The Use and Potential Benefits of N-Acetylcysteine in Non-Acetaminophen Acute Liver Failure: An Etiology-Based Review
Abstract
1. Introduction
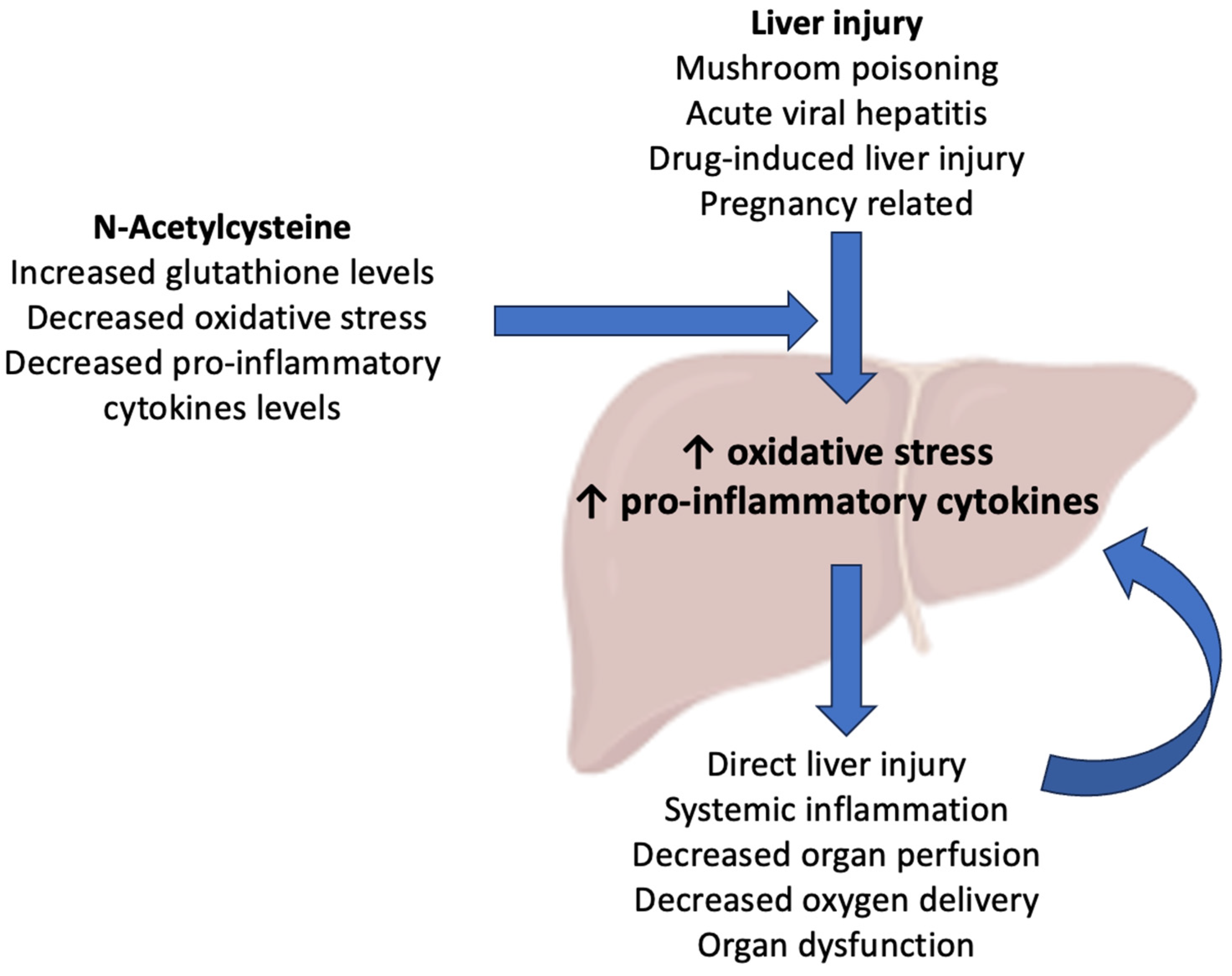
2. Pharmacological Rationale behind the Use of N-Acetylcysteine in Acute Liver Failure
3. Acute Liver Failure Due to Mushroom Poisoning
4. ALF Due to Viral Hepatitis
5. Acute Liver Failure Due to Non-Paracetamol Drug-Induced Liver Injury
6. Pregnancy-Related Acute Liver Failure
7. Pooled Analyses of Acute Liver Failure Etiologies
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tandon, B.N.; Joshi, Y.K.; Tandon, M. Acute liver failure: Experience with 145 patients. J. Clin. Gastroenterol. 1986, 8, 664–668. [Google Scholar] [CrossRef] [PubMed]
- Bihari, D. Acute liver failure. Clin. Anaesthesiol. 1985, 3, 973–998. [Google Scholar] [CrossRef]
- Donnelly, M.C.; Davidson, J.S.; Martin, K.; Baird, A.; Hayes, P.C.; Simpson, K.J. Acute liver failure in Scotland: Changes in aetiology and outcomes over time (the Scottish Look-Back Study). Aliment. Pharmacol. Ther. 2017, 45, 833–843. [Google Scholar] [CrossRef] [PubMed]
- Wendon, J.; Cordoba, J.; Dhawan, A.; Larsen, F.S.; Manns, M.; Nevens, F.; Samuel, D.; Simpson, K.J.; Yaron, I.; Bernardi, M. EASL Clinical Practical Guidelines on the management of acute (fulminant) liver failure. J. Hepatol. 2017, 66, 1047–1081. [Google Scholar] [CrossRef] [PubMed]
- Alshamsi, F.; Alshammari, K.; Belley-Cote, E.; Dionne, J.; Albrahim, T.; Albudoor, B.; Ismail, M.; Al-judaibi, B.; Baw, B.; Subramanian, R.M.; et al. Extracorporeal liver support in patients with liver failure: A systematic review and meta-analysis of randomized trials. Intensive Care Med. 2020, 46, 1–16. [Google Scholar] [CrossRef]
- Kanjo, A.; Ocskay, K.; Gede, N.; Kiss, S.; Szakács, Z.; Párniczky, A.; Mitzner, S.; Stange, J.; Hegyi, P.; Molnár, Z. Efficacy and safety of liver support devices in acute and hyperacute liver failure: A systematic review and network meta-analysis. Sci. Rep. 2021, 11, 4189. [Google Scholar] [CrossRef]
- Bernal, W.; Lee, W.M.; Wendon, J.; Larsen, F.S.; Williams, R. Acute liver failure: A curable disease by 2024? J. Hepatol. 2015, 62, S112–S120. [Google Scholar]
- Bernal, W.; Auzinger, G.; Dhawan, A.; Wendon, J. Acute liver failure. Lancet 2010, 376, 190–201. [Google Scholar] [CrossRef]
- Mian, P.; Van Den Anker, J.N.; van Calsteren, K.; Annaert, P.; Tibboel, D.; Pfister, M.; Allegaert, K.; Dallmann, A. Physiologically based pharmacokinetic modeling to characterize acetaminophen pharmacokinetics and N-acetyl-p-benzoquinone imine (NAPQI) formation in non-pregnant and pregnant women. Clin. Pharmacokinet. 2020, 59, 97–110. [Google Scholar] [CrossRef]
- Harrison, P.; Wendon, J.; Williams, R. Evidence of increased guanylate cyclase activation by acetylcysteine in fulminant hepatic failure. Hepatology 1996, 23, 1067–1072. [Google Scholar] [CrossRef]
- Harrison, P.M.; Wendon, J.A.; Gimson, A.E.; Alexander, G.J.; Williams, R. Improvement by acetylcysteine of hemodynamics and oxygen transport in fulminant hepatic failure. N. Engl. J. Med. 1991, 324, 1852–1857. [Google Scholar] [CrossRef]
- Liou, G.G.; Hsieh, C.C.; Lee, Y.J.; Li, P.H.; Tsai, M.S.; Li, C.T.; Wang, S.H. N-Acetyl cysteine overdose inducing hepatic steatosis and systemic inflammation in both propacetamol-induced hepatotoxic and normal mice. Antioxidants 2021, 10, 442. [Google Scholar] [CrossRef]
- Singh, M.; Sasi, P.; Gupta, V.H.; Rai, G.; Amarapurkar, D.N.; Wangikar, P.P. Protective effect of curcumin, silymarin and N-acetylcysteine on antitubercular drug-induced hepatotoxicity assessed in an in vitro model. Hum. Exp. Toxicol. 2012, 31, 788–797. [Google Scholar] [CrossRef]
- Antoniades, C.G.; Berry, P.A.; Wendon, J.A.; Vergani, D. The importance of immune dysfunction in determining outcome in acute liver failure. J. Hepatol. 2008, 49, 845–861. [Google Scholar] [CrossRef] [PubMed]
- Faghfouri, A.H.; Zarezadeh, M.; Tavakoli-Rouzbehani, O.M.; Radkhah, N.; Faghfuri, E.; Kord-Varkaneh, H.; Tan, S.C.; Ostadrahimi, A. The effects of N-acetylcysteine on inflammatory and oxidative stress biomarkers: A systematic review and meta-analysis of controlled clinical trials. Eur. J. Pharmacol. 2020, 884, 173368. [Google Scholar] [CrossRef] [PubMed]
- Stravitz, R.T.; Sanyal, A.J.; Reisch, J.; Bajaj, J.S.; Mirshahi, F.; Cheng, J.; Lee, W.M.; The Acute Liver Failure Study Group. Effects of N-acetylcysteine on cytokines in non-acetaminophen acute liver failure: Potential mechanism of improvement in transplant-free survival. Liver Int. 2013, 33, 1324–1331. [Google Scholar] [CrossRef] [PubMed]
- Bémeur, C.; Vaquero, J.; Desjardins, P.; Butterworth, R.F. N-acetylcysteine attenuates cerebral complications of non-acetaminophen-induced acute liver failure in mice: Antioxidant and anti-inflammatory mechanisms. Metab. Brain Dis. 2010, 25, 241–249. [Google Scholar] [CrossRef]
- Jaeschke, H.; Ramachandran, A. Reactive oxygen species in the normal and acutely injured liver. J. Hepatol. 2011, 55, 227. [Google Scholar] [CrossRef]
- Jaeschke, H. Reactive oxygen and mechanisms of inflammatory liver injury: Present concepts. J. Gastroenterol. Hepatol. 2011, 26, 173–179. [Google Scholar] [CrossRef]
- Mukhopadhyay, P.; Horváth, B.; Zsengellėr, Z.; Bátkai, S.; Cao, Z.; Kechrid, M.; Holovac, E.; Erdėlyi, K.; Tanchian, G.; Liaudet, L.; et al. Mitochondrial reactive oxygen species generation triggers inflammatory response and tissue injury associated with hepatic ischemia–reperfusion: Therapeutic potential of mitochondrially targeted antioxidants. Free Radic. Biol. Med. 2012, 53, 1123–1138. [Google Scholar] [CrossRef]
- Brandenburg, W.E.; Ward, K.J. Mushroom poisoning epidemiology in the United States. Mycologia 2018, 110, 637–641. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Pu, L.Y.; Lu, L.; Wang, X.H.; Zhang, F.; Rao, J.H. N-acetylcysteine attenuates reactive-oxygen-species-mediated endoplasmic reticulum stress during liver ischemia-reperfusion injury. World J. Gastroenterol. 2014, 20, 15289. [Google Scholar] [CrossRef]
- Wennig, R.; Eyer, F.; Schaper, A.; Zilker, T.; Andresen-Streichert, H. Mushroom poisoning. Dtsch. Arztebl. Int. 2020, 117, 701. [Google Scholar] [CrossRef]
- Eren, S.H.; Demirel, Y.; Ugurlu, S.; Korkmaz, I.; Aktas, C.; Güven, F.M.K. Mushroom poisoning: Retrospective analysis of 294 cases. Clinics 2010, 65, 491–496. [Google Scholar] [CrossRef]
- Vetter, J. Toxins of Amanita phalloides. Toxicon 1998, 36, 13–24. [Google Scholar] [CrossRef]
- Ye, Y.; Liu, Z. Management of Amanita phalloides poisoning: A literature review and update. J. Crit. Care 2018, 46, 17–22. [Google Scholar] [CrossRef]
- Locatelli, C.; Maccarini, D.; Travaglia, A.; Manzo, L. Prolonged high-dose-acetylcysteine treatment of amanita phalloides and chlorinated hydrocarbon poisoning. Pharmacol. Res. 1992, 26, 201. [Google Scholar] [CrossRef]
- Rodrigues, D.F.; Pires das Neves, R.; Carvalho, A.T.; Lourdes Bastos, M.; Costa, V.M.; Carvalho, F. In vitro mechanistic studies on α-amanitin and its putative antidotes. Arch. Toxicol. 2020, 94, 2061–2078. [Google Scholar] [CrossRef] [PubMed]
- Le Daré, B.; Ferron, P.J.; Gicquel, T. Toxic effects of amanitins: Repurposing toxicities toward new therapeutics. Toxins 2021, 13, 417. [Google Scholar] [CrossRef]
- Leist, M.; Gantner, F.; Naumann, H.; Bluethmann, H.; Vogt, K.; Brigelius-Flohe, R.; Nicotera, P.; Hans-Dieter, V.; Albrecht, W. Tumor necrosis factor-induced apopto- sis during the poisoning of mice with hepatotoxins. Gastroenterology 1997, 112, 923–934. [Google Scholar] [CrossRef]
- Zheleva, A.; Tolekova, A.; Zhelev, M.; Uzunova, V.; Platikanova, M.; Gadzheva, V. Free radical reactions might contribute to severe alpha amanitin hepatotoxicity-a hypothesis. Med. Hypotheses 2007, 69, 361–367. [Google Scholar] [CrossRef]
- Zheleva, A. Phenoxyl radicals formation might contribute to severe toxicity of mushrooms toxin alpha-amanitin- an electron paramagnetic resonance study. TJS 2013, 11, 33–38. [Google Scholar]
- Schneider, S.M.; Michelson, E.A.; Vanscoy, G. Failure of N-Acetylcysteine to reduce alpha amanitin toxicity. J. Appl. Toxicol. 1992, 12, 141–142. [Google Scholar] [CrossRef]
- Yamada, E.G.; Mohle-Boetani, J.; Olson, K.R.; Werner, S.B. Mushroom poisoning due to amatoxin. Northern California, Winter 1996–1997. West J. Med. 1998, 169, 380–384. [Google Scholar] [PubMed]
- Montaninia, S.; Sinardia, D.; Praticò, C.; Sinardia, A.U.; Trimarchi, G. Use of acetylcysteine as the life-saving antidote in Amanita phalloides (death cap) poisoning. Arzneimittelforschung 1999, 49, 1044–1047. [Google Scholar] [CrossRef] [PubMed]
- Locatelli, C.A.; Petrolini, V.M.; Vecchio, S.; Bigi, S.; Lonati, D.; Giampreti, A.; Coccini, T.; Roda, E.; Acerbi, D.; Manzo, L. Outcome in 157 alpha-amanitin-poisoned patients treated with the “Pavia protocol”. Toxicol. Lett. 2010, 196, S91. [Google Scholar] [CrossRef]
- Ahishali, E.; Boynuegri, B.; Ozpolat, E.; Surmeli, H.; Dolapcioglu, C.; Dabak, R.; Bahcebasi, Z.B.; Bayramicli, O.U. Approach to mushroomintoxication and treatment: Can we decrease mortality? Clin. Res. Hepatol. Gastroenterol. 2012, 36, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Akın, A.; Keşkek, Ş.Ö.; Kılıç, D.A.; Aliustaoğlu, M.E.; Keşkek, N. The effects of N-acetylcysteine in patients with Amanita phalloides intoxication. J. Drug Metab. Toxicol. 2013, 4, 2. [Google Scholar]
- Karvellas, C.J.; Tillman, H.; Leung, A.A.; Lee, W.M.; Schilsky, M.L.; Hameed, B.; Stravitz, R.T.; McGuire, B.M.; Fix, O.K.; United States Acute Liver Failure Study Group. Acute liver injury and acute liver failure from mushroom poisoning in North America. Liver Int. 2016, 36, 1043–1050. [Google Scholar] [CrossRef]
- Albertson, T.E.; Clark, R.F.; Smollin, C.G.; Vohra, R.; Lewis, J.C.; Chenoweth, J.A.; Stocking, J.C. A ten-year retrospective California Poison Control System experience with possible amatoxin mushroom calls. Clin. Toxicol. 2023, 61, 974–981. [Google Scholar] [CrossRef]
- Tan, J.L.; Stam, J.; van den Berg, A.P.; van Rheenen, P.F.; Dekkers, B.G.; Touw, D.J. Amanitin intoxication: Effects of therapies on clinical outcomes–a review of 40 years of reported cases. Clin. Toxicol. 2022, 60, 1251–1265. [Google Scholar] [CrossRef]
- Razavi, H. Global epidemiology of viral hepatitis. Gastroenterol. Clin. 2020, 49, 179–189. [Google Scholar] [CrossRef]
- Patterson, J.; Hussey, H.S.; Silal, S.; Goddard, L.; Setshedi, M.; Spearman, W.; Hussey, G.D.; Kagina, B.M.; Muloiwa, R. Systematic review of the global epidemiology of viral-induced acute liver failure. BMJ Open 2020, 10, e037473. [Google Scholar] [CrossRef]
- Phipps, M.M.; Barraza, L.H.; LaSota, E.D.; Sobieszczyk, M.E.; Pereira, M.R.; Zheng, E.X.; Fox, A.N.; Zucker, J.; Verna, E.C. Acute liver injury in COVID-19: Prevalence and association with clinical outcomes in a large US cohort. Hepatology 2020, 72, 807–817. [Google Scholar] [CrossRef]
- Sekiyama, K.D.; Yoshiba, M.; Thomson, A.W. Circulating proinflammatory cytokines (IL-1β, TNF-α, and IL-6) and IL-1 receptor antagonist (IL-1Ra) in fulminant hepatic failure and acute hepatitis. Clin. Exp. Immunol. 1994, 98, 71–77. [Google Scholar] [CrossRef]
- Li, Z.; Xu, X.; Leng, X.; He, M.; Wang, J.; Cheng, S.; Wu, H. Roles of reactive oxygen species in cell signaling pathways and immune responses to viral infections. Arch. Virol. 2017, 162, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Ferraz, A.C.; da Silva Menegatto, M.B.; Lima, R.L.S.; Ola-Olub, O.S.; Costa, D.C.; de Magalhães, J.C.; Rezende, I.M.; LaBeaud, A.D.; Monath, T.P.; Alves, P.A.; et al. Yellow fever virus infection in human hepatocyte cells triggers an imbalance in redox homeostasis with increased reactive oxygen species production, oxidative stress, and decreased antioxidant enzymes. Free Radic. Biol. Med. 2024, 213, 266–273. [Google Scholar] [CrossRef]
- Chandrasena, L.; De Silva, A.; De Mel, C.; Peiris, H.; Abesuriya, V.; De Mel, S.; Seneviratne, S.; Bandara, S. Glutathione enzymes and liver injury in acute dengue viral infection. J. Biosci. Med. 2019, 7, 61. [Google Scholar] [CrossRef]
- Marginean, C.M.; Pirscoveanu, D.; Popescu, M.; Vasile, C.M.; Docea, A.O.; Mitruț, R.; Mărginean, I.C.; Iacob, G.A.; Firu, D.M.; Mitruț, P. Challenges in Diagnosis and Therapeutic Approach of Acute on Chronic Liver Failure—A Review of Current Evidence. Biomedicines 2023, 11, 1840. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.L.; Yin, X.J.; Li, X.L.; Wang, F.D.; Zhou, J.; Tao, Y.C.; Wang, Y.H.; Wu, D.B.; Chen, E.Q. Retrospective analysis of the clinical efficacy of n-acetylcysteine in the treatment of hepatitis B virus related acute-on-chronic liver failure. Front. Med. 2021, 8, 724224. [Google Scholar] [CrossRef]
- Sotelo, N.; de los Ángeles Durazo, M.; Gonzalez, A.; Dhanakotti, N. Early treatment with N-acetylcysteine in children with acute liver failure secondary to hepatitis A. Ann. Hepatol. 2009, 8, 353–358. [Google Scholar] [CrossRef]
- Saleem, A.F.; Abbas, Q.; Haque, A. Use of N-acetylcysteine in children with fulminant hepatic failure caused by acute viral hepatitis. J. Coll. Physicians Surg. Pak. 2015, 25, 354. [Google Scholar] [PubMed]
- Parkas, A.; Asghar, M.; Haider, N. Non-acetaminophen induced acute liver failure of viral etiology: Treatment with and without N-acetylcysteine; comparing the length of hospital stay and survival status in children at the tertiary care hospital. Infect. Dis. J. Pak. 2016, 25, 11–14. [Google Scholar]
- Mumtaz, K.; Azam, Z.; Hamid, S.; Abid, S.; Memon, S.; Ali Shah, H.; Jafri, W. Role of N-acetylcysteine in adults with non-acetaminophen-induced acute liver failure in a center without the facility of liver transplantation. Hepatol. Int. 2009, 3, 563–570. [Google Scholar] [CrossRef]
- Gunduz, H.; Karabay, O.; Tamer, A.; Özaras, R.; Mert, A.; Tabak, Ö.F. N-acetyl cysteine therapy in acute viral hepatitis. World J. Gastroenterol. 2003, 9, 2698. [Google Scholar] [CrossRef] [PubMed]
- Dissanayake, D.M.D.I.B.; Gunaratne, W.M.S.N.; Kumarihamy, K.W.M.P.P.; Kularatne, S.A.M.; Kumarasiri, P.V.R. Use of intravenous N-acetylcysteine in acute severe hepatitis due to severe dengue infection: A case series. BMC Infect. Dis. 2021, 21, 978. [Google Scholar] [CrossRef]
- Katarey, D.; Verma, S. Drug-induced liver injury. Clin. Med. 2016, 16 (Suppl. S6), s104. [Google Scholar] [CrossRef]
- Chalasani, N.; Bonkovsky, H.L.; Fontana, R.; Lee, W.; Stolz, A.; Talwalkar, J.; Reddy, R.K.; Watkins, P.B.; Navarro, V.; Barnhart, H.; et al. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN prospective study. Gastroenterology 2015, 148, 1340–1352. [Google Scholar] [CrossRef]
- de Abajo, F.J.; Montero, D.; Madurga, M.; García Rodríguez, L.A. Acute and clinically relevant drug-induced liver injury: A population based case-control study. Br. J. Clin. Pharmacol. 2004, 58, 71–80. [Google Scholar] [CrossRef]
- Allameh, A.; Niayesh-Mehr, R.; Aliarab, A.; Sebastiani, G.; Pantopoulos, K. Oxidative stress in liver pathophysiology and disease. Antioxidants 2023, 12, 1653. [Google Scholar] [CrossRef] [PubMed]
- Villanueva-Paz, M.; Morán, L.; López-Alcántara, N.; Freixo, C.; Andrade, R.J.; Lucena, M.I.; Cubero, F.J. Oxidative stress in drug-induced liver injury (DILI): From mechanisms to biomarkers for use in clinical practice. Antioxidants 2021, 10, 390. [Google Scholar] [CrossRef]
- Yew, W.W.; Chang, K.C.; Chan, D.P. Oxidative stress and first-line antituberculosis drug-induced hepatotoxicity. Antimicrob. Agents Chemother. 2018, 62, 10–1128. [Google Scholar] [CrossRef]
- Bonkovsky, H.L.; Barnhart, H.X.; Foureau, D.M.; Steuerwald, N.; Lee, W.M.; Gu, J.; Fontana, R.J.; Hayashi, P.J.; Chalasani, N.; Navarro, V.M.; et al. Cytokine profiles in acute liver injury—Results from the US Drug-Induced Liver Injury Network (DILIN) and the Acute Liver Failure Study Group. PLoS ONE 2018, 13, e0206389. [Google Scholar] [CrossRef]
- Roth, R.A.; Maiuri, A.R.; Ganey, P.E. Idiosyncratic drug-induced liver injury: Is drug-cytokine interaction the linchpin? J. Pharmacol. Exp. Ther. 2017, 360, 368–377. [Google Scholar] [CrossRef]
- Baniasadi, S.; Eftekhari, P.; Tabarsi, P.; Fahimi, F.; Raoufy, M.R.; Masjedi, M.R.; Velayati, A.A. Protective effect of N-acetylcysteine on antituberculosis drug-induced hepatotoxicity. Eur. J. Gastroenterol. Hepatol. 2010, 22, 1235–1238. [Google Scholar] [CrossRef]
- Attri, S.; Rana, S.V.; Vaiphei, K.; Sodhi, C.P.; Katyal, R.; Goel, R.C.; Nain, C.K.; Singh, K. Isoniazid–and rifampicin–induced oxidative hepatic injury–protection by N–acetylcysteine. Hum. Exp. Toxicol. 2000, 19, 517–522. [Google Scholar] [CrossRef]
- Moosa, M.S.; Maartens, G.; Gunter, H.; Allie, S.; Chughlay, M.F.; Setshedi, M.; Wasserman, S.; Stead, D.F.; Hickman, N.; Stewart, A.; et al. A Randomized Controlled Trial of Intravenous N-Acetylcysteine in the Management of Anti-tuberculosis Drug–Induced Liver Injury. Clin. Infect. Dis. 2021, 73, e3377–e3383. [Google Scholar] [CrossRef]
- Eroglu, N.; Erduran, E.; Reis, G.P.; Bahadır, A. Therapeutic effect of N-acetylcysteine on chemotherapy-induced liver injury. Ir. J. Med. Sci. 2020, 189, 1189–1194. [Google Scholar] [CrossRef]
- Mudalel, M.L.; Dave, K.P.; Hummel, J.P.; Solga, S.F. N-acetylcysteine treats intravenous amiodarone induced liver injury. World J. Gastroenterol. 2015, 21, 2816. [Google Scholar] [CrossRef] [PubMed]
- Elliott, T.R.; Symes, T.; Kannourakis, G.; Angus, P. Resolution of norfloxacin-induced acute liver failure after N-acetylcysteine therapy: Further support for the use of NAC in drug-induced ALF? Case Rep. 2016, 2016, bcr2015213189. [Google Scholar]
- El Rahi, C.; Thompson-Moore, N.; Mejia, P.; De Hoyos, P. Successful use of N-Acetylcysteine to treat severe hepatic injury caused by a dietary fitness supplement. Pharmacotherapy 2015, 35, e96–e101. [Google Scholar] [CrossRef]
- Chughlay, M.F.; Kramer, N.; Spearman, C.W.; Werfalli, M.; Cohen, K. N-acetylcysteine for non-paracetamol drug-induced liver injury: A systematic review. Br. J. Clin. Pharmacol. 2016, 81, 1021–1029. [Google Scholar] [CrossRef]
- Sanabria-Cabrera, J.; Tabbai, S.; Niu, H.; Alvarez-Alvarez, I.; Licata, A.; Björnsson, E.; Andrade, R.J.; Lucena, M.I. N-acetylcysteine for the management of non-acetaminophen drug-induced liver injury in adults: A systematic review. Front. Pharmacol. 2022, 13, 876868. [Google Scholar] [CrossRef]
- Shrestha, D.B.; Budhathoki, P.; Sedhai, Y.R.; Adhikari, A.; Poudel, A.; Aryal, B.; Baniya, R. N-acetyl cysteine versus standard of care for non-acetaminophen induced acute liver injury: A systematic review and meta-analysis. Ann. Hepatol. 2021, 24, 100340. [Google Scholar] [CrossRef]
- Bacak, S.J.; Thornburg, L.L. Liver failure in pregnancy. Crit. Care Clin. 2016, 32, 61–72. [Google Scholar] [CrossRef]
- Casey, L.C.; Fontana, R.J.; Aday, A.; Nelson, D.B.; Rule, J.A.; Gottfried, M.; Tran, M.; Lee, W.M.; Acute Liver Failure Study Group. Acute liver failure (ALF) in pregnancy: How much is pregnancy related? Hepatology 2020, 72, 1366–1377. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Sikachi, R.R.; Gerasimov, M.; Aronsohn, J.; Palleschi, G. Acute fatty liver of pregnancy leading to a delayed hepatic failure necessitating liver transplantation: A case report. J. Obstet. Anaesth. Crit. Care 2021, 11, 124–126. [Google Scholar] [CrossRef]
- Morris, R.; Spencer, S.K.; Barnes, A.; Bowles, T.; Kyle, P.B.; Wallace, K. Attenuation of oxidative stress and hypertension in an animal model of HELLP syndrome. Eur. J. Pharmacol. 2018, 834, 136–141. [Google Scholar] [CrossRef]
- Petca, A.; Miron, B.C.; Pacu, I.; Dumitrașcu, M.C.; Mehedințu, C.; Șandru, F.; Petca, R.C.; Rotar, I.C. HELLP syndrome—Holistic insight into pathophysiology. Medicina 2022, 58, 326. [Google Scholar] [CrossRef]
- Torrance, H.L.; Krediet, T.G.; Vreman, H.J.; Visser, G.H.; Van Bel, F. Oxidative stress and proinflammatory cytokine levels are increased in premature neonates of preeclamptic mothers with HELLP syndrome. Neonatology 2008, 94, 138–142. [Google Scholar] [CrossRef]
- Menteşe, A.; Güven, S.; Demir, S.; Sumer, A.; Yaman, S.; Alver, A.; Sönmez, M.; Karahan, S. Circulating parameters of oxidative stress and hypoxia in normal pregnancy and HELLP syndrome. Adv. Clin. Exp. Med. 2018, 27, 1567–1572. [Google Scholar] [CrossRef]
- Shabani, S.; Baghbahadorani, F.K.; Jazaeri, F.; Ganji, F.; Mortazavi, N.S.; Mahmoudnia, L. The Effects of Silymarin and N-Acetylcysteine on Liver and Kidney Dysfunction in Subjects with Severe Pre-eclampsia. J. Iran. Med. Counc. 2021, 4, 173–182. [Google Scholar] [CrossRef]
- Roes, E.M.; Raijmakers, M.T.; de Boo, T.M.; Zusterzeel, P.L.; Merkus, H.M.; Peters, W.H.; Steegers, E.A. Oral N-acetylcysteine administration does not stabilize the process of established severe preeclampsia. Obstet. Gynecol. Surv. 2006, 61, 757–758. [Google Scholar] [CrossRef]
- Lee, W.M.; Hynan, L.S.; Rossaro, L.; Fontana, R.J.; Stravitz, R.T.; Larson, A.M.; Davern, T.J.; Murray, N.G.; McCashland, T.; Reisch, J.S.; et al. Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Gastroenterology 2009, 137, 856–864. [Google Scholar] [CrossRef]
- Darweesh, S.K.; Ibrahim, M.F.; El-Tahawy, M.A. Effect of N-acetylcysteine on mortality and liver transplantation rate in non-acetaminophen-induced acute liver failure: A multicenter study. Clin. Drug Investig. 2017, 37, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Nabi, T.; Nabi, S.; Rafiq, N.; Shah, A. Role of N-acetylcysteine treatment in non-acetaminophen-induced acute liver failure: A prospective study. Saudi J. Gastroenterol. 2017, 23, 169. [Google Scholar] [CrossRef]
- Hu, J.; Zhang, Q.; Ren, X.; Sun, Z.; Quan, Q. Efficacy and safety of acetylcysteine in “non-acetaminophen” acute liver failure: A meta-analysis of prospective clinical trials. Clin. Res. Hepatol. Gastroenterol. 2015, 39, 594–599. [Google Scholar] [CrossRef]
- Walayat, S.; Shoaib, H.; Asghar, M.; Kim, M.; Dhillon, S. Role of N-acetylcysteine in non-acetaminophen-related acute liver failure: An updated meta-analysis and systematic review. Ann. Gastroenterol. 2021, 34, 235. [Google Scholar] [CrossRef]
| Author, Year | Type of Study | Number of Cases | Age of Participants (Years) | Dose of NAC | Co-Treatment/ Comparator | Observed Effects | Mortality |
|---|---|---|---|---|---|---|---|
| Mushroom poisoning (Amanita phalloides) | |||||||
| Locatelli C. et al., 1992 [27] | Case series | 73 | 2–84 | 150 mg/kg bolus, followed by 50 mg/kg at 4 h intervals for 3–18 days | Forced diuresis |
| 8% |
| Schneider S. et al., 1992 [33] | Experimental animal model | NA | NA | 1.2 g/kg | None |
| NA |
| Locatelli C. et al., 2010 [36] | Cohort of patients | 157 | Mean: 52 | 150 mg/kg followed by 300 mg/kg/day until 48 h | Forced diuresis, activated charcoal |
| 2.5% |
| Ahishali E. et al., 2012 [37] | Cohort of patients | 77 | Mean: 42 | 210 mg/kg/day for 3–5 days | Activated charcoal, Penicillin G, Sylibin, hemofiltration |
| 2.6% |
| Akin A. et al., 2013 [38] | Case–control | 40 patients: 24 in the NAC group vs. 16 in the control group | NAC: mean 32 Control: mean 34 | 12 g/day in four divided doses | Standard medical care |
| 4.4% in the NAC group vs. 18.7% in the control group |
| Tan J. et al., 2022 [41] | Review of 133 studies | 877 cases | NA | variable | NR |
| NR |
| Viral hepatitis | |||||||
| Parkas A. et al., 2016 [53] | Cohort of patients | 32 patients: 12 receiving NAC and 12 control | NAC: mean 7.2 Control: mean 7.3 | 100 mg/kg/day | Standard medical care |
| 44% in NAC group vs. 69% in control group |
| Gunduz H. et al., 2003 [55] | Randomized control trial | 41 patients with VHA or VHB ALF | 15–52 | 200 mg orally, three times per day | Standard medical care |
| NR |
| Dissanayake D. et al., 2021 [56] | Case series | 30 patients with dengue fever and severe hepatitis | Mean: 49.9 | 100 mg/h for 3–5 days | Standard medical care |
| 3.3% |
| Drug-induced liver injury | |||||||
| Moosa M. et al., 2020 [67] | Randomized control trial | 53 patients with tuberculostatic-induced liver injury | NAC: mean 37 Placebo: mean 38 | 150 mg/kg over 1 h, 50 mg/kg over 4 h, and 100 mg/kg over 16 h | NR |
| 14% |
| Eroglu N. et al., 2020 [68] | Case–control | 102 pediatric patients with chemotherapy-induced hepatotoxicity: 70 received NAC | 2–17 in both groups | 3 μg/kg in a 24 h infusion | NR |
| NR |
| Chughlay M. et al., 2016 [72] | Meta-analysis | 45 patients: 19 in NAC group vs. 27 controls | NR | 150 mg/kg/h over 1 h, then 12.5 mg/kg/h for 4 h, then 6.25 mg/kg/h for 67 h | NR |
| 21% in NAC group vs. 35% in controls |
| Sanabria-Cabrera J. et al., 2022 [73] | Systematic review | 11 studies | NR (≥18) | Varying in different studies | NR |
| NR |
| Shrestha D. et al., 2021 [74] | Meta-analysis | 11 studies: 565 patients in the NAC group vs. 552 in the control group | NR | Varying in different studies | standard of care |
| 23.7% in NAC group vs. 35.1% in control group |
| Pregnancy-related ALF | |||||||
| Shabani S. et al., 2021 [82] | Randomized control trial | 60 patients with severe pre-eclampsia | Mean: 26 | 600 mg at 0, 12, and 24 h after delivery | 70 mg of silymarin |
| NR |
| Roes E. et al., 2006 [83] | Randomized control trial | 38 patients with severe pre-eclampsia and/or HELLP | NAC: 22–34 Control: 23–40 | 1800 mg every 8h | placebo |
| NR |
| Pooled analysis (all etiologies) | |||||||
| Lee W. et al., 2009 [84] | Randomized control trial | 81 patients in the NAC group vs. 92 patients in the placebo group | NAC: 17–69 Control: 18–71 | 150 mg/kg/h for 1 h, followed by 12.5 mg/kg/h for 4 h and 6.25 mg/kg/h for 67 h | placebo |
| 30% in NAC group vs. 34% in control group |
| Mumtaz K. et al., 2009 [54] | Prospective study | 47 patients in NAC group vs. 44 patients in historical cohort | NAC: 27 Control: 37 | 140 mg/kg orally, followed by 70 mg/kg at 4 h intervals for a total of 17 doses | Standard of care |
| 53.2% in NAC group vs. 72.7% in historical cohort |
| Darweesh S. et al., 2017 [85] | Randomized control trial | 85 patients in the NAC group vs. 70 patients in the control group | NAC: 33 Placebo: 34 | 150 mg/kg for 1/2 h, followed by 70 mg/kg for 4 h, then 70 mg/kg for 16 h, and 150 mg/kg/day afterward | placebo |
| 3.3% in treatment group vs. 23.3% in control group |
| Hu J. et al., 2015 [87] | Meta-analysis | 4 studies: 331 patients in the NAC group vs. 285 patients in the control group | NR (adults and children) | orally or intravenously, in different doses | NR |
| 29.0% in treatment group vs. 33.0% in control group |
| Walayat S. et al., 2021 [88] | Meta-analysis | 7 studies: 472 patients in the NAC group vs. 411 in the control group | NAC: 21 Control: 26 | orally or intravenously, in different doses | NR |
| 23.7% in treatment group vs. 35.7% in control group |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popescu, M.; Bratu, A.; Agapie, M.; Borjog, T.; Jafal, M.; Sima, R.-M.; Orban, C. The Use and Potential Benefits of N-Acetylcysteine in Non-Acetaminophen Acute Liver Failure: An Etiology-Based Review. Biomedicines 2024, 12, 676. https://doi.org/10.3390/biomedicines12030676
Popescu M, Bratu A, Agapie M, Borjog T, Jafal M, Sima R-M, Orban C. The Use and Potential Benefits of N-Acetylcysteine in Non-Acetaminophen Acute Liver Failure: An Etiology-Based Review. Biomedicines. 2024; 12(3):676. https://doi.org/10.3390/biomedicines12030676
Chicago/Turabian StylePopescu, Mihai, Angelica Bratu, Mihaela Agapie, Tudor Borjog, Mugurel Jafal, Romina-Marina Sima, and Carmen Orban. 2024. "The Use and Potential Benefits of N-Acetylcysteine in Non-Acetaminophen Acute Liver Failure: An Etiology-Based Review" Biomedicines 12, no. 3: 676. https://doi.org/10.3390/biomedicines12030676
APA StylePopescu, M., Bratu, A., Agapie, M., Borjog, T., Jafal, M., Sima, R.-M., & Orban, C. (2024). The Use and Potential Benefits of N-Acetylcysteine in Non-Acetaminophen Acute Liver Failure: An Etiology-Based Review. Biomedicines, 12(3), 676. https://doi.org/10.3390/biomedicines12030676





