Para-Anastomotic Pseudoaneurysms as a Long-Term Complication After Surgical Treatment of Peripheral Artery Disease: Clinical Characteristics and Surgical Treatment
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
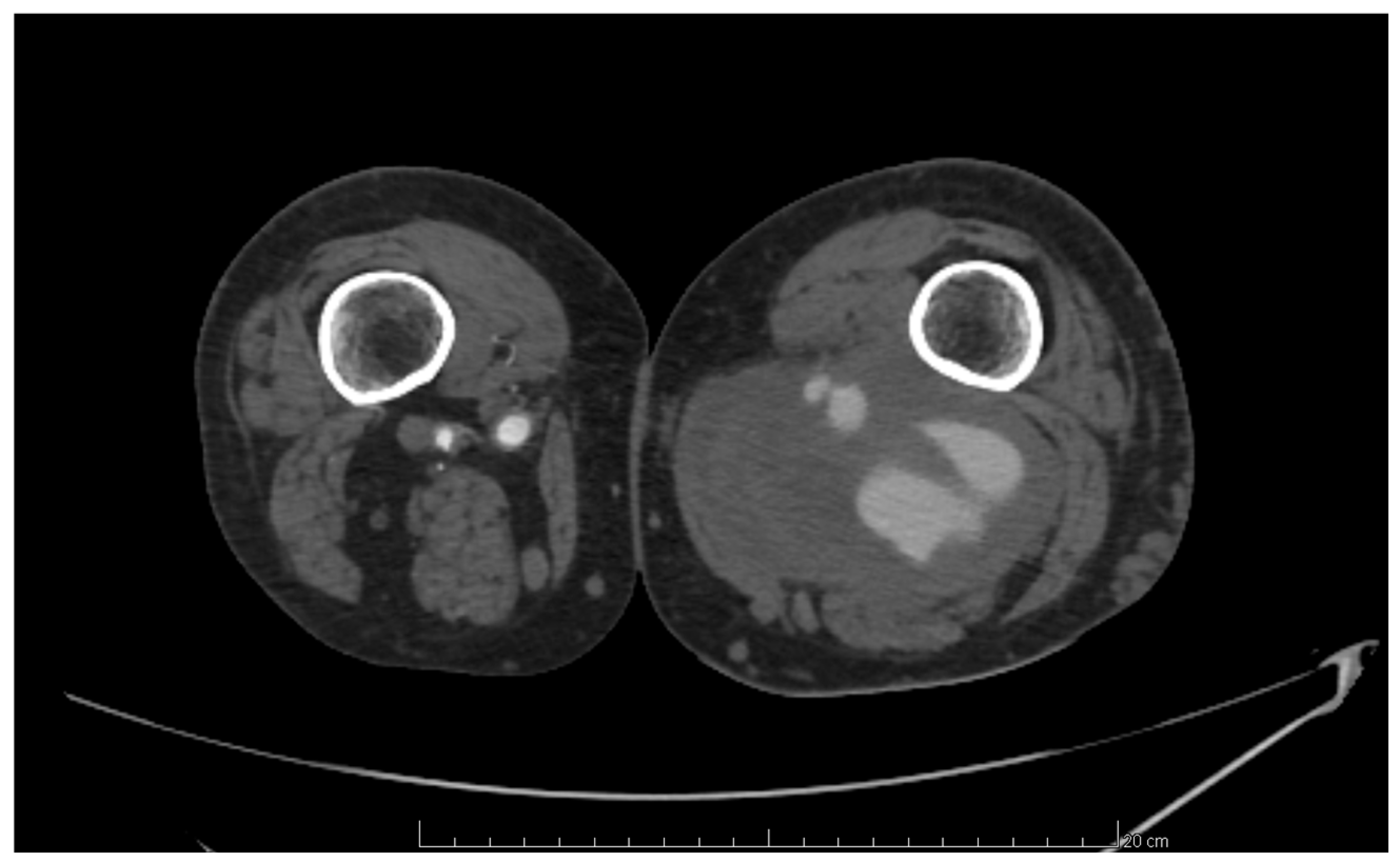
2.2. Anastomotic Pseudoaneurysm Diagnostic Criteria
2.3. Treatment Methods
2.4. Term Definitions
2.5. Data Analyzed in the Study
2.6. Statistical Analysis
3. Results
3.1. Demographic and Descriptive Data of the Patients
3.2. Characteristics of Anastomotic Aneurysms
3.3. Perioperative Data and Short-Term Outcomes
3.4. Patients’ Long-Term Outcomes After Anastomotic Aneurysm Treatment
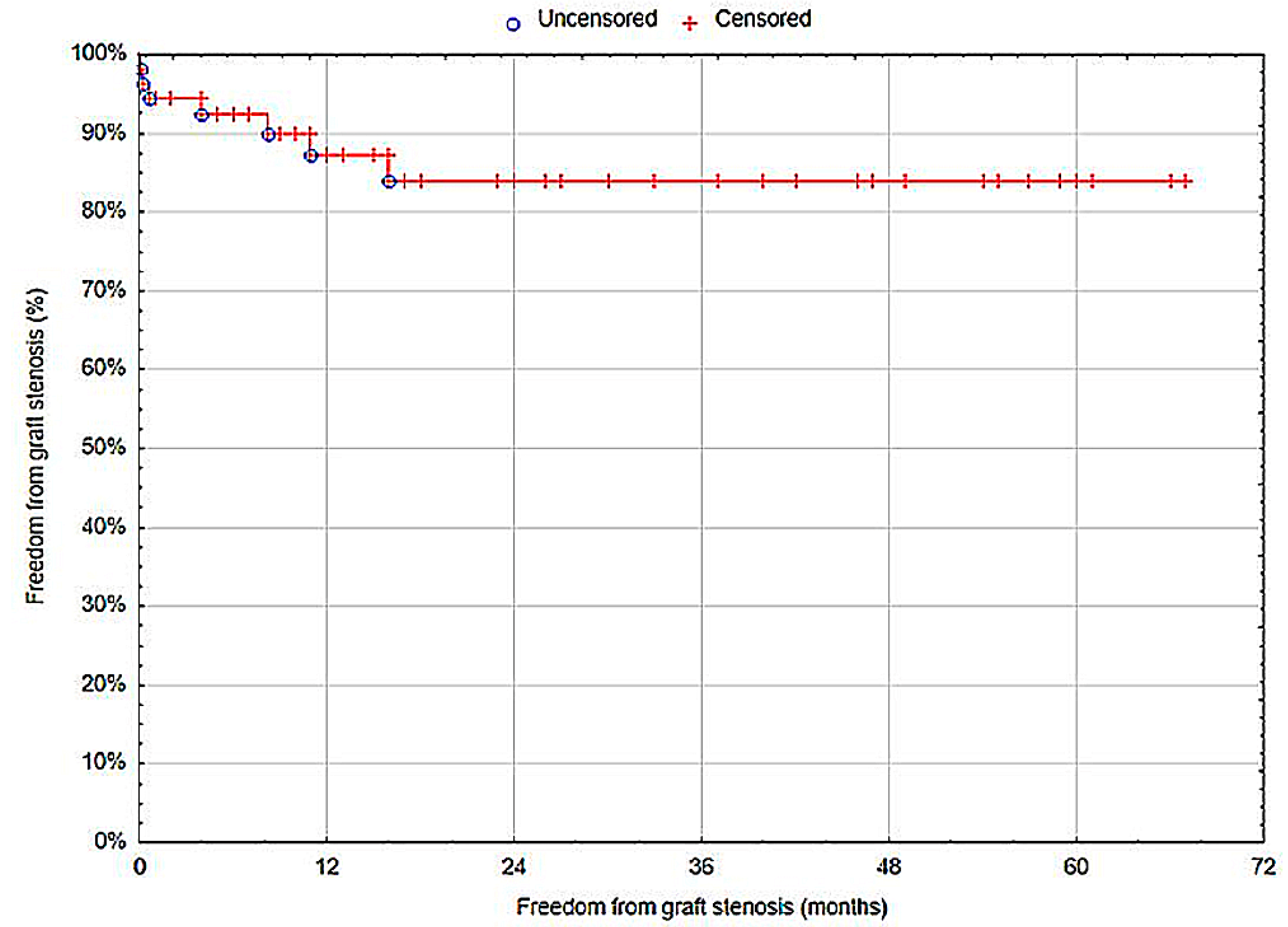
3.4.1. Graft Patency
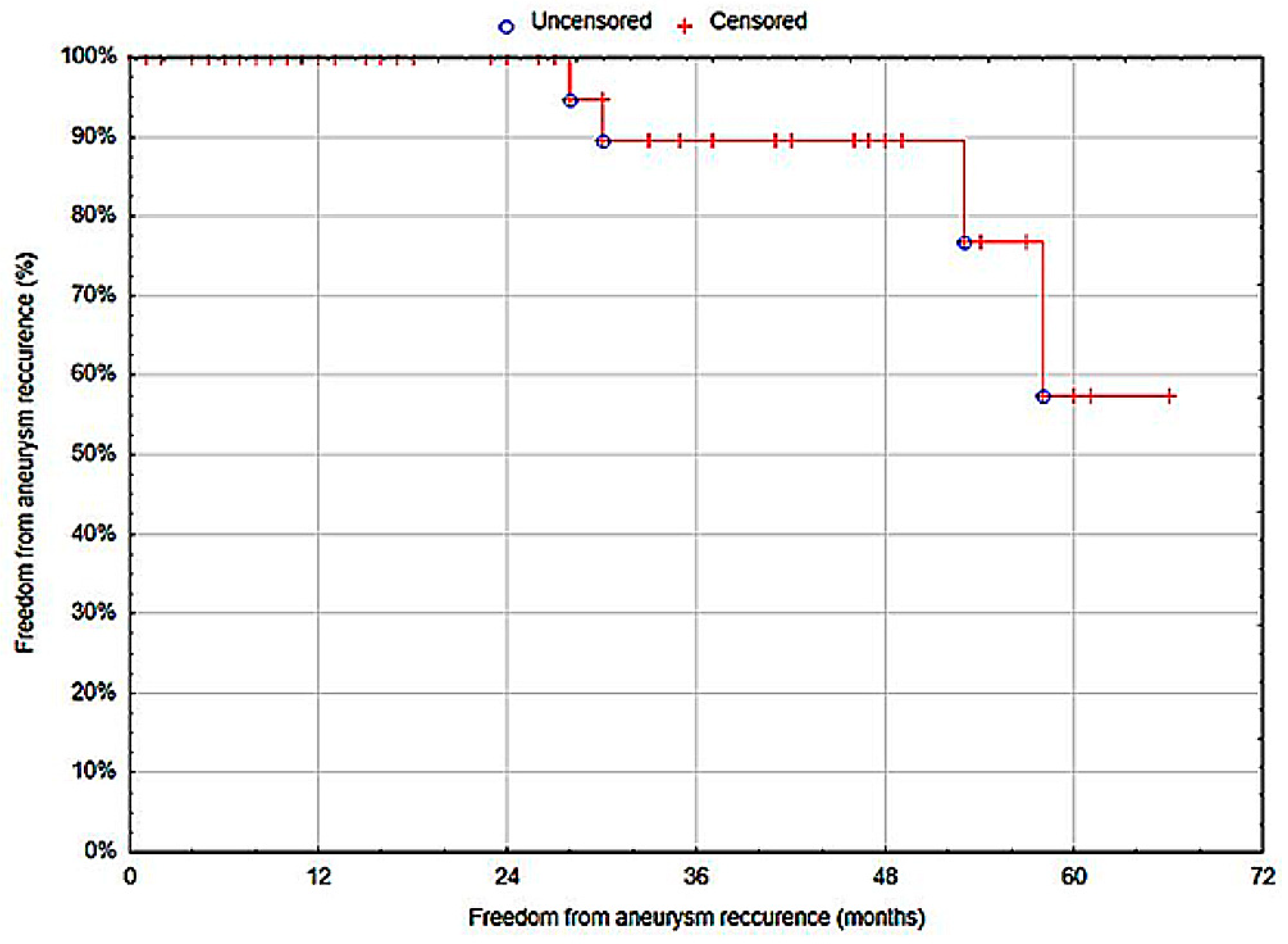
3.4.2. Anastomotic Pseudoaneurysm Recurrence
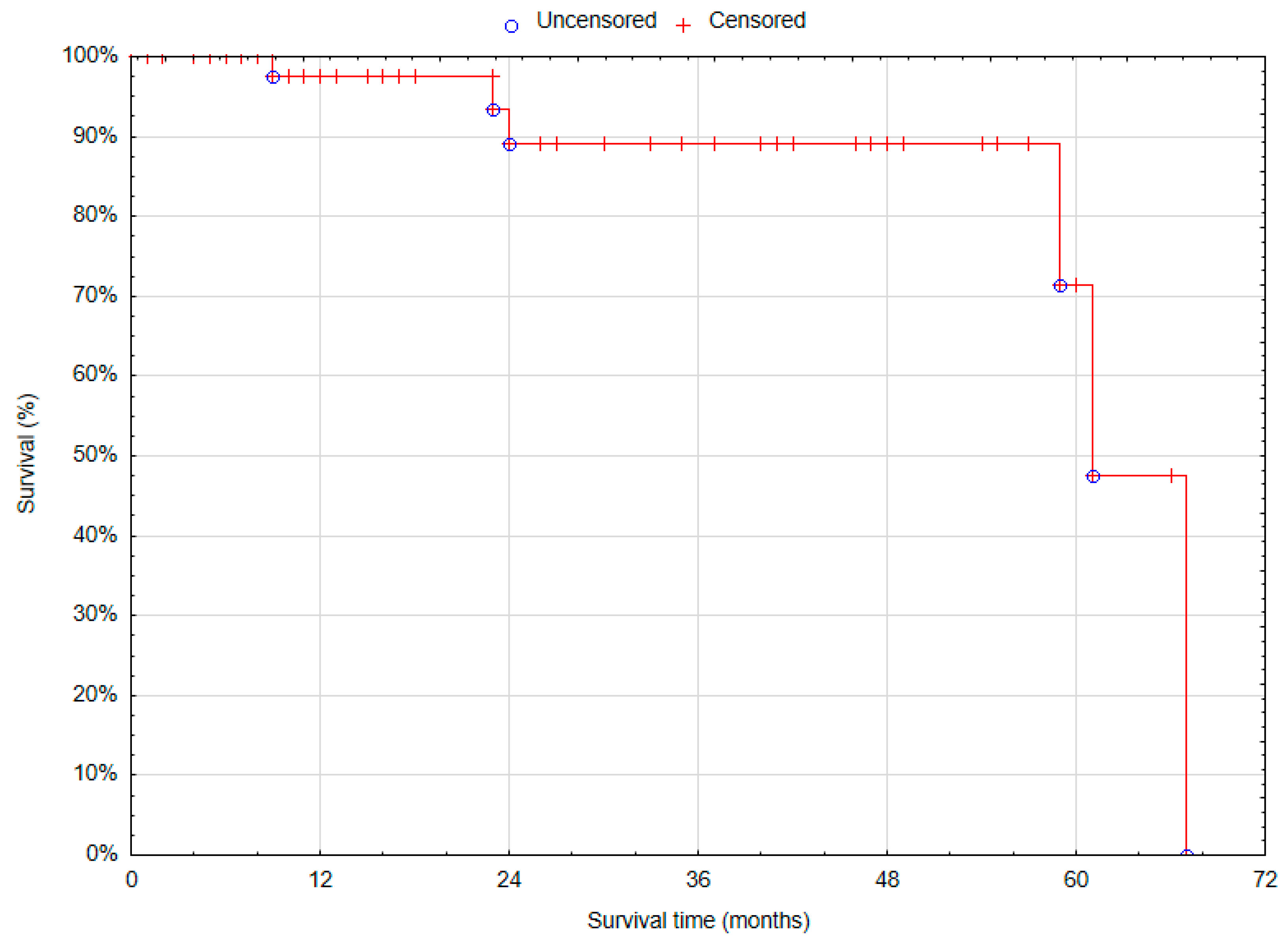
3.4.3. Overall Survival
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Criqui, M.H.; Matsushita, K.; Aboyans, V.; Hess, C.N.; Hicks, C.W.; Kwan, T.W.; McDermott, M.M.; Misra, S.; Ujueta, F. Lower Extremity Peripheral Artery Disease: Contemporary Epidemiology, Management Gaps, and Future Directions: A Scientific Statement From the American Heart Association. Circulation 2021, 144, e171–e191, Erratum in Circulation 2021, 144, e193. [Google Scholar] [CrossRef] [PubMed]
- Eid, M.A.; Mehta, K.S.; Goodney, P.P. Epidemiology of peripheral artery disease. Semin. Vasc. Surg. 2021, 34, 38–46. [Google Scholar] [CrossRef]
- Nordanstig, J.; Behrendt, C.A.; Baumgartner, I.; Belch, J.; Bäck, M.; Fitridge, R.; Hinchliffe, R.; Lejay, A.; Mills, J.L.; Rother, U.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2024 Clinical Practice Guidelines on the Management of Asymptomatic Lower Limb Peripheral Arterial Disease and Intermittent Claudication. Eur. J. Vasc. Endovasc. Surg. 2024, 67, 9–96. [Google Scholar] [CrossRef] [PubMed]
- Sokhal, B.S.; Ma, Y.; Rajagopalan, S. Femoral artery aneurysms. Br. J. Hosp. Med. 2022, 83, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Roberts, K.; Revell, M.; Youssef, H.; Bradbury, A.W.; Adam, D.J. Hypotensive resuscitation in patients with ruptured abdominal aortic aneurysm. Eur. J. Vasc. Endovasc. Surg. 2006, 31, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Serizawa, F.; Ohara, M.; Kotegawa, T.; Watanabe, S.; Shimizu, T.; Akamatsu, D. The Incidence of Para-Anastomotic Aneurysm After Open Repair Surgery for Abdominal Aortic Aneurysm Through Routine Annual Computed Tomography Imaging. Eur. J. Vasc. Endovasc. Surg. 2021, 62, 187–192. [Google Scholar] [CrossRef]
- Diwan, A.; Sarkar, R.; Stanley, J.C.; Zelenock, G.B.; Wakefield, T.W. Incidence of femoral and popliteal artery aneurysms in patients with abdominal aortic aneurysms. J. Vasc. Surg. 2000, 31, 863–869. [Google Scholar] [CrossRef]
- Wanhainen, A.; Verzini, F.; Van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; van Herwaarden, J.; Karkos, C.; Koelemay, M.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 8–93, Erratum in Eur. J. Vasc. Endovasc. Surg. 2020, 59, 494. [Google Scholar] [CrossRef]
- Jacobowitz, G.R. Color Duplex Ultrasound for Diagnosis of Peripheral Artery Aneurysms (Lower and Upper Extremity). In Noninvasive Vascular Diagnosis, 2nd ed.; AbuRahma, A.F., Perler, B.A., Eds.; Springer: Cham, Switzerland, 2022; Volume 3, pp. 154–196. [Google Scholar] [CrossRef]
- Roy, J.; Labruto, F.; Beckman, M.O.; Danielson, J.; Johansson, G.; Swedenborg, J. Bleeding into the intraluminal thrombus in abdominal aortic aneurysms is associated with rupture. J. Vasc. Surg. 2008, 48, 1108–1113. [Google Scholar] [CrossRef]
- Koza, Y.; Kaya, U. Retrospective Analysis of 120 Cases of Iatrogenic and Traumatic Peripheral Arterial Pseudoaneurysms. Eurasian J. Med. 2020, 52, 180–184. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stone, P.A.; Campbell, J.E.; AbuRahma, A.F. Femoral pseudoaneurysms after percutaneous access. J. Vasc. Surg. 2014, 60, 1359–1366. [Google Scholar] [CrossRef] [PubMed]
- Ylönen, K.; Biancari, F.; Leo, E.; Rainio, P.; Salmela, E.; Lahtinen, J.; Satta, J.; Pokela, R.; Lepojärvi, M.; Juvonen, T. Predictors of development of anastomotic femoral pseudoaneurysms after aortobifemoral reconstruction for abdominal aortic aneurysm. Am. J. Surg. 2004, 187, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.; Turner, S.A.; Torrie, P.; Gibson, M. Iatrogenic femoral artery pseudoaneurysms--a review of current methods of diagnosis and treatment. Clin. Radiol. 2008, 63, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Morgan, R.; Belli, A.M. Current treatment methods for postcatheterization pseudoaneurysms. J. Vasc. Interv. Radiol. 2003, 14, 697–710. [Google Scholar] [CrossRef]
- Middleton, W.D.; Dasyam, A.; Teefey, S.A. Diagnosis and treatment of iatrogenic femoral artery pseudoaneurysms. Ultrasound Q. 2005, 21, 3–17. [Google Scholar]
- Marković, D.M.; Davidović, L.B.; Kostić, D.M.; Maksimović, L.; Kuzmanovic, I.B.; Koncar, I.B.; Cvetkovic, D.M. False anastomotic aneurysms. Vascular 2007, 15, 141–148. [Google Scholar] [CrossRef]
- Serafin, M.; Łyko-Morawska, D.; Szostek, J.; Stańczyk, D.; Mąka, M.; Kania, I.; Kuczmik, W. A Five-Year Retrospective Study from a Single Center on the Location, Presentation, Diagnosis, and Management of 110 Patients with Aneurysms of the Femoral and Popliteal Arteries of the Lower Limb. J. Clin. Med. 2024, 13, 4323. [Google Scholar] [CrossRef]
- Kim, G.E.; Imparato, A.M.; Nathan, I.; Riles, T.S. Dilatation of synthetic grafts and junctional aneurysms. Arch. Surg. 1979, 114, 1296–1303. [Google Scholar]
- Clark, E.T.; Gewertz, B.L. Pseudoaneurysms. In Vascular Surgery, 4th ed.; Rutherford, R.B., Ed.; W.B. Saunders: Philadelphia, PA, USA, 1995; pp. 1153–1161. [Google Scholar]
- Paasche, R.E.; Kinly, C.E.; Dolan, F.G.; Gozna, E.; Marble, A. Consideration of suture line stresses in the selection of synthetic grafts for implantation. J. Biomech. 1973, 6, 253–259. [Google Scholar] [CrossRef]
- Corriere, M.A.; Guzman, R.J. True and false aneurysms of the femoral artery. Semin. Vasc. Surg. 2005, 18, 216–223. [Google Scholar] [CrossRef]
- Rowlands, C.; Youssef, S.; Rajagopalan, S. Popliteal arterial aneurysms. Br. J. Hosp. Med. 2022, 83, 1–7. [Google Scholar] [CrossRef]
- Demarche, M.; Waltregny, D.; van Damme, H.; Limet, R. Femoral anastomotic aneurysms: Pathogenic factors, clinical presentations and treatment. A study of 142 cases. Cardiovasc. Surg. 1999, 7, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Rivera, P.A.; Dattilo, J.B. Pseudoaneurysm. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Beregi, J.P.; Prat, A.; Willoteaux, S.; Vasseur, M.A.; Boularand, V.; Desmoucelle, F. Covered stents in the treatment of peripheral arterial aneurysms: Procedural results and midterm follow-up. Cardiovasc. Intervent Radiol. 1999, 22, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Müller-Hülsbeck, S.; Link, J.; Schwarzenberg, H.; Walluscheck, K.P.; Heller, M. Percutaneous endoluminal stent and stent-graft placement for the treatment of femoropopliteal aneurysms: Early experience. Cardiovasc. Intervent Radiol. 1999, 22, 96–102. [Google Scholar] [CrossRef] [PubMed]
- van Sambeek, M.R.; Gussenhoven, E.J.; van der Lugt, A.; Honkoop, J.; du Bois, N.A.; van Urk, H. Endovascular stent-grafts for aneurysms of the femoral and popliteal arteries. Ann. Vasc. Surg. 1999, 13, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Wiesinger, B.; Beregi, J.P.; Oliva, V.L.; Dietrich, T.; Tepe, G.; Bosiers, M.; Hüttl, K.; Müller-Hülsbeck, S.; Bray, A.; Tielemans, H.; et al. PTFE-covered self-expanding nitinol stents for the treatment of severe iliac and femoral artery stenoses and occlusions: Final results from a prospective study. J. Endovasc. Ther. 2005, 12, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Thalhammer, C.; Kirchherr, A.S.; Uhlich, F.; Waigand, J.; Gross, C.M. Postcatheterization pseudoaneurysms and arteriovenous fistulas: Repair with percutaneous implantation of endovascular covered stents. Radiology. 2000, 214, 127–131. [Google Scholar] [CrossRef]
- Wang, W.; Zhao, T.; Geng, K.; Yuan, G.; Chen, Y.; Xu, Y. Smoking and the Pathophysiology of Peripheral Artery Disease. Front. Cardiovasc. Med. 2021, 8, 704106. [Google Scholar] [CrossRef]
- Huang, Y.; Gloviczki, P.; Noel, A.A.; Sullivan, T.M.; Kalra, M.; Gullerud, R.E.; Hoskin, T.L.; Bower, T.C. Early complications and long-term outcome after open surgical treatment of popliteal artery aneurysms: Is exclusion with saphenous vein bypass still the gold standard? J. Vasc. Surg. 2007, 45, 706–715. [Google Scholar] [CrossRef]
- Perini, P.; Jean-Baptiste, E.; Vezzosi, M.; Raynier, J.-L.; Mottini, F.; Batt, M.; Hassen-Khodja, R.; Salcuni, P. Surgical management of isolated superficial femoral artery degenerative aneurysms. J. Vasc. Surg. 2014, 59, 152–158. [Google Scholar] [CrossRef][Green Version]
- Pogorzelski, R.; Fiszer, P.; Toutounchi, S.; Krajewska, E.; Szostek, M.M.; Tworus, R.; Jakuczun, W.; Skórski, M. Anastomotic aneurysms—20-years of experience from one center. Pol. Przegl Chir. 2013, 85, 181–191. [Google Scholar] [CrossRef] [PubMed]
- San Norberto García, E.M.; González-Fajardo, J.A.; Gutiérrez, V.; Carrera, S.; Vaquero, C. Femoral pseudoaneurysms post-cardiac catheterization surgically treated: Evolution and prognosis. Interact. Cardiovasc. Thorac. Surg. 2009, 8, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Honda, T.; Fujimoto, K.; Miyao, Y.; Koga, H.; Ishii, M. Current cigarette smoking is an independent risk factor for subacute stent thrombosis in acute myocardial infarction patients. J. Cardiol. 2014, 63, 358–364. [Google Scholar] [CrossRef] [PubMed]
| Variable | n (%), Mean/Median (Range, SD/IQR) |
|---|---|
| Age (years) | 67.45 (54–83, SD: 6.89) |
| Gender | |
| Male | 41 (74.55%) |
| Female | 14 (25.45%) |
| Presence of comorbidities (yes) | 49 (89.09%) |
| Arterial hypertension | 38 (69.09%) |
| General atherosclerosis | 26 (47.27%) |
| Coronary artery disease | 19 (34.55%) |
| Diabetes mellitus | 15 (27.27%) |
| History of myocardial infarction | 13 (23.64%) |
| Dyslipidemia | 11 (20.00%) |
| Heart failure | 7 (12.73%) |
| COPD | 1 (1.82%) |
| Dialysis dependence | 1 (1.82%) |
| History of cigarette smoking (yes) | 30 (54.55%) |
| Current cigarette smoking (yes) | 21 (38.18%) |
| Clinical symptoms (yes) | 34 (61.82%) |
| Lower-limb pain | 19 (34.55%) |
| Intermittent claudication | 9 (16.36%) |
| Ulcer | 4 (7.27%) |
| Aneurysm rupture | 4 (7.27%) |
| Acute limb ischemia | 3 (5.45%) |
| Gangrene | 2 (3.64%) |
| Limb swelling | 2 (3.64%) |
| Variable | n (%), Mean/Median (Range, SD/IQR) |
|---|---|
| Primary anastomosis | |
| Aortobifemoral bypass | 36 (65.46%) |
| Femoropopliteal bypass | 11 (20.00%) |
| Iliofemoral bypass | 5 (9.09%) |
| Aortofemoral bypass | 3 (5.45%) |
| Time after primary procedure to diagnosis of anastomotic aneurysm (years) | 8.78 (0.21–25.24, IQR: 8.70) |
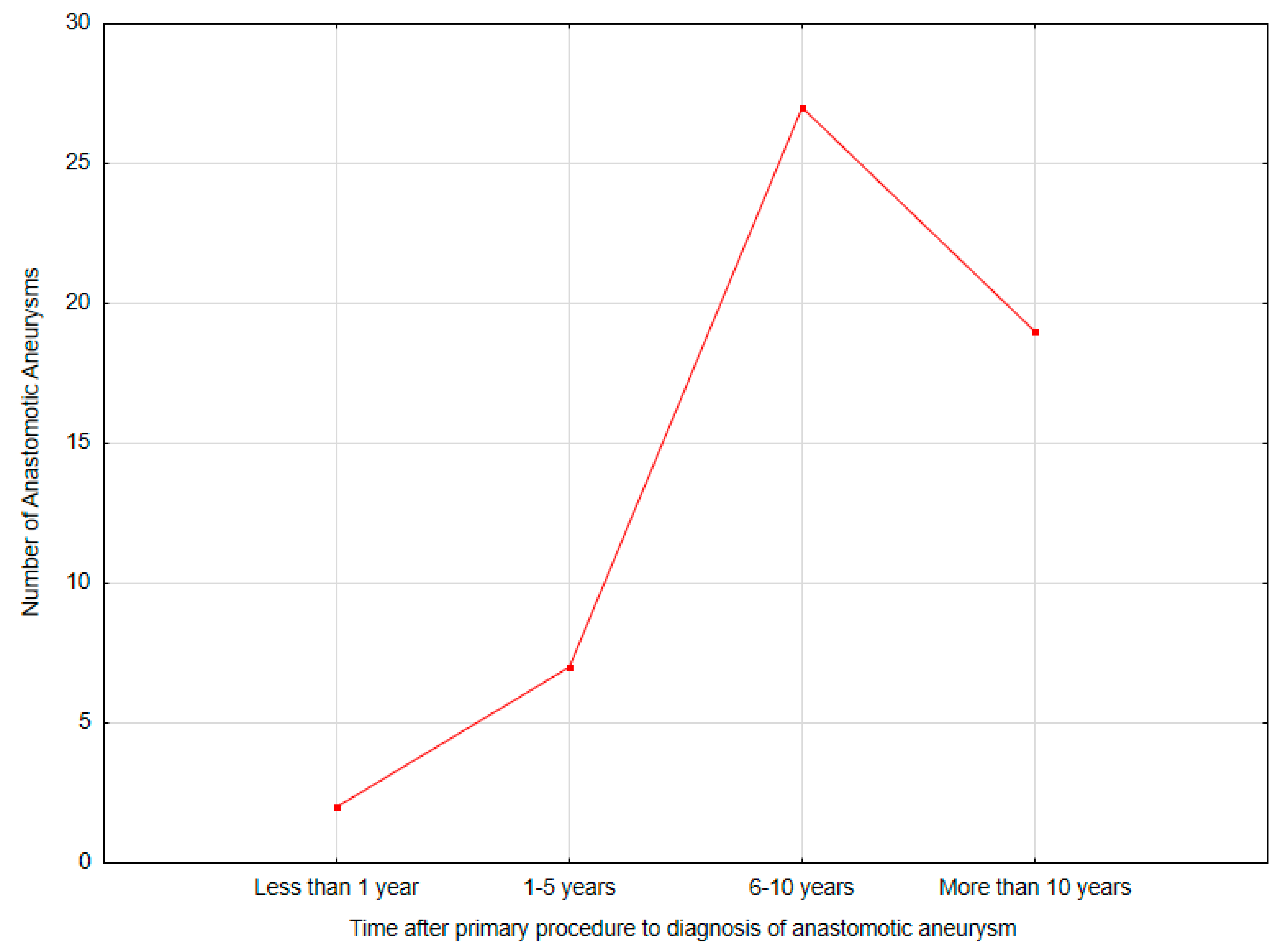
| Time after primary procedure to diagnosis of anastomotic pseudoaneurysm (time groups) | |
| Less than 1 year | 2 (3.64%) |
| 1–5 years | 7 (12.73%) |
| 6–10 years | 27 (49.09%) |
| More than 10 years | 19 (34.55%) |
| Anastomotic pseudoaneurysm localization | |
| Common femoral artery | 50 (90.91%) |
| Popliteal artery | 3 (5.45%) |
| Superficial femoral artery | 1 (1.82%) |
| Deep femoral artery | 1 (1.82%) |
| Pseudoaneurysm size (mm) | 38 (18–260, IQR: 24) |
| Variable | n (%), Mean/Median (Range, SD/IQR) |
|---|---|
| Duration of procedure (minutes) | 150 (55–365, IQR: 60) |
| Type of procedure | |
| Aneurysmectomy with graft interposition | 46 (83.64%) |
| Aneurysmectomy with extra-anatomical bypass | 6 (10.91%) |
| EVAR | 3 (5.45%) |
| Intraoperative blood loss | |
| <400 mL | 52 (94.55%) |
| >400 mL | 3 (5.45%) |
| Transfusion of red blood cells | 2 (3.64%) |
| Transfusion of fresh frozen plasma | 1 (1.82%) |
| Graft material | |
| Synthetic | 47 (85.45%) |
| Patient’s vein | 4 (7.27%) |
| Non-reversed saphenous vein | 3 (5.45%) |
| In situ saphenous vein | 1 (1.82%) |
| Duration of hospitalization (days) | 8 (4–100, IQR: 4) |
| Duration of hospitalization after procedure (days) | 4 (2–90, IQR: 4) |
| Postoperative complications (yes) * | 9 (16.36%) |
| Acute limb ischemia | 3 (5.45%) |
| Surgical site infection | 3 (5.45%) |
| Myocardial infarction | 2 (3.64%) |
| Hematoma | 2 (3.64%) |
| Reoperations | 5 (11.11%) |
| Variable | n (%), Mean/Median (Range, SD/IQR) |
|---|---|
| Follow-up time (months) | 16.5 (1–67, IQR: 33) |
| Late complications * | 17 (30.91%) |
| Acute limb ischemia | 4 (7.27%) |
| Graft infection | 4 (7.27%) |
| Anastomotic aneurysm recurrence | 4 (7.27%) |
| Chronic limb ischemia | 2 (3.64%) |
| Myocardial infarction | 2 (3.64%) |
| Late reoperations | 10 (18.18%) |
| Mortality | 6 (10.91%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Łacna, J.; Serafin, M.; Łyko-Morawska, D.; Szostek, J.; Stańczyk, D.; Kania, I.; Mąka, M.; Kuczmik, W. Para-Anastomotic Pseudoaneurysms as a Long-Term Complication After Surgical Treatment of Peripheral Artery Disease: Clinical Characteristics and Surgical Treatment. Biomedicines 2024, 12, 2727. https://doi.org/10.3390/biomedicines12122727
Łacna J, Serafin M, Łyko-Morawska D, Szostek J, Stańczyk D, Kania I, Mąka M, Kuczmik W. Para-Anastomotic Pseudoaneurysms as a Long-Term Complication After Surgical Treatment of Peripheral Artery Disease: Clinical Characteristics and Surgical Treatment. Biomedicines. 2024; 12(12):2727. https://doi.org/10.3390/biomedicines12122727
Chicago/Turabian StyleŁacna, Julia, Michał Serafin, Dorota Łyko-Morawska, Julia Szostek, Dariusz Stańczyk, Iga Kania, Magdalena Mąka, and Waclaw Kuczmik. 2024. "Para-Anastomotic Pseudoaneurysms as a Long-Term Complication After Surgical Treatment of Peripheral Artery Disease: Clinical Characteristics and Surgical Treatment" Biomedicines 12, no. 12: 2727. https://doi.org/10.3390/biomedicines12122727
APA StyleŁacna, J., Serafin, M., Łyko-Morawska, D., Szostek, J., Stańczyk, D., Kania, I., Mąka, M., & Kuczmik, W. (2024). Para-Anastomotic Pseudoaneurysms as a Long-Term Complication After Surgical Treatment of Peripheral Artery Disease: Clinical Characteristics and Surgical Treatment. Biomedicines, 12(12), 2727. https://doi.org/10.3390/biomedicines12122727






