Effect of High-Intensity Focused Electromagnetic Technology in the Treatment of Female Stress Urinary Incontinence
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Participants and Basic Characteristic Description
3.2. The Effect of HIFEM Treatment on Urology-Related Questionnaires
3.3. Urodynamics Parameters Change Under HIFEM Treatment
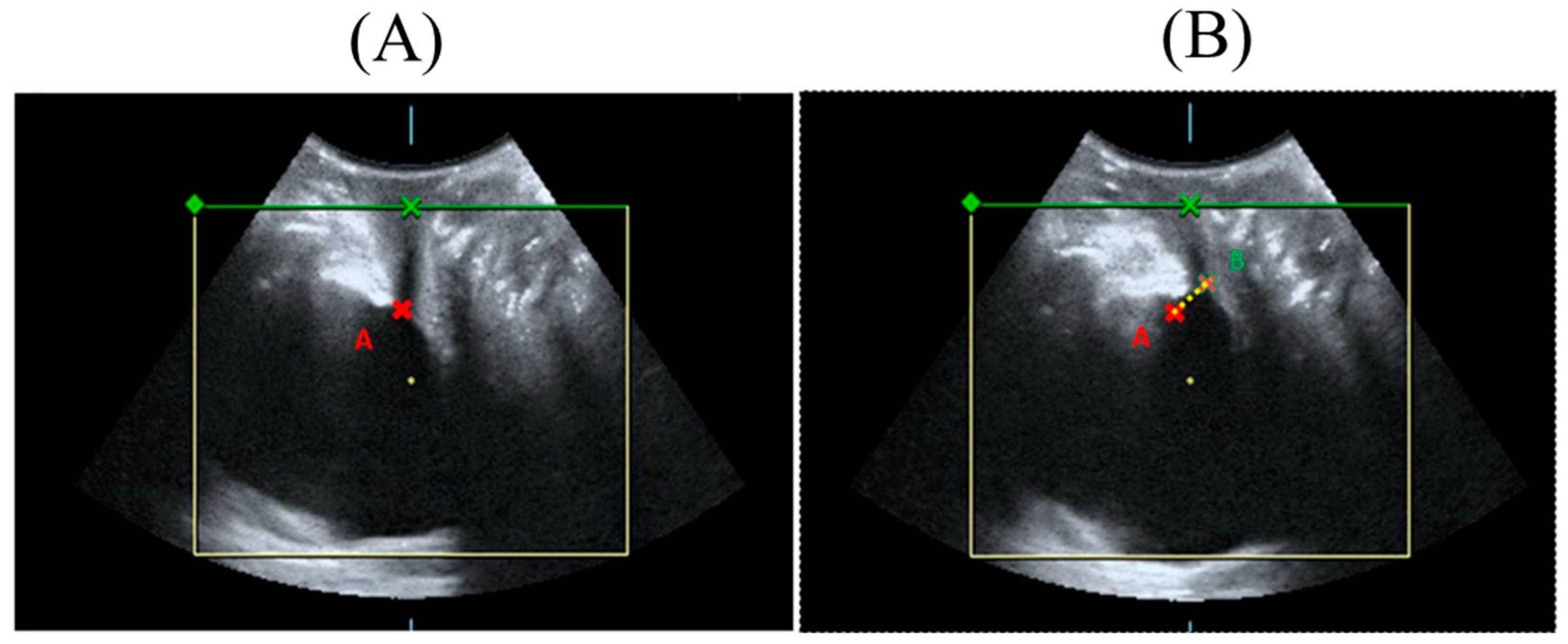
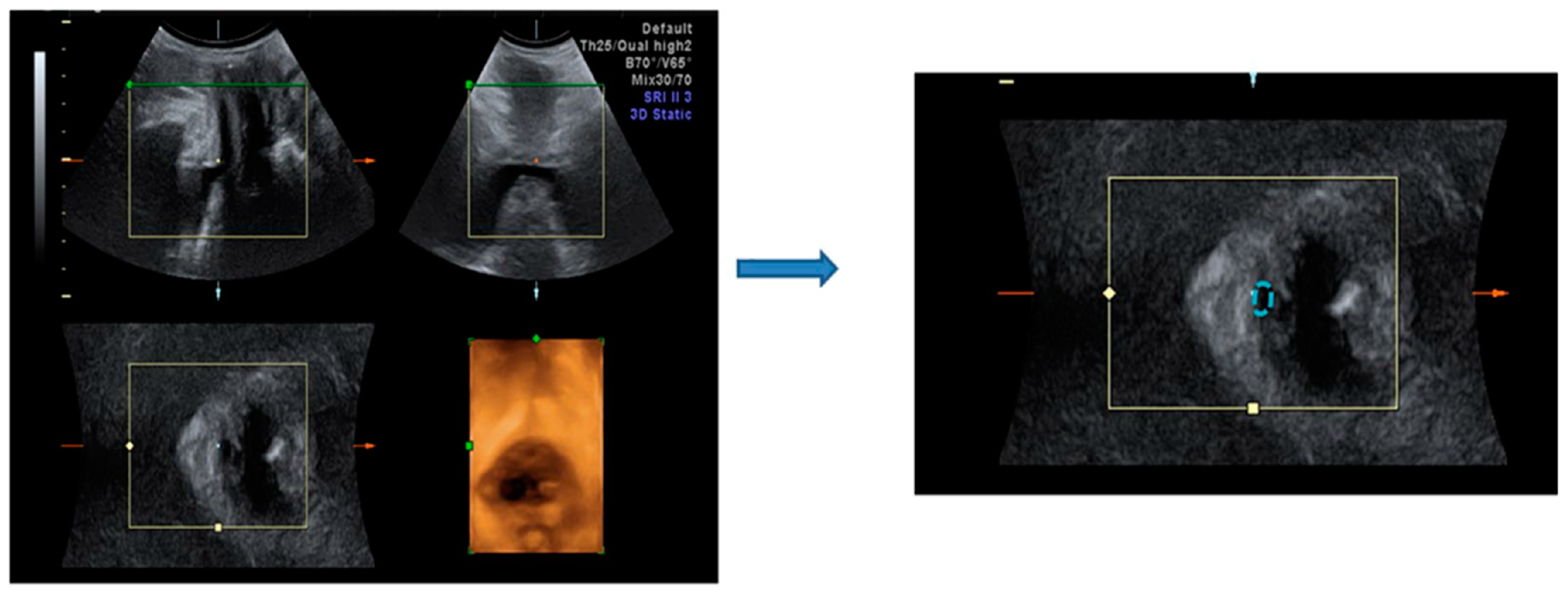
3.4. Effect of HIFEM Treatment on Bladder Neck Mobility in Ultrasound Topography
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, R.Q.; Xia, M.C.; Cui, F.; Chen, J.W.; Bian, X.D.; Xie, H.J.; Shuang, W.B. Epidemiological Survey of Adult Female Stress Urinary Incontinence. BMC Women’s Health 2021, 21, 172. [Google Scholar] [CrossRef]
- Toozs-Hobson, P.; Freeman, R.; Barber, M.; Maher, C.; Haylen, B.; Athanasiou, S.; Swift, S.; Whitmore, K.; Ghoniem, G.; De Ridder, D. An International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Report on the Terminology for Reporting Outcomes of Surgical Procedures for Pelvic Organ Prolapse. Int. Urogynecol. J. 2012, 23, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Lim, R.; Liong, M.L.; Leong, W.S.; Khan, N.A.K.; Yuen, K.H. Effect of Stress Urinary Incontinence on the Sexual Function of Couples and the Quality of Life of Patients. J. Urol. 2016, 196, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Waetjen, L.E.; Xing, G.; Johnson, W.O.; Melnikow, J.; Gold, E.B. Study of Women’s Health Across the Nation (SWAN Factors Associated with Seeking Treatment for Urinary Incontinence during the Menopausal Transition. Obstet. Gynecol. 2015, 125, 1071–1079. [Google Scholar] [CrossRef] [PubMed]
- Sen, I.; Onaran, M.; Aksakal, N.; Acar, C.; Tan, M.O.; Acar, A.; Bozkirli, I. The Impact of Urinary Incontinence on Female Sexual Function. Adv. Ther. 2006, 23, 999–1008. [Google Scholar] [CrossRef] [PubMed]
- Trowbridge, E.R.; Hoover, E.F. Evaluation and Treatment of Urinary Incontinence in Women. Gastroenterol. Clin. 2022, 51, 157–175. [Google Scholar] [CrossRef]
- Hu, J.S.; Pierre, E.F. Urinary Incontinence in Women: Evaluation and Management. Am. Fam. Physician 2019, 100, 339–348. [Google Scholar]
- Kobashi, K.C.; Albo, M.E.; Dmochowski, R.R.; Ginsberg, D.A.; Goldman, H.B.; Gomelsky, A.; Kraus, S.R.; Sandhu, J.S.; Shepler, T.; Treadwell, J.R. Surgical Treatment of Female Stress Urinary Incontinence: AUA/SUFU Guideline. J. Urol. 2017, 198, 875–883. [Google Scholar] [CrossRef] [PubMed]
- Hengel, A.R.; Carlson, K.V.; Baverstock, R.J. Prevention, Diagnosis, and Management of Midurethral Mesh Sling Complications. Can. Urol. Assoc. J. 2017, 11, S135. [Google Scholar] [CrossRef]
- Bayrak, O.; Coskun, B.; Dincer, M.; Onem, K.; Onur, R. Management of the Complications of Pubovaginal Sling Surgery. Eur. Res. J. 2017, 3, 264–268. [Google Scholar] [CrossRef]
- Demirci, F.; Petri, E. Perioperative Complications of Burch Colposuspension. Int. Urogynecol. J. 2000, 11, 170–175. [Google Scholar] [CrossRef]
- Abouassaly, R.; Steinberg, J.R.; Lemieux, M.; Marois, C.; Gilchrist, L.I.; Bourque, J.; Tu, L.M.; Corcos, J. Complications of Tension-free Vaginal Tape Surgery: A Multi-institutional Review. BJU Int. 2004, 94, 110–113. [Google Scholar] [CrossRef]
- Kaelin-Gambirasio, I.; Jacob, S.; Boulvain, M.; Dubuisson, J.-B.; Dällenbach, P. Complications Associated with Transobturator Sling Procedures: Analysis of 233 Consecutive Cases with a 27 Months Follow-Up. BMC Women’s Health 2009, 9, 28. [Google Scholar] [CrossRef]
- Richter, H.E.; Burgio, K.L.; Goode, P.S.; Borello-France, D.; Bradley, C.S.; Brubaker, L.; Handa, V.L.; Fine, P.M.; Visco, A.G.; Zyczynski, H.M. Non-Surgical Management of Stress Urinary Incontinence: Ambulatory Treatments for Leakage Associated with Stress (ATLAS) Trial. Clin. Trials 2007, 4, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Samuels, J.B.; Pezzella, A.; Berenholz, J.; Alinsod, R. Safety and Efficacy of a Non-invasive High-intensity Focused Electromagnetic Field (HIFEM) Device for Treatment of Urinary Incontinence and Enhancement of Quality of Life. Lasers Surg. Med. 2019, 51, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Madill, S.J.; Harvey, M.-A.; McLean, L. Women with SUI Demonstrate Motor Control Differences during Voluntary Pelvic Floor Muscle Contractions. Int. Urogynecol. J. 2009, 20, 447–459. [Google Scholar] [CrossRef]
- Galloway, N.T.; El-Galley, R.E.; Sand, P.K.; Appell, R.A.; Russell, H.W.; Carlan, S.J. Extracorporeal Magnetic Innervation Therapy for Stress Urinary Incontinence. Urology 1999, 53, 1108–1111. [Google Scholar] [CrossRef]
- Fujishiro, T.; Enomoto, H.; Ugawa, Y.; Takahashi, S.; Ueno, S.; Kitamura, T. Magnetic Stimulation of the Sacral Roots for the Treatment of Stress Incontinence: An Investigational Study and Placebo Controlled Trial. J. Urol. 2000, 164, 1277–1279. [Google Scholar] [CrossRef]
- Manganotti, P.; Zaina, F.; Vedovi, E.; Pistoia, L.; Rubilotta, E.; D’Amico, A.; Falso, M. Repetitive Magnetic Stimulation of the Sacral Roots for the Treatment of Stress Incontinence: A Brief Report. Eur. Medicophys. 2007, 43, 339–344. [Google Scholar]
- Gilling, P.J.; Wilson, L.C.; Westenberg, A.M.; McAllister, W.J.; Kennett, K.M.; Frampton, C.M.; Bell, D.F.; Wrigley, P.M.; Fraundorfer, M.R. A Double-blind Randomized Controlled Trial of Electromagnetic Stimulation of the Pelvic Floor vs. Sham Therapy in the Treatment of Women with Stress Urinary Incontinence. BJU Int. 2009, 103, 1386–1390. [Google Scholar] [CrossRef]
- Hlavinka, T.; Turcan, P.; Bader, A. The Use of HIFEM Technology in the Treatment of Pelvic Floor Muscles as a Cause of Female Sexual Dysfunction: A Multi-Center Pilot Study. J. Women’s Health Care 2019, 8, 455. [Google Scholar]
- Hilton, M.P. The Stamey Procedure for Stress Incontinence. Curr. Obstet. Gynaecol. 1991, 1, 103–108. [Google Scholar] [CrossRef]
- Long, C.-Y.; Lin, K.-L.; Lee, Y.-C.; Chuang, S.-M.; Lu, J.-H.; Wu, B.-N.; Chueh, K.-S.; Ker, C.-R.; Shen, M.-C.; Juan, Y.-S. Therapeutic Effects of Low Intensity Extracorporeal Low Energy Shock Wave Therapy (LiESWT) on Stress Urinary Incontinence. Sci. Rep. 2020, 10, 5818. [Google Scholar] [CrossRef] [PubMed]
- Mezzana, P.; Pieri, L.; Leone, A.; Fusco, I. Schwarzy: The New System for Muscle Toning and Body Shaping. J. Cosmet. Dermatol. 2021, 20, 2678–2680. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, D.J.; Enright, K.M.; Goldfarb, R.; Katz, B.; Gold, M. The Role and Clinical Benefits of High-Intensity Focused Electromagnetic Devices for Non-Invasive Lipolysis and beyond: A Narrative Review and Position Paper. J. Cosmet. Dermatol. 2021, 20, 2096–2101. [Google Scholar] [CrossRef] [PubMed]
- Homma, Y.; Yoshida, M.; Seki, N.; Yokoyama, O.; Kakizaki, H.; Gotoh, M.; Yamanishi, T.; Yamaguchi, O.; Takeda, M.; Nishizawa, O. Symptom Assessment Tool for Overactive Bladder Syndrome--Overactive Bladder Symptom Score. Urology 2006, 68, 318–323. [Google Scholar] [CrossRef]
- Shumaker, S.A.; Wyman, J.F.; Uebersax, J.; McClish, D.; Fantl, J.A. Continence Program in Women (CPW) Research Group Health-Related Quality of Life Measures for Women with Urinary Incontinence: The Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Qual. Life Res. 1994, 3, 291–306. [Google Scholar] [CrossRef] [PubMed]
- Corcos, J.; Behlouli, H.; Beaulieu, S. Identifying Cut-off Scores with Neural Networks for Interpretation of the Incontinence Impact Questionnaire. Neurourol. Urodyn. Off. J. Int. Cont. Soc. 2002, 21, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.G.; Sandoz, E.K.; Kitchens, J.; Roberts, M. The Valued Living Questionnaire: Defining and Measuring Valued Action within a Behavioral Framework. Psychol. Rec. 2010, 60, 249–272. [Google Scholar] [CrossRef]
- Sendag, F.; Vidinli, H.; Kazandi, M.; Itil, I.M.; Askar, N.; Vidinli, B.; Pourbagher, A. Role of Perineal Sonography in the Evaluation of Patients with Stress Urinary Incontinence. Aust. N. Z. J. Obstet. Gynaecol. 2003, 43, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Călinescu, B.C.; Neacșu, A.; Martiniuc, A.E.; Dumitrescu, D.; Stănică, C.D.; Roșu, G.-A.; Chivu, L.I.; Ioan, R.G. Surgical Treatments for Women with Stress Urinary Incontinence: A Systematic Review. Life 2023, 13, 1480. [Google Scholar] [CrossRef] [PubMed]
- Disha, T.; Haque, F. Prevalence and Risk Factors of Vulvovaginal Candidosis during Pregnancy: A Review. Infect. Dis. Obstet. Gynecol. 2022, 2022, 6195712. [Google Scholar] [CrossRef]
- Rovner, E.S.; Wein, A.J. Treatment Options for Stress Urinary Incontinence. Rev. Urol. 2004, 6, S29. [Google Scholar]
- Smith, A.L.; Wein, A.J. Urinary Incontinence—Pharmacotherapy Options. Ann. Med. 2011, 43, 461–476. [Google Scholar] [CrossRef] [PubMed]
- Yamanishi, T.; Suzuki, T.; Sato, R.; Kaga, K.; Kaga, M.; Fuse, M. Effects of Magnetic Stimulation on Urodynamic Stress Incontinence Refractory to Pelvic Floor Muscle Training in a Randomized Sham-controlled Study. LUTS Low. Urin. Tract Symptoms 2019, 11, 61–65. [Google Scholar] [CrossRef]
- Jung, R.; Ichihara, K.; Venkatasubramanian, G.; Abbas, J.J. Chronic Neuromuscular Electrical Stimulation of Paralyzed Hindlimbs in a Rodent Model. J. Neurosci. Methods 2009, 183, 241–254. [Google Scholar] [CrossRef]
- Novak, S.; Guerron, G.; Zou, Z.; Cheung, G.; Berteau, J.-P. New Guidelines for Electrical Stimulation Parameters in Adult Patients with Knee Osteoarthritis Based on a Systematic Review of the Current Literature. Am. J. Phys. Med. Rehabil. 2020, 99, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Rambhia, P.H.; Turner, L.; Ugonabo, N.; Chapas, A. Muscle Stimulation for Aesthetic Body Shaping: A Comprehensive and Critical Review. Dermatol. Surg. 2022, 48, 1076–1082. [Google Scholar] [CrossRef] [PubMed]
- Alazab, I.M.; Fayez, E.S.; El-Deen, A.G.; Khalaf, M.; El-kassas, T.A.; Said, S.M.; Shymaa, A.F.A. Effect of Peripheral Pulsed Electromagnetic Stimulation Versus Neuromuscular Stimulation on Stroke-Induced Shoulder Subluxation. NeuroQuantology 2022, 20, 1596. [Google Scholar]
- Silantyeva, E.; Zarkovic, D.; Astafeva, E.; Soldatskaia, R.; Orazov, M.; Belkovskaya, M.; Kurtser, M. A Comparative Study on the Effects of High-Intensity Focused Electromagnetic Technology and Electrostimulation for the Treatment of Pelvic Floor Muscles and Urinary Incontinence in Parous Women: Analysis of Posttreatment Data. Urogynecology 2021, 27, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Braga, A.; Castronovo, F.; Caccia, G.; Papadia, A.; Regusci, L.; Torella, M.; Salvatore, S.; Scancarello, C.; Ghezzi, F.; Serati, M. Efficacy of 3 Tesla Functional Magnetic Stimulation for the Treatment of Female Urinary Incontinence. J. Clin. Med. 2022, 11, 2805. [Google Scholar] [CrossRef]
- Doğanay, M.; Kilic, S.; Yilmaz, N. Long-Term Effects of Extracorporeal Magnetic Innervations in the Treatment of Women with Urinary Incontinence: Results of 3-Year Follow-Up. Arch. Gynecol. Obstet. 2010, 282, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Brandeis, J. (126) Application of HIFEM Therapy Improves Orgasmic, Urinary and Erectile Function by Stimulation of Pelvic Floor Muscles. J. Sex. Med. 2024, 21, qdae001.120. [Google Scholar] [CrossRef]
- Long, C.-Y.; Lee, J.P.-N.; Loo, Z.-X.; Liu, Y.-Y.; Yeh, C.-L.; Feng, C.-W.; Lin, K.-L. The Clinical Effects of Pixel CO2 Laser on Bladder Neck and Stress Urinary Incontinence. J. Clin. Med. 2022, 11, 4971. [Google Scholar] [CrossRef]
- Long, C.-Y.; Chang, C.-Y.; Liu, Y.-Y.; Loo, Z.-X.; Yeh, C.-L.; Wu, M.-P.; Lin, K.-L.; Tang, F.-H. Tape-Releasing Suture with “Long Loop” on Mid-Urethral Sling: A Novel Procedure for Management of Iatrogenic Urethral Obstruction. J. Clin. Med. 2023, 12, 3938. [Google Scholar] [CrossRef] [PubMed]
| SUI Surgery Options | Complications | Reference |
|---|---|---|
| Pubovaginal sling | 10–15% failure rate 5–10% voiding difficulties 10–15% bladder urgency or urge incontinence 5% wound or urinary tract infection 1% clotting in the legs or lungs <1% blood loss requiring transfusion <1% damage to the bladder or lower urinary tract | [10] |
| Burch colposuspension | <5% bladder injuries 1% urethral injury 20% voiding dysfunction 6.8~40% infection | [11] |
| Tension-free vaginal tape (TVT) | 4.5% bladder perforation damage to pelvic blood vessels or viscera. 4% voiding difficulties and urinary retention 3–15% urgency and frequency 1.3% groin pain (1.3%) | [12] |
| Transobturator tape (TOT) | 5–10% bladder irritability 2–3% damage to the vagina, bladder, urethra, or blood vessels 1–5% urinary tract infections 1–5% difficulty passing urine 1% risk of a wound infection 1% blood clots in the legs or chest | [13] |
| n = 19 | Pre-Tx | Post-Tx | p Value |
|---|---|---|---|
| Mean age (years) | 55.2 ± 13.0 | ||
| Mean BMI (kg/m2) | 24.0 ± 3.2 | ||
| Menopause | 17 (89.5%) | ||
| One hour Pad test (g) | 4.2 ± 5.5 | 0.6 ± 1.3 | 0.045 * |
| SUI grade by ICIQ | |||
| Mild | 3 (15.8%) | ||
| Moderate | 12 (63.2%) | ||
| Severe | 4 (21.1%) | ||
| Very severe | 1 (5.3%) | ||
| Effectiveness for SUI | 13/19 (68.4%) | <0.001 * | |
| Follow-up (months) | 6M |
| n = 19 | Pre-Tx | Post-Tx 1M | Post-Tx 6M | p Value 1M | p Value 3M |
|---|---|---|---|---|---|
| OABSS | 5.3 ± 3.9 | 3.9 ± 3.6 | 3.6 ± 3.0 | 0.008 * | 0.023 * |
| UDI-6 | 35.7 ± 22.3 | 26.5 ± 20.0 | 15.2 ± 10.6 | 0.013 * | <0.001 * |
| IIQ-7 | 33.1 ± 28.7 | 25.5 ± 30.3 | 14.3 ± 17.2 | 0.006 * | 0.005 * |
| ICIQ-SF | 9.4 ± 5.0 | 7.3 ± 4.1 | 5.4 ± 3.6 | 0.008 * | <0.001 * |
| VLQ | 3.5 ± 0.7 | 3.8 ± 0.8 | 4.2 ± 0.8 | 0.363 | 0.189 |
| n = 11 | Pre-Tx | Post-Tx 6M | p Value * |
|---|---|---|---|
| Qmax (mL/s) | 20.4 ± 5.7 | 21.0 ± 8.5 | 0.968 |
| RU (mL) | 37.9 ± 44.2 | 28.9 ± 25.7 | 0.664 |
| Vfst (mL) | 142.9 ± 79.4 | 149.9 ± 75.2 | 0.913 |
| MCC (mL) | 432.2 ± 136.5 | 458.2 ± 112.0 | 0.783 |
| Pdet Qmax (mmHg) | 12.7 ± 11.9 | 26.7 ± 21.5 | 0.186 |
| MUCP (mmHg) | 46.4 ± 25.2 | 58.1 ± 21.2 | 0.017 * |
| FUL (cm) | 28.7 ± 11.4 | 30.1 ± 5.1 | 0.795 |
| UCA (°) | 705.3 ± 302.3 | 990.0 ± 439.6 | 0.001 * |
| n = 14 | Pre-Tx | Post-Tx 6M | p Value | |
|---|---|---|---|---|
| Bladder neck mobility (mm) | 1.2 ± 0.4 | 1.1 ± 0.3 | 0.34 | |
| Urethral area (mm²) | proximal | 0.8 ± 0.4 | 0.7 ± 0.2 | 0.58 |
| Resting | middle | 0.8 ± 0.3 | 0.8 ± 0.2 | 0.17 |
| distal | 2.3 ± 1.0 | 2.5 ± 1.2 | 0.44 | |
| Urethral area (mm²) | proximal | 4.1 ± 1.3 | 5.3 ± 17.2 | 0.34 |
| straining | middle | 0.8 ± 0.2 | 0.8 ± 0.3 | 0.17 |
| distal | 0.7 ± 0.2 | 0.6 ± 0.2 | 0.19 | |
| n = 14 | Rest | Stress | |||||
|---|---|---|---|---|---|---|---|
| Pre-Tx | Post-Tx 6M | p Value | Pre-Tx | Post-Tx 6M | p Value | ||
| Vaginal width | Proximal | 4.6 ± 0.5 | 4.4 ± 0.5 | 0.75 | 4.6 ± 0.5 | 4.4 ± 0.6 | 0.67 |
| Middle | 4.2 ± 0.4 | 4.2 ± 0.5 | 0.44 | 4.4 ± 0.5 | 4.2 ± 0.5 | 0.19 | |
| Distal | 4.3 ± 0.3 | 4.0 ± 0.4 | 0.05 * | 4.4 ± 0.5 | 4.1 ± 0.4 | 0.04 * | |
| Vaginal area | Proximal | 6.1 ± 1.6 | 4.0 ± 1.2 | <0.001 * | 6.9 ± 1.3 | 5.2 ± 2.0 | 0.002 * |
| Middle | 5.6 ± 1.2 | 4.0 ± 1.1 | 0.002 * | 6.5 ± 1.0 | 4.8 ± 1.6 | 0.003 * | |
| Distal | 5.7 ± 1.4 | 4.1 ± 1.1 | 0.001 * | 6.4 ± 1.2 | 4.4 ± 1.3 | <0.001 * | |
| Levator hiatus | Area | 12.0 ± 2.7 | 10.2 ± 2.7 | 0.028 * | 13.5 ± 2.8 | 11.8 ± 3.4 | 0.024 * |
| Short axis | 4.5 ± 0.5 | 4.2 ± 0.5 | 0.104 | 4.7 ± 0.5 | 4.3 ± 0.5 | 0.013 * | |
| Long axis | 3.5 ± 0.6 | 3.4 ± 0.6 | 1.0 | 3.9 ± 0.6 | 3.7 ± 0.6 | 0.5 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Long, C.-Y.; Lin, K.-L.; Yeh, J.-L.; Feng, C.-W.; Loo, Z.-X. Effect of High-Intensity Focused Electromagnetic Technology in the Treatment of Female Stress Urinary Incontinence. Biomedicines 2024, 12, 2883. https://doi.org/10.3390/biomedicines12122883
Long C-Y, Lin K-L, Yeh J-L, Feng C-W, Loo Z-X. Effect of High-Intensity Focused Electromagnetic Technology in the Treatment of Female Stress Urinary Incontinence. Biomedicines. 2024; 12(12):2883. https://doi.org/10.3390/biomedicines12122883
Chicago/Turabian StyleLong, Cheng-Yu, Kun-Ling Lin, Jian-Lin Yeh, Chien-Wei Feng, and Zi-Xi Loo. 2024. "Effect of High-Intensity Focused Electromagnetic Technology in the Treatment of Female Stress Urinary Incontinence" Biomedicines 12, no. 12: 2883. https://doi.org/10.3390/biomedicines12122883
APA StyleLong, C.-Y., Lin, K.-L., Yeh, J.-L., Feng, C.-W., & Loo, Z.-X. (2024). Effect of High-Intensity Focused Electromagnetic Technology in the Treatment of Female Stress Urinary Incontinence. Biomedicines, 12(12), 2883. https://doi.org/10.3390/biomedicines12122883




