Diagnostic Performance of Serum Leucine-Rich Alpha-2-Glycoprotein 1 in Pediatric Acute Appendicitis: A Prospective Validation Study
Abstract
1. Introduction
2. Material and Methods
2.1. Ethics
2.2. Study Design
2.3. Primary and Secondary Outcomes
2.4. Sample Size Calculation
2.5. Analyzed Variables
2.6. Sample Collection and Determination of LRG-1
2.7. Statistical Analysis
3. Results
3.1. Sociodemographic and Clinical Characteristics
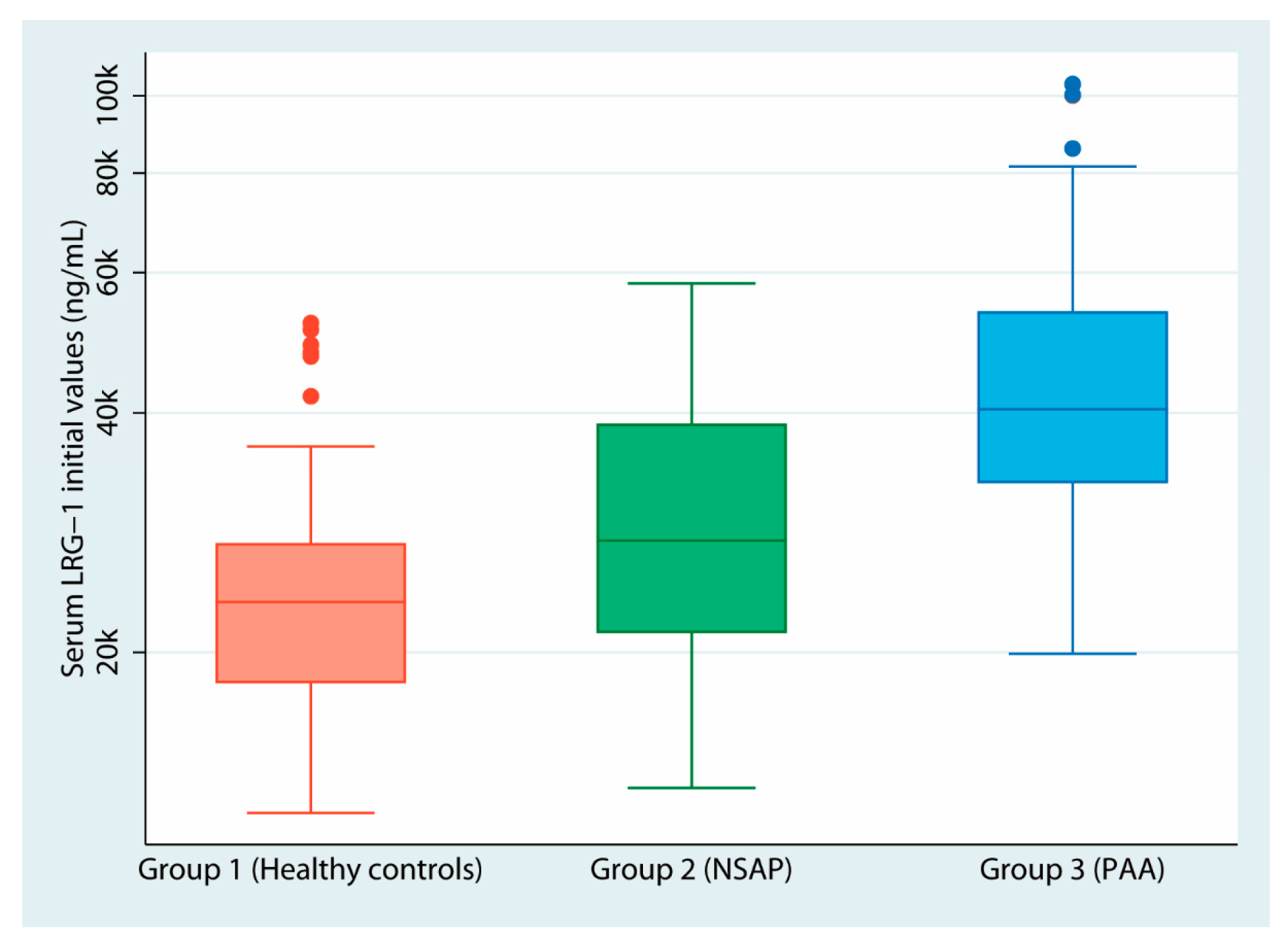
3.2. Serum LRG-1 Values
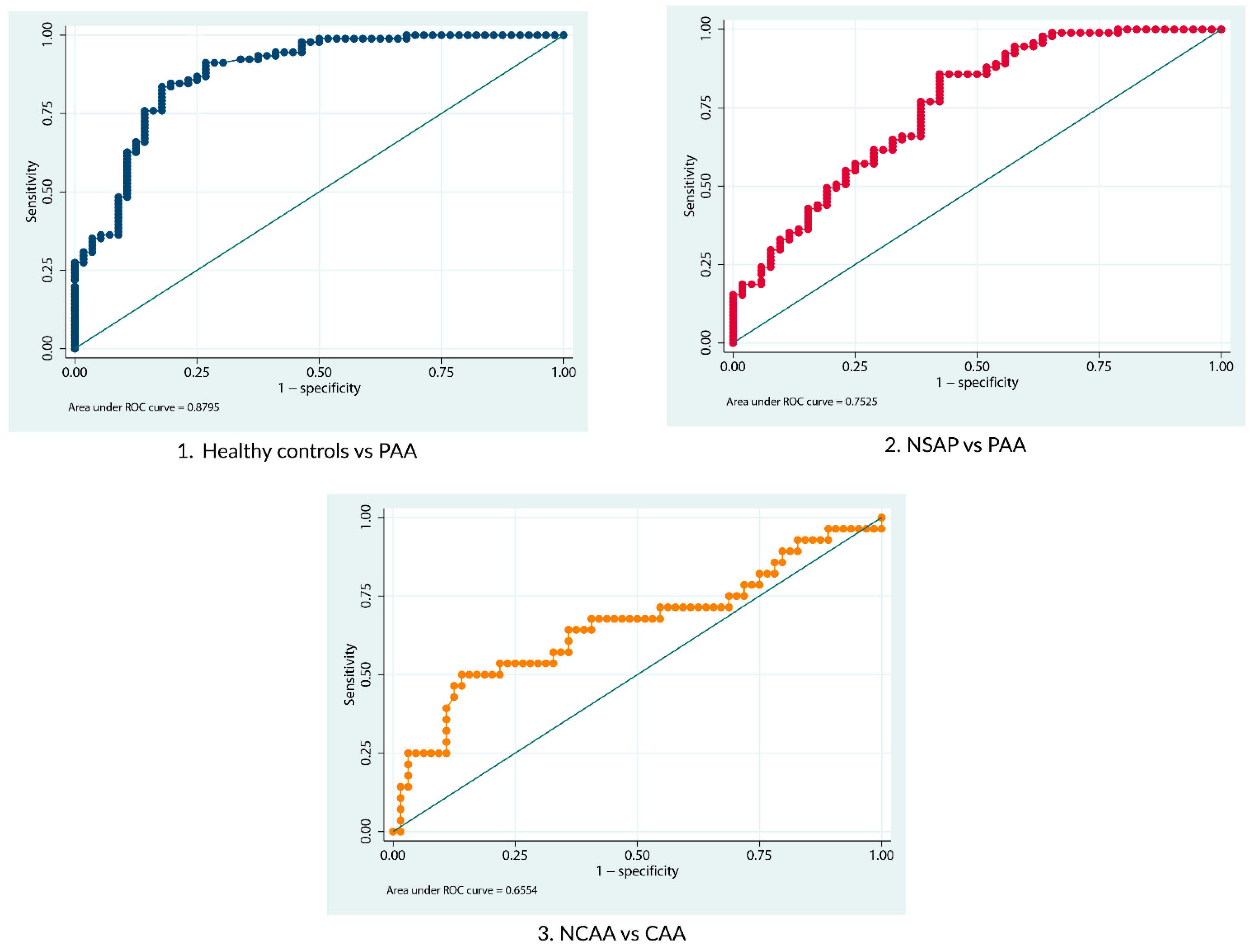
3.3. Diagnostic Performance of LRG-1 for Diagnosing Pediatric Acute Appendicitis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gadiparthi, R.; Waseem, M. Pediatric Appendicitis. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar] [PubMed]
- Mostafa, R.; El-Atawi, K. Misdiagnosis of Acute Appendicitis Cases in the Emergency Room. Cureus 2024, 16, e57141. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Benabbas, R.; Hanna, M.; Shah, J.; Sinert, R. Diagnostic Accuracy of History, Physical Examination, Laboratory Tests, and Point-of-care Ultrasound for Pediatric Acute Appendicitis in the Emergency Department: A Systematic Review and Meta-analysis. Acad. Emerg. Med. 2017, 24, 523–551. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.M.; Suh, C.H.; Cho, Y.A.; Kim, J.R.; Lee, J.S.; Jung, A.Y.; Kim, J.H.; Lee, J.Y.; Kim, S.Y. The diagnostic performance of reduced-dose CT for suspected appendicitis in pediatric and adult patients: A systematic review and diagnostic meta-analysis. Eur. Radiol. 2018, 28, 2537–2548. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.M.; Kulaylat, A.N.; Hollenbeak, C.S.; Engbrecht, B.W.; Dillman, J.R.; Methratta, S.T. Magnetic resonance imaging in pediatric appendicitis: A systematic review. Pediatr. Radiol. 2016, 46, 928–939. [Google Scholar] [CrossRef] [PubMed]
- Gudjonsdottir, J.; Marklund, E.; Hagander, L.; Salö, M. Clinical Prediction Scores for Pediatric Appendicitis. Eur. J. Pediatr. Surg. 2021, 31, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Arredondo Montero, J.; Bardají Pascual, C.; Antona, G.; Ros Briones, R.; López-Andrés, N.; Martín-Calvo, N. The BIDIAP index: A clinical, analytical and ultrasonographic score for the diagnosis of acute appendicitis in children. Pediatr. Surg. Int. 2023, 39, 175. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Delgado-Miguel, C.; Muñoz-Serrano, A.; San Basilio, M.; Miguel-Ferrero, M.; de Ceano-Vivas, M.; Martínez, L. The role of the neutrophil-to-lymphocyte ratio in avoiding negative appendectomies. An. Pediatr. (Engl. Ed.) 2023, 98, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Elliver, M.; Salö, M.; Roth, B.; Ohlsson, B.; Hagander, L.; Gudjonsdottir, J. Associations between Th1-related cytokines and complicated pediatric appendicitis. Sci. Rep. 2024, 14, 4613. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, T.; Cheng, Y.; Zhou, Y.; Zhang, Z.; Qi, S.; Pan, Z. Diagnostic performance of type I hypersensitivity-specific markers combined with CRP and IL-6 in complicated acute appendicitis in pediatric patients. Int. Immunopharmacol. 2023, 124, 110977. [Google Scholar] [CrossRef] [PubMed]
- Druhan, L.J.; Lance, A.; Li, S.; Price, A.E.; Emerson, J.T.; Baxter, S.A.; Gerber, J.M.; Avalos, B.R. Leucine Rich α-2 Glycoprotein: A Novel Neutrophil Granule Protein and Modulator of Myelopoiesis. PLoS ONE 2017, 12, e0170261. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zou, Y.; Xu, Y.; Chen, X.; Wu, Y.; Fu, L.; Lv, Y. Research Progress on Leucine-Rich Alpha-2 Glycoprotein 1: A Review. Front. Pharmacol. 2022, 12, 809225. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Arredondo Montero, J.; Pérez Riveros, B.P.; Bueso Asfura, O.E.; Rico Jiménez, M.; López-Andrés, N.; Martín-Calvo, N. Leucine-Rich Alpha-2-Glycoprotein as a non-invasive biomarker for pediatric acute appendicitis: A systematic review and meta-analysis. Eur. J. Pediatr. 2023, 182, 3033–3044, Erratum in: Eur. J. Pediatr. 2023, 182, 3045–3047. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tintor, G.; Jukić, M.; Šupe-Domić, D.; Jerončić, A.; Pogorelić, Z. Diagnostic Accuracy of Leucine-Rich α-2-Glycoprotein 1 as a Non-Invasive Salivary Biomarker in Pediatric Appendicitis. Int. J. Mol. Sci. 2023, 24, 6043. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Daniels, J.; Montgomery, E. Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas, 2nd ed.; W.B. Saunders: Philadelphia, PA, USA, 2009; pp. 395–404. ISBN 9781416040590. [Google Scholar]
- Kharbanda, A.B.; Rai, A.J.; Cosme, Y.; Liu, K.; Dayan, P.S. Novel serum and urine markers for pediatric appendicitis. Acad. Emerg. Med. 2012, 19, 56–62. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Arredondo Montero, J.; Antona, G.; Bronte Anaut, M.; Bardají Pascual, C.; Ros Briones, R.; Fernández-Celis, A.; Rivero Marcotegui, A.; López-Andrés, N.; Martín-Calvo, N. Diagnostic performance of serum pentraxin-3 in pediatric acute appendicitis: A prospective diagnostic validation study. Pediatr. Surg. Int. 2022, 39, 27, Erratum in: Pediatr. Surg. Int. 2022, 39, 49. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kentsis, A.; Ahmed, S.; Kurek, K.; Brennan, E.; Bradwin, G.; Steen, H.; Bachur, R. Detection and diagnostic value of urine leucine-rich α-2-glycoprotein in children with suspected acute appendicitis. Ann. Emerg. Med. 2012, 60, 78–83.e1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Salö, M.; Roth, B.; Stenström, P.; Arnbjörnsson, E.; Ohlsson, B. Urinary biomarkers in pediatric appendicitis. Pediatr. Surg. Int. 2016, 32, 795–804. [Google Scholar] [CrossRef] [PubMed]
- Yap, T.L.; Fan, J.D.; Chen, Y.; Ho, M.F.; Choo, C.S.; Allen, J.; Low, Y.; Jacobsen, A.S.; Nah, S.A. A novel noninvasive appendicitis score with a urine biomarker. J. Pediatr. Surg. 2019, 54, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Mahalik, S.K.; Bandyopadhyay, D.; Tripathy, B.B.; Pati, A.B.; Mohanty, M.K. Diagnostic accuracy of Leucine-rich α-2 glycoprotein (LRG) as a urinary biomarker in pediatric appendicitis: A prospective observational pilot study from Eastern India. Ann. Pediatr. Surg. 2021, 17, 22. [Google Scholar] [CrossRef]
- Kakar, M.; Berezovska, M.M.; Broks, R.; Asare, L.; Delorme, M.; Crouzen, E.; Zviedre, A.; Reinis, A.; Engelis, A.; Kroica, J.; et al. Serum and Urine Biomarker Leucine-Rich Alpha-2 Glycoprotein 1 Differentiates Pediatric Acute Complicated and Uncomplicated Appendicitis. Diagnostics 2021, 11, 860. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yap, T.L.; Fan, J.D.; Ho, M.F.; Choo, C.S.C.; Ong, L.Y.; Chen, Y. Salivary biomarker for acute appendicitis in children: A pilot study. Pediatr. Surg. Int. 2020, 36, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Tintor, G.; Jukić, M.; Šupe-Domić, D.; Jerončić, A.; Pogorelić, Z. Diagnostic Utility of Serum Leucine-Rich α-2-Glycoprotein 1 for Acute Appendicitis in Children. J. Clin. Med. 2023, 12, 2455. [Google Scholar] [CrossRef] [PubMed]
- Rainer, T.H.; Leung, L.Y.; Chan, C.; Leung, Y.K.; Cheng, N.M.; Lai, P.; Cheung, Y.S.; Graham, C.A. Circulating human leucine-rich α-2-glycoprotein 1 mRNA and protein levels to detect acute appendicitis in patients with acute abdominal pain. Clin. Biochem. 2017, 50, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Lontra, M.B.; Savaris, R.F.; Cavazzola, L.T.; Maissiat, J. Comparison of leucine-rich alpha-2-glycoprotein-1 (LRG-1) plasma levels between patients with and without appendicitis, a case-controlled study. Sci. Rep. 2021, 11, 5574. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Demirci, O.L.; Cevik, Y.; Corbacioglu, S.K.; Taner, A. Value of Leucine-rich alpha-2-glycoprotein-1 (LRG-1) on diagnosis of acute appendicitis in female patients with right lower-quadrant abdominal pain. J. Pak. Med. Assoc. 2017, 67, 1383–1386. [Google Scholar] [PubMed]
| Sociodemographics | Group 1 (Healthy Controls) n = 56 | Group 2 (NSAP) n = 52 | Group 3 (PAA) n = 92 | Total | p-Value |
|---|---|---|---|---|---|
| Age (years) | 8.68 (3.26) | 11.09 (2.48) | 9.6 (3.01) | 9.73 (3.08) | <0.001 |
| Sex, Male/Total (percentage) | 46/56 (82.1%) | 24/52 (46.2%) | 59/92 (64.1%) | 129/200 (64.5%) | <0.001 |
| Weight, kg | 35.75 (18.38) | 45.36 (15.40) | 35.77 (12.09) | 38.27 (15.47) | <0.001 |
| Clinical Variables | Healthy Controls (n = 56) | NSAP (n = 52) | PAA (n = 92) | p-Value |
|---|---|---|---|---|
| Hours since the onset of pain | - | 31.58 (23.13) | 27.14 (19.42) | 0.38 |
| Fever at home >37.8 °C, Yes/no/missing | - | 15/37 | 29/62/1 | 0.85 |
| Number of diarrheal stools | - | 0.4 (1.21) | 0.68 (2.48) | 0.59 |
| Urinary symptoms, Yes/no/missing | - | 8/44 | 21/70/1 | 0.39 |
| Number of emetic episodes | - | 0.56 (1.96) | 2.48 (2.49) | <0.001 |
| Hyporexia, Yes/no/missing | - | 35/15/2 | 71/17/4 | 0.21 |
| Leukocytes (×109/L) * | - | 9.6 (7.8–12.5) | 16.1 (13–18.8) | 0.0001 *** |
| Neutrophils (×109/L) * | - | 5.9 (4.1–8.4) | 13.2 (9.5–16.2) | 0.0001 *** |
| C-Reactive Protein (mg/L) | - | 1.7 (1–22.2) | 26.9 (6.4–63.3) | 0.0001 *** |
| Initial LRG-1 (ng/mL) * | 23,145 (18,246–27,453) | 27,655 (21,151–38,795) | 40,409 (32,631–53,655) | <0.0001 ** <0.0001 *** |
| Clinical Variables | NCAA (n = 64) | CAA (n = 28) | p-Value |
|---|---|---|---|
| Hours since the onset of pain | 24.63 (18.72) | 32.77 (20.12) | 0.03 |
| Fever at home >37.8 °C, Yes/no/ missing | 13/50/1 | 16/12 | 0.001 |
| Number of diarrheal stools | 0.75 (2.82) | 0.54 (1.50) | 0.78 |
| Urinary symptoms, Yes/no/missing | 14/49/1 | 7/21 | 0.79 |
| Number of emetic episodes | 2.24 (2.31) | 3.04 (2.81) | 0.23 |
| Hyporexia, Yes/no/missing | 48/13/3 | 23/4/1 | 0.56 |
| Leukocytes (×109/L) * | 15.2 (12.1–17.6) | 18 (15.4–21.8) | 0.002 |
| Neutrophils (×109/L) * | 12.1 (8.8–15.3) | 15.3 (12.9–17.6) | 0.001 |
| C-Reactive Protein (mg/L) | 18.2 (4.7–40.1) | 63.3 (17.4–108) | 0.0006 |
| Initial serum LRG-1 (ng/mL) * | 38,686 (31,804–48,816) | 51,857 (34,013–64,202) | 0.02 |
| Serum LRG-1 at 12 h post-surgery (ng/mL) *, ** | 41,226 (33,904–50,918) | 60,432 (44,809–69,370) | 0.002 |
| Group Comparison | AUC Value | 95% CI | Proposed Serum LRG-1 Cut Off (ng/mL) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|
| Healthy Controls vs. PAA | 0.88 | 0.82–0.94 | 25,610 | 91.2 | 73.2 |
| NSAP vs. PAA | 0.75 | 0.67–0.84 | 28,614 | 85.7 | 57.7 |
| NCAA vs. CAA | 0.66 | 0.52–0.79 | 44,382 | 64.3 | 64.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arredondo Montero, J.; Ros Briones, R.; Fernández-Celis, A.; López-Andrés, N.; Martín-Calvo, N. Diagnostic Performance of Serum Leucine-Rich Alpha-2-Glycoprotein 1 in Pediatric Acute Appendicitis: A Prospective Validation Study. Biomedicines 2024, 12, 1821. https://doi.org/10.3390/biomedicines12081821
Arredondo Montero J, Ros Briones R, Fernández-Celis A, López-Andrés N, Martín-Calvo N. Diagnostic Performance of Serum Leucine-Rich Alpha-2-Glycoprotein 1 in Pediatric Acute Appendicitis: A Prospective Validation Study. Biomedicines. 2024; 12(8):1821. https://doi.org/10.3390/biomedicines12081821
Chicago/Turabian StyleArredondo Montero, Javier, Raquel Ros Briones, Amaya Fernández-Celis, Natalia López-Andrés, and Nerea Martín-Calvo. 2024. "Diagnostic Performance of Serum Leucine-Rich Alpha-2-Glycoprotein 1 in Pediatric Acute Appendicitis: A Prospective Validation Study" Biomedicines 12, no. 8: 1821. https://doi.org/10.3390/biomedicines12081821
APA StyleArredondo Montero, J., Ros Briones, R., Fernández-Celis, A., López-Andrés, N., & Martín-Calvo, N. (2024). Diagnostic Performance of Serum Leucine-Rich Alpha-2-Glycoprotein 1 in Pediatric Acute Appendicitis: A Prospective Validation Study. Biomedicines, 12(8), 1821. https://doi.org/10.3390/biomedicines12081821









