The Role of the Estimated Plasma Volume Variation in Assessing Decongestion in Patients with Acute Decompensated Heart Failure
Abstract
1. Introduction
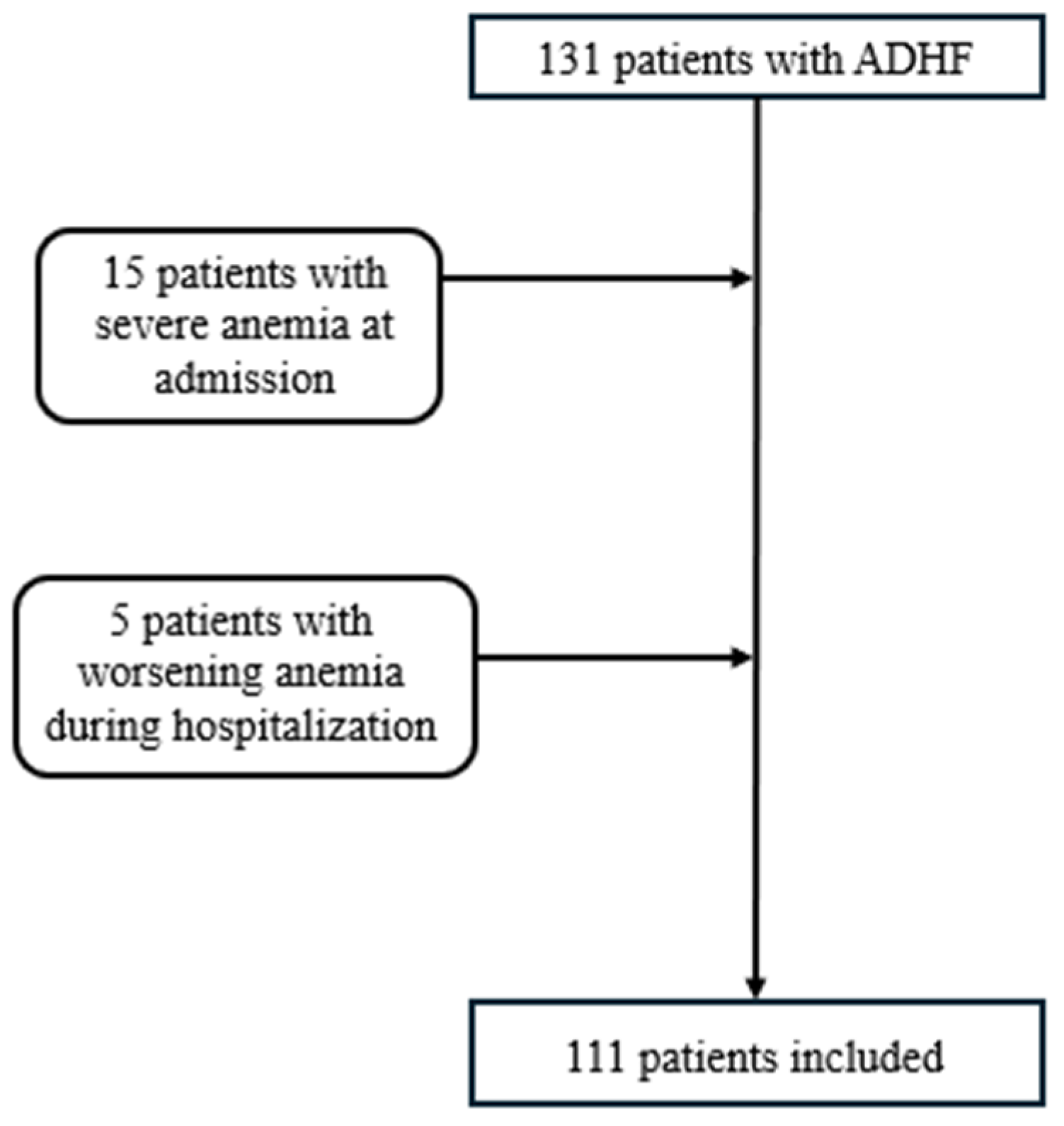
2. Materials and Methods
- Patients with episodes of decompensated HF, regardless of left ventricular ejection fraction (LVEF).
- Severe anemia (Hb < 8 g/dL);
- Worsening anemia, defined as a decrease in Hb > 2 g/dL during hospitalization;
- Patients having received a blood transfusion, specifically those with an increase in Hb of more than 3 g/dL from admission to discharge;
- Hyponatremia requiring correction;
- Advanced malignancies with a life expectancy of less than 1 year;
- Septic shock;
- Patients with stage V chronic kidney disease (eGFR < 15 mL/min/1.73 m2) or hemodialysis;
- Any type of surgical intervention;
- Pregnant females.
2.1. Clinical and Laboratory Evaluation
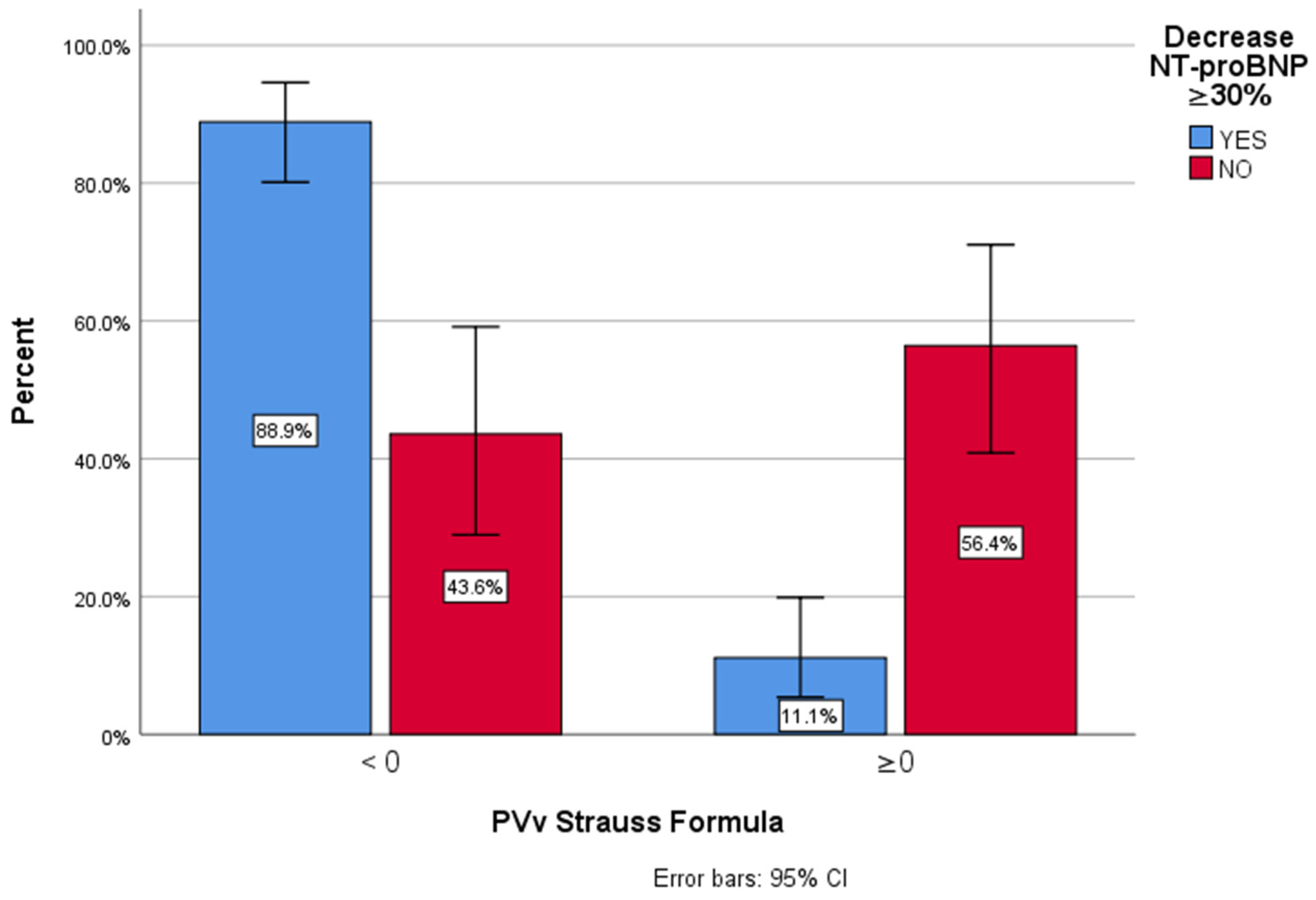
- Group 1 (<0%)—hemoconcentration;
- Group 2 (≥0%)—hemodilution.
2.2. Ultrasound
2.3. Statistical Analysis
3. Results
3.1. Clinical Congestion Parameters
3.2. Echocardiography and Lung Ultrasound
3.3. Biochemical Parameters and Diuretic Treatment
3.4. ∆ePVS and Renal Function
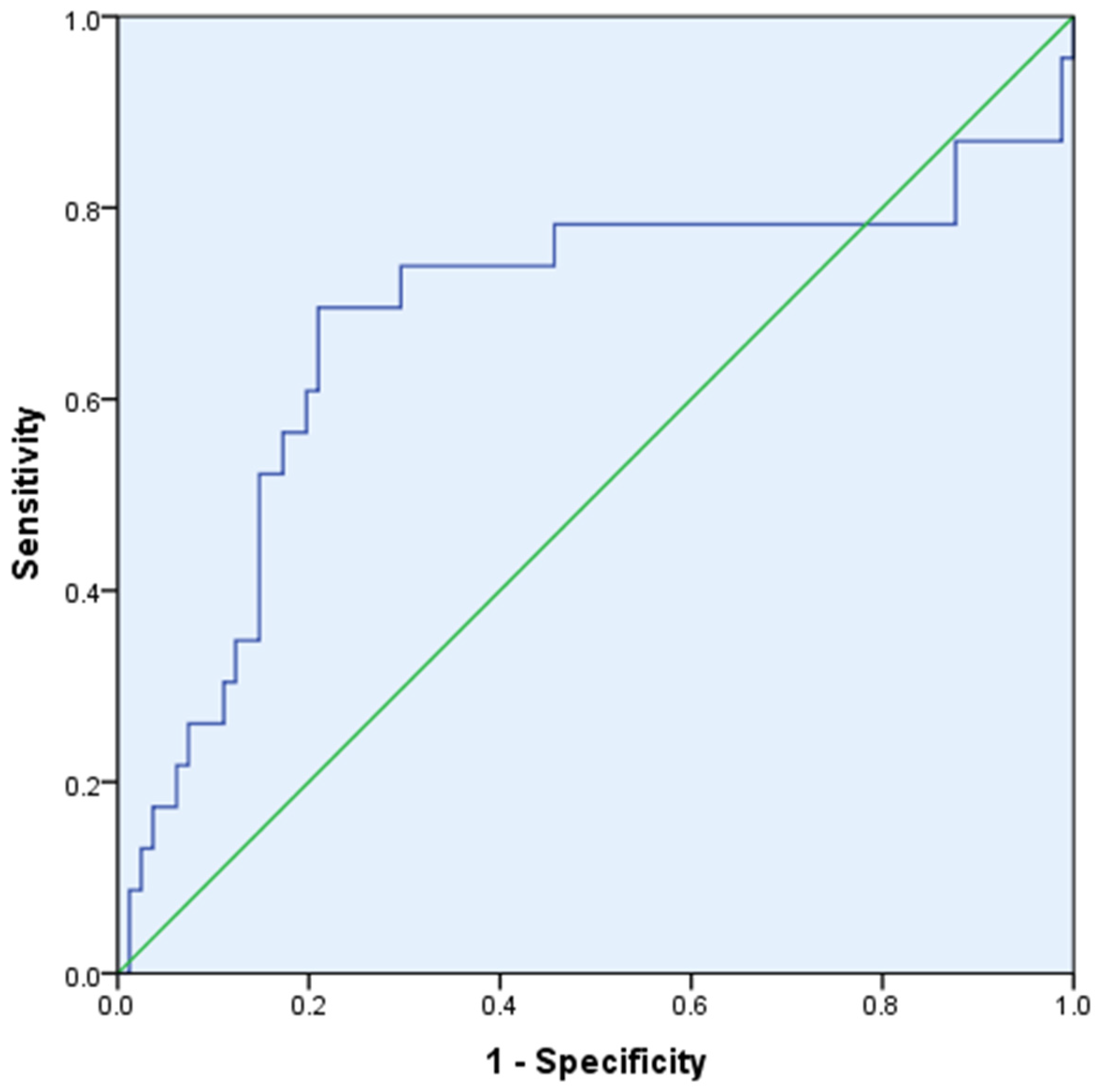
3.5. ∆ePVS and NT-proBNP
3.6. ∆ePVS and Clinical Outcomes
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pandhi, P.; ter Maaten, J.M.; Anker, S.D.; Ng, L.L.; Metra, M.; Samani, N.J.; Lang, C.C.; Dickstein, K.; de Boer, R.A.; van Veldhuisen, D.J.; et al. Pathophysiologic Processes and Novel Biomarkers Associated with Congestion in Heart Failure. JACC Heart Fail. 2022, 10, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Felker, G.M.; Fudim, M. Are We Getting Any Closer to Understanding Congestion? JACC Heart Fail. 2022, 10, 633–636. [Google Scholar] [CrossRef] [PubMed]
- Pellicori, P.; Platz, E.; Dauw, J.; ter Maaten, J.M.; Martens, P.; Pivetta, E.; Cleland, J.G.; McMurray, J.J.; Mullens, W.; Solomon, S.D.; et al. Ultrasound imaging of congestion in heart failure: Examinations beyond the heart. Eur. J. Heart Fail. 2021, 23, 703–712. [Google Scholar] [CrossRef]
- Verbrugge, F.H.; Guazzi, M.; Testani, J.M.; Borlaug, B.A. Altered Hemodynamics and End-Organ Damage in Heart Failure. Circulation 2020, 142, 998–1012. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, N.R.; Mazzola, M.; Bandini, G.; Barbieri, G.; Spinelli, S.; De Biase, N.; Masi, S.; Moggi-Pignone, A.; Ghiadoni, L.; Taddei, S.; et al. Prognostic Role of Sonographic Decongestion in Patients with Acute Heart Failure with Reduced and Preserved Ejection Fraction: A Multicentre Study. J. Clin. Med. 2023, 12, 773. [Google Scholar] [CrossRef]
- Girerd, N.; Seronde, M.F.; Coiro, S.; Chouihed, T.; Bilbault, P.; Braun, F.; Kenizou, D.; Maillier, B.; Nazeyrollas, P.; Roul, G.; et al. Integrative Assessment of Congestion in Heart Failure Throughout the Patient Journey. JACC Heart Fail. 2018, 6, 273–285. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726, Erratum in Eur. Heart J. 2021, 42, 4901. [Google Scholar] [CrossRef] [PubMed]
- Grigore, M.; Grigore, A.-M.; Ilieșiu, A.-M. Portal Vein Pulsatility: A Valuable Approach for Monitoring Venous Congestion and Prognostic Evaluation in Acute Decompensated Heart Failure. Diagnostics 2024, 14, 2029. [Google Scholar] [CrossRef] [PubMed]
- Hudson, S.R.; Chan, D.; Ng, L.L. Change in plasma volume and prognosis in acute decompensated heart failure: An observational cohort study. J. R. Soc. Med. 2016, 109, 337–346. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kobayashi, M.; Girerd, N.; Duarte, K.; Chouihed, T.; Chikamori, T.; Pitt, B.; Zannad, F.; Rossignol, P. Estimated plasma volume status in heart failure: Clinical implications and future directions. Clin. Res. Cardiol. 2021, 110, 1159–1172. [Google Scholar] [CrossRef] [PubMed]
- Swolinsky, J.S.; Tuvshinbat, E.; Leistner, D.M.; Edelmann, F.; Knebel, F.; Nerger, N.P.; Lemke, C.; Roehle, R.; Haase, M.; Costanzo, M.R.; et al. Discordance between estimated and measured changes in plasma volume among patients with acute heart failure. ESC Heart Fail. 2022, 9, 66–76. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Buffaloe, G.W.; Heineken, F.G. Plasma volume nomograms for use in therapeutic plasma exchange. Transfusion 1983, 23, 355–357. [Google Scholar] [CrossRef] [PubMed]
- Sprenger, K.B.; Huber, K.; Kratz, W.; Henze, E. Nomograms for the prediction of patient’s plasma volume in plasma exchange therapy from height, weight, and hematocrit. J. Clin. Apher. 1987, 3, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Emmens, J.E.; Ter Maaten, J.M.; Matsue, Y.; Figarska, S.M.; Sama, I.E.; Cotter, G.; Cleland, J.G.F.; Davison, B.A.; Felker, G.M.; Givertz, M.M.; et al. Worsening renal function in acute heart failure in the context of diuretic response. Eur. J. Heart Fail. 2022, 24, 365–374. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Knebel, F.; Schimke, I.; Pliet, K.; Schattke, S.; Martin, S.; Borges, A.C.; Baumann, G. NT-ProBNP in acute heart failure: Correlation with invasively measured hemodynamic parameters during recompensation. J. Card. Fail. 2005, 11, S38–S41. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of, Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–270, Erratum in Eur. Heart J. Cardiovasc. Imaging 2016, 17, 412. [Google Scholar] [CrossRef] [PubMed]
- Ilieșiu, A.M.; Hodorogea, A.S.; Balahura, A.M.; Bădilă, E. Non-Invasive Assessment of Congestion by Cardiovascular and Pulmonary Ultrasound and Biomarkers in Heart Failure. Diagnostics 2022, 12, 962. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.; Lobo, R. Why is Diuresis-related Weight Loss Not a Consistent Predictor of Clinical Outcomes in Heart Failure? -need to Account For Variability in Volume Status. J. Card. Fail. 2020, 26, S27. [Google Scholar] [CrossRef]
- Lam-Chung, C.E. Comprehensive review of SGLT2 inhibitors’ efficacy through their diuretic mode of action in diabetic patients. Front. Endocrinol. 2023, 14, 1174692. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Van Aelst, L.N.L.; Arrigo, M.; Placido, R.; Akiyama, E.; Girerd, N.; Zannad, F.; Manivet, P.; Rossignol, P.; Badoz, M.; Sadoune, M.; et al. Acutely decompensated heart failure with preserved and reduced ejection fraction present with comparable haemodynamic congestion. Eur. J. Heart Fail. 2018, 20, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Darawsha, W.; Chirmicci, S.; Solomonica, A.; Wattad, M.; Kaplan, M.; Makhoul, B.F.; Abassi, Z.A.; Azzam, Z.S.; Aronson, D. Discordance Between Hemoconcentration and Clinical Assessment of Decongestion in Acute Heart Failure. J. Card. Fail. 2016, 22, 680–688. [Google Scholar] [CrossRef] [PubMed]
- Metra, M.; Davison, B.; Bettari, L.; Sun, H.; Edwards, C.; Lazzarini, V.; Piovanelli, B.; Carubelli, V.; Bugatti, S.; Lombardi, C.; et al. Is worsening renal function an ominous prognostic sign in patients with acute heart failure? The role of congestion and its interaction with renal function. Circ. Heart Fail. 2012, 5, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Damman, K.; Tang, W.H.; Testani, J.M.; McMurray, J.J. Terminology and definition of changes renal function in heart failure. Eur. Heart J. 2014, 35, 3413–3416. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zannad, F.; Rossignol, P. Cardiorenal Syndrome Revisited. Circulation 2018, 138, 929–944. [Google Scholar] [CrossRef] [PubMed]
- Davison, B.A.; Metra, M.; Cotter, G.; Massie, B.M.; Cleland, J.G.F.; Dittrich, H.C.; Edwards, C.; Filippatos, G.; Givertz, M.M.; Greenberg, B.; et al. Worsening Heart Failure Following Admission for Acute Heart Failure: A Pooled Analysis of the PROTECT and RELAX-AHF Studies. JACC Heart Fail. 2015, 3, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L., Jr.; Camargo, C.A.; Anwaruddin, S.; Baggish, A.L.; Chen, A.A.; Krauser, D.G.; Tung, R.; Cameron, R.; Nagurney, J.T.; Chae, C.U.; et al. The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am. J. Cardiol. 2005, 95, 948–954. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L.; van Kimmenade, R.; Lainchbury, J.; Bayes-Genis, A.; Ordonez-Llanos, J.; Santalo-Bel, M.; Pinto, Y.M.; Richards, M. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: An. international pooled analysis of 1256 patients: The International Collaborative of NT-proBNP Study. Eur. Heart J. 2006, 27, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.; Rossignol, P.; Ferreira, J.P.; Aragão, I.; Paku, Y.; Iwasaki, Y.; Watanabe, M.; Fudim, M.; Duarte, K.; Zannad, F.; et al. Prognostic value of estimated plasma volume in acute heart failure in three cohort studies. Clin. Res. Cardiol. 2019, 108, 549–561, Erratum in Clin. Res. Cardiol. 2019, 108, 562. [Google Scholar] [CrossRef] [PubMed]
- Greene, S.J.; Gheorghiade, M.; Vaduganathan, M.; Ambrosy, A.P.; Mentz, R.J.; Subacius, H.; Maggioni, A.P.; Nodari, S.; Konstam, M.A.; Butler, J.; et al. Haemoconcentration, renal function, and post-discharge outcomes among patients hospitalized for heart failure with reduced ejection fraction: Insights from the EVEREST trial. Eur. J. Heart Fail. 2013, 15, 1401–1411. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Testani, J.M.; Chen, J.; McCauley, B.D.; Kimmel, S.E.; Shannon, R.P. Potential effects of aggressive decongestion during the treatment of decompensated heart failure on renal function and survival. Circulation 2010, 122, 265–272. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Davila, C.; Reyentovich, A.; Katz, S.D. Clinical correlates of hemoconcentration during hospitalization for acute decompensated heart failure. J. Card. Fail. 2011, 17, 1018–1022. [Google Scholar] [CrossRef] [PubMed]
| Baseline Admission Characteristics | Total (111 Patients) | Groups | ||
|---|---|---|---|---|
| Group 1 81 Patients | Group 2 30 Patients | p-Value | ||
| Age, years, median (IQR) | 74 (67–82) | 73 (66–82) | 74 (70–85) | 0.20 |
| Sex, female (%) | 39.29 | 40.7 | 36.67 | 0.56 |
| BMI (kg/m2), median (IQR) | 28.71 (24–33) | 28.57 (24–45) | 30.51 (27–32) | 0.23 |
| HR, beats/min, median (IQR) | 76 (69–100) | 75 (70–100) | 76.5 (66–100) | 0.66 |
| SBP, mmHg, median (IQR) | 130 (110–149) | 130 (115–147) | 130 (110–150) | 0.68 |
| Smoker (%) | 41.08 | 41.98 | 40 | 0.59 |
| Comorbidities | ||||
| IHD, (%) | 39.29 | 44.44 | 26.67 | 0.14 |
| HTN, (%) | 82.14 | 81.48 | 86.67 | 0.49 |
| DM (%) | 36.61 | 39.51 | 30 | 0.39 |
| CKD (%) | 60.71 | 56.79 | 73.33 | 0.16 |
| AF (%) | 57.14 | 54.32 | 66.67 | 0.30 |
| COPD (%) | 22.32 | 20.99 | 26.67 | 0.49 |
| Medication at admission | ||||
| ACEi (%) | 33.04 | 32.10 | 36.67 | 0.54 |
| ARB (%) | 16.07 | 18.52 | 10 | 0.33 |
| ARNI (%) | 17.86 | 20.99 | 10 | 0.24 |
| Beta-blocker (%) | 83.93 | 90.12 | 70 | 0.06 |
| MRA (%) | 68.75 | 79.01 | 43.33 | 0.0008 |
| SGLT-2 inhibitors (%) | 34.82 | 37.04 | 30 | 0.47 |
| CRT (%) | 5.40 | 5 | 1 | 0.08 |
| Parameter | Total (111 Patients) | Group 1 (81 Patients) | Group 2 (30 Patients) | p-Value |
|---|---|---|---|---|
| Weight (kg) | ||||
| Admission, mean | 83 ± 18.02 | 83.5 ± 18.82 | 83.8 ± 15.95 | 0.92 |
| Discharge, mean | 82 ± 17.10 | 80 ± 17.77 | 82 ± 14.55 | 0.17 |
| Weight difference, median, IQR | 2 (0–3) | 2 (1–3) | 1 (0–2) | 0.046 |
| Lower-limb edema (%) | ||||
| Admission | 36 | 31 | 48 | 0.28 |
| Discharge | 9 | 7 | 12 | 0.15 |
| Jugular vein distention (%) | ||||
| Admission | 71 | 68 | 75 | 0.38 |
| Discharge | 13 | 11 | 15 | 0.29 |
| Parameter | Total 111 Patients | Group 1 (81 Patients) | Group 2 (31 Patients) | p-Value |
|---|---|---|---|---|
| Echocardiography | ||||
| LVEF, mean | 46.74 ± 15.08 | 46.19 ± 15.16 | 46.03 ± 12.77 | 0.95 |
| E/e’ medial ratio, median | 28 (20–37) | 28.33 (19–39) | 29 (21–32) | 0.31 |
| LAd (mm), mean | 47 ± 6.99 | 47 ± 5.8 | 48 ± 8.9 | 0.87 |
| TAPSE (mm), mean | 17 ± 3.9 | 17 ± 3.8 | 16 ± 4.2 | 0.50 |
| S′RV (cm/s), mean | 11 ± 2 | 11.73 ± 1.9 | 11.31 ± 2.5 | 0.49 |
| IVC (mm), mean | 22 ± 4.8 | 22 ± 4.6 | 21 ± 5.3 | 0.82 |
| sPAP (mm Hg), mean | 49 ± 14.1 | 49 ± 13 | 50 ± 16 | 0.36 |
| Lung Ultrasound | ||||
| Pleural fluid (%) | 48.65 | 46.91 | 53.33 | 0.45 |
| Signs of pulmonary congestion (%) | 87.39 | 86.42 | 90 | 0.54 |
| Baseline | Total (111 Patients) | Group 1 (81 Patients) | Group 2 (30 Patients) | p-Value | Total 111 Patients | Group 1 (81 Patients) | Group 2 (30 Patients) | p-Value |
|---|---|---|---|---|---|---|---|---|
| Time | Admission | Discharge | ||||||
| Biochemical | ||||||||
| Hb (g/dL), mean | 12 ± 2.66 | 12.3 ± 2.68 | 11.75 ± 2.63 | 0.90 | 12.7 ± 2.4 | 13.4 ±2.34 | 11.2 ± 2.74 | 0.33 |
| Ht (%) | 37.4 ± 7.7 | 37.34 ± 7.62 | 37.8 ± 7.82 | 0.92 | 39.1 ± 7.02 | 40.6 ± 6.79 | 34.5 ± 9.01 | 0.33 |
| Creatinine (mg/dL), mean | 1.16 ± 0.65 | 1.08 ± 0.49 | 1.34 ± 0.57 | 0.048 | 1.19 ± 0.43 | 1.13 ± 0.49 | 1.32 ± 0.61 | 0.00418 |
| eGFR, (1.73 mL/min/mp), median | 54.50 (41–71) | 56 (43–73) | 51 (31–61) | 0.89 | 58.89 (44–73) | 59.67 (45–74) | 55.86 (40–64) | 0.86 |
| WRF (%) | 42.34 | 39.51 | 50 | 0.27 | ||||
| Serum urea (mg/dL) | 56 ± 38.5 | 54 ± 30 | 73 ± 55 | 0.0051 | 59 ± 37.1 | 54 ± 34.4 | 88 ± 53 | 0.09 |
| K (mmol/L) | 4.5 ± 0.56 | 4.45 ± 0.54 | 4.72 ± 0.61 | 0.57 | 4.17 ± 0.55 | 4.3 ± 0.56 | 3.89 ± 0.54 | 0.66 |
| Na (mmol/L) | 139 ± 3.80 | 139 ± 3.56 | 139 ± 4.11 | 0.37 | 138 ± 13.1 | 138 ± 16.61 | 137 ±3.48 | 0.60 |
| NT-proBNP (pg/dL), median | 4060 (1865–7085) | 3626 (2456–6254) | 4855.5 (1203–14,243) | 0.005 | 1561.5 (1013–2921) | 1454 (1002–2741) | 1899 (1120–5242) | 0.01 |
| Diuretic dose at admission and at discharge | ||||||||
| Furosemide (mg/day), median (IQR) | 20 (0–40) | 20 (0–35) | 20 (0–40) | 0.06 | 60 (40–80) | 60 (40–80) | 100 (40–120) | 0.03 |
| Diuretic dose during hospitalization | ||||||||
| Furosemide (mg/day), median (IQR) | 85 (60–110) | 75 (50–90) | 95 (70–120) | 0.03 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grigore, A.-M.; Grigore, M.; Balahura, A.-M.; Uscoiu, G.; Verde, I.; Nicolae, C.; Bădilă, E.; Ilieșiu, A.-M. The Role of the Estimated Plasma Volume Variation in Assessing Decongestion in Patients with Acute Decompensated Heart Failure. Biomedicines 2025, 13, 88. https://doi.org/10.3390/biomedicines13010088
Grigore A-M, Grigore M, Balahura A-M, Uscoiu G, Verde I, Nicolae C, Bădilă E, Ilieșiu A-M. The Role of the Estimated Plasma Volume Variation in Assessing Decongestion in Patients with Acute Decompensated Heart Failure. Biomedicines. 2025; 13(1):88. https://doi.org/10.3390/biomedicines13010088
Chicago/Turabian StyleGrigore, Andreea-Maria, Mihai Grigore, Ana-Maria Balahura, Gabriela Uscoiu, Ioana Verde, Camelia Nicolae, Elisabeta Bădilă, and Adriana-Mihaela Ilieșiu. 2025. "The Role of the Estimated Plasma Volume Variation in Assessing Decongestion in Patients with Acute Decompensated Heart Failure" Biomedicines 13, no. 1: 88. https://doi.org/10.3390/biomedicines13010088
APA StyleGrigore, A.-M., Grigore, M., Balahura, A.-M., Uscoiu, G., Verde, I., Nicolae, C., Bădilă, E., & Ilieșiu, A.-M. (2025). The Role of the Estimated Plasma Volume Variation in Assessing Decongestion in Patients with Acute Decompensated Heart Failure. Biomedicines, 13(1), 88. https://doi.org/10.3390/biomedicines13010088









