem, H.F.; Ibrahim, M.A. Non-echo planar diffusion-weighted imaging in the detection of recurrent or residual cholesteatoma: A systematic review and meta-analysis of diagnostic studies. Cureus 2022, 14, e32127. [Google Scholar] [CrossRef]
- Bovi, C.; Luchena, A.; Bivona, R.; Borsetto, D.; Creber, N.; Danesi, G. Recurrence in cholesteatoma surgery: What have we learnt and where are we going? A narrative review. ACTA Otorhinolaryngol. Ital. 2023, 43, S48. [Google Scholar] [CrossRef]
- Tomlin, J.; Chang, D.; McCutcheon, B.; Harris, J. Surgical technique and recurrence in cholesteatoma: A meta-analysis. Audiol. Neurotol. 2013, 18, 135–142. [Google Scholar] [CrossRef]
- van der Toom, H.F.; van der Schroeff, M.P.; Pauw, R.J. Single-stage mastoid obliteration in cholesteatoma surgery and recurrent and residual disease rates: A systematic review. JAMA Otolaryngol.–Head Neck Surg. 2018, 144, 440–446. [Google Scholar] [CrossRef]
- Barbara, M.; Covelli, E.; Monini, S.; Bandiera, G.; Filippi, C.; Margani, V.; Volpini, L.; Salerno, G.; Romano, A.; Bozzao, A. Early non-EPI DW-MRI after cholesteatoma surgery. Ear Nose Throat J. 2024, 103, 435–441. [Google Scholar] [CrossRef]
- Romano, A.; Covelli, E.; Confaloni, V.; Rossi-Espagnet, M.C.; Butera, G.; Barbara, M.; Bozzao, A. Role of non-echo-planar diffusion-weighted images in the identification of recurrent cholesteatoma of the temporal bone. La Radiol. Medica 2020, 125, 75–79. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Muka, T.; Glisic, M.; Milic, J.; Verhoog, S.; Bohlius, J.; Bramer, W.; Chowdhury, R.; Franco, O.H. A 24-step guide on how to design, conduct, and successfully publish a systematic review and meta-analysis in medical research. Eur. J. Epidemiol. 2020, 35, 49–60. [Google Scholar] [CrossRef]
- Luchini, C.; Stubbs, B.; Solmi, M.; Veronese, N. Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World J. Meta-Anal. 2017, 5, 80–84. [Google Scholar] [CrossRef]
- Melsen, W.; Bootsma, M.; Rovers, M.; Bonten, M. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin. Microbiol. Infect. 2014, 20, 123–129. [Google Scholar] [CrossRef]
- Binti Abdullah, A.; Hashim, S.M.; Awang, M.A.; Saim, L. Outcome of canal wall down mastoidectomy: Experience in Sixty three cases. Med. J. Malays. 2013, 68, 217–221. [Google Scholar]
- Abraham, L.; Philip, A.; Lepcha, A.; Augustine, A.M.; Mathews, S.S.; Paul, R.R.; Mammen, M.D. A Comparative Study of Outcomes and Quality of Life in Canal Wall up Mastoidectomies and Canal Wall down Mastoidectomies. Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 600–607. [Google Scholar] [CrossRef] [PubMed]
- Adriaansens, C.; Bekkers, S.; Aarts, M.C.J. Determinants influencing cholesteatoma recurrence in daily practice: A retrospective analysis. J. Laryngol. Otol. 2022, 136, 119–124. [Google Scholar] [CrossRef]
- Alam, M.; Chandra, K. Ears with Cholesteatoma: Outcomes of Canal Wall Up and Down Tympano-Mastoidectomies-A Comparative Prospective Study. Indian J. Otolaryngol. Head Neck Surg. Off. Publ. Assoc. Otolaryngol. India 2022, 74, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Alicandri-Ciufelli, M.; Marchioni, D.; Kakehata, S.; Presutti, L.; Villari, D. Endoscopic Management of Attic Cholesteatoma Long-Term Results. Otolaryngol. Clin. N. Am. 2016, 49, 1265–1270. [Google Scholar] [CrossRef] [PubMed]
- Álvarez, F.L.; Gómez, J.R.; Bernardo, M.J.; Suárez, C. Management of petrous bone cholesteatoma: Open versus obliterative techniques. Eur. Arch. Oto-Rhino-Laryngol. Off. J. Eur. Fed. Oto-Rhino-Laryngol. Soc. (EUFOS) Affil. Ger. Soc. Oto-Rhino-Laryngol.-Head Neck Surg. 2011, 268, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Arias Marzán, F.; Pacheco Coronel, E.R.; Lemes Robayna, A.; Salom Lucena, M.C.; De Lucas Carmona, G.; Muñoz Cordero, M.G.; Macias Rodríguez, D.H.; Jimenez Sosa, A. Effectiveness and Safety of Attic Exposition–Antrum Exclusion versus Canal Wall-Up in Patients with Acquired Stage Ib and II Cholesteatoma Affecting the Attic and Tympanic Cavity. J. Clin. Med. 2023, 12, 49. [Google Scholar] [CrossRef]
- Aslan Felek, S.; Islam, A.; Celik, H.; Demirci, M.; Samim, E.; Kose, S.K. The functional and anatomical results of the canal wall down tympanoplasty in extensive cholesteatoma. Acta Oto-Laryngol. 2009, 129, 1388–1394. [Google Scholar] [CrossRef]
- Bakaj, T.; Zbrozkova, L.B.; Salzman, R.; Tedla, M.; Starek, I. Recidivous cholesteatoma: DWI MR after canal wall up and canal wall down mastoidectomy. Bratisl. Med. J. 2016, 117, 515–520. [Google Scholar] [CrossRef]
- Barakate, M.; Bottrill, I. Combined approach tympanoplasty for cholesteatoma: Impact of middle-ear endoscopy. J. Laryngol. Otol. 2008, 122, 120–124. [Google Scholar] [CrossRef]
- Chamoli, P.; Singh, C.V.; Radia, S.; Shah, A.K. Functional and Anatomical Outcome of Inside Out Technique For Cholesteatoma Surgery. Am. J. Otolaryngol. 2018, 39, 423–430. [Google Scholar] [CrossRef]
- Cheng, T.-C.; Ho, C.-Y.; Wu, J.-L. The role of planned two-stage surgery in the management of congenital cholesteatoma. Int. J. Pediatr. Otorhinolaryngol. 2023, 171, 111641. [Google Scholar] [CrossRef]
- Cho, H.S.; Kim, H.G.; Jung, D.J.; Jang, J.H.; Lee, S.H.; Lee, K.-Y. Clinical Aspects and Surgical Outcomes of Congenital Cholesteatoma in 93 Children: Increasing Trends of Congenital Cholesteatoma from 1997 through 2012. J. Audiol. Otol. 2016, 20, 168–173. [Google Scholar] [CrossRef]
- Choi, H.-G.; Park, K.H.; Park, S.N.; Jun, B.C.; Lee, D.H.; Park, Y.-S.; Chang, K.H.; Park, S.-Y.; Noh, H.; Yeo, S.W. Clinical experience of 71 cases of congenital middle ear cholesteatoma. Acta Otolaryngol. 2010, 130, 62–67. [Google Scholar] [CrossRef]
- Crowson, M.G.; Ramprasad, V.H.; Chapurin, N.; Cunningham, C.D., 3rd; Kaylie, D.M. Cost analysis and outcomes of a second-look tympanoplasty-mastoidectomy strategy for cholesteatoma. Laryngoscope 2016, 126, 2574–2579. [Google Scholar] [CrossRef] [PubMed]
- Danesi, G.; Cooper, T.; Panciera, D.T.; Manni, V.; Côté, D.W. Sanna classification and prognosis of cholesteatoma of the petrous part of the temporal bone: A retrospective series of 81 patients. Otol. Neurotol. 2016, 37, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Darrouzet, V.; Duclos, J.Y.; Portmann, D.; Bebear, J.P. Preference for the closed technique in the management of cholesteatoma of the middle ear in children: A retrospective study of 215 consecutive patients treated over 10 years. Am. J. Otol. 2000, 21, 474–481. [Google Scholar]
- Das, S.; Dutta, M.; Panja, T.; Sinha, R. Chronic Draining Ear and Cholesteatoma Recidivism: A Retrospection from Clinical, Imaging, and Surgical Perspectives. Turk. Arch. Otorhinolaryngol. 2019, 57, 133–139. [Google Scholar] [CrossRef] [PubMed]
- De Corso, E.; Marchese, M.R.; Scarano, E.; Paludetti, G. Aural acquired cholesteatoma in children: Surgical findings, recurrence and functional results. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 1269–1273. [Google Scholar] [CrossRef]
- DeRowe, A.; Stein, G.; Fishman, G.; Berco, E.; Avraham, S.; Landsberg, R.; Sadé, J. Long-term outcome of atticotomy for cholesteatoma in children. Otol. Neurotol. 2005, 26, 472–475. [Google Scholar] [CrossRef][Green Version]
- Diom, E.; Cisse, Z.; Tall, A.; Ndiaye, M.; Pegbessou, E.; Ndiaye, I.; Diallo, B.; Diouf, R.; Diop, E. Management of acquired cholesteatoma in children: A 15 year review in ENT service of CHNU de FANN Dakar. Int. J. Pediatr. Otorhinolaryngol. 2013, 77, 1998–2003. [Google Scholar] [CrossRef]
- Edfeldt, L.; Kinnefors, A.; Strömbäck, K.; Köbler, S.; Rask-Andersen, H. Surgical treatment of paediatric cholesteatoma: Long-term follow up in comparison with adults. Int. J. Pediatr. Otorhinolaryngol. 2012, 76, 1091–1097. [Google Scholar] [CrossRef]
- Edfeldt, L.; Strömbäck, K.; Kinnefors, A.; Rask-Andersen, H. Surgical treatment of adult cholesteatoma: Long-term follow-up using total reconstruction procedure without staging. Acta Otolaryngol. 2013, 133, 28–34. [Google Scholar] [CrossRef]
- Erfurt, C.; Westerhout, S.F.; Straatman, L.V.; Smit, A.L.; Stokroos, R.J.; Thomeer, H.G. Canal-wall up cholesteatoma surgery with mastoid obliteration leads to lower rates of disease recurrence without affecting hearing outcomes. Front. Surg. 2024, 11, 1381481. [Google Scholar] [CrossRef] [PubMed]
- Ferlito, S.; La Mantia, I.; Merlino, F.; Cocuzza, S.; Di Stadio, A.; Cammaroto, G.; Bartel, R.; Fadda, G.; Iannella, G.; Mat, Q.; et al. Long-Term Anatomical and Hearing Outcomes of Canal Wall down Tympanoplasty for Tympano-Mastoid Cholesteatoma: A 20-Year Retrospective Study. Life 2022, 12, 1745. [Google Scholar] [CrossRef] [PubMed]
- Glikson, E.; Feinmesser, G.; Sagiv, D.; Wolf, M.; Migirov, L.; Shapira, Y. Trans-canal endoscopic ear surgery and canal wall-up tympano-mastoidectomy for pediatric middle ear cholesteatoma. Eur. Arch. Oto-Rhino-Laryngol. Off. J. Eur. Fed. Oto-Rhino-Laryngol. Soc. (EUFOS) Affil. Ger. Soc. Oto-Rhino-Laryngol.-Head Neck Surg. 2019, 276, 3021–3026. [Google Scholar] [CrossRef] [PubMed]
- Govil, N.; Stapleton, A.L.; Georg, M.W.; Yellon, R.F. The role of tympanostomy tubes in surgery for acquired retraction pocket cholesteatoma. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 2015–2019. [Google Scholar] [CrossRef] [PubMed]
- Hatano, M.; Ito, M.; Yoshizaki, T. Retrograde mastoidectomy on demand with soft-wall reconstruction in pediatric cholesteatoma. Acta Otolaryngol. 2010, 130, 1113–1118. [Google Scholar] [CrossRef][Green Version]
- Hatano, M.; Ito, M.; Sugimoto, H.; Noda, M.; Hasegawa, H.; Yoshizaki, T. Soft-wall reconstruction of the canal wall with retrograde bone work for pediatric cholesteatoma: Long-term results. Int. J. Pediatr. Otorhinolaryngol. 2016, 91, 159–165. [Google Scholar] [CrossRef]
- Hellingman, C.A.; Geerse, S.; de Wolf, M.J.F.; Ebbens, F.A.; van Spronsen, E. Canal wall up surgery with mastoid and epitympanic obliteration in acquired cholesteatoma. Laryngoscope 2019, 129, 981–985. [Google Scholar] [CrossRef]
- Hou, Z.; Wang, F.; Zuo, W.; Liu, Y.; Wang, W.; Hou, K.; Jia, J.; Yang, S. Application of a novel transcanal keyhole technique in endoscopic cholesteatoma surgery. Acta Otolaryngol. 2021, 141, 328–333. [Google Scholar] [CrossRef]
- Hu, X.; Chen, M.; Dai, W.; Zhang, C.; Li, S. Efficiency of intraoperative endoscopic inspection in reducing residuals in canal-wall-up surgery for pediatric cholesteatoma involving the mastoid. Eur. Arch. Oto-Rhino-Laryngol. 2023, 280, 3593–3600. [Google Scholar] [CrossRef]
- Ikeda, M.; Yoshida, S.; Ikui, A.; Shigihara, S. Canal wall down tympanoplasty with canal reconstruction for middle-ear cholesteatoma: Post-operative hearing, cholesteatoma recurrence, and status of re-aeration of reconstructed middle-ear cavity. J. Laryngol. Otol. 2003, 117, 249–255. [Google Scholar] [CrossRef]
- Inanli, S.; Öztürk, Ö.; Batman, C.; Tutkun, A.; Üneri, C.; Sehitoglu, M.A. Clinical importance of supratubal recess in cholesteatoma surgery. Otol. Neurotol. 2001, 22, 754–760. [Google Scholar] [CrossRef]
- James, A.L. Cholesteatoma Severity Determines the Risk of Recurrent Paediatric Cholesteatoma More Than the Surgical Approach. J. Clin. Med. 2024, 13, 836. [Google Scholar] [CrossRef]
- Jenks, C.M.; Purcell, P.L.; Federici, G.; Villari, D.; Presutti, L.; James, A.L.; Hoff, S.R. Transcanal endoscopic ear surgery for congenital cholesteatoma: A multi-institutional series. Otolaryngol.-Head Neck Surg. 2022, 167, 537–544. [Google Scholar] [CrossRef]
- Killeen, D.E.; Tolisano, A.M.; Kou, Y.F.; Kutz, J.W.; Isaacson, B. Recidivism After Endoscopic Treatment of Cholesteatoma. Otol. Neurotol. Off. Publ. Am. Otol. Soc. Am. Neurotol. Soc. Eur. Acad. Otol. Neurotol. 2019, 40, 1313–1321. [Google Scholar] [CrossRef]
- Kim, J.H.; Choi, S.H.; Chung, J.W. Clinical results of atticoantrotomy with attic reconstruction or attic obliteration for patients with an attic cholesteatoma. Clin. Exp. Otorhinolaryngol. 2009, 2, 39–43. [Google Scholar] [CrossRef]
- Komori, M.; Yanagihara, N.; Hyodo, J.; Minoda, R.; Hinohira, Y. Five-year postoperative outcomes of modified staged canal wall up tympanoplasty for primary acquired cholesteatoma. Eur. Arch. Oto-Rhino-Laryngol. Off. J. Eur. Fed. Oto-Rhino-Laryngol. Soc. (EUFOS) Affil. Ger. Soc. Oto-Rhino-Laryngol.-Head Neck Surg. 2018, 275, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Komori, M.; Morita, Y.; Tono, T.; Matsuda, K.; Yamamoto, Y.; Sakagami, M.; Hato, N.; Kojima, H.; Takahashi, H. Nationwide survey of middle ear cholesteatoma surgery cases in Japan: Results from the Japan Otological society registry using the JOS staging and classification system. Auris Nasus Larynx 2021, 48, 555–564. [Google Scholar] [CrossRef]
- Kuo, C.L.; Shiao, A.S.; Liao, W.H.; Ho, C.Y.; Lien, C.F. Can long-term hearing preservation be expected in children following cholesteatoma surgery? Results from a 14-year-long study of atticotomy-limited mastoidectomy with cartilage reconstruction. Audiol. Neurotol. 2012, 17, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Lazard, D.S.; Roger, G.; Denoyelle, F.; Chauvin, P.; Garabédian, E.N. Congenital cholesteatoma: Risk factors for residual disease and retraction pockets—A report on 117 cases. Laryngoscope 2007, 117, 634–637. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Hong, S.M.; Kim, C.W.; Park, Y.H.; Baek, S.-H. Attic cholesteatoma with tiny retraction of pars flaccida. Auris Nasus Larynx 2015, 42, 107–112. [Google Scholar] [CrossRef]
- Manzoor, N.F.; Totten, D.J.; McLeod, M.E.; Sherry, A.D.; Perkins, E.L.; Haynes, D.S.; Rivas, A. Comparative Analysis of Recidivism After Endoscopic and Microscopic-Based Cholesteatoma Resection. Otol. Neurotol. 2022, 43, 466–471. [Google Scholar] [CrossRef]
- Marchioni, D.; Villari, D.; Mattioli, F.; Alicandri-Ciufelli, M.; Piccinini, A.; Presutti, L. Endoscopic Management of Attic Cholesteatoma A Single-Institution Experience. Otolaryngol. Clin. N. Am. 2013, 46, 201. [Google Scholar] [CrossRef]
- Marchioni, D.; Soloperto, D.; Rubini, A.; Villari, D.; Genovese, E.; Artioli, F.; Presutti, L. Endoscopic exclusive transcanal approach to the tympanic cavity cholesteatoma in pediatric patients: Our experience. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 316–322. [Google Scholar] [CrossRef]
- Minovi, A.; Venjacob, J.; Volkenstein, S.; Dornhoffer, J.; Dazert, S. Functional results after cholesteatoma surgery in an adult population using the retrograde mastoidectomy technique. Eur. Arch. Oto-Rhino-Laryngol. Off. J. Eur. Fed. Oto-Rhino-Laryngol. Soc. (EUFOS) Affil. Ger. Soc. Oto-Rhino-Laryngol.-Head Neck Surg. 2014, 271, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Mishiro, Y.; Sakagami, M.; Kitahara, T.; Kondoh, K.; Okumura, S.I. The investigation of the recurrence rate of cholesteatoma using Kaplan-Meier survival analysis. Otol. Neurotol. Off. Publ. Am. Otol. Soc. Am. Neurotol. Soc. Eur. Acad. Otol. Neurotol. 2008, 29, 803–806. [Google Scholar] [CrossRef] [PubMed]
- Mizutari, K.; Takihata, S.; Kimura, E.; Inuzuka, E.; Shiotani, A. Patency of Anterior Epitympanic Space and Surgical Outcomes After Endoscopic Ear Surgery for the Attic Cholesteatoma. Otol. Neurotol. Off. Publ. Am. Otol. Soc. Am. Neurotol. Soc. Eur. Acad. Otol. Neurotol. 2021, 42, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Møller, P.R.; Pedersen, C.N.; Grosfjeld, L.R.; Faber, C.E.; Djurhuus, B.D. Recurrence of cholesteatoma-a retrospective study including 1,006 patients for more than 33 years. Int. Arch. Otorhinolaryngol. 2020, 24, e18–e23. [Google Scholar] [CrossRef]
- Morita, Y.; Yamamoto, Y.; Oshima, S.; Takahashi, K.; Takahashi, S. Acquired cholesteatoma in children: Clinical features and surgical outcome. Auris Nasus Larynx 2014, 41, 417–421. [Google Scholar] [CrossRef]
- Morita, Y.; Takahashi, K.; Izumi, S.; Kubota, Y.; Ohshima, S.; Yamamoto, Y.; Takahashi, S.; Horii, A. Risk factors of recurrence in pediatric congenital cholesteatoma. Otol. Neurotol. 2017, 38, 1463–1469. [Google Scholar] [CrossRef]
- Motegi, M.; Yamamoto, Y.; Ouchi, K.; Akutsu, T.; Tada, T.; Kurihara, S.; Takahashi, M.; Sampei, S.; Sano, H.; Morino, T.; et al. The impact of middle ear aeration on surgical outcome after intact canal wall tympanoplasty for cholesteatoma. Auris Nasus Larynx 2020, 47, 965–975. [Google Scholar] [CrossRef]
- Myers, E.N.; Stangerup, S.E.; Drozdziewicz, D.; Tos, M.; Hougaard-Jensen, A. Recurrence of attic cholesteatoma: Different methods of estimating recurrence rates. Otolaryngol.-Head Neck Surg. 2000, 123, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Nassif, N.; Redaelli de Zinis, L.O. The Role of Endoscopic Assistance in Surgery for Pediatric Cholesteatoma in Reducing Residual and Recurrent Disease. Children 2024, 11, 369. [Google Scholar] [CrossRef]
- Neudert, M.; Lailach, S.; Lasurashvili, N.; Kemper, M.; Beleites, T.; Zahnert, T. Cholesteatoma recidivism: Comparison of three different surgical techniques. Otol. Neurotol. Off. Publ. Am. Otol. Soc. Am. Neurotol. Soc. Eur. Acad. Otol. Neurotol. 2014, 35, 1801–1808. [Google Scholar] [CrossRef] [PubMed]
- Pareschi, R.; Lepera, D.; Nucci, R. Canal wall down approach for tympano-mastoid cholesteatoma: Long-term results and prognostic factors. Acta Otorhinolaryngol. Ital. 2019, 39, 122. [Google Scholar] [CrossRef] [PubMed]
- Park, K.H.; Park, S.N.; Chang, K.H.; Jung, M.K.; Yeo, S.W. Congenital middle ear cholesteatoma in children; retrospective review of 35 cases. J. Korean Med. Sci. 2009, 24, 126. [Google Scholar] [CrossRef]
- Park, K.T.; Song, J.J.; Moon, S.J.; Lee, J.H.; Chang, S.O.; Oh, S.H. Choice of approach for revision surgery in cases with recurring chronic otitis media with cholesteatoma after the canal wall up procedure. Auris Nasus Larynx 2011, 38, 190–195. [Google Scholar] [CrossRef]
- Piras, G.; Sykopetrites, V.; Taibah, A.; Russo, A.; Caruso, A.; Grinblat, G.; Sanna, M. Long term outcomes of canal wall up and canal wall down tympanomastoidectomies in pediatric cholesteatoma. Int. J. Pediatr. Otorhinolaryngol. 2021, 150, 110887. [Google Scholar] [CrossRef]
- Prasad, S.C.; La Melia, C.; Medina, M.; Vincenti, V.; Bacciu, A.; Bacciu, S.; Pasanisi, E. Long-term surgical and functional outcomes of the intact canal wall technique for middle ear cholesteatoma in the paediatric population. Acta Otorhinolaryngol. Ital. Organo Uff. Della Soc. Ital. Di Otorinolaringol. E Chir. Cervico-Facciale 2014, 34, 354–361. [Google Scholar]
- Presutti, L.; Anschuetz, L.; Rubini, A.; Ruberto, M.; Alicandri-Ciufelli, M.; Dematte, M.; Caversaccio, M.; Marchioni, D. The impact of the transcanal endoscopic approach and mastoid preservation on recurrence of primary acquired attic cholesteatoma. Otol. Neurotol. 2018, 39, 445–450. [Google Scholar] [CrossRef]
- Qotb, M.; Fawzy, T.; Ragab, W. Single Stage Canal Wall Down Mastoidectomy with Reconstruction of the Canal Wall: 5 Years’ Experience in Fayoum Province, Egypt. J. Int. Adv. Otol. 2017, 13, 181–185. [Google Scholar] [CrossRef]
- Quérat, C.; Martin, C.; Prades, J.-M.; Richard, C. Canal wall up tympanoplasty for cholesteatoma with intact stapes. Comparison of hearing results between cartilage and PORP on stapes and impact of malleus removal and total reinforcement of the tympanic membrane by cartilage. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2014, 131, 211–216. [Google Scholar] [CrossRef]
- Reddy, T.N.; Shetty, A.; Dutt, S.N.; Maini, S. Transcanal atticoaditotomy and transcortical mastoidectomy for cholesteatoma: The Farrior-Olaizola technique revisited. Ann. Otol. Rhinol. Laryngol. 2001, 110, 739–745. [Google Scholar] [CrossRef]
- Roth, T.N.; Ziglinas, P.; Haeusler, R.; Caversaccio, M.D. Cholesteatoma surgery in children: Long-term results of the inside-out technique. Int. J. Pediatr. Otorhinolaryngol. 2013, 77, 843–846. [Google Scholar] [CrossRef]
- Roux, A.; Bakhos, D.; Lescanne, E.; Cottier, J.-P.; Robier, A. Canal wall reconstruction in cholesteatoma surgeries: Rate of residual. Eur. Arch. Oto-Rhino-Laryngol. Off. J. Eur. Fed. Oto-Rhino-Laryngol. Soc. (EUFOS) Affil. Ger. Soc. Oto-Rhino-Laryngol.-Head Neck Surg. 2015, 272, 2791–2797. [Google Scholar] [CrossRef] [PubMed]
- Schraff, S.A.; Strasnick, B. Pediatric cholesteatoma: A retrospective review. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 385–393. [Google Scholar] [CrossRef]
- Shin, C.H.; Kang, W.S.; Park, H.J.; Chung, J.W.; Ahn, J.H. Is there a clinical difference in paediatric congenital cholesteatoma according to age? J. Laryngol. Otol. 2023, 137, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Silvola, J.; Palva, T. One-stage revision surgery for pediatric cholesteatoma: Long-term results and comparison with primary surgery. Int. J. Pediatr. Otorhinolaryngol. 2000, 56, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Song, I.S.; Han, W.G.; Lim, K.H.; Nam, K.J.; Yoo, M.H.; Rah, Y.C.; Choi, J. Clinical characteristics and treatment outcomes of congenital cholesteatoma. J. Int. Adv. Otol. 2019, 15, 386. [Google Scholar] [CrossRef]
- Sun, J.; Sun, J.; Hu, Y.; Lv, Q.; Wang, Y.; Li, X.; Xu, W.; Wang, S.; Mei, Z.; Wan, G. Canal wall-down mastoidectomy with mastoid obliteration for pediatric cholesteatoma. Acta Oto-Laryngol. 2010, 130, 259–262. [Google Scholar] [CrossRef]
- Trinidade, A.; Skingsley, A.; Yung, M.W. Pediatric cholesteatoma surgery using a single-staged canal wall down approach: Results of a 5-year longitudinal study. Otol. Neurotol. Off. Publ. Am. Otol. Soc. Am. Neurotol. Soc. Eur. Acad. Otol. Neurotol. 2015, 36, 82–85. [Google Scholar] [CrossRef]
- van Dinther, J.J.; Vercruysse, J.P.; Camp, S.; De Foer, B.; Casselman, J.; Somers, T.; Zarowski, A.; Cremers, C.W.; Offeciers, E. The Bony Obliteration Tympanoplasty in Pediatric Cholesteatoma: Long-term Safety and Hygienic Results. Otol. Neurotol. 2015, 36, 1504–1509. [Google Scholar] [CrossRef]
- van Waegeningh, H.F.; van Dinther, J.J.; Vanspauwen, R.; Zarowski, A.; Offeciers, E. The bony obliteration tympanoplasty in cholesteatoma: Safety, hygiene and hearing outcome: Allograft versus autograft tympanic membrane reconstruction. Eur. Arch. Oto-Rhino-Laryngol. Off. J. Eur. Fed. Oto-Rhino-Laryngol. Soc. (EUFOS) Affil. Ger. Soc. Oto-Rhino-Laryngol.-Head Neck Surg. 2021, 278, 1805–1813. [Google Scholar] [CrossRef]
- Vartiainen, E. Ten-year results of canal wall down mastoidectomy for acquired cholesteatoma. Auris Nasus Larynx 2000, 27, 227–229. [Google Scholar] [CrossRef]
- Visvanathan, V.; Kubba, H.; Morrissey, M.S.C. Cholesteatoma surgery in children: 10-year retrospective review. J. Laryngol. Otol. 2012, 126, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Walker, P.C.; Mowry, S.E.; Hansen, M.R.; Gantz, B.J. Long-term results of canal wall reconstruction tympanomastoidectomy. Otol. Neurotol. Off. Publ. Am. Otol. Soc. Am. Neurotol. Soc. Eur. Acad. Otol. Neurotol. 2014, 35, e24–e30. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.F.; Hoggan, R.N.; Shelton, C. Tympanoplasty with intact canal wall mastoidectomy for cholesteatoma: Long-term surgical outcomes. Otolaryngol.--Head Neck Surg. Off. J. Am. Acad. Otolaryngol.-Head Neck Surgery 2013, 149, 292–295. [Google Scholar] [CrossRef] [PubMed]
- Wu, N.; Zuo, W.; Wang, F.; Hou, K.; Yang, S.; Hou, Z. Scutum reconstruction technique and classification in endoscopic middle ear cholesteatoma surgery. Acta Oto-Laryngol. 2020, 140, 904–908. [Google Scholar] [CrossRef]
- Yamamoto, Y.; Takahashi, K.; Morita, Y.; Ohshima, S.; Takahashi, S. Long-term follow-up results of canal wall down tympanoplasty with mastoid obliteration using the bone pate plate for canal wall reconstruction in cholesteatoma surgery. Otol. Neurotol. Off. Publ. Am. Otol. Soc. Am. Neurotol. Soc. Eur. Acad. Otol. Neurotol. 2014, 35, 961–965. [Google Scholar] [CrossRef]
- Yang, W.-Y.; Watson, C. Recurrence rate of cholesteatoma with autoclaved incus autograft. Otol. Neurotol. Off. Publ. Am. Otol. Soc. Am. Neurotol. Soc. Eur. Acad. Otol. Neurotol. 2014, 35, e307–e309. [Google Scholar] [CrossRef]
- Yung, M.; Jacobsen, N.L.; Vowler, S.L. A 5-year observational study of the outcome in pediatric cholesteatoma surgery. Otol. Neurotol. Off. Publ. Am. Otol. Soc. Am. Neurotol. Soc. Eur. Acad. Otol. Neurotol. 2007, 28, 1038–1040. [Google Scholar] [CrossRef]
- Zanetti, D.; Di Lella, F.; Negri, M.; Vincenti, V. Surgical management of middle ear cholesteatoma in children with Turner syndrome: A multicenter experience. Acta Bio-Medica Atenei Parm. 2018, 89, 382–388. [Google Scholar] [CrossRef]
- Shewel, Y.; Tawfik, S.A.S.; Aaref, A.A.; Saleh, N. Recidivism of childhood cholesteatoma and surgical techniques: A meta-analysis study. Egypt. J. Otolaryngol. 2020, 36, 38. [Google Scholar] [CrossRef]
- Körmendy, K.B.; Shenker-Horvath, K.; Shulze Wenning, A.; Fehérvári, P.; Harnos, A.; Hegyi, P.; Molnár, Z.; Illes, K.; Horvath, T. Predicting residual cholesteatoma with the Potsic staging system still lacks evidence: A systematic review and meta-analysis. Eur. Arch. Oto-Rhino-Laryngol. 2024, 281, 3557–3568. [Google Scholar] [CrossRef]
- Al Saeed, A.A.; AlShabib, N.S.; Al Taisan, A.A.; Kreary, Y.A. Association of retinal vascular manifestation and obstructive sleep apnea (OSA): A narrative review. Clin. Ophthalmol. 2021, 15, 3315–3320. [Google Scholar] [CrossRef]
- Xun, M.; Liu, X.; Sha, Y.; Zhang, X.; Liu, J.P. The diagnostic utility of diffusion-weighted magnetic resonance imaging and high-resolution computed tomography for cholesteatoma: A meta-analysis. Laryngoscope Investig. Otolaryngol. 2023, 8, 627–635. [Google Scholar] [CrossRef]
- Muzaffar, J.; Metcalfe, C.; Colley, S.; Coulson, C. Diffusion-weighted magnetic resonance imaging for residual and recurrent cholesteatoma: A systematic review and meta-analysis. Clin. Otolaryngol. 2017, 42, 536–543. [Google Scholar] [CrossRef] [PubMed]
| Number of Studies | Pooled Rate (%) | 95% CI | I2 (%) | p-Value | |
|---|---|---|---|---|---|
| Country | 0.001 | ||||
| Belgium | 1 | 3% | 0–8% | N/A | |
| China | 4 | 3% | 1–6% | 0.05% | |
| Czech Republic | 1 | 7% | 0–19% | N/A | |
| Denmark | 3 | 24% | 0–48% | 98.91% | |
| Egypt | 1 | 5% | 0–10% | N/A | |
| England | 1 | 3% | 0–6% | N/A | |
| Finland | 2 | 17% | 11–22% | 0.01% | |
| France | 4 | 6% | 0–12% | 88.14% | |
| Germany | 2 | 12% | 9–15% | 0.12% | |
| India | 3 | 29% | 0–70% | 98.61% | |
| Israel | 2 | 24% | 15–34% | 10.88% | |
| Italy | 12 | 12% | 7–17% | 96.44% | |
| Japan | 12 | 7% | 4–10% | 95.16% | |
| Korea | 8 | 8% | 3–13% | 79.81% | |
| Malaysia | 1 | 4% | 0–10% | N/A | |
| Senegal | 1 | 14% | 5–22% | N/A | |
| Spain | 2 | 10% | 4–16% | 0% | |
| Sweden | 2 | 10% | 8–12% | 0.02% | |
| Switzerland | 1 | 16% | 10–22% | N/A | |
| Taiwan | 2 | 4% | 0–9% | 29.49% | |
| The Netherlands | 4 | 13% | 3–23% | 90.51% | |
| Turkey | 2 | 12% | 5–20% | 85.20% | |
| United Kingdom | 5 | 7% | 0–14% | 91.51% | |
| United States of America | 8 | 6% | 3–9% | 75.37% | |
| Age | 0.001 | ||||
| Adults | 25 | 10% | 6–14% | 97.80% | |
| Children | 36 | 13% | 9–16% | 95.33% | |
| Adults and Children | 15 | 11% | 4–18% | 97.19% | |
| Gender | 0.96 | ||||
| Male | 3 | 17% | 8–27% | 76.09% | |
| Female | 3 | 18% | 10–25% | 24.20% | |
| Laterality | 0.79 | ||||
| Right | 3 | 15% | 6–25% | 31.87% | |
| Left | 3 | 18% | 3–32% | 77.29% | |
| Cholesteatoma Type | 0.2 | ||||
| Acquired | 14 | 12% | 8–16% | 80.35% | |
| Congenital | 13 | 7% | 3–11% | 92.36% | |
| Recurrent Cholesteatoma Definition | 0.62 | ||||
| Defined | 31 | 11% | 7–14% | 96.61% | |
| Not Defined | 53 | 10% | 7–12% | 97.64% | |
| Stage of Cholesteatoma | 0.01 | ||||
| Stage I | 8 | 4% | 0–7% | 33.70% | |
| Stage II | 7 | 10% | 3–17% | 67.06% | |
| Stage III | 7 | 14% | 3–25% | 88.54% | |
| Stage IV | 5 | 18% | 9–28% | 0% | |
| Cholesteatoma Location | 0.001 | ||||
| Attic | 11 | 10% | 4–15% | 91.06% | |
| Aural | 2 | 20% | 12–28% | 86.74% | |
| Mastoid | 3 | 16% | 3–30% | 72.51% | |
| Middle Ear (not classified) | 7 | 16% | 9–23% | 86.57% | |
| Pars Flaccida | 3 | 12% | 0–25% | 95.37% | |
| Pars Tensa | 3 | 8% | 2–14% | 85.56% | |
| Petrous bone | 2 | 19% | 5–33% | 74.96% | |
| Pars Tensa + Flaccida | 3 | 15% | 2–28% | 88.06% | |
| Tympano-mastoid | 2 | 1% | 0–2% | 14.48% | |
| Surgical Intent | 0.17 | ||||
| Primary Surgery | 8 | 9% | 5–14% | 84.59% | |
| Revision Surgery | 12 | 17% | 7–27% | 95.39% | |
| Staged Surgery | 0.87 | ||||
| Single-stage surgery | 11 | 8% | 4–13% | 91.41% | |
| Staged surgery (2 stages or more) | 5 | 9% | 6–12% | 0.05% | |
| Surgery Type | 0.001 | ||||
| Atticotomy-based procedure | 4 | 7% | 0–15% | 91.33% | |
| CWD Procedure | 29 | 7% | 4–9% | 94.43% | |
| CWDM | 8 | 6% | 2–10% | 72.16% | |
| CWDT | 7 | 7% | 0–13% | 98.23% | |
| CWDTM | 3 | 1% | 0–2% | 0.03% | |
| CWU Procedure | 27 | 16% | 11–21% | 95.78% | |
| CWUM | 4 | 9% | 1–16% | 40.40% | |
| CWUT | 2 | 19% | 10–27% | 47.90% | |
| CWUTM | 9 | 12% | 5–19% | 92.45% | |
| Combined approach tympanoplasty | 2 | 17% | 0–39% | 92.39% | |
| Endoscopic Approach | 14 | 8% | 5–11% | 79.81% | |
| TEA | 10 | 8% | 4–11% | 83.60% | |
| Mastoid-sparing surgery | 4 | 11% | 3–19% | 92.32% | |
| Microscopic approach | 2 | 11% | 0–26% | 80.67% | |
| Retrograde mastoidectomy | 3 | 8% | 1–14% | 56.35% | |
| iCW Procedure | 8 | 12% | 7–17% | 85.39% | |
| Second-look Surgery | 0.42 | ||||
| Planned 2nd look | 4 | 13% | 6–19% | 60.80% | |
| Not planned | 5 | 10% | 7–12% | 32.64% | |
| Mastoid Obliteration | 0.04 | ||||
| Yes | 14 | 9% | 4–14% | 96.66% | |
| No | 4 | 29% | 11–47% | 94.63% | |
| Ossicular Reconstruction (any) | 0.11 | ||||
| Complete reconstruction | 12 | 6% | 4–9% | 62.37% | |
| No reconstruction | 3 | 16% | 4–28% | 54.15% | |
| Perioperative Ventilation Tube | 0.64 | ||||
| Yes | 2 | 18% | 6–30% | 0% | |
| No | 2 | 26% | 0–59% | 92.79% | |
| Follow-up | 0.001 | ||||
| 12 months | 9 | 7% | 3–12% | 96.76% | |
| 24 months | 16 | 9% | 6–13% | 95.76% | |
| 30 months | 3 | 7% | 0–15% | 77.74% | |
| 36 months | 16 | 16% | 11–21% | 91.06% | |
| 48 months | 13 | 15% | 9–21% | 94.97% | |
| 55 months | 2 | 9% | 0–21% | 77.34% | |
| 60 months | 23 | 18% | 12–24% | 98.14% | |
| 72 months | 6 | 10% | 6–14% | 81.35% | |
| 84 months | 3 | 14% | 2–26% | 82.94% | |
| 96 months | 3 | 15% | 2–29% | 87.86% | |
| 120 months | 11 | 17% | 8–27% | 98.85% | |
| 132 months | 2 | 14% | 8–20% | 57.90% | |
| 144 months | 2 | 20% | 10–31% | 73.26% | |
| 180 months | 2 | 39% | 21–56% | 96.58% | |
| Unadjusted Model | Adjusted Model | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | Z | p-Value | Low CI | High CI | Coefficient | SE | Z | p-Value | Low CI | High CI | |
| Revision surgery (per %) | 0.0032 | 0.0004 | 7.49 | <0.001 | 0.0024 | 0.0040 | 0.0016 | 0.0023 | 0.7 | 0.4850 | −0.0029 | 0.0061 |
| Planned second look (per %) | 0.0010 | 0.0003 | 2.89 | 0.0040 | 0.0003 | 0.0016 | −0.0145 | 0.0067 | −2.16 | 0.0300 | −0.0276 | −0.0014 |
| Staged surgery (per %) | 0.0011 | 0.0004 | 3.06 | 0.0020 | 0.0004 | 0.0018 | 0.0153 | 0.0070 | 2.18 | 0.0290 | 0.0015 | 0.0291 |
| Age (per year) | 0.0028 | 0.0005 | 5.99 | <0.001 | 0.0019 | 0.0037 | 0.0036 | 0.0013 | 2.76 | 0.0060 | 0.0010 | 0.0062 |
| Recurrence defined (vs. not defined) | 0.1100 | 0.0222 | 4.96 | <0.001 | 0.0666 | 0.1534 | −0.1215 | 0.0876 | −1.39 | 0.1650 | −0.2933 | 0.0502 |
| Follow-up (per month) | 0.0011 | 0.0001 | 7.68 | <0.001 | 0.0008 | 0.0014 | 0.0004 | 0.0005 | 0.81 | 0.4170 | −0.0006 | 0.0014 |
| Ossicular reconstruction (per %) | 0.0012 | 0.0004 | 3.08 | 0.0020 | 0.0004 | 0.0019 | Omitted (due to collinearity) | |||||
| Ossicular erosion (per %) | 0.0021 | 0.0004 | 5.82 | <0.001 | 0.0014 | 0.0028 | Omitted (due to collinearity) | |||||
| Mastoid obliteration (per %) | 0.0711 | 0.0191 | 3.72 | <0.001 | 0.0336 | 0.1085 | Omitted (due to collinearity) | |||||
| Acquired Cholesteatoma (vs. Congenital) | 0.1229 | 0.0249 | 4.94 | <0.001 | 0.0741 | 0.1717 | Omitted (no observations) | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Massoud, S.; Farhat, R.; Abd Elhadi, U.; Awawde, R.; Merchavy, S.; Safia, A. Incidence Rate and Determinants of Recurrent Cholesteatoma Following Surgical Management: A Systematic Review, Subgroup, and Meta-Regression Analysis. Biomedicines 2025, 13, 2506. https://doi.org/10.3390/biomedicines13102506
Massoud S, Farhat R, Abd Elhadi U, Awawde R, Merchavy S, Safia A. Incidence Rate and Determinants of Recurrent Cholesteatoma Following Surgical Management: A Systematic Review, Subgroup, and Meta-Regression Analysis. Biomedicines. 2025; 13(10):2506. https://doi.org/10.3390/biomedicines13102506
Chicago/Turabian StyleMassoud, Saqr, Raed Farhat, Uday Abd Elhadi, Rifat Awawde, Shlomo Merchavy, and Alaa Safia. 2025. "Incidence Rate and Determinants of Recurrent Cholesteatoma Following Surgical Management: A Systematic Review, Subgroup, and Meta-Regression Analysis" Biomedicines 13, no. 10: 2506. https://doi.org/10.3390/biomedicines13102506
APA StyleMassoud, S., Farhat, R., Abd Elhadi, U., Awawde, R., Merchavy, S., & Safia, A. (2025). Incidence Rate and Determinants of Recurrent Cholesteatoma Following Surgical Management: A Systematic Review, Subgroup, and Meta-Regression Analysis. Biomedicines, 13(10), 2506. https://doi.org/10.3390/biomedicines13102506






