Abstract
Background: The objective of this study was to investigate the effect of ultrasound-guided corticosteroid injection to the subacromial-subdeltoid bursa (SSB) and coracohumeral ligament (CHL) in treating adhesive capsulitis, with a particular focus on evaluating the potential benefits of regular electrotherapy and conventional rehabilitation exercises. Methods: A total of 29 patients with unilateral shoulder pain and restricted shoulder range of motion (ROM) were included. Corticosteroids were delivered to the subacromial-subdeltoid bursa (SSB) and coracohumeral ligament (CHL) through a single percutaneous injection. Group 1 consisted of 18 patients who received injections only, while Group 2 comprised 11 patients who received injections in combination with regular physiotherapy. Shoulder Pain and Disability Index (SPADI) scores and ROM were assessed before the injection, and again at 4, 8, and 12 weeks following the intervention. A multivariate mixed-effects model with repeated measurements was conducted for the variables. Results: Electrotherapy and traditional rehabilitation exercises did not enhance the effectiveness of this injection approach. Pain, upper extremity function, and ROM in all planes were all significantly improved with a corticosteroid injection to the CHL and SSB. Conclusions: Physiotherapy did not offer additional benefits when combined with ultrasound-guided corticosteroid injection to the CHL and SSB. The injection alone significantly improved pain, disability, and ROM in patients with adhesive capsulitis. Further research is required to optimize current physiotherapy with electrotherapy and traditional rehabilitation exercises after ultrasound-guided corticosteroid injections.
1. Introduction
Shoulder pain is the third most frequently encountered musculoskeletal complaint in clinics and imposes a significant burden on patients’ daily activities as well as healthcare costs []. Adhesive capsulitis is a common shoulder disorder with a lifetime prevalence of 2–5%, particularly affecting middle-aged women [,]. Commonly referred to as “frozen shoulder”, the condition is characterized by pain and progressive, global glenohumeral joint range of motion (ROM) limitation []. Although adhesive capsulitis is generally considered a self-limiting disease that resolves within two to three years, symptoms can be debilitating and may persist in up to 50% of patients [].
Pathogenesis of adhesive capsulitis is complex and likely multifactorial. Chronic inflammation, fibroblast proliferation, and an imbalance in extracellular matrix turnover ultimately lead to capsular stiffness []. Notably, the predominant pathological changes are found at the rotator interval, both radiologically and histologically [,,]. The rotator interval is a triangular anatomical space located at the anterosuperior aspect of the shoulder, bordered superiorly by the supraspinatus, inferiorly by the subscapularis, and with the coracoid process forming its base []. Key structures within this interval include the coracohumeral ligament (CHL), the superior glenohumeral ligament (SGHL), the long head of the biceps tendon, and the anterior joint capsule. These components play a critical role in maintaining the stability of the glenohumeral joint. Contracture of the rotator interval along with fibrosis, hyalinization, and fibroid degeneration of the CHL have been linked to the loss of shoulder external rotation in adhesive capsulitis [,]. On the other hand, studies have found elevated levels of inflammatory mediators not only in the joint capsule but also in the subacromial-subdeltoid bursa (SSB) [,,,].
There is a wide variety of treatments available for adhesive capsulitis, ranging from non-operative approaches such as nonsteroidal anti-inflammatory drugs (NSAIDs), physiotherapy, corticosteroid injections, and joint hydrodilatation, to surgical options like manipulation under anesthesia and arthroscopic capsular release []. Corticosteroids exert a general suppressive effect on the inflammatory response and inhibit the differentiation of fibroblasts into myofibroblasts. Given that both the SSB and the CHL play a role in the development of adhesive capsulitis—with the CHL primarily contributing to the loss of external rotation—we adopted an extra-articular approach. These two sites can be efficiently and accurately targeted under ultrasound guidance through the same puncture site.
The objective of this study was to assess the effectiveness of SSB and CHL corticosteroids injection in treating adhesive capsulitis, with a specific emphasis on examining the potential additional benefits of electrotherapy and conventional rehabilitation exercises.
2. Materials and Methods
2.1. Participants
Patients with unilateral shoulder pain and restricted ROM were recruited from outpatient clinics. Our study was approved by the institution review board of a tertiary medical center (IRB ID: 201407713A3C501). All patients signed informed consent before participation. Inclusion criteria were as follows: (1) aged between 20 and 70 years, (2) unilateral shoulder pain lasting more than one month with a Numerical Rating Scale (NRS) score greater than 3, and (3) restricted shoulder ROM in the coronal, sagittal, and frontal planes. The exclusion criteria were (1) sonography-confirmed supraspinatus tendon tear, (2) presence of calcified tendinopathy, (3) presence of cervical radiculopathy, (4) a history of tumors in the shoulder region, (5) receipt of corticosteroid injections or physical therapy for the affected shoulder within the previous three months, (6) a history of cerebrovascular accidents, and (7) allergy to corticosteroid injections.
A total of 29 patients, comprising 23 females and 6 males, were included in the study. The patients were subsequently divided into two groups. Group 1 consisted of 18 patients who received corticosteroid injections only, while Group 2 included 11 patients who received injections in combination with regular electrotherapy and conventional rehabilitation exercises during the 12-week follow-up period. Table 1 presents demographics and baseline characteristics for the two groups. These two groups were compatible with respect to age, height, weight, and body mass index (BMI), and no significant difference in shoulder ROM and SPADI at baseline was found in these two groups (p > 0.05).

Table 1.
Demographic data.
2.2. Ultrasound Examination and Intervention
Shoulder ultrasound examination was conducted following standard protocol [] using a Philips iU22 ultrasound machine equipped with a probe frequency range of 5–12 MHz. The same senior ultrasound operator performed all ultrasound examinations and injections in this study with dynamic focus, gain, and time-gain compensation settings fixed.
To perform ultrasound-guided corticosteroid injections targeting the SSB and CHL, patients were positioned in a side-lying posture, with the arm fully internally rotated and placed behind the back, and the elbow flexed. A round pillow was positioned under the upper back to ensure posture stability (Figure 1).

Figure 1.
Patient positioning.
Two syringes of injectates were prepared, each containing a mixture of 7 mg betamethasone and 4 mL of 1% lidocaine. A 23-gauge, 2.5-inch needle was used for the injections. The ultrasound transducer was first placed over the lateral border of the coracoid process and supraspinatus tendon to obtain the axial oblique view (Figure 2a). The SSB was revealed between the deltoid muscle and supraspinatus tendon, and the CHL was seen as a hyperechoic band between the SSB and coracoid process (Figure 2b). The needle traveled through the SSB and ended up at the CHL to deliver the first injection (Figure 2c). The probe was then turned about 90 degrees and repositioned to the long-axis view of the supraspinatus tendon (Figure 3a). Afterward, the needle was redirected along the long-axis, from medial to lateral, targeting the SSB. The second injection was administered at this site (Figure 3b) []. This approach offered two key advantages: (1) The entire stretch of the CHL could be visualized, allowing precise drug delivery along the ligament; and (2) a single puncture site could be used to access both the CHL and SSB, minimizing patient discomfort during the procedure. If the patient could not achieve at least 80% of the ROM compared to the unaffected side in the sagittal, frontal, and transverse planes, an additional injection was administered after a four-week interval. The maximum number of injection sessions allowed was three. Acetaminophen was given in case of pain.
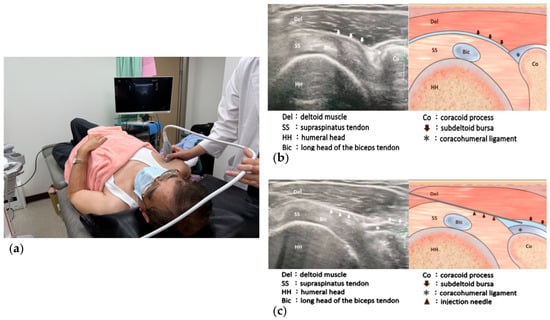
Figure 2.
(a) Patient positioning and transducer placement for ultrasound-guided injection to the coracohumeral ligament (CHL); (b) Ultrasound image and illustration of the supraspinatus tendon axial oblique view; (c) Ultrasound image and illustration of the needle targeting the subacromial-subdeltoid bursa and CHL.
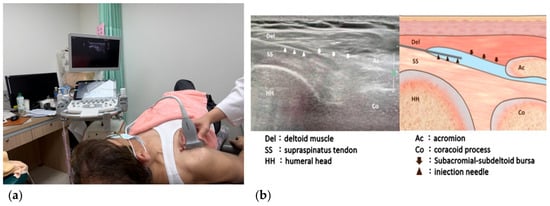
Figure 3.
(a) Patient positioning and transducer placement for ultrasound-guided injection to the subacromial-subdeltoid bursa (SSB); (b) Ultrasound image and illustration of the needle passing through the SSB along the long axis of supraspinatus tendon.
2.3. Clinical Assessment
The Shoulder Pain and Disability Index (SPADI) and shoulder ROM at the point where pain occurred were used as outcome measures. The clinical assessments were performed before the injection, 4 weeks (first endpoint), 8 weeks (second endpoint), and 12 weeks (third endpoint) following the initial injection of the SSB and CHL.
2.4. Shoulder Pain and Disability Index (SPADI)
SPADI is a self-administered questionnaire which evaluates pain and functional activities. It contains 13 questions: five addressing the severity of pain and eight focusing on the difficulty of daily living activities that involve upper-extremity use. [,]. The SPADI demonstrated satisfactory reliability and validity properties in patients with frozen shoulder []. The original version of the SPADI was well adapted and translated into Chinese. The Cronbach alpha ranged from 0.812 to 0.912 in all subscales and total scale of the Chinese-SPADI, indicating good or excellent internal consistency. The test–retest reliability (ICC = 0.887–0.915, SEM = 5.47, MDC = 15.16) was proven to be good or excellent []. Pain score, disability score, and the total SPADI score were calculated based on the patients’ responses.
2.5. Range of Motion (ROM) of Shoulder
Standard universal goniometric assessments were performed to evaluate bilateral shoulder ROM. All measurements were conducted by the same occupation therapist.
For shoulder flexion, patients were positioned supine. Goniometric measurements were taken with the fulcrum placed anterior to the acromion process, the stationary arm aligned parallel to the midaxillary line, and the moving arm aligned with the midline of the humerus. For shoulder extension, patients were positioned prone. The fulcrum was placed anterior to the acromion process, the stationary arm was aligned parallel to the midaxillary line, and the moving arm was aligned with the midline of the humerus. For shoulder internal rotation, patients were positioned supine with the shoulder abducted to 90 degrees and the elbow flexed to 90 degrees. The fulcrum was placed over the olecranon process of the ulna, with the stationary arm aligned vertically and the moving arm aligned with the ulnar styloid process. For shoulder external rotation, patients were also positioned supine with the shoulder abducted to 90 degrees and the elbow flexed to 90 degrees. The fulcrum was placed over the olecranon process of the ulna, the stationary arm aligned vertically, and the moving arm aligned with the ulnar styloid process. For shoulder abduction, patients were kept in prone position, and goniometric assessments were conducted by placing the fulcrum and body anterior to the acromion process, the stationary arm parallel to the midline of the trunk, and the moving arm aligned with the midline of the humeral bone. For shoulder abduction, patients were positioned prone. Goniometric assessments were performed by placing the fulcrum anterior to the acromion process, aligning the stationary arm parallel to the midline of the trunk, and aligning the moving arm with the midline of the humerus.
Riddle et al. revealed that intraclass correlation coefficients (ICCs) for intratester reliability were 0.98 for flexion, 0.98 for abduction, 0.94 for extension, 0.90 for horizontal adduction, 0.99 for lateral rotation, and 0.94 for medial rotation. ICCs reflecting intertester reliability were notably lower, ranging from 0.26 to 0.90 [].
2.6. Statistical Analysis
Two sample t-test was used to compare differences of age, height, weight, BMI, and baseline ROM and SPADI between Group 1 and Group 2. Fisher’s exact test was used to compare the difference of gender distributions between the 2 groups.
Comparisons of ROM and SAPDI across over all time points between the 2 groups were assessed by mixed effects model with repeated measurements (MMRM) analysis. The MMRM analysis was based on unstructured variance–covariance matrix and denominator degree of freedom using the Kenward Roger method including a between-group fixed effect (Group 1 vs. Group 2) and a within-patient repeated factor (evaluation time: pre-treatment, 4 weeks after treatment, 8 weeks after treatment, and 12 weeks after treatment), as well as group-by-time interaction with individual patient as a cluster unit. Additionally, the MMRM model also included the ROM assessment from the untreated (normal) arm and time-by-ROM assessment from the untreated (normal) arm as covariates.
All significance levels were set at two-sided p < 0.05, and SAS Studio version 3.1M1 was used to perform all statistical analyses.
This is a preliminary proof-of-concept study; as such, the sample size is not powered. Further enrollment will be continued and the study will be powered for confirmatory purpose.
3. Results
3.1. Shoulder Pain and Disability Index (SPADI)
Table 2 and Figure 4 summarize the effect of time and group on pain score, disability score, and total SPADI score. Significant improvement over time was found for all of the three scores. However, the within-group comparison for these three scores illustrated that significant improvements were identified at all post-treatment timepoints in Group 1 but only at week 8 in Group 2. No significant time-by-group interaction was identified for pain scores. Group 1 tended to achieve more favorable outcomes on the disability score (p = 0.0723 for time-by-group interaction) and total score (p = 0.0877 for time-by-group interaction).

Table 2.
Shoulder Pain and Disability Index.
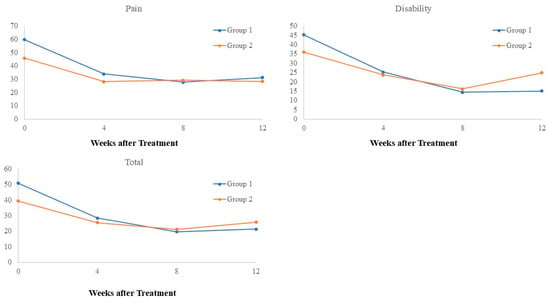
Figure 4.
Effect of time and group on SPADI.
3.2. Shoulder Range of Motion (ROM)
Table 3 and Figure 5 summarize the active range of motion (AROM) of the shoulder. Significant improvements in flexion, abduction, and external rotation were observed in both groups at 4, 8, and 12 weeks post-treatment. However, no significant time-by-group interactions were detected for these movements. For internal rotation, Group 1 showed significant improvements at 4 and 12 weeks post-treatment, whereas Group 2 demonstrated significant improvements at all post-treatment time points. Despite these differences, the time-by-group interaction was not significant for internal rotation. Conversely, a significant time-by-group interaction was observed for extension (p = 0.0371). Group 1 showed no significant changes in extension across all time points, while Group 2 exhibited an increase in extension ROM at week 8 followed by a decrease at week 12. However, these changes in Group 2 were not statistically significant.

Table 3.
Effect of time and group on AROM.
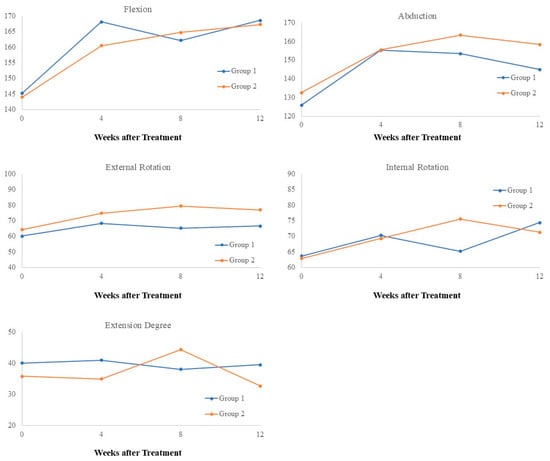
Figure 5.
Effect of time and group on AROM.
Table 4 and Figure 6 present the passive range of motion (PROM) of the shoulder. Significant improvements in flexion and abduction were observed in both groups. However, Group 1 showed significant improvements at all post-treatment time points, while Group 2 displayed improvements only at weeks 4 and 8. For internal rotation, significant improvements were observed across all post-treatment time points in both groups, with no significant time-by-group interaction detected. For external rotation, Group 1 demonstrated significant improvements across all post-treatment time points, while no significant improvements were noted in Group 2. The time-by-group interaction for external rotation was not significant (p = 0.4658). Regarding extension, no significant improvements were observed in Group 1 across all time points. In Group 2, extension ROM did not significantly change at weeks 4 and 8 but showed significant deterioration at week 12. A significant time-by-group interaction was noted for extension ROM (p = 0.0512).

Table 4.
Effect of time and group on PROM.
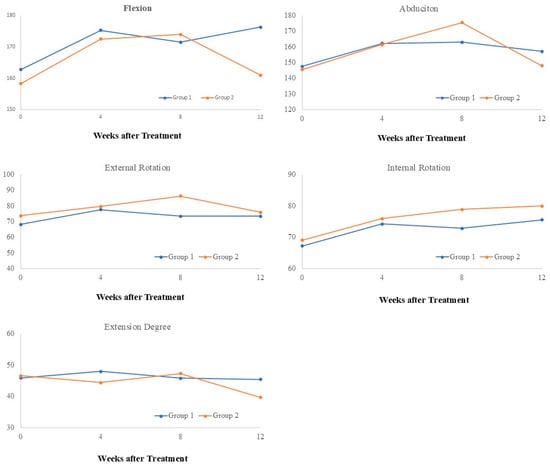
Figure 6.
Effect of time and group on PROM.
Overall, these results illustrate that injection of corticosteroid provided significant improvements in ROM in both groups. Notably, eight patients (five from Group 1 and three from Group 2) achieved more than 80% ROM in all planes after the first injection and therefore did not require a second one. Following the second injection, 10 patients (five from each group) reached more than 80% ROM compared to the unaffected side in all planes and subsequently did not require further treatment.
4. Discussion
The main finding of this study was that physiotherapy did not enhance the effectiveness of a single percutaneous ultrasound-guided injection to the SSB and CHL in treating adhesive capsulitis. This injection approach resulted in significant improvements in pain, upper extremity function, and ROM across the frontal, sagittal, and coronal planes.
Pain reduction as well as functional improvement and restoration in flexion, abduction, and external rotation ROM were observed after a single ultrasound-guided steroid injection to the SSB and CHL. Additional improvement of internal rotation ROM was seen with repeat injections in both Group 1 and Group 2. Therefore, a thorough evaluation of the ROM limitation should be performed prior to the injection, and the consecutive injections might be needed when the limitation is severe and internal rotation limitation is considerably serious.
Dual-target ultrasound corticosteroid injections have been purposely repeatedly in order to enhance treatment effect and lower patient discomfort. This approach most commonly targets the SSB/supraspinatus tendon and the long head of the biceps tendon. It has shown to extend the duration of pain relief in shoulder impingement cases and has produced greater improvements in pain, ROM, and function in hemiplegic shoulders [,]. The distinct pathology of adhesive capsulitis warrants a different dual-target approach, focusing on the SSB and CHL, which can be achieved through a single injection following our protocol. With thorough anatomical knowledge and the aid of ultrasound guidance, direct puncture of the tendon can be avoided. This allows corticosteroids to suppress inflammation and facilitate tissue remodeling to their fullest potential.
The optimal injection strategy for adhesive capsulitis remains a subject of debate. Hydrodilatation of the glenohumeral joint is a long-established treatment for adhesive capsulitis, aimed at stretching the contracted joint cavity and reducing intra-articular inflammation. A Cochrane systematic review analyzing five studies found that only one had a low risk of bias. This study demonstrated that joint distension with saline and corticosteroids was more effective than a placebo in improving pain, function, and ROM at the three-week follow-up. However, the benefits were inconsistent at 6 and 12 weeks []. In a 2019 meta-analysis, Shang et al. [] compared the effects of intra-articular and subacromial corticosteroid injections in patients with adhesive capsulitis. The study found no significant differences in flexion, abduction, and external ROM up to 24 weeks, nor in VAS pain scores beyond the three-week mark. Additionally, a recent prospective clinical trial involved 54 patients with adhesive capsulitis, who were administered 1 mL of triamcinolone acetonide (20 mg/mL) and 1 mL of prilocaine (2%) either anteriorly, between the CHL and the biceps tendon, or posteriorly into the joint []. Improvements in pain, function, and active ROM were similar between the two groups during the six-week follow-up period. Our findings aligned with the existing literature and underscored the effectiveness of extra-articular injections in the management of adhesive capsulitis. Furthermore, intra-articular communication with the subacromial space may occur in cases of adhesive capsulitis, potentially leading to corticosteroid leakage and providing additional therapeutic effects. Clinicians should consider both intra-articular and extra-articular injection techniques as viable treatment options for managing patients with this condition.
Interestingly, in the group combining corticosteroids injection and rehabilitation, the restoration of flexion was impeded and a second injection was necessitated. Meanwhile, abduction ROM failed to increase at the second and third endpoints. A meta-analysis based on two studies involving 86 participants suggested that adding manual therapy, exercise, and electrotherapy to intra-articular corticosteroid injections did not result in better outcomes in terms of pain, function, or quality of life []. Moreover, according to a meta-analysis including 2402 participants, intra-articular corticosteroids injection was only superior to physiotherapy for ER ROM during the first 6 weeks []. The results for pain, function, and mid- to long-term ROM were similar between the two approaches []. Moreover, cost-effectiveness analysis indicated that corticosteroid injections alone may be more cost-effective than corticosteroids with adjuvant physiotherapy or physiotherapy alone []. It is important to note that the nature and duration of rehabilitation programs vary greatly, and manipulation techniques are dependent on the therapist’s expertise. The long-term outcomes of physiotherapy remain uncertain due to the limited evidence. Currently, there are no definitive guidelines for the clinical management of adhesive capsulitis. Nevertheless, our results emphasize the promise and cost-effectiveness of using extra-articular corticosteroid injections as a standalone treatment option.
There were several limitations in this study. First, the sample size was relatively small, which may limit the generalizability of the findings. Second, the follow-up period was restricted to only three months, which may not have been sufficient to fully capture the long-term effects of the treatment or potential relapses. Third, we did not conduct subgroup analyses based on the stage of the disease (e.g., freezing, frozen, and thawing stages), which may have influenced the treatment outcomes. Future research should include patients at various disease stages and follow them for longer periods to allow for a more comprehensive assessment. Finally, conclusions regarding the optimal type or duration of rehabilitative intervention could not be drawn from this study. It remains unclear whether certain rehabilitation protocols are more effective than others when combined with injection therapy. Further studies are necessary to identify the most effective rehabilitation strategies to maximize patient recovery.
5. Conclusions
Physiotherapy did not provide additional benefits for patients with adhesive capsulitis beyond those achieved with a dual-target, ultrasound-guided corticosteroid injection targeting the SSB and CHL. The injection alone was effective in decreasing shoulder pain and disability. Significant improvements in shoulder ROM were also achieved. This approach may serve as a viable treatment option for affected patients. Because of the small sample size of this study, larger-scale research to optimize current physiotherapy with electrotherapy and traditional rehabilitation exercises after ultrasound-guided corticosteroid injections is warranted.
Author Contributions
Conceptualization, C.-W.T. and F.-T.T.; methodology, C.-W.T.; software, C.-W.T.; validation, C.-W.T. and F.-T.T.; formal analysis, C.-W.T. and P.-C.S.; investigation, T.-Y.L. and P.-C.S.; data curation, T.-Y.L. and P.-C.S.; writing—original draft preparation, C.-W.T.; writing—review and editing, T.-Y.L.; visualization, P.-C.S.; supervision, F.-T.T.; project administration, F.-T.T.; funding acquisition, F.-T.T. All authors have read and agreed to the published version of the manuscript.
Funding
This project was supported by the Chang Gung Medical Foundation, project number: CMRPG3F0541, and by the Lo Hsu Medical Foundation.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Chang Gung Medical Foundation. The IRB ID was 201407713A3C501.
Informed Consent Statement
Informed consent was obtained from all patients involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
We express our appreciation to Wei-Jen Chang for his illustrations of the injection procedure.
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- Schwarzkopf, R.; Oron, A.; Loebenberg, M. Shoulder pain: Assessment, diagnosis and treatment of common problems. Harefuah 2008, 147, 71–76, 93. [Google Scholar] [PubMed]
- Fields, B.K.K.; Skalski, M.R.; Patel, D.B.; White, E.A.; Tomasian, A.; Gross, J.S.; Matcuk, G.R. Adhesive capsulitis: Review of imaging findings, pathophysiology, clinical presentation, and treatment options. Skelet. Radiol. 2019, 48, 1171–1184. [Google Scholar] [CrossRef] [PubMed]
- Millar, N.L.; Meakins, A.; Struyf, F.; Willmore, E.; Campbell, A.L.; Kirwan, P.D.; Akbar, M.; Moore, L.; Ronquillo, J.C.; Murrell, G.A.; et al. Frozen shoulder. Nat. Rev. Dis. Primers 2022, 8, 59. [Google Scholar] [CrossRef] [PubMed]
- Le, H.V.; Lee, S.J.; Nazarian, A.; Rodriguez, E.K. Adhesive capsulitis of the shoulder: Review of pathophysiology and current clinical treatments. Shoulder Elb. 2017, 9, 75–84. [Google Scholar] [CrossRef]
- Ozaki, J.; Nakagawa, Y.; Sakurai, G.; Tamai, S. Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J. Bone Jt. Surg. 1989, 71, 1511–1515. [Google Scholar] [CrossRef]
- Homsi, C.; Bordalo-Rodrigues, M.; Da Silva, J.J.; Stump, X.M. Ultrasound in adhesive capsulitis of the shoulder: Is assessment of the coracohumeral ligament a valuable diagnostic tool? Skelet. Radiol. 2006, 35, 673–678. [Google Scholar] [CrossRef]
- Stella, S.M.; Gualtierotti, R.; Ciampi, B.; Trentanni, C.; Sconfienza, L.M.; Del Chiaro, A.; Pacini, P.; Miccoli, M.; Galletti, S. Ultrasound features of adhesive capsulitis. Rheumatol. Ther. 2022, 9, 481–495. [Google Scholar] [CrossRef]
- Gaskill, T.R.; Braun, S.; Millett, P.J. The Rotator Interval: Pathology and Management. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 556–567. [Google Scholar] [CrossRef]
- Petchprapa, C.N.; Beltran, L.S.; Jazrawi, L.M.; Kwon, Y.W.; Babb, J.S.; Recht, M.P. The Rotator Interval: A Review of Anatomy, Function, and Normal and Abnormal MRI Appearance. Am. J. Roentgenol. 2010, 195, 567–576. [Google Scholar] [CrossRef]
- Lho, Y.-M.; Ha, E.; Cho, C.-H.; Song, K.-S.; Min, B.-W.; Bae, K.-C.; Lee, K.-J.; Hwang, I.; Park, H.-B. Inflammatory cytokines are overexpressed in the subacromial bursa of frozen shoulder. J. Shoulder Elb. Surg. 2013, 22, 666–672. [Google Scholar] [CrossRef]
- Bunker, T.D.; Reilly, J.; Baird, K.S.; Hamblen, D.L. Expression of growth factors, cytokines and matrix metalloproteinases in frozen shoulder. J. Bone Jt. Surg. 2000, 82, 768–773. [Google Scholar] [CrossRef]
- Kabbabe, B.; Ramkumar, S.; Richardson, M. Cytogenetic analysis of the pathology of frozen shoulder. Int. J. Shoulder Surg. 2010, 4, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Saccomanni, B. Inflammation and shoulder pain--a perspective on rotator cuff disease, adhesive capsulitis, and osteoarthritis: Conservative treatment. Clin. Rheumatol. 2009, 28, 495–500. [Google Scholar] [CrossRef]
- Ramirez, J. Adhesive capsulitis: Diagnosis and management. Am. Fam. Physician 2019, 99, 297–300. [Google Scholar]
- Lee, M.H.; Sheehan, S.E.; Orwin, J.F.; Lee, K.S. Comprehensive Shoulder US Examination: A Standardized Approach with Multimodality Correlation for Common Shoulder Disease. RadioGraphics 2016, 36, 1606–1627. [Google Scholar] [CrossRef]
- Chang, K.-V.; Mezian, K.; Naňka, O.; Wu, W.-T.; Lin, C.-P.; Özçakar, L. Ultrasound-guided interventions for painful shoulder: From anatomy to evidence. J. Pain Res. 2018, 11, 2311–2322. [Google Scholar] [CrossRef] [PubMed]
- Roach, K.E.; Budiman-Mak, E.; Songsiridej, N.; Lertratanakul, Y. Development of a shoulder pain and disability index. Arthritis Rheum. 1991, 4, 143–149. [Google Scholar] [CrossRef]
- Williams, J.W., Jr.; Holleman, D.R.; Simel, D.L. Measuring shoulder function with the Shoulder Pain and Disability Index. J. Rheumatol. 1995, 22, 727–732. [Google Scholar]
- Venturin, D.; Giannotta, G.; Pellicciari, L.; Rossi, A.; Pennella, D.; Goffredo, M.; Poser, A. Reliability and validity of the Shoulder Pain and Disability Index in a sample of patients with frozen shoulder. BMC Musculoskelet. Disord. 2023, 24, 212. [Google Scholar] [CrossRef]
- Wang, W.; Jia, Z.-Y.; Liu, J.; Xie, Q.-Y.; Cui, J.; Zheng, W.; Xu, W.-D. Cross-cultural adaptation and validation of the Chinese version of the shoulder pain and disability index in patients with symptomatic shoulder pain A prospective case series. Medicine 2018, 97, e11227. [Google Scholar] [CrossRef]
- Riddle, D.L.; Rothstein, J.M.; Lamb, R.L. Goniometric reliability in a clinical setting. Shoulder measurements. Phys. Ther. 1987, 67, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-C.; Chang, K.-V.; Wu, W.-T.; Han, D.-S.; Özçakar, L. Ultrasound-Guided Standard vs Dual-Target Subacromial Corticosteroid Injections for Shoulder Impingement Syndrome: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2019, 100, 2119–2128. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; Zhang, T.; Liu, W.; Lu, M.; Wang, Y. The Effectiveness of Ultrasound-Guided Subacromial-Subdeltoid Bursa Combined With Long Head of the Biceps Tendon Sheath Corticosteroid Injection for Hemiplegic Shoulder Pain: A Randomized Controlled Trial. Front. Neurol. 2022, 13, 899037. [Google Scholar] [CrossRef] [PubMed]
- Buchbinder, R.; Green, S.; Youd, J.M.; Johnston, R.V.; Cumpston, M. Arthrographic distension for adhesive capsulitis (frozen shoulder). Cochrane Database Syst. Rev. 2008, CD007005. [Google Scholar] [CrossRef] [PubMed]
- Shang, X.; Zhang, Z.; Pan, X.; Li, J.; Li, Q. Intra-Articular versus Subacromial Corticosteroid Injection for the Treatment of Adhesive Capsulitis: A Meta-Analysis and Systematic Review. BioMed Res. Int. 2019, 2019, 1274790. [Google Scholar] [CrossRef]
- Sensoz, E.; Sevım, O.F.; Cakmak, H.; Edız, S.S.; Ecevız, E.; Ergun, S. Similar short-term outcomes of ultrasound guided posterior intra-articular and anterior extra-articular corticosteroid injection in the treatment of primary frozen shoulder. A randomized controlled, single-blind study. Acta Orthop. Traumatol. Turc. 2024, 58, 223–228. [Google Scholar] [CrossRef]
- Page, M.J.; Green, S.; Kramer, S.; Johnston, R.V.; McBain, B.; Chau, M.; Buchbinder, R. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst. Rev. 2014, 2014, CD011275. [Google Scholar] [CrossRef]
- Challoumas, D.; Biddle, M.; McLean, M.; Millar, N.L. Comparison of Treatments for Frozen Shoulder: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e2029581. [Google Scholar] [CrossRef]
- Maund, E.; Craig, D.; Suekarran, S.; Neilson, A.; Wright, K.; Brealey, S.; Dennis, L.; Goodchild, L.; Hanchard, N.; Rangan, A.; et al. Management of frozen shoulder: A systematic review and cost-effectiveness analysis. Health Technol. Assess. 2012, 16, 1–419. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).