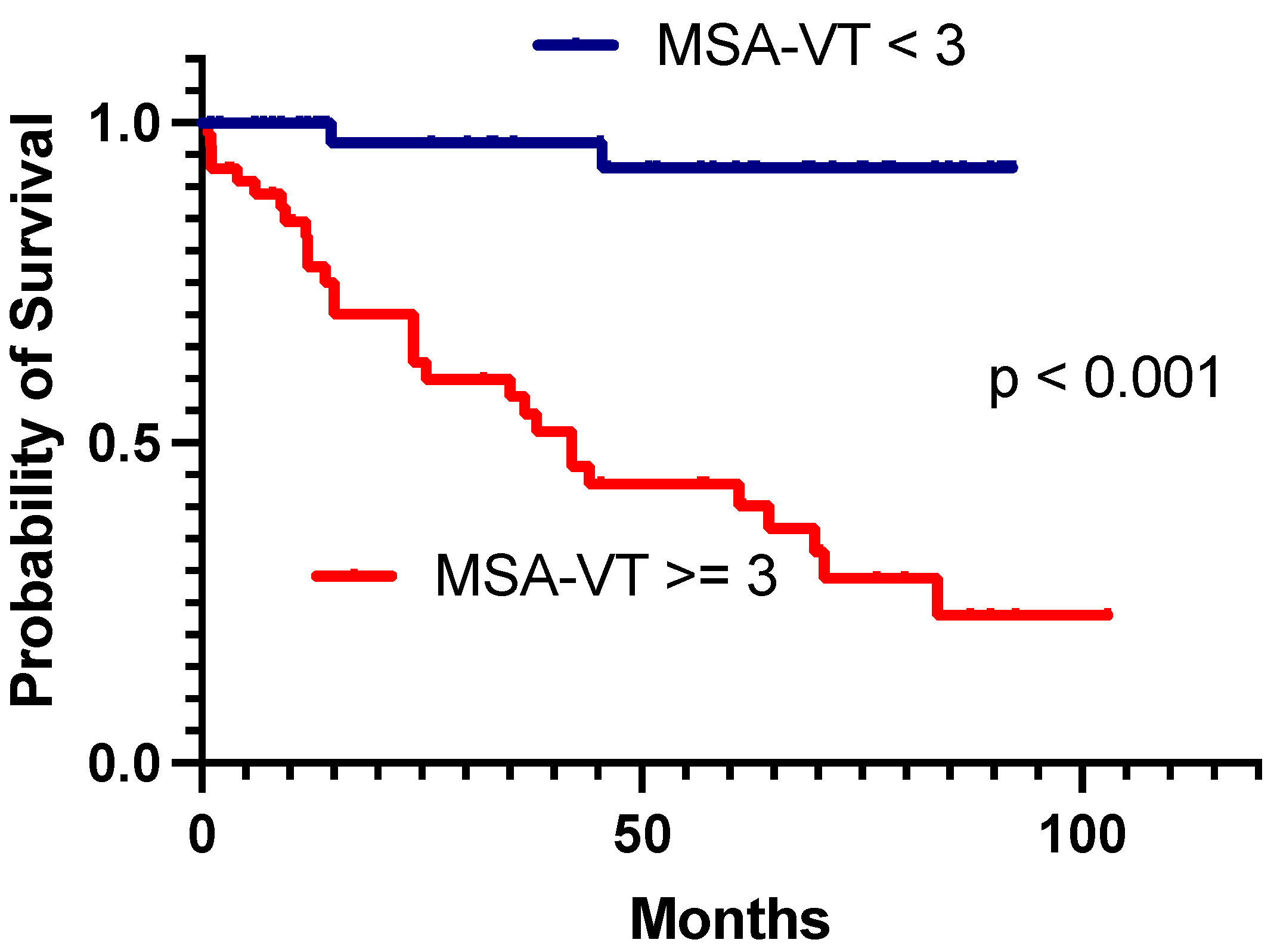
MSA-VT Score for Assessment of Long-Term Prognosis after Electrical Storm Ablation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
- -
- -
- Treated by radiofrequency catheter ablation (RFCA) targeting ventricular arrhythmic substrate from January 2014 to December 2022.
2.2. Imaging, Electrophysiology Study and Ablation Strategy
2.3. Follow-Up Protocol
2.4. Endpoints
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. MSA-VT to Predict Death and Recurrences in Comparison with Previous Scoring Algorithms
4.2. MSA-VT Risk Factors’ Effect on Long-Term Outcomes
5. Limitations
- This analysis is based on a relatively small-scale sample of 101 patients. Previous studies that assessed the role of scoring algorithms analyzed samples ranging from approximately 175–193 patients (MORTALITIES-VA and PAINESD scores) up to 1251–1417 patients (I-VT and RIVA scores). However, all of these studies included VT patients treated by ablation (and not exclusively ES).
- The findings of this study are based on a single-center population analysis. External validation of the newly proposed scoring algorithm (MSA-VT) on larger samples from distinct ablation centers is required. Internal validation was based on selection of a randomized sub-sample of 75% of the initial cohort and showed higher values of AUC compared to previously mentioned scores.
- No mechanical circulatory support (MCS) was available during this study. This is a significant difference in protocol compared to previously published experience, (in particular, the PAINESD study). However, most patients were previously stabilized (thus optimized in terms of HF) and subsequently ablated (predominantly by substrate ablation during sinus rhythm).
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dinov, B.; Darma, A.; Nedios, S.; Hindricks, G. Management of patients with electrical storm: An educational review. Eur. Heart J. Acute Cardiovasc. Care 2023, 12, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, A.A.; Szili-torok, T. Editor’s Choice-The treatment of electrical storm: An educational review. Eur. Heart J. Acute Cardiovasc. Care 2018, 7, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Hohnloser, S.H.; Al-Khalidi, H.R.; Pratt, C.M.; Brum, J.M.; Tatla, D.S.; Tchou, P.; Dorian, P. Electrical storm in patients with an implantable defibrillator: Incidence, features, and preventive therapy: Insights from a randomized trial. Eur. Heart J. 2006, 27, 3027–3032. [Google Scholar] [CrossRef]
- Darma, A.; Bertagnolli, L.; Dinov, B.; Torri, F.; Shamloo, A.S.; Lurz, J.A.; Dagres, N.; Husser-Bollmann, D.; Bollmann, A.; Hindricks, G.; et al. Predictors of long-term mortality after catheter ablation of ventricular tachycardia in a contemporary cohort of patients with structural heart disease. EP Eur. 2020, 22, 1672–1679. [Google Scholar] [CrossRef] [PubMed]
- Ninni, S.; Layec, J.; Brigadeau, F.; Behal, H.; Labreuche, J.; Klein, C.; Schurtz, G.; Potelle, C.; Coisne, A.; Lemesle, G.; et al. Incidence and predictors of mortality after an electrical storm in the ICU. Eur. Heart J. Acute Cardiovasc. Care 2022, 11, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Guerra, F.; Shkoza, M.; Scappini, L.; Flori, M.; Capucci, A. Role of electrical storm as a mortality and morbidity risk factor and its clinical predictors: A meta-analysis. EP Eur. 2014, 16, 347–353. [Google Scholar] [CrossRef]
- Zeppenfeld, K.; Tfelt-Hansen, J.; de Riva, M.; Winkel, B.G.; Behr, E.R.; Blom, N.A.; Charron, P.; Corrado, D.; Dagres, N.; de Chillou, C.; et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Developed by the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC) Endorsed by the Association for European Paediatric and Congenital Cardiology (AEPC). Eur. Heart J. 2022, 43, 3997–4126. [Google Scholar] [CrossRef]
- Carbucicchio, C.; Santamaria, M.; Trevisi, N.; Maccabelli, G.; Giraldi, F.; Fassini, G.; Riva, S.; Moltrasio, M.; Cireddu, M.; Veglia, F.; et al. Catheter Ablation for the Treatment of Electrical Storm in Patients with Implantable Cardioverter-Defibrillators. Circulation 2008, 117, 462–469. [Google Scholar] [CrossRef]
- Laredo, M.; Da Silva, L.O.; Extramiana, F.; Lellouche, N.; Varlet, É.; Amet, D.; Algalarrondo, V.; Waintraub, X.; Duthoit, G.; Badenco, N.; et al. Catheter ablation of electrical storm in patients with arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm 2019, 17, 41–48. [Google Scholar] [CrossRef]
- Muser, D.; Liang, J.J.; Pathak, R.K.; Magnani, S.; Castro, S.A.; Hayashi, T.; Garcia, F.C.; Supple, G.E.; Riley, M.P.; Lin, D.; et al. Long-Term Outcomes of Catheter Ablation of Electrical Storm in Nonischemic Dilated Cardiomyopathy Compared with Ischemic Cardiomyopathy. JACC Clin. Electrophysiol. 2017, 3, 767–778. [Google Scholar] [CrossRef]
- Vergara, P.; Tung, R.; Vaseghi, M.; Brombin, C.; Frankel, D.; Biase, D.; Nagashima, K.; Tedrow, U.; Tzou, W.S.; Sauer, W.H.; et al. Successful ventricular tachycardia ablation in patients with electrical storm reduces recurrences and improves survival. Heart Rhythm 2017, 15, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Deneke, T.; Lemke, B.; Mügge, A.; Shin, D.-I.; Grewe, P.H.; Horlitz, M.; Balta, O.; Bösche, L.; Lawo, T. Catheter ablation of electrical storm. Expert Rev. Cardiovasc. Ther. 2016, 9, 1051–1058. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Z.; Tan, M.-C.; Karikalan, S.; Deshmukh, A.J.; Srivathsan, K.; Shen, W.K.; El-Masry, H.; Scott, L.; Asirvatham, S.J.; Cha, Y.-M.; et al. Causes of Early Mortality After Ventricular Tachycardia Ablation in Patients with Reduced Ejection Fraction. JACC Clin. Electrophysiol. 2023, 9, 824–832. [Google Scholar] [CrossRef] [PubMed]
- Tilz, R.R.; Lin, T.; Eckardt, L.; Deneke, T.; Andresen, D.; Wieneke, H.; Brachmann, J.; Kääb, S.; Chun, K.R.J.; Münkler, P.; et al. Ablation Outcomes and Predictors of Mortality Following Catheter Ablation for Ventricular Tachycardia: Data from the German Multicenter Ablation Registry. J. Am. Heart Assoc. 2023, 7, e007045. [Google Scholar] [CrossRef] [PubMed]
- Muser, D.; Liang, J.J.; Castro, S.A.; Hayashi, T.; Enriquez, A.; Troutman, G.S.; McNaughton, N.W.; Supple, G.; Birati, E.Y.; Schaller, R.; et al. Outcomes with prophylactic use of percutaneous left ventricular assist devices in high-risk patients undergoing catheter ablation of scar-related ventricular tachycardia: A propensity-score matched analysis. Heart Rhythm 2018, 15, 1500–1506. [Google Scholar] [CrossRef] [PubMed]
- Vergara, P.; Tzou, W.S.; Tung, R.; Brombin, C.; Nonis, A.; Vaseghi, M.; Frankel, D.S.; Di Biase, L.; Tedrow, U.; Mathuria, N.; et al. Predictive Score for Identifying Survival and Recurrence Risk Profiles in Patients Undergoing Ventricular Tachycardia Ablation. Circ. Arrhythmia Electrophysiol. 2018, 11, e006730. [Google Scholar] [CrossRef] [PubMed]
- Mathew, S.; Fink, T.; Feickert, S.; Inaba, O.; Hashiguchi, N.; Schlüter, M.; Wohlmuth, P.; Wissner, E.; Tilz, R.R.; Heeger, C.-H.; et al. Complications and mortality after catheter ablation of ventricular arrhythmias: Risk in VT ablation (RIVA) score. Clin. Res. Cardiol. Off. J. Ger. Card. Soc. 2022, 111, 530–540. [Google Scholar] [CrossRef]
- Bennett, R.G.; Garikapati, K.; Campbell, T.G.; Kotake, Y.; Turnbull, S.; Bhaskaran, A.; De Silva, K.; Kanawati, J.; Zhou, J.; Wong, M.S.; et al. Mortality after catheter ablation of structural heart disease related ventricular tachycardia. Int. J. Cardiol. 2023, 386, 50–58. [Google Scholar] [CrossRef]
- Vătășescu, R.; Cojocaru, C.; Năstasă, A.; Popescu, S.; Iorgulescu, C.; Bogdan, Ș.; Gondoș, V.; Berruezo, A. Monomorphic VT Non-Inducibility after Electrical Storm Ablation Reduces Mortality and Recurrences. J. Clin. Med. 2022, 11, 3887. [Google Scholar] [CrossRef]
- Cojocaru, C.; Nastasa, A.; Bogdan, S.; Iorgulescu, C.; Deaconu, A.; Onciul, S.; Vatasescu, R. Non-revascularized chronic total occlusions impact on substrate and post-ablation results in drug-refractory electrical storm. Front. Cardiovasc. Med. 2023, 10, 1258373. [Google Scholar] [CrossRef]
- Könemann, H.; Dagres, N.; Merino, J.L.; Sticherling, C.; Zeppenfeld, K.; Tfelt-Hansen, J.; Eckardt, L. Spotlight on the 2022 ESC guideline management of ventricular arrhythmias and prevention of sudden cardiac death: 10 novel key aspects. EP Eur. 2023, 25, euad091. [Google Scholar] [CrossRef] [PubMed]
- Baldi, E.; Conte, G.; Zeppenfeld, K.; Lenarczyk, R.; Guerra, J.M.; Farkowski, M.M.; de Asmundis, C.; Boveda, S. Contemporary management of ventricular electrical storm in Europe: Results of a European Heart Rhythm Association Survey. EP Eur. 2023, 25, 1277–1283. [Google Scholar] [CrossRef] [PubMed]
- Kowlgi, G.N.; Cha, Y.-M. Management of ventricular electrical storm: A contemporary appraisal. EP Eur. 2020, 22, 1768–1780. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. Off. Publ. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef] [PubMed]
- Berruezo, A.; Fernández-Armenta, J.; Andreu, D.; Penela, D.; Herczku, C.; Evertz, R.; Cipolletta, L.; Acosta, J.; Borràs, R.; Arbelo, E.; et al. Scar dechanneling: New method for scar-related left ventricular tachycardia substrate ablation. Circ. Arrhythmia Electrophysiol. 2015, 8, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Deyell, M.W.; Doucette, S.; Parkash, R.; Nault, I.; Gula, L.; Gray, C.; Gardner, M.; Sterns, L.D.; Healey, J.S.; Essebag, V.; et al. Ventricular tachycardia characteristics and outcomes with catheter ablation vs. antiarrhythmic therapy: Insights from the VANISH trial. EP Eur. 2022, 24, 1112–1118. [Google Scholar] [CrossRef] [PubMed]
- Muser, D.; Castro, S.A.; Liang, J.J.; Santangeli, P. Identifying Risk and Management of Acute Haemodynamic Decompensation During Catheter Ablation of Ventricular Tachycardia. Arrhythmia Electrophysiol. Rev. 2018, 7, 282–287. [Google Scholar] [CrossRef]
- Doldi, F.; Doldi, P.M.; Plagwitz, L.; Westerwinter, M.; Wolfes, J.; Korthals, D.; Willy, K.; Wegner, F.K.; Könemann, H.; Ellermann, C.; et al. Predictors for major in-hospital complications after catheter ablation of ventricular arrhythmias: Validation and modification of the Risk in Ventricular Ablation (RIVA) Score. Clin. Res. Cardiol. Off. J. Ger. Card. Soc. 2023, 112, 1778–1789. [Google Scholar] [CrossRef]
- Jiménez Candil, J.; Castro, J.C.; Hernández, J.; Fernández-Portales, J.; Durán, M.; Durán, O.; Pérez, J.; Elices, J.; Moríñigo, J.L.; Martín, F.; et al. Timing of Ablation and Prognosis of Patients with Electrical Storm and Scar-Related Left Ventricular Dysfunction. Am. J. Cardiol. 2020, 136, 87–93. [Google Scholar] [CrossRef]
- Jin, Q.; Jacobsen, P.K.; Pehrson, S.; Chen, X. Prediction and prognosis of ventricular tachycardia recurrence after catheter ablation with remote magnetic navigation for electrical storm in patients with ischemic cardiomyopathy. Clin. Cardiol. 2017, 40, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.M.; Silverio Antonio, P.; Couto Pereira, S.; Brito, J.; Valente Silva, B.; Alves Da Silva, P.; Garcia, A.B.; Simoes De Oliveira, C.; Nunes Ferreira, A.; Lima Da Silva, G.; et al. Is it possible to predict mortality and recurrence of VT after ablation? PAINESD risk score applicability vs new predictors. EP Eur. 2022, 24 (Suppl. 1), euac053.089. [Google Scholar] [CrossRef]
- Kulchetscki, R.M.; Pisani, C.F.; Alexandre, F.K.B.; Mayrink, M.P.; Ferraz, A.P.; Gouvea, F.C.; Goncalves, A.L.M.; Hardy, C.A.; Melo, S.L.; Chokr, M.O.; et al. Applicability of the PAINESD risk score for 30-day mortality prediction post ventricular tachycardia catheter ablation in Chagas disease. J. Interv. Card. Electrophysiol. Int. J. Arrhythm. Pacing 2021, 62, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Parker, J.; Hedley, J.; Incognito, C.; Gangidi, S.; Wazni, O.M.; Rickard, J. B-AB15-04 PAINESD RISK SCORE AS A PREDICTOR OF OUTCOMES IN ELECTRICAL STORM. Heart Rhythm 2021, 18, S30. [Google Scholar] [CrossRef]
- Fernandez-Armenta, J.; Soto-Iglesias, D.; Silva, E.; Penela, D.; Jáuregui, B.; Linhart, M.; Bisbal, F.; Acosta, J.; Fernandez, M.; Borras, R.; et al. Safety and Outcomes of Ventricular Tachycardia Substrate Ablation During Sinus Rhythm. JACC Clin. Electrophysiol. 2020, 6, 1435–1448. [Google Scholar] [CrossRef] [PubMed]
- Tzou, W.S.; Tung, R.; Frankel, D.S.; Vaseghi, M.; Bunch, T.J.; Di Biase, L.; Tholakanahalli, V.N.; Lakkireddy, D.; Dickfeld, T.; Saliaris, A.; et al. Ventricular Tachycardia Ablation in Severe Heart Failure. Circ. Arrhythmia Electrophysiol. 2017, 10, e004494. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, U.; Dherange, P.; Reddy, R.; DeVillier, J.; Chong, J.; Ihsan, A.; Jones, R.; Duddyala, N.; Reddy, P.; Dominic, P. Atrial Fibrillation Is Associated with Higher Overall Mortality in Patients with Implantable Cardioverter-Defibrillator: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2018, 7, e010156. [Google Scholar] [CrossRef]
- Stein, K.M.; Euler, D.E.; Mehra, R.; Seidl, K.; Slotwiner, D.J.; Mittal, S.; Markowitz, S.M.; Lerman, B.B. Do atrial tachyarrhythmias beget ventricular tachyarrhythmias in defibrillator recipients? J. Am. Coll. Cardiol. 2002, 40, 335–340. [Google Scholar] [CrossRef]
- Santangeli, P.; Rame, J.E.; Birati, E.Y.; Marchlinski, F.E. Management of Ventricular Arrhythmias in Patients with Advanced Heart Failure. J. Am. Coll. Cardiol. 2017, 69, 1842–1860. [Google Scholar] [CrossRef]
- Benito-González, T.; Estévez-Loureiro, R.; Garrote-Coloma, C.; Arellano-Serrano, C.; Tundidor-Sanz, E.; Fernández-Lozano, I.; Toquero, J.; Pérez de Prado, A.; Goicolea, J.; Fernández-Vázquez, F. Effect of Successful Edge-to-Edge Mitral Valve Repair on Ventricular Arrhythmic Burden in Patients with Functional Mitral Regurgitation and Implantable Cardiac Devices. Am. J. Cardiol. 2019, 124, 1113–1119. [Google Scholar] [CrossRef]
- Benito Gonzalez, T.; Freixa, X.; Godino, C.; Taramasso, M.; Estevez-Loureiro, R.; Pascual, I.; Serrador, A.; Nombela, L.; Grande, D.; Cruz, I.; et al. Ventricular arrhythmias in patients with functional mitral regurgitation and implantable cardiac devices: Implications of mitral valve repair with Mitraclip. Eur. Heart J. 2020, 41 (Suppl. 2), ehaa946.2636. [Google Scholar] [CrossRef]
- Geis, N.A.; Göbbel, A.; Kreusser, M.M.; Täger, T.; Katus, H.A.; Frey, N.; Schlegel, P.; Raake, P.W. Impact of Percutaneous Mitral Valve Repair Using the MitraClipTM System on Ventricular Arrhythmias and ICD Therapies. Life 2022, 12, 344. [Google Scholar] [CrossRef]
- Ledwoch, J.; Nommensen, A.; Keelani, A.; Meyer-Saraei, R.; Stiermaier, T.; Saad, M.; Pöss, J.; Desch, S.; Tilz, R.; Thiele, H.; et al. Impact of transcatheter mitral valve repair on ventricular arrhythmias. EP Eur. 2019, 21, 1385–1391. [Google Scholar] [CrossRef]

| Overall | Ischemic Cardiomyopathy (67.3% (n = 68)) | Non-Ischemic Cardiomyopathy (32.7% (n = 33)) | p | |
|---|---|---|---|---|
| Males, % (n) | 86.1% (n = 87) | 86.8% (n = 59) | 84.8% (n = 28) | 0.76 |
| Age, mean (SD) | 59.6 ± 12.8 | 62.4 ± 11.1 | 54 ± 14.4 | 0.002 |
| BMI ≥ 25 kg/sqm, % (n) | 34.7% (n = 35) | 35.3% (n = 24) | 33.3 (n = 11) | 0.99 |
| COPD, % (n) | 8.9% (n = 9) | 7.4% (n = 5) | 12.1% (n = 4) | 0.46 |
| T2DM, % (n) | 62.4% (n = 63) | 30.9% (n = 21) | 15.2% (n = 5) | 0.14 |
| Hypertension, % (n) | 62.4% (n = 63) | 73.5% (n = 50) | 39.4% (n = 13) | 0.002 |
| Dyslipidemia, % (n) | 61.4% (n = 62) | 75% (n = 51) | 33.3% (n = 11) | <0.001 |
| Smoker, % (n) | 18.8% (n = 19) | 25% (n = 17) | 6.1% (n = 2) | 0.02 |
| CKD, % (n) | 18.8% (n = 19) | 26.5% (n = 18) | 3% (n = 1) | 0.005 |
| Previous CRT, % (n) | 14.9% (n = 15) | 11.8% (n = 8) | 21.2% (n = 7) | 0.24 |
| BB prior to ES | 82% (n = 83) | 80.% (n = 55) | 84.8% (n = 28) | 0.78 |
| BB after ES ablation | 86.1% (n = 87) | 85.3% (n = 58) | 87.9% (n = 29) | 0.99 |
| Amiodarone prior to ES | 68.3% (n = 69) | 61.8% (n = 42) | 78.8% (n = 26) | 0.11 |
| Amiodarone after ES ablation | 71.3% (n = 72) | 66.2% (n = 45) | 81.8% (n = 27) | 0.15 |
| Weeks from ES to ablation | 1.76 ± 2.85 | 1.8 ± 2.6 | 1.6 ± 3.2 | 0.85 |
| Number of ICD therapies, mean (SD) | 14.12 ± 23.66 | 12.7 ± 16.5 | 16.5 ± 32.9 | 0.59 |
| Admission creatinine, mean (SD) | 1.11 ± 0.59 | 1.16 ± 0.7 | 1.02 ± 0.2 | 0.27 |
| AF at admission, % (n) | 12.9% (n = 13) | 13.2% (n = 9) | 12.1% (n = 4) | 0.99 |
| History of AF, % (n) | 39.6% (n = 40) | 35.3% (n = 24) | 48.5% (n = 16) | 0.27 |
| LVEF, mean (SD) | 32% ± 11.6 | 31.5 ± 10.8 | 33 ± 13.4 | 0.55 |
| Moderate/severe MR, % (n) | 32.7% (n = 33) | 35.3% (n = 24) | 27.3% (n = 9) | 0.5 |
| NYHA III-IV at admission, % (n) | 28.7% (n= 29) | 26.5% (n = 18) | 33.3% (n = 11) | 0.49 |
| PAINESD score, mean (SD) | 14.5 ± 6.11 | 16.8 ± 5 | 9.9 ± 5.5 | <0.001 |
| Postprocedural I-VT risk score for death, mean (SD) | 1.1 ± 1.6 | 1.04 ± 1.49 | 1.24 ± 1.83 | 0.56 |
| RIVA score, mean (SD) | 12.3 ± 4.7 | 12.6 ± 4.6 | 11.6 ± 5 | 0.3 |
| MSA-VT score, mean (SD) | 4.26 ± 4.24 | 4.13 ± 3.96 | 4.54 ± 4.82 | 0.64 |
| Overall | Ischemic Cardiomyopathy (67.3% (n = 68)) | Non-Ischemic Cardiomyopathy (32.7% (n = 33)) | p | |
|---|---|---|---|---|
| Previous ablation procedures, % (n) | 31.7% (n = 32) | 27.9% (n = 19) | 39.4% (n = 13) | 0.26 |
| Substrate mapping & ablation, % (n) | 94.9% (n = 93) | 97% (n = 65) | 90.3% (n = 28) | 0.32 |
| Activation mapping, % (n) | 61.4% (n = 62) | 54.4% (n = 37) | 75.8% (n = 25) | 0.05 |
| Number of SMVTs induced during the procedure mean (SD) | 2.26 ± 0.1 | 2.16 ± 2.1 | 2.45 ± 1.65 | 0.52 |
| Remote magnetic navigation mapping & ablation, % (n) | 78.2% (n = 79) | 77.9% (n = 53) | 78.8% (n = 26) | 0.99 |
| Endocardial + epicardial ablation, % (n) | 20.8% (n = 21) | 8.8% (n = 6) | 45.5% (n = 15) | <0.001 |
| Ablation type—acute, % (n) | 5% (n = 5) | 5.9% (n = 4) | 3% (n = 1) | 0.69 |
| Ablation type—stabilized, % (n) | 80.2% (n = 81) | 77.9% (n = 53) | 84.8% (n = 28) | |
| Ablation type—elective, % (n) | 14.9% (n = 15) | 16.2% (n = 11) | 12.1% (n = 4) | |
| 4-ESx PES, % (n) | 66.3% (n = 67) | 69.7% (n = 47) | 60.6% (n = 20) | 0.37 |
| Endocardial mapping points (median, IQR) | 1900 (1100–2455) | 1983 (1310.5–2546.5) | 1750 (589.75–2165.2) | 0.11 |
| Ablation points, (IQR) | 37 (22–57) | 47.5 (28–61) | 27 (16–42) | 0.001 |
| Multielectrode catheter mapping, % (n) | 27% (n = 26.7) | 26.4% (n = 18) | 27.3% (n = 9) | 0.99 |
| Residual SMVT inducible at PES after ablation, % (n) | 31.7% (n = 32) | 27.9% (n = 19) | 39.4% (n = 13) | 0.26 |
| Days of hospitalization, mean (SD) | 10 ± 9.9 | 8.1 ± 6.9 | 14 ± 13.6 | 0.028 |
| All-cause mortality during follow-up, % (n) | 30.7% (n = 31) | 27.9% (n = 19) | 36.4% (n = 12) | 0.49 |
| Post-discharge 30-days mortality, % (n) | 4% (n = 4) | 4.4% (n = 30 | 3% (n =1) | 0.99 |
| SMVT/VF recurrences during follow-up, % (n) | 35.6% (n = 36) | 29.4% (n = 20) | 48.5% (n = 16) | 0.077 |
| Parameter | HR | CI 95% | p |
|---|---|---|---|
| Residually inducible SMVT at PES after ablation | 4.9 | 2.3–10.2 | <0.001 |
| NYHA III-IV at admission | 3.2 | 1.5–6.2 | 0.002 |
| Moderate/severe MR | 4.2 | 2–8.7 | <0.001 |
| AF at admission | 3.5 | 1.6–7.8 | 0.002 |
| Ischemic cardiomyopathy | 1.07 | 0.5–2.2 | 0.85 |
| Age | 1.06 | 1.02–1.1 | 0.001 |
| LVEF < 25% | 1.7 | 0.8–3.6 | 0.11 |
| COPD | 2 | 0.7–6 | 0.16 |
| T2DM | 1.5 | 0.7–3.1 | 0.28 |
| CKD | 2.4 | 0.9–6.2 | 0.051 |
| Total number of ablation procedures | 1.1 | 0.6–2.1 | 0.6 |
| Number of VTs induced during the procedure | 1.1 | 0.9–1.2 | 0.054 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vatasescu, R.; Cojocaru, C.; Gondos, V.; Iorgulescu, C.; Bogdan, S.; Onciul, S.; Berruezo, A. MSA-VT Score for Assessment of Long-Term Prognosis after Electrical Storm Ablation. Biomedicines 2024, 12, 493. https://doi.org/10.3390/biomedicines12030493
Vatasescu R, Cojocaru C, Gondos V, Iorgulescu C, Bogdan S, Onciul S, Berruezo A. MSA-VT Score for Assessment of Long-Term Prognosis after Electrical Storm Ablation. Biomedicines. 2024; 12(3):493. https://doi.org/10.3390/biomedicines12030493
Chicago/Turabian StyleVatasescu, Radu, Cosmin Cojocaru, Viviana Gondos, Corneliu Iorgulescu, Stefan Bogdan, Sebastian Onciul, and Antonio Berruezo. 2024. "MSA-VT Score for Assessment of Long-Term Prognosis after Electrical Storm Ablation" Biomedicines 12, no. 3: 493. https://doi.org/10.3390/biomedicines12030493
APA StyleVatasescu, R., Cojocaru, C., Gondos, V., Iorgulescu, C., Bogdan, S., Onciul, S., & Berruezo, A. (2024). MSA-VT Score for Assessment of Long-Term Prognosis after Electrical Storm Ablation. Biomedicines, 12(3), 493. https://doi.org/10.3390/biomedicines12030493







